Abstract
Background
Prescription quality can be a direct predictor of the net outcome of a health care delivery effort. Quality of prescription may be considered as a cumulative matrix of multiple components of a prescription on the basis of their relative importance. Prescription quality index is a recognized tool in clinical medicine for multiple purposes including the prediction of health care intervention outcome.
Objectives
Considering the importance of prescription quality among every system of medicine, an attempt was made to design a prescription quality index for Ayurveda.
Materials and methods
The Prescription Quality Index for Ayurveda was designed through item selection following a thorough literature search and was validated through multiple peer group discussions. Final draft of index containing 38 individual items carrying different scores as per their importance in the prescription was subjected to a pilot test upon 1576 indoor prescriptions generated in 2015 at State Ayurvedic College Hospital, Lucknow.
Results
The study revealed large information gaps in the components of the prescription where it was supposed to be noted by the prescribers. These gaps in the Ayurvedic prescriptions were most significant in the areas pertaining to Ayurvedic fundamentals of clinical examination, disease diagnosis and Ayurvedic drug intake methods.
Conclusion
Prescription Quality Index for Ayurveda was found useful in underlining the gaps between the ideal and generated prescriptions. This can be utilized as a useful tool to evaluate the quality of Ayurvedic prescriptions by seeing their adherence to the standard prescription template.
Keywords: Prescription quality, Prescribing quality, Index, Ayurveda
1. Introduction
A medical prescription is the proposed intervention plan drafted by the concerned physician, aiming to deal with certain kind of illness of a person [1]. It forms the prime document for medical procedure or intervention to execute. Despite the differences among healthcare systems or underlying specialty, medical prescriptions have few common generic features. They usually contain the basic details of the patient and prescriber identification followed by the details of the medications including its dose, intake schedules and total duration of drug consumption. Therefore, the prescription is primarily written for the intermediary staff including nurse or pharmacist responsible for healthcare delivery in a hospital setting or for individual patient in an OP setting [2]. Besides this primary role, a prescription has its expanded role in many other domains. It acts as a piece of evidence when the illness and the treatments are linked with some legal issues. It can play the role of evidence of past illness, past treatment and past adverse events related to the drug intake and can also act as the ground paper for second opinions [3].
For the physician himself who has generated the prescription, it acts as a record to evaluate the role of interventions during follow ups. Needless to say, a good prescription also becomes the spine of evidence-based medical practice as it may lead to a good case report if the records are reported meticulously [4].
Importance of writing a good prescription in legible hand writing is beyond doubt [5]. Even a carefully drafted prescription can lead to execution problems if it is not readable. Besides legibility, there can also be other issues related with prescription writing which may eventually lead to poor execution of treatment plan or adversities in worst possible cases. Errors of omission or commission are two broad passes through which an undesired functioning of the prescription may creep in. The former one addresses the missing components of a prescription whereas the latter emphasizes the over stressed components [6]. This is a common observation that missing an instruction in the prescription makes it labile to subjective interpretations. Prescription errors are little different than prescribing errors. In the former, the focus remains on the basic format of the prescription for the ease of its execution. In the latter however, the individual components of the prescription are critically analyzed for their optimality as per the disease condition [7].
Prescriptions are the sole instruments ensuring the successful management of a disease. If the treatment is executed as per the initial plan of the physician, it is mandatory to ensure what information it should contain. A poor elaboration of the plan or an unreadable plan can lead to number of morbid eventualities. Similarly missing some essential component in a prescription can also open a wide array of unforeseen erroneous happenings in future.
Prescription Quality Index (PQI) was initially proposed as a mean to identify the prescription related errors in order to improve them further. Various PQI tools have been developed in clinical medicine addressing the prescriptions related to the type of illness or clinical specialty. These tools have been validated and are in regular use as a measure to improve the prescription quality in Allopathy [8].
Prescription quality is obviously and equally important in other systems of healthcare dealing with medicine and procedures. Ayurveda offers healthcare to its patients through variety of means including herbs, minerals, metals, animal products and also a variety of biocleansing procedures included under panchakarma. Adversities due to Ayurvedic drugs are well reported in medical literature and at occasions these adversities are reported to occur due to wrong medication, overdose, or poor quality of medicine [9]. A wrong medicine can well be the result of a clumsy prescription.
In the conventional format of prescription, disease diagnosis and a brief description favoring the arrival of the diagnosis is always mentioned. This description generates an understanding about pathogenesis and helps physician choosing most appropriate medicine for a given condition. As Ayurveda has its own understanding about the pathogenesis and derives the treatment plan on the basis of such understanding, this is obvious to advocate a mention of such findings in the Ayurvedic prescription. Poor quality of Ayurvedic prescriptions is an undercurrent observation not brought into notice frequently [10]. Ayurvedic practice of medicine is largely criticized for not utilizing its own concepts of disease diagnosis and management but rather borrowing and imposing the modern concepts of pathogenesis and treatments upon their own treatment principles [11]. There have not been serious efforts to improve the quality of practice, education and research in Ayurveda. It is for this reason, despite of a turning around of the world towards Ayurveda; it does not seem ready to utilize the opportunities coming in its way [12].
PQI can come up as a measure to delineate the unexposed errors of prescription quality in Ayurveda with a long term goal of eliminating such problems through educating the prescribers about the importance of various components of an Ayurvedic prescription. With the help of a thorough literature review, a comprehensive prescription quality index pertaining to Ayurveda was thus attempted to be developed, validated and subsequently pilot tested upon sample prescriptions at a secondary care Ayurveda teaching hospital. The index development was able to propose many constituents of Ayurvedic understanding of disease management thought important for their inclusion in a prescription. Similarly the pilot test was also able to reveal many underlying limitations in contemporary Ayurvedic prescription writing. The study has many future implications. At one point it identifies the existing gaps in contemporary Ayurvedic clinical practice and can help finding the measure to meet such gaps. At the same time, the index also proposes to act as a tool of prediction of the net outcome on the basis of quality of a prescription judged upon the basis of PQI [13].
2. Materials and methods
2.1. Setting
The study was conducted at State Ayurvedic College and Hospital, Lucknow. The development and validation of the prescription quality index for Ayurveda (PQIA) was done primarily at this setting however the face and content validity in part was done at New Delhi by involving many Ayurveda experts from Ministry of Ayush, Govt of India. The pilot testing of the PQIA was done at State Ayurvedic College and Hospital, Lucknow.
2.2. Study conduction time
The development and validation process for PQIA was carried out in 2015 and it took about 1 year. For pilot testing of the PQIA, data was collected between February 2016 to April 2016. The whole data was subsequently analyzed in later part of 2016.
2.3. Ethical clearance
An approval of the Institutional Ethics Committee at State Ayurvedic College, Lucknow was sought to conduct the study. The same was granted.
2.4. Development of the PQIA
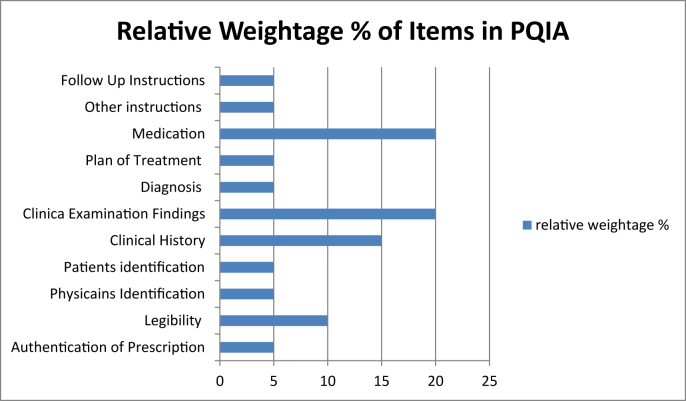
A thorough literature review was done to explore existing PQI in clinical medicine and of Ayurvedic classical literature to see the essentials of prescription in Ayurveda. A prescription was thought to contain essentially the information related to patient, physician and treatment center identification. A detailed disease and medication description from Ayurvedic perspective was also considered essential. A Donabedian conceptualization of structure, process and result was employed for the purpose of the development of initial draft of PQIA [14]. Initial draft of PQIA contained 24 items tentatively divided into the score of 100. A relative weightage was given to every item as per its importance in prescription.
2.5. Face and content validity
In the process of face and content validity, the preliminary draft of PQIA was subjected to peer review. Initial discussion among the peers (KS, SS, RB, SJ) was done at State Ayurvedic College, Lucknow which resulted in addition of 6 items, deletion of 2 items and revision of another 2 items. As a result the revised PQIA consisted 28 items. The same was again subjected to another rigorous review for language and scores. This review resulted in addition of 4 more items and subsequent adjustment of scores as per the revised items. A final review of the PQIA was done at New Delhi involving higher level professionals from Ayurvedic practice (MN, AKS, BLG, GPR, AK). This review resulted in further addition of 6 more items resulting in a total of 38 items in the finally revised PQIA. This finally revised PQIA was then subjected to language editing and score adjustments as per the relative weightage of the items (Fig. 1).
Fig. 1.
Relative weightage of various items in PQIA.
2.6. Pilot testing
Final draft of the PQIA was subjected to pilot testing upon the indoor prescriptions generated in year 2015 at State Ayurvedic College Hospital, Lucknow. The indoor prescription record was accessed from the record section of the hospital. Every prescription within the specified period was individually observed for the presence or absence of items specified in the PQIA. An individual score for each item and each prescription was calculated subsequently. The data was plotted on Microsoft Excel and was analyzed using GraphPad Quickcalcs.
2.7. Data collection
Data collection was done by the investigator; however, for better observation, at some places (particularly to judge legibility) help from junior nursing staff or residents was also sought.
3. Results
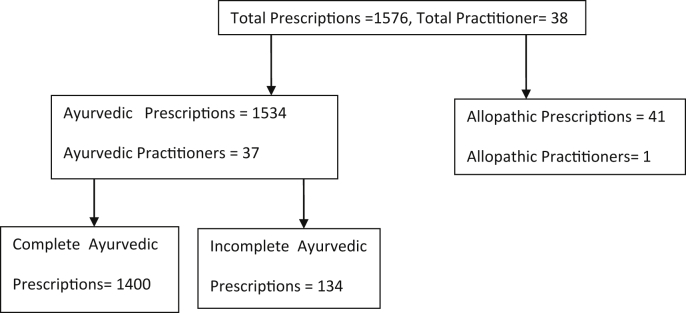
Total 1576 prescriptions were generated in year 2015 at IP section of State Ayurveda College Hospital, Lucknow. These prescriptions were generated by 38 physicians including one Allopathic physician (YKS). 41 prescriptions generated by the Allopathic physician were eliminated from the study. Remaining 1535 prescriptions given by 37 Ayurvedic physicians were screened initially for their completeness. 1400 prescription were found complete and hence included in the detailed study (Fig. 2). All 37 Ayurvedic prescribers involved in the study were evaluated for their qualification and clinical specialty. 31 (83.77%) among them had higher qualifications (MD and PhD) in Ayurveda. Among total prescribers, 26 (70.29%) were from various clinical specialties in Ayurveda.
Fig. 2.
Study flow chart.
Prescription quality score was calculated for each item on every prescription. Seeing the response of the prescriptions as per the PQIA, a floor effect and a ceiling effect was calculated which was 9 and 85 respectively. The floor effect was the minimum possible score for the index whereas the ceiling effect was the maximum possible score for the index [15]. These were calculated on the basis of total score of the items consistently reported negative in all the prescriptions (score = 0%) or consistently reported positive (score = 100%) in all the prescriptions (Table 1, Table 2). A consistent positive or negative reporting of a few items in index was endorsing its convergent validity stating for similar meaning for similar components of index. Minimum observed score in the study was 12 whereas the maximum score was 65. Average, median and mode scores for the PQIA were 34.86, 27.5 and 31.5 respectively. It was observed that approximately 87.43% prescriptions were below the half score level (below 50%) of PQIA (Table 3).
Table 1.
Items represented positively in all the prescriptions (Floor Effect).
| No. | Item | Score |
|---|---|---|
| 1 | Name, address and contact details of treatment center | 1 |
| 2 | Date of prescription | 2 |
| 3. | Signature of the prescriber | 2 |
| 4 | Name of physician | 1 |
| 5 | Name of patient | 1 |
| 6 | Age of patient | 2 |
| Total score | 9 |
Table 2.
Item represented negatively in all the prescriptions (Ceiling Effect).
| No. | Item | Score |
|---|---|---|
| 1 | Contact details of patient | 1 |
| 2 | Prakriti | 2 |
| 3 | Vikriti | 2 |
| 4 | Nadi | 2 |
| 5 | Roga Bala | 2 |
| 6 | Rogi Bala | 2 |
| 7 | Samprapti | 2 |
| 8 | Sadhya-asadhyata | 2 |
| Total score | 15 |
Table 3.
Distribution of prescription quality index score obtained.
| Score distribution group | No. of prescriptions | % |
|---|---|---|
| 0–25 | 358 | 25.57% |
| 26–50 | 866 | 61.8% |
| 51–75 | 176 | 12.56% |
| 76–100 | 0 | 0% |
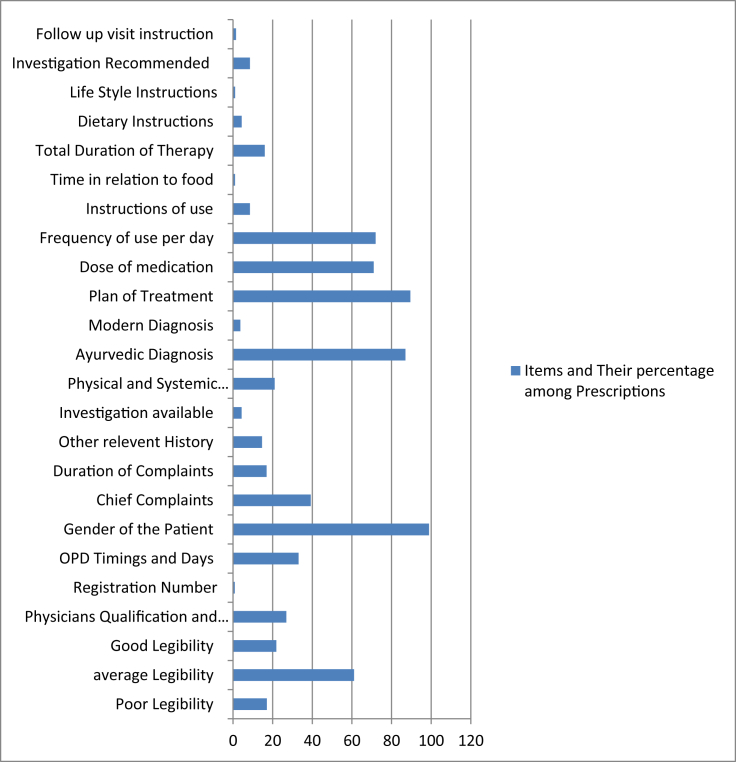
All the prescriptions screened under the study were also evaluated for the ease of their reading. For a common understanding, the legibility of prescription was divided into three categories namely poor, average and good. The help of a trainee nursing staff or a resident doctor was taken to make this judgment more objective. A prescription readable without any extra efforts was considered good. A prescription requiring some extra effort to read was considered average and the prescription requiring help of some senior staff or the clarification from the physician was considered poor in terms of legibility. Among all the prescriptions screened 239 (17.07%) were found under the category of poorly legible, 855 (61.07%) as average and 306 (21.85%) as having a good legibility (Table 4).
Table 4.
Legibility of the prescription.
| Legibility of the prescription | No. of prescriptions | % |
|---|---|---|
| Poor | 239 | 17.07% |
| Average | 855 | 61.07% |
| Good | 306 | 21.85% |
The prescriptions were observed for key information needed to authenticate the prescription. These components were ‘name, address and telephone number of the treatment center, date of prescription and the signature of the prescriber’. All the screened prescriptions had information referring to the authentication of the prescription.
Further to the authentication of prescription, identification of the prescriber and his credentials were also sought in the form of his name, qualification, designation, registration number, OP timings and OP days. All the prescriptions in the study had the name of the prescriber (100%), however the qualification and the designation was seen in 377 (26.92%), registration number was seen in 12 (0.85 1%) prescriptions and OP timings and days were seen in 463 (33.07%) prescriptions.
In order to identify the patient, their name, age, gender and contact details were sought in the prescription. Name and age of the patient was found in all screened prescriptions (100%). Gender was mentioned in 98.92% (1385) prescriptions. Contact details of the patient were unavailable in all prescriptions.
The prescriptions were further screened for the clinical history recording by seeing the information like chief complaints, duration of the complaints, past history and investigation records available. 39.21% (549) prescriptions had chief complaints noted although the duration of such complaints was mentioned in 16.92% (237) prescriptions only. 14.6% (205) prescriptions had records of past history. Prescriptions having records of investigations available were limited to 4.3% (61) only (Table 5).
Table 5.
Clinical history.
| Clinical history | No of prescriptions | % |
|---|---|---|
| Chief complaints | 549 | 39.21 |
| Duration | 237 | 16.92 |
| Past history | 205 | 14.6 |
| Investigations available | 61 | 4.3 |
The prescriptions were further screened for the information related to clinical examination of the patient. Clinical findings from Ayurvedic perspective were sought for their incorporation in the prescription. 21% (294) prescriptions had descriptions related to the clinical examination of the patient. This is important to note that Ayurvedic components of clinical examination including prakriti, vikriti, rog bala, rogi bala, samprapti and saadhya asaadhyata were missing all together in all the prescription screened (Table 6).
Table 6.
Clinical examination findings.
| Clinical examination findings | No. of prescriptions | % |
|---|---|---|
| Physical and systemic examination | 294 | 21 |
| Prakriti | 0 | 0 |
| Vikrati | 0 | 0 |
| Nadi | 0 | 0 |
| Roga Bala | 0 | 0 |
| Rogi Bala | 0 | 0 |
| Samprapti | 0 | 0 |
| Sadhya-asaadhyata | 0 | 0 |
All the prescriptions were screened for a mention of Ayurvedic/Allopathic diagnosis upon them. 87% (1218) prescriptions had Ayurvedic diagnosis. 3.07% (43) prescriptions had Allopathic diagnosis. A small fraction of all prescriptions (8, 0.57%) had a dual diagnosis. 8.5% (131) prescriptions had no diagnosis.
About 89.5% (1253) prescriptions had a treatment plan in some or other way. 10.5% (147) prescriptions were found devoid of any such treatment plan.
All the prescriptions were examined for the mention of dose, frequency, anupana, time of use in relation to food, and total duration of therapy. 71% (994) prescriptions had a mention of drug dosage. 72% (1008) had the mention of frequency of drug use. Anupana (post medicine drink) was available in 8.5% (119) prescriptions. Only 1.01% [15] prescriptions had a mention of drug intake in relation to food. Total duration of therapy was mentioned in 16% (224) prescriptions (Table 7).
Table 7.
Medication.
| Medication | No. | % |
|---|---|---|
| Dose | 994 | 71 |
| Frequency | 1008 | 72 |
| Anupana | 119 | 8.5 |
| Time of use in relation to food | 15 | 1.01 |
| Total duration for therapy | 224 | 16 |
Apart from the medication and its dosage, Ayurvedic prescriptions also consist of ahara (dietary) and vihara (life style) recommendation including exercises. All the prescriptions were screened for such information. About 4.35% (61) prescriptions had a mention of recommended and avoidable diet. Only 1.07% [15] prescriptions had a mention of life style modification or exercise.
All the prescriptions were screened for follow up instructions also. Only 8.5% (133) had a mention of investigations to be brought in follow-up. Follow-up visit instruction was mentioned in 1.5% [21] prescriptions (Table 8, Fig. 3).
Table 8.
Summary of the observations made in the study as per the PQIA.
| Relative weightage | Parameters | Individual components | Score | Observed % of prescriptions |
|---|---|---|---|---|
| 5% | Authentication of the prescription |
|
1 | 100 |
|
2 | 100 | ||
|
2 | 100 | ||
| 10% | Legibility of the prescription |
|
0 | 17.07 |
|
5 | 61.07 | ||
|
10 | 21.85 | ||
| 5% | Physician's identity |
|
1 | 100 |
|
2 | 26.92 | ||
|
1 | 0.85 | ||
|
1 | 33.07 | ||
| 5% | Patient's identity |
|
1 | 100 |
|
2 | 100 | ||
|
1 | 98.92 | ||
|
1 | 0 | ||
| 15% | Clinical history |
|
5 | 39.21 |
|
5 | 16.92 | ||
|
3 | 14.6 | ||
|
2 | 4.3 | ||
| 20% | Clinical examination findings |
|
6 | 21 |
|
2 | 0 | ||
|
2 | 0 | ||
|
2 | 0 | ||
|
2 | 0 | ||
|
2 | 0 | ||
|
2 | 0 | ||
|
2 | 0 | ||
| 5% | Diagnosis |
|
3 | 87 |
|
2 | 3.7 | ||
|
0.57 | |||
|
9.35 | |||
| 5% | Plan of treatment |
|
5 | 89.5 |
| 20% | Medication |
|
4 | 71 |
|
4 | 72 | ||
|
4 | 8.5 | ||
|
4 | 1.01 | ||
|
4 | 16 | ||
| 5% | Other instructions |
|
3 | 4.35 |
|
2 | 1.07 | ||
| 5% | Follow up instructions |
|
2 | 8.5 |
|
3 | 1.5 |
Fig. 3.
Summary of performance of PQIA for items between the floor and ceiling value.
4. Discussion
Seeing the importance of a medical prescription, this is beyond doubt that it should be prepared with utmost care. A prescription should consider every possible role it may play in the precise management of the disease and also multiple ancillary roles where it may come as an evident medical record for reference.
Reports of negligence in prescription writing are neither new nor few [16]. These are besides the reports of medical negligence where the doctors are charged for not taking the right decision on part of patient management [17]. There are also reports of thousands of people dying every year because of poor communication of disease management decisions to the healthcare team. This eventually happens with the poorly written or incomplete prescriptions allowing room for lapses and medication errors. Many hospital admissions every year are convicted to the prescription errors alone. A poorly drafted prescription defeats its own goal of offering a cure to the patient as its therapeutic plan may not be executed religiously for want of clarity [18].
PQI has been approached in Allopathy as a mean of identifying the lapses in common prescriptions. Such indexes address different styles and set of practices as per the disease or clinical specialty.
Such approaches of looking at the quality of prescription are however altogether lacking in practice of complementary and alternative medicine (CAM). Ayurveda, a commonly practiced system of medicine in India, South East Asia and a partly practiced system in many other parts of the world, utilizes its own understanding of disease and health to offer a cure through multiple modalities namely herbs, metals, minerals and animal products. Diet and daily routine adjustments also form a crucial component of net Ayurvedic management approach. Besides the routine drug prescribing, Ayurveda sometimes radically approaches towards the disease by offering elimination of disease causing toxins, pathogens or factors. Panchakarma or the biocleansing is an Ayurvedic approach offering a radical cure to a disease [19].
Besides treatments, the diagnostic approach of Ayurveda is also quite unique. It focuses upon severity of the disease and strength of the sick. A treatment is therefore planned under the influence of these two dynamic duos. There are many other things important from the perspectives of a disease diagnosis and treatment selection in Ayurveda [20]. A clinical examination from Ayurvedic view point hence seems important in treatment selection.
Contemporary Ayurvedic practice is largely criticized for not following its own dictums of science and logics to unearth the mysteries of health and disease and rather trying to fit modern science to their own logics in every case [21]. Ayurvedic practitioners not following their own principles of disease management is a common scenario in India. Ayurvedic prescriptions are the window through which a glimpse of contemporary Ayurvedic practice in India may be seen.
Utilizing the concept of PQI in order to identify the gaps in Ayurvedic practice was therefore attempted as a mean to make things better by knowing what is being missed. A comprehensive PQI for Ayurveda used in the study was the outcome of a long process of peer discussions, brainstorming, drafting and revisions. The final draft comprised of 11 identifiable groups of differential weightage expandable into 38 independent items to be reported from every prescription. The information sought in the PQIA was available from multiple sources, viz., pre-printed prescription, registration desk and prescriber. The findings of the study suggest that maximum deficits found in the prescription were confined to prescriber part. This observation becomes even more valuable when we see that the prescriptions in the pilot study have mostly been generated by the highly qualified clinical specialists of Ayurveda. ‘Not following the Ayurvedic principles of disease diagnosis and its management’ this under current criticism of Ayurvedic contemporary practice finds a ground reality in the study when we see that not a single prescription used in the study had a mention of any finding related to Ayurvedic understanding of pathogenesis and disease management.
In the first instance, one may feel consoled by seeing that majority prescriptions contained a diagnosis and so the error of omission of writing about Ayurvedic clinical findings may seem diluted by seeing a finding one step ahead. Unfortunately a serious enquiry about the diagnosis revealed that the diagnosis in prescription under the study was customarily being written by the resident doctors in order to complete the records and was almost never written by the prescriber on the day of prescription generation. The finding of diagnosis in the study is therefore dubious and may not be considered seriously.
The descriptions about medications were also inadequately reported in the prescriptions. There was a negligible mention of the post-medication drink and relation of drug intake with meal timings. This is important to note that these two are considered substantially important in determining the role of same medication for a variety of conditions as per the dosha specifications.
The findings observed in the study are alarming in their nature and are reflective of contemporary Ayurvedic practice in India. Although conducted as a pilot study at one center, the study is able to give us a glimpse of the magnitude of the problem if a multicentre study of such kind is conducted.
The question which may be asked here is why were indoor prescriptions considered in this pilot study. Indoor prescriptions by default are different from outdoor prescriptions because in the former, the prescriber has an opportunity to correct the mistakes in ongoing visits while the patient is still available as in patient. In the latter however, once the prescription is generated, it is only the next follow-up when the physician may be able to see it again. It is therefore obvious to see that the perfection of a prescription is more urgently required in outpatient departments rather than in patient departments.
Moreover, the indoor prescriptions are usually generated provisionally as a more concrete treatment plan may take its time to arrive in wake of further investigations recommended to reach at a final diagnosis in a given case.
Here this is important to underline again the difference between Ayurvedic and modern approach of disease diagnosis and management. In Ayurvedic method of disease identification and treatment planning, it is usually done in a single stretch by the concerned physician and investigations usually play a small role in changing the therapeutic plan. Moreover whatever treatment is recommended at the time of admission may be continued in Ayurvedic approach for some time unless a phasic approach of treatment is adopted. This is why, from Ayurvedic perspective, indoor prescriptions should not differ much comparing to the outpatient prescriptions.
Indoor prescriptions were preferred in the study for ease of the data collection and possibility of cross checking of the data.
Conduction of the pilot test at one center only may be considered as another limitation of the study. As there are large differences in region based Ayurvedic clinical practice, a large study conducted at different geographical locations in the country may give rise more reveling findings.
5. Conclusion
Prescription quality is a prelude to the effective delivery of healthcare. In this sense, quality of the prescription can be considered as a direct predictor of the net outcome in a given case. Judging the prescription quality on the basis of a validated PQI therefore can be a pragmatic proposition to predict the outcome in a medical system or specialty. This can also act as a tool to underline the difference in the outcome in a similar condition approached by two different styles of practices pertaining to different geographical area. As Ayurveda has its own understanding of diseases and its management, a PQI for Ayurveda essentially requires the components addressing the Ayurvedic fundamentals. A thoroughly reviewed and validated PQIA was developed in this study as an outcome of a peer discussion process and was subjected to the pilot study on indoor prescriptions from a renowned Ayurvedic hospital. The findings were revealing in many ways and were able to demonstrate the minimal utilization of Ayurvedic concepts of disease diagnosis and management in contemporary Ayurvedic practice. The study warrants further studies for two reasons: one to revalidate the PQIA in different Ayurvedic practice settings and second to identify the deficits in contemporary Ayurvedic practice in different geographical area of the country. The study proposes PQIA as a direct predictor to the possible outcome in a given medical condition and hence may be considered seriously for its use in cost, time and outcome analysis studies in future [22].
Sources of funding
None.
Conflict of interest
None.
Footnotes
Peer review under responsibility of Transdisciplinary University, Bangalore.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jaim.2017.02.008.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Guide to Good prescribing, A practical manual, WHO Geneva. Available at: http://apps.who.int/medicinedocs/pdf/whozip23e/whozip23e.pdf (Accessed 5 March 2016).
- 2.Ni K., Siang C., Ramli M. Non compliance with prescription writing requirements and prescribing errors in an outpatient department. Malays J Pharma. 2002;1:45–50. [Google Scholar]
- 3.Cheung Ka-Chun, Bouvy Marcel L., De Smet Peter A.G. M. Medication errors: the importance of safe dispensing. Br J Clin Pharmacol. 2009 Jun;67(6):676–680. doi: 10.1111/j.1365-2125.2009.03428.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schnoor J., Rogalski C., Frontini R., Engelmann N., Heyde C. Case report of a medication error by look-alike packaging: a classic surrogate marker of an unsafe system. Patient Saf Surg. 2015;9:12. doi: 10.1186/s13037-014-0047-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lechevallier-Michel N., Gautier-Bertrand M., Alperovitch A., Berr C., Belmin J., Legrain S., On behalf of 3C Study Group Frequency and risk factors of potentially inappropriate medication use in a community dwelling elderly population: results from a 3 C study. Eur J Clin Pharmcol. 2005;60:813–819. doi: 10.1007/s00228-004-0851-z. [DOI] [PubMed] [Google Scholar]
- 6.Avery T., Barbar N., Ghaleb M., Franklin B.D., Armstrong S., Crowe S. 2012. Investigating the prevalence and causes of prescribing errors in general practice, a report for GMC. [Google Scholar]
- 7.Velo Giampaolo P., Minuz Pietro. Medication errors: prescribing faults and prescription errors. Br J Clin Pharmacol. 2009 Jun;67(6):624–628. doi: 10.1111/j.1365-2125.2009.03425.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hassan N.B., Ismail H.C., Naing L., Conroy R.M., Abdul Rahman A.R. Development and validation of a new prescription quality index. Br J Clin Pharmacol. 2010 Oct;70(4):500–513. doi: 10.1111/j.1365-2125.2009.03597.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rastogi S. Poor quality and improper use: a review of common reasons of possible adversity in Ayurvedic practice. Int J Risk Saf Med. 2009;21(3):121–130. [Google Scholar]
- 10.Mallick S. Challenges of mainstreaming: ayurvedic practice in Delhi Government health institutions. J Ayurveda Integr Med. 2016 Mar;7(1):57–61. doi: 10.1016/j.jaim.2015.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gawde Suchita R., Shetty Yashashri C., Pawar Dattatray B. Knowledge, attitude, and practices toward ayurvedic medicine use among allopathic resident doctors: a cross-sectional study at a tertiary care hospital in India. Perspect Clin Res. 2013 Jul–Sep;4(3):175–180. doi: 10.4103/2229-3485.115380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Singh R.H. Exploring issues in contemporary Ayurvedic education. AYU. 2015;36:361–363. doi: 10.4103/0974-8520.190692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Colais P., Martino M.D., Fusco D., Davoli M., Aylin P., Perucci C.A. Using clinical variables and drug prescription data to control for confounding in outcome comparisons between hospitals. BMC Health Serv Res. 2014;14:495. doi: 10.1186/s12913-014-0495-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Donebedian A., Wheeler J.R., Wyszewianski L. Quality, cost and health: an integrative model. Med Care. 1982;20:975–992. doi: 10.1097/00005650-198210000-00001. [DOI] [PubMed] [Google Scholar]
- 15.Wang Lijuan, Zhang Zhiyong. Investigating ceiling effects in longitudinal data analysis. Multivar Behav Res. 2009 Jul 1;43(3):476–496. doi: 10.1080/00273170802285941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Exploring the costs of unsafe care in the NHS: a report prepared for the Department of Health. Frontier Economics; London: Oct 2014. [Google Scholar]
- 17.Medication errors cost the NHS up to £2.5bn a year, Pharm J 1 November 2014; 293: 7834, online| DOI: 10.1211/PJ.2014.20066893.
- 18.Legal obligation to write clearly. JR College Gen Pract; 1989. pp. 347–348. [Google Scholar]
- 19.Samhita Kashyap, Sharma Hem Raj. 2004. Chaukhambha Sanskrit Sansthan, Varanasi. [Google Scholar]
- 20.Samhita Saharangdhara, Tripathi B.N. 1990. Chaukhambha Surbharati Prakashan, Varanasi. [Google Scholar]
- 21.Mallick S. Autumn 2013. From heritage to practice: Ayurveda in Delhi's public healthcare system. The Focus | 27 The Newsletter, No. 65. [Google Scholar]
- 22.Hamdy H., Prasad K., Anderson M.B., Scherpbier A., Williams R., Zwierstra R. BEME systematic review: predictive values of measurements obtained in medical schools and future performance in medical practice. Med Teach. 2006;28(2):103–116. doi: 10.1080/01421590600622723. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.