Abstract
Background
Taping is commonly prescribed to treat plantar fasciitis for runners by virtue of its alleged ability to offload the plantar fascia and facilitate positive injury prognosis. Our study aimed to investigate how different taping methods could change the loading on the plantar fascia during running using computational simulations.
Methods
A finite element foot model was modified from a previous version to fit the study's purpose. The model featured twenty bones, bulk soft tissue, foot muscles, ligaments/tendons, and a solid part representing the plantar fascia. A runner performed several running trials under one untaped condition and two taped conditions—Low-Dye taping and Fascia taping, which were implemented by a physiotherapist using the Kinesio tapes. The captured motion data were processed to drive a scaled musculoskeletal model and calculate segmental kinematics, foot muscle force, and joint reaction force. These variables were then input as the boundary/loading conditions for finite element analyses of running. The principal tensile strain on the plantar fascia, subtalar eversion, and navicular height during the stance phase were averaged across five trials of each condition and compared using Friedman's test.
Results
Maximal subtalar eversion did not differ among conditions (p = 0.449). Fascia taping significantly reduced maximal strains on the fascia band (p = 0.034, Kendall's W = 0.64–0.76) and increased the navicular height (p = 0.013, Kendall's W = 0.84) compared with nontaping. There were no significant differences in all outcome variables between Low-Dye taping and nontaping (p = 0.173–0.618).
Conclusion
From a mechanical point of view, our study provided quantitative evidence to support the application of taping treatments for overstrained plantar fascia. The untensed fascia band by Fascia taping could be a potential indicator of pain relief for the runners. However, a prospective study targeting the patient population would be needed to address the point.
The Translational Potential of this Article
The study quantified the loading status of the plantar fascia during running and provided mechanical evidence to support the usage of taping as a mean to reduce fascial strain, thus possibly controlling injury risks for the runners. The results of the study also highlighted the importance of selecting specific taping methods based on individuals' needs.
Keywords: Athletic tape, Biomechanics, Finite element analysis, Plantar fascia, Running
Introduction
Plantar fasciitis is one of the most common foot complaints accounting for a quarter of foot injuries [1]. Annually, around two million Americans suffer from plantar fasciitis [2], and runners are particularly vulnerable to the foot problem [3]. Patients with plantar fasciitis usually present pinpointed pain at the calcaneal tubercle during the first few steps in the morning. Runners could abstain from training owing to the continuous aggravation of symptoms. The projected yearly costs of plantar fascia treatment could range from 192 to 376 million dollars in the United States, which are huge economic burdens for both the society and individuals [4]. Although its pathologies are not fully understood, plantar fasciitis is primarily thought to result from repeated overstrain on the plantar fascia [5].
Taping is commonly used to treat plantar fasciitis, particularly for palliative management of heel pain at an early pathological stage [6]. Tapes attached to the foot were opined to correct faulty biomechanics and take the strain off the plantar fascia [7], hereby to improve the symptoms of plantar fasciitis. Currently, a variety of taping methods have been introduced. Regardless of the differences in terminology, two major categories, Low-Dye taping and Fascia taping, are the most frequently applied taping modalities based on their functions.
The Low-Dye taping, which is also referred to the antipronation taping, was first introduced by Dr. Dye to treat plantar fasciitis [8]. Low-Dye taping is characterized by tapes wrapping the heel to fix the rotatory axis of the subtalar joint, subsequently control foot arch flattening through coupling of the foot segments [9], and relax the plantar fascia. On the other hand, Fascia taping attaches tapes directly to the plantar foot surface that connect the forefoot to the heel [10]. It is designed to stabilise the plantar ligaments and limit abnormal movements of the plantar fascia by exploiting the arch-raising effects of the foot windlass mechanism [11].
Both taping methods have received much research attention with regard to their treatment effects on plantar fasciitis [12], [13]. Although their clinical applications are prevalent, the reported outcomes were oftentimes conflicting. One explanation for the inconsistency is a lack of a unified taping standard. In the clinic, selection of taping methods is largely anecdotal [14]. Variances in taping modality increase the heterogeneity and hinder conclusive statements on the pooled data. Besides, direct comparisons among taping methods are few. It is still unclear how various taping modalities could change the foot biomechanics differently. In fact, current evaluations of the taping treatment effects are concentrated on general gait parameters, patients' feedback on pain relief, and function recovery [13]. These variables do not necessarily reflect the changes in loading on the plantar fascia. Plantar fascia is mainly loaded by tensile strains for body weight acceptance and impact absorption during the running gait [15]. Excessive strains on the fascia band repeating over gait cycles can be associated with tissue microtears, local inflammations, and collagen degeneration [16]. Collectively, these changes contribute to pathology of plantar fasciitis. As a matter of fact, reducing fascial strain could facilitate tissue repair and diminish injuries for the runners [8], which should lay the primary mechanical foundation for taping treatment and justify its functionality. Nevertheless, neither noninvasive assessments of loading on deep foot tissues nor real-time measurements of the fascial strains during running are easily feasible. Previously, ultrasound imaging from beneath the foot could detect the fascial material property and reflect its loading status. However, this measurement method is largely static and remains qualitative [17].
Because the treatment effects of taping mostly reside in its capacity of offloading the plantar fascia, more quantitative evidence is needed to substantiate this statement and support its application in the clinic from a mechanical standpoint. The recently advancing computer technology and finite element method have enabled comprehensive modelling of the human foot [18], [19], with which its internal biomechanics, such as loading on the plantar fascia, can be calculated through computational simulation of segmental deformation during a running manoeuver [19]. The simulation results could be a complement to a research field where in vivo measurements of fascial strain were difficult.
In the study, we aimed to investigate and compare loading on the plantar fascia during running between the taped conditions (Low-Dye taping and Fascia taping) and untaped condition (control) by means of a computational foot model. Besides, the ability of taping to constrain subtalar motion and support the foot arch was also evaluated. The significance of the study was to quantify the strain level of the plantar fascia in the running gait. The primary outcomes were the principal tensile strain on the plantar fascia, subtalar eversion, and navicular height during the stance phase. Our hypotheses were that (1) the plantar fascia would be less strained and the navicular height would be increased by both Low-Dye taping and Fascia taping compared with nontaping and (2) the subtalar eversion would be reduced by Low-Dye taping compared with Fascia taping and nontaping.
Methods
Participant information
A recreational runner (male, aged 30 years, 170-cm tall, and 68 kg in mass) was recruited for the computer model reconstruction and gait experiments. The participant was an experienced recreational runner (running experiences: 12 years, average weekly mileage: 15 km, and usual pacing: 6 min/km) using a rearfoot strike technique and had never changed his foot strike pattern before the experiments. His foot arch is neutral with a measured arch index of 0.25 [20]. He reported no musculoskeletal diseases/injuries (e.g., rearfoot overpronation and heel pain) or medical history that could influence his running performance at recruitment. He was fully informed of the research procedure and signed the consent form. The experimental protocol was approved by the institution authority (No. HSEARS20170626003).
Experimental procedure
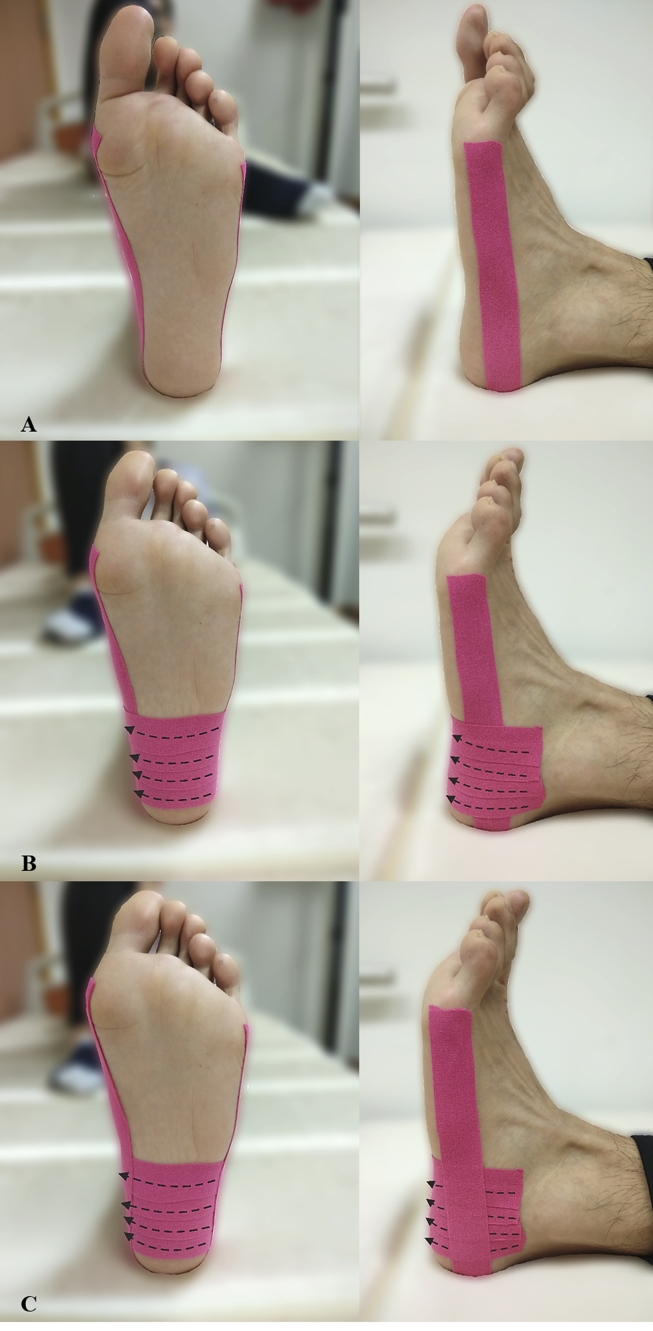
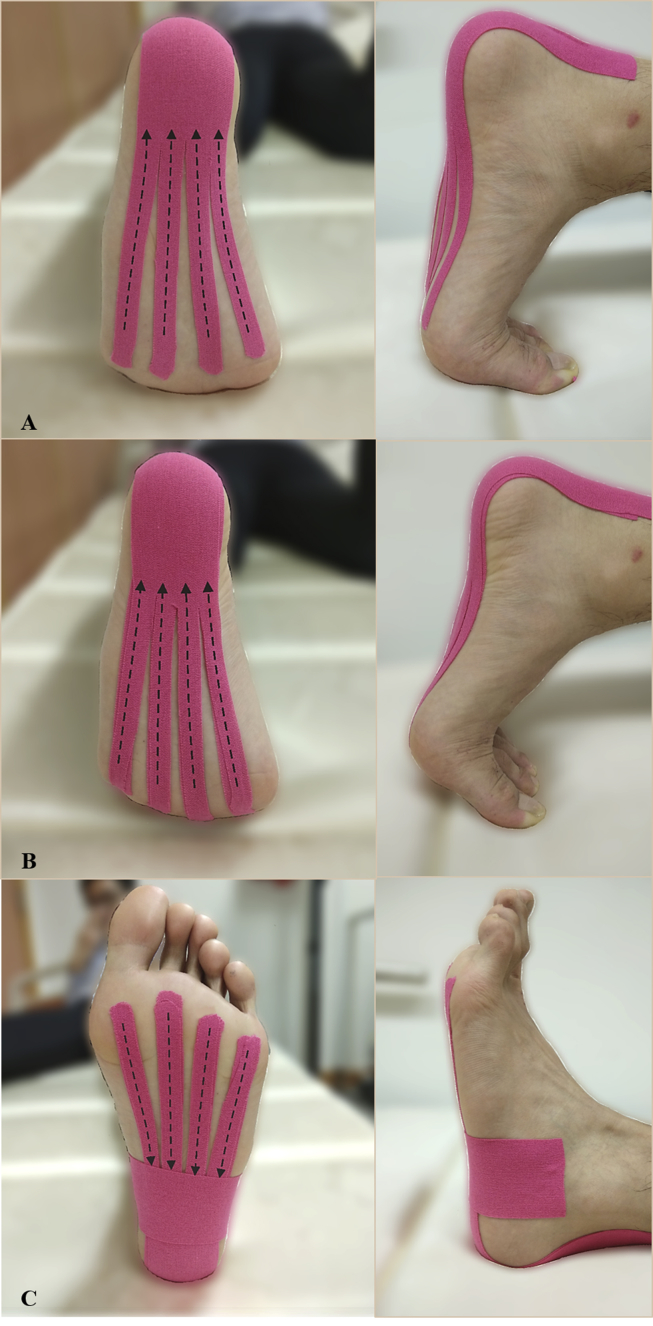
The experiment comprised several running trials under one untaped condition and two taped conditions (Low-Dye taping and Fascia taping). A physiotherapist (T.L.-W.C.) implemented taping to the runner using the Kinesio tapes (Kinesio Tex Classic; Kinesio, Albuquerque, NM, USA). The methods for Low-Dye taping and Fascia taping are illustrated in Figure 1, Figure 2, respectively [8], [10].
Figure 1.
(A) The first step of Low-Dye taping; (B) The second step of Low-Dye taping; (C) The third step of Low-Dye taping. In the first step, the first strap, which served as the anchor tape, was applied with gentle compression. It started at the medial first metatarsal head, stretched proximally along the medial border of the foot, went around the back of the heel, and attached to the lateral fifth metatarsal head. In the second step, a series of stirrups were applied when the rearfoot was slightly supinated. The first stirrup started distal to the lateral malleolus, pulled the calcaneus medially with a 50% stretch (50% tensile strain), and attached to just below the medial malleolus. The second, third, and fourth stirrup followed the same pattern with an overlap of approximately one-third of the tape width, moving in the distal direction. In the third step, the last strap was applied in the similar form of the first strap to secure the whole taping structure. Dash arrows denote the direction of stretch.
Figure 2.
(A) The first step of Fascia taping; (B) The second step of Fascia taping; (C) The third step of Fascia taping. In the first step, after the metatarsophalangeal joints were dorsiflexed, the first strap was adhered firmly to the posterior heel at its proximal end. The other end of the strap was cut into four slices of equal width. Each slice was applied with a 50% stretch (50% tensile strain) and attached to the plantar forefoot. In the second step, another strap was applied following the same pattern and overlapped the first strap. In the third step, the last strap was applied with gentle compression across the bases of the four slices beneath the foot and wrapped around the rearfoot. Dashed arrows denote the direction of stretch.
Before the experiment, the participant was given ample time to warm up. The three running conditions (untaped/taped) were tested in a randomised sequence with a 5-min rest interval. The participant ran barefoot to eliminate the influence of footwear. For each condition, the participant was instructed to run through the motion capture volume at his usual pacing (10 km/h). Two pairs of photoelectric cells were placed 2.6 m apart along the runway to monitor the running speed. Running trials were repeated until five sets of successive data were obtained for each condition. Data were considered successive when the running speed fell with 5% variance of the target value (10 km/h) and the footstep landed completely within the force platforms.
A motion capture system with eight optical-based cameras (Vicon; Oxford Metrics Ltd., Oxford, UK) and four force platforms (OR6; AMTI, Watertown, NY, USA) was used to record marker trajectories and ground reaction force. The data were sampled at 250 Hz and 1000 Hz. Thirty-six retroreflective markers were affixed to the following anatomic landmarks for motion capture: acromioclavicular joints, posterior/anterior iliac spines, greater trochanters, lateral/medial femoral epicondyles, lateral/medial malleoli, calcaneal tuberosity, the base/head of the first and fifth metatarsals, and the distal phalanx of the hallux.
Musculoskeletal model
The kinematic and kinetic data collected from the running trials (five trials for each condition) were input into the musculoskeletal modelling platform (OpenSim, version 3.3; National Centre for Simulation in Rehabilitation Research, Stanford, CA, USA). A generic model [21] with 12 rigid body segments, 23 degrees of freedom, and 92 musculotendinous units was scaled to accommodate the mass and anthropometry of the participant. Inverse kinematics was then solved, and the dynamic inconsistency was reduced by small adjustments to model mass properties. Forces of the extrinsic foot muscles were estimated by the built-in computed muscle control modulus. Joint reaction force and segmental kinematics were generated by the built-in analyse toolkit (OpenSim, National Center for Simulation in Rehabilitation Research, Stanford, CA, USA). The aforementioned variables were exported as the boundary and loading conditions for the subsequent finite element analyses.
Finite element model
Geometry reconstruction
The geometry of the left foot model was reconstructed from the Magnetic Resonance Images of the participant, which was also reported in our previous study [18]. In brief, it was acquired by using a 3.0T MRI scanner (GoldSeal Certified Signa HDxt; General Electric Company, Boston, MA, USA) at T1 sequence, 1-mm slice interval, and 0.625-mm pixel size when the participant's leg was fixed at the neutral position by using a customised ankle-foot orthosis. The image was processed, and the model was reconstructed using segmentation software (Mimics and 3-matics version 19.0; Materialise, Leuven, Belgium).
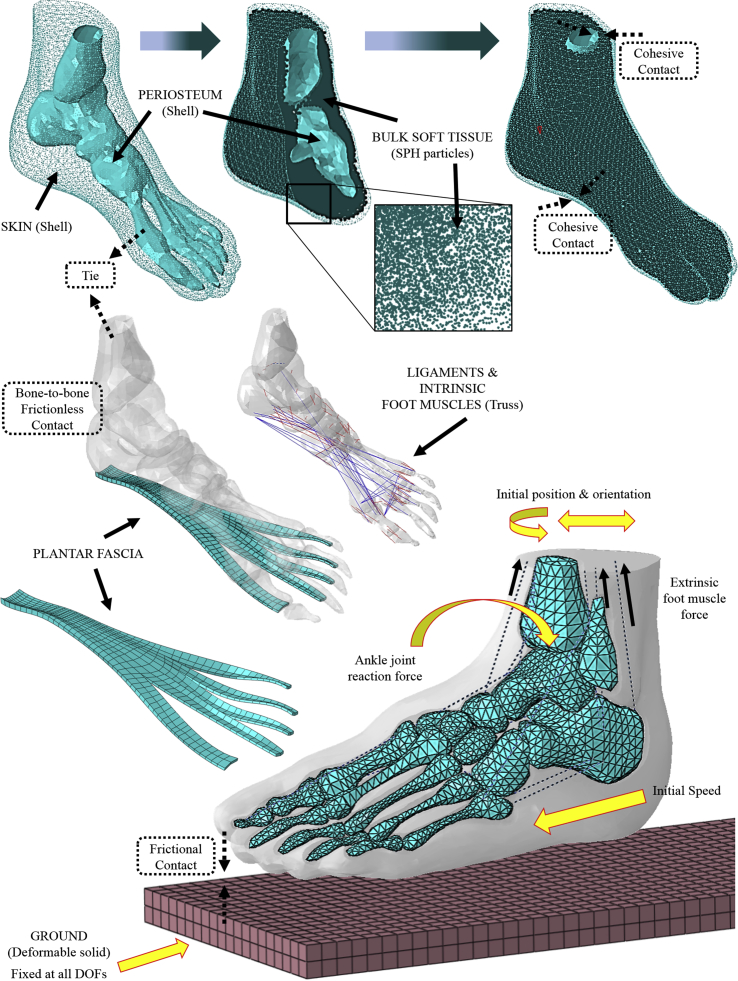
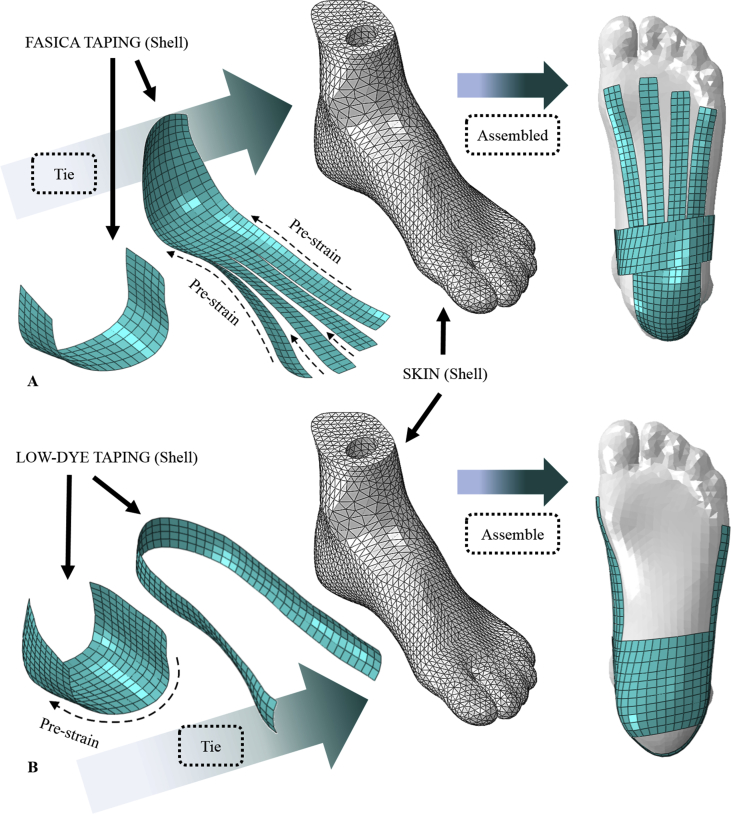
The model included 20 bony segments, 26 ligaments, 9 intrinsic foot muscles, and 11 extrinsic foot muscles, as shown in Figure 3 [18]. The bulk soft tissue was modelled by a cluster of smoothed-particle hydrodynamics particles encapsulated in a shell unit using the cohesive property. The shell unit consisted of interior and exterior surfaces, representing the periosteum layer (tied to the bony structures) and skin layer (in contact with the ground), respectively (Figure 3). In addition, the geometry of the plantar fascia was reconstructed as a three-dimensional solid based on the bony structures from the MRI scans and the human anatomy atlas [22] using computer-aided design software (SolidWorks version 2014; Dassault Systèmes, Waltham, MA, USA). From the origin to the distal end, the thickness of the fascia bands gradually reduced from 3 mm to 1.3 mm. The plantar fascia was tied to the inferior calcaneus proximally and to the five phalanges distally. The Kinesio tapes were modelled as shell units with 0.5-mm thickness, based on the product catalogue. Different strap designs were reproduced and tied to the skin surface in the model to mimic the two taped conditions (Figure 4). Prestrain (+50% elongation) was applied on the tape straps, as shown in Figure 4.
Figure 3.
Setup overview of the finite element foot model and boundary conditions. Solid black arrows denote the names of the parts. Solid maize arrows represent boundary/loading conditions. Dashed frames denote the interactions among parts. The bulk soft tissue was modelled as SPH particle elements and encapsulated in a shell unit that possessed an interior profundal fascia layer and exterior skin layer. The internal layer of the shell was tied to the skeletal structures. The plantar foot was connected by ligaments (truss unit), intrinsic foot muscles (truss unit), and the plantar fascia (three-dimensional solid). The ground plate was fully fixed, and the foot model was placed at an initial position/orientation. Three-dimensional ankle joint reaction force, extrinsic foot muscle force, and initial transitional velocity were applied to the model to drive the simulation. DOFs = degrees of freedom; SPH = smoothed-particle hydrodynamics.
Figure 4.
(A) Modelling of Fascia taping in the simulations; (B) modelling of Low-Dye taping in the simulations. Dashed arrows denote the direction assigned with a prestrain of 50% to mimic stretch on the tapes. Solid black arrows denote the names of the parts. Shell units that represented the tape straps were tied to the skin surface.
Material properties and mesh creation
The material properties of different components were adopted from the existing literature (Table 1). The bone, periosteum, and bulk soft tissue were assumed linearly elastic and isotropic [18], whereas the plantar fascia [23] and Kinesio tapes [24] were assumed hyperelastic and isotropic. The mesh of the model was created using finite element software (Abaqus version 6.14; Simulia, Dassault Systèmes, Johnston, RI, USA). The overall mesh size was determined as 3.5 mm for the osseous and soft tissue components as supported by our previous study [18]. Another mesh convergence test was conducted targeting on the mesh size of the plantar fascia by simulating the midstance phase of a representative barefoot running trial conducted in the present study. The mesh size was reduced every 10% from 5.5 mm. The predicted strain deviation of the plantar fascia was less than 5% when the mesh size was reduced to 4.0 mm. The element type and mesh count of each component are detailed in Table 1.
Table 1.
Element type, material property, and mesh count for the model components.
| Element type | Material property | Density | Poisson's ratio | Mesh count | |
|---|---|---|---|---|---|
| Skin | Linear triangular shell (S3R) | Hyperelastic (first-order Ogden model, μ = 0.122 MPa, α = 18) Thickness: 2.0 mm |
950 kg/m3 | N/A | 4807 |
| Bulk soft tissue | SPH particle (PC3D) | Linearly elastic (Young's modulus: 0.83 MPa for the plantar heel, 0.70 MPa for the plantar forefoot/toe, 0.67 MPa for the plantar midfoot, and 0.20 MPa for the rest) | 950 kg/m3 | 0.4 | 45008 |
| Periosteum | Linear triangular shell (S3R) | Linearly elastic (Young's modulus: 0.9 MPa) Thickness: 1.5 mm |
1000 kg/m3 | 0.4 | 11576 |
| Bone | Linear tetrahedral solid (C3D4) | Linearly elastic (Young's modulus: 17000 MPa) | 1990 kg/m3 | 0.3 | 18965 |
| Extrinsic foot muscles | Slip ring connector | Linearly elastic (stiffness: 157.4 N/mm) | 1000 kg/m3 | N/A | N/A |
| Intrinsic foot muscles | Two-node truss (T3D2) | Linearly elastic (Young's modulus: 264.8 MPa) Cross-sectional area: 10 mm2 |
1000 kg/m3 | 0.4 | 24 |
| Rearfoot ligaments | Two-node truss (T3D2) | Linearly elastic (Young's modulus: 100–320 MPa) Cross-sectional area: 7.1–256 mm2 |
1000 kg/m3 | 0.4 | 20 |
| Other ligaments | Two-node truss (T3D2) | Linearly elastic (Young's modulus: 264.8 MPa) Cross-sectional area: 10 mm2 |
1000 kg/m3 | 0.4 | 67 |
| Ground plate | Linear tetrahedral solid (C3D4) | Linearly elastic (Young's modulus: 17000 MPa) | 1000 kg/m3 | 0.3 | 12800 |
| Plantar fascia | Linear hexahedron solid (C3D8R) | Hyperelastic (second-order polynomial model, C10: −222.1, C01: 290.97, C20: −1.1257, C11: 4.7267, C02: 79.602) |
1000 kg/m3 | 0.4 | 438 |
| Kinesio tape | Linear quadrilateral shell (S4R) | Hyperelastic (first-order Ogden model, μ = 0.206 MPa, α = 8.88) Thickness: 0.5 mm |
1150 kg/m3 | 0.4 | 464–492 |
SPH = smoothed-particle hydrodynamics.
Parameters and equations for material property were based on the same references in our previous work [18].
A frictionless contact algorithm was used for the bone-to-bone interface to mimic the function of cartilages [19]. The interaction between the skin and the ground plate was “hard” contact with a friction coefficient of 0.6 [25].
Boundary and loading conditions
The finite element foot model was assigned with the boundary and loading conditions generated by the musculoskeletal model. Concentric connector force was applied to the slip ring connectors to simulate extrinsic foot muscle force. Three-dimensional ankle joint reaction force was loaded on the ankle surface of the talus (Figure 3). All force data were input into a tabulated time series matrix to drive the finite element analysis. The whole-foot model was initially placed at the position and orientation corresponding to the instant before foot strike. A predefined velocity was also conferred to the whole-foot model (data of boundary and loading conditions can be accessed in the linked data repository). Gravity was enabled throughout the simulation steps using the force/mass ratio of 9.8.
Simulation solver and data output
For each running condition, simulations of five trials were performed using Abaqus dynamic explicit solver (version 6.14; Simulia, Dassault Systèmes, Johnston, RI, USA). The principal tensile strain on the plantar fascia, subtalar eversion, and navicular height were reported and compared among the conditions. After excluding the regions that were tied to the bones, the plantar fascia was equally divided into three portions from proximal to distal. Principal tensile strain was averaged across all elements of each portion, and the mean values were used for the statistical analysis. Strain contours of the plantar fascia of representative running trials were also plotted. Subtalar eversion was calculated as the angle between the longitudinal axes of the tibia and the calcaneus on the frontal plane. Longitudinal axes of the foot segments were defined by prelabeled anatomical landmarks on the foot model based on an established method [26]. Navicular height was measured as the distance between navicular tuberosity and the plantar foot surface [1].
Model validation
Model validation was conducted by replicating the loading conditions of a cadaveric study [27]. In brief, the established foot model was fixed at proximal tibia and constantly loaded by 98.1 N on the plantar forefoot, which imitated plantar fascia–stretching exercise. Strains along the fascia band approximal to its attachment to the calcaneus were reported. The agreement between our simulations and the cadaveric study was examined by comparing the predicted and measured stain values using linear regression. The regression parameters (slope, intercept, and R2) were calculated to demonstrate the accuracy of the finite element model.
Statistical analysis
Statistics were conducted in SPSS (version 19.0; IBM, Armonk, NY, USA) at a significance level of 0.05. Maximal strains of the proximal, middle, and distal plantar fascia, maximal subtalar eversion, and minimal navicular height during the running stance were compared among the three conditions. Nonparametric Friedman's test for related samples was used to examine the differences. Dunn's pairwise comparison test with the Bonferroni correction was carried out for post hoc analysis. The effect size (Kendall's W) was calculated to demonstrate the strength of the results. The coefficients were interpreted as trivial effect (<0.2), small effect (<0.5), medium effect (<0.8), and large effect (≥0.8) [28].
Results
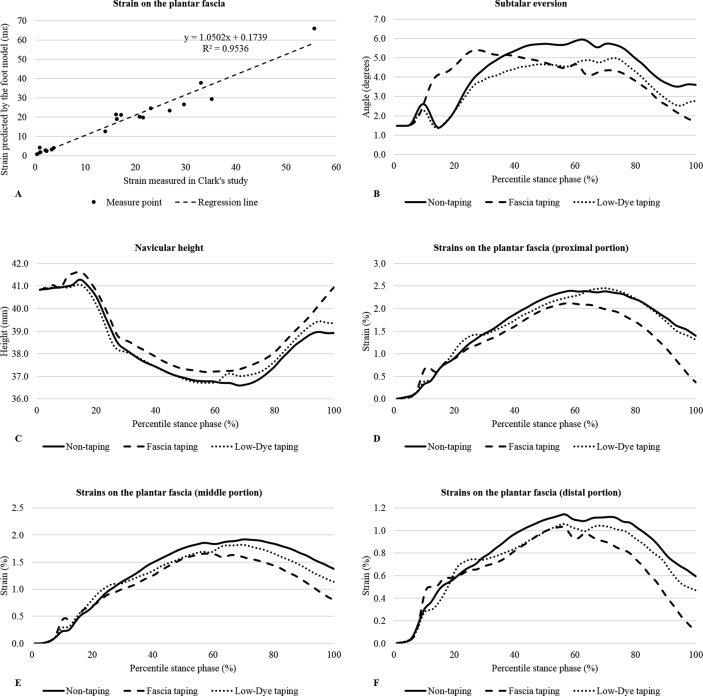
Figure 5 (A) shows the validation results (regression analysis) of the predicted and measured fascial strains under the loading condition of plantar fascia–stretching exercise. The Pearson correlation coefficient was 0.95 with a slope of 1.05 and an intercept of 0.17, which indicated a good agreement between our simulation and Clark's experiment [27].
Figure 5.
(A) Results of model validation; (B) predicted subtalar eversion; (C) predicted navicular height; (D) predicted strains on the proximal plantar fascia; (E) predicted strains on the middle plantar fascia; (F) predicted strains on the distal plantar fascia. Each dot in the validation plot denotes the simulated and measured strain value of one measurement point as depicted in Clark's study. Parameters of the trend line (R2: 0.95, slope: 1.05, intercept: 0.17) indicated a good agreement between the model estimates and experimental outcomes; all outcome variables in the predictions are scaled to the percentile stance phase.
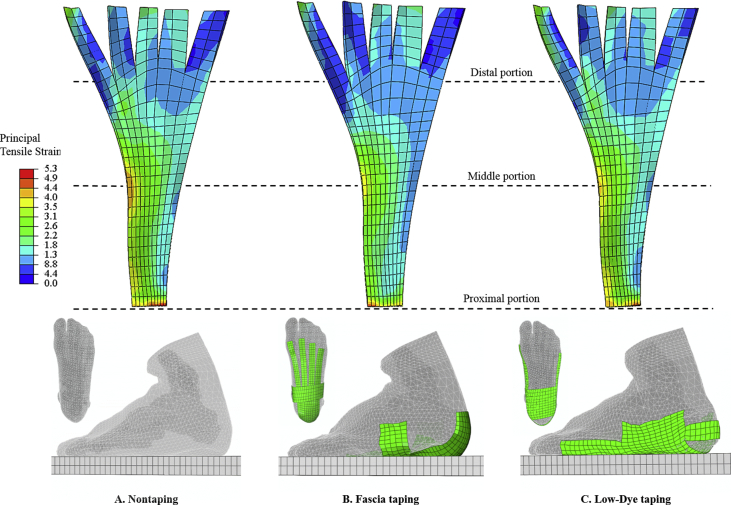
Figure 5 (B–F) plots the outcome variables as a function of the percentile stance phase. Friedman's test reported significant differences in the maximal strains of the plantar fascia (p = 0.022–0.041 for all three portions) and minimal navicular height (p = 0.015). Maximal subtalar eversion was similar among the three conditions (p = 0.449) (Table 2). Post hoc analysis showed that Fascia taping significantly increased the navicular height (p = 0.013, Kendall's W = 0.84) and reduced strains on the proximal (p = 0.034, Kendall's W = 0.76), middle (p = 0.034, Kendall's W = 0.64), and distal portions of the plantar fascia (p = 0.034, Kendall's W = 0.64) compared with nontaping (Figure 6). There were no significant differences between Low-Dye taping and nontaping (p = 0.173–0.618).
Table 2.
Results of the finite element analyses (mean ± standard deviation).
| Nontaping | Fascia taping | Low-Dye taping | p value | ||
|---|---|---|---|---|---|
| Maximal subtalar eversion (degrees) | 6.33 ± 2.32 | 5.43 ± 0.67 | 5.07 ± 0.47 | 0.449 | |
| Minimal navicular height (mm) | 36.53 ± 0.28a | 37.17 ± 0.15a | 36.71 ± 0.21 | 0.015 | |
| Maximal strains on the plantar fascia (%) | Proximal | 2.46 ± 0.10a | 2.17 ± 0.08a | 2.46 ± 0.08 | 0.022 |
| Middle | 1.95 ± 0.10a | 1.70 ± 0.08a | 1.83 ± 0.10 | 0.041 | |
| Distal | 1.20 ± 0.07a | 1.04 ± 0.03a | 1.09 ± 0.08 | 0.041 | |
Significant difference in the post hoc pairwise comparison. Bold text for p-value indicates p < 0.05.
Figure 6.
(A) Strain contour of plantar fascia for the non-taping condition; (B) Strain contour of plantar fascia for the Fascia taping condition; (C) Strain contour for the plantar fascia for the Low-Dye taping condition. The contour plots were extracted at the instant of maximal strain for a representative trial. The images are colour coded based on the distribution of principal tensile strains. Red means the highest strain, and blue means the lowest strain. Regions of the plantar fascia that are tied to the bony segments are removed from display, and the remainder is equally divided into three portions from proximal to distal. The figure shows that Fascia taping produced an apparently larger cool-tonal area, which indicates a lower strain level on average.
Discussion
The purpose of the study was to compare plantar fascia loading between untaped and taped conditions during running using a finite element foot model. Our goal was to ascertain that taping can offload the plantar fascia, whereby the application of taping treatment for overstrained plantar fascia could be supported from a mechanical perspective. In partial accordance with our hypothesis, strains on the fascia band (from proximal to distal portions) were significantly reduced by Fascia taping compared with nontaping. Fascia taping also elevated the navicular height during the stance phase. However, there were no significant differences between Low-Dye taping and nontaping.
In our study, the predicted peak value of subtalar eversion fell within the suggested normal range of 8–12° for recreational running [29], and our findings suggested that subtalar eversion was not influenced by either Low-Dye taping or Fascia taping. Particularly, Low-Dye taping did not constrain the subtalar motion as what it was structurally designed for. Previous studies usually evaluated Low-Dye taping on individuals with rearfoot overpronation, and they reported that it had little to no effects in restricting rearfoot motion during walking or running [30], [31]. Low-Dye taping may be effective in foot pronation control under static conditions [32], but the efficacy appeared to diminish shortly after dynamic tasks [12], [30]. Researchers attributed the loss of pronatory control of Low-Dye taping to its insufficient strap coverage to the heel region, which exerts poor leverage to counteract excessive rearfoot motions [31]. This defect of Low-Dye taping seemed to also limit its supportive capacity to the foot arch and the plantar fascia. Little evidence was shown in previous studies that Low-Dye taping could elevate navicular height [33], [34] and so was it in the present study.
Changes in navicular height and plantar fascia loading are closely related [35]. Both of the outcome variables were obviously altered by Fascia taping. The effectiveness of Fascia taping resides in the pretencion and alignment of the tape straps to the plantar ligaments that took up some of the total foot arch burdens and shield the loading for the plantar fascia [10]. For a running manoeuver, the degree of navicular lift by Fascia taping (0.64 mm) in the study was considered moderate compared with that reported for the less intense activity (1.45–1.5 mm), such as walking and jogging [33], [36]. Yet this small change in foot arch deformation appeared to yield apparent strain offload from the plantar fascia, which was supported by the fact that heel pain alleviation may not be necessarily facilitated by substantial improvements in arch height [1]. We believed that our prediction of fascial strain was adequately reasonable under the premise that our findings in the control condition (1.20–2.46%) were comparable with those (1.51–2.73%) reported by McDonald et al [37]. The Fascia taping reduced fascial strains by 0.16–0.29% compared with nontaping. This magnitude of changes is similar to the measurements of a cadaveric study, which reported a strain alteration of 0.4% is approximately equivalent to windlass the fascia by dorsiflexing the first metatarsophalangeal joint by around 15° [38]. Interestingly, patients with plantar fasciitis had significantly less active and passive range of motion in the first metatarsophalangeal joint possibly due to the reluctance to strains on the plantar fascia [39]. In this regard, we speculated that the decreased fascial strain by Fascia taping, although at a small degree, might possess clinical importance in terms of either pain relief or function improvement.
Albeit not completely supported by our findings, the satisfactory clinical outcomes of using Low-Dye taping are undeniable [40]. Many Low-Dye taping studies to date did not perform participants' screening based on their rearfoot alignment [6], [41]. Studies controlling this factor were more consistent in the outcomes—symptom alleviation was showed in patients with rearfoot overpronation [8], [42], but not in those having a neutral foot [43]. As a result, we believed that Low-Dye taping is better indicated for patients with plantar fasciitis and rearfoot overpronation, but not to those having a healthy rearfoot alignment [1]. In contrast, Fascia taping could be relatively more applicable to a boarder patient population because the design targets on the plantar fascia strain directly and shall not be attenuated by the rearfoot alignment. Although there are currently no normative strain values for treatment evaluation and injury prognosis and the reduction of fascial strains by Fascia taping seemed small, its accumulative effects over thousands of gait cycles may still be profound, given that the dense connective tissue of plantar fascia normally requires a slow and prolonged recovery procedure [43]. Our findings partially supported the recommendation of using taping as the immediate tension-release management for overstrained plantar fascia [44].
To accommodate patients' conditions, taping modalities were usually modified and could vary greatly from their original forms [12]. Thus, evaluating all kinds of taping modalities remains infeasible. However, a mixed application of more than one taping modality seemed to address multiple factors and provide satisfactory outcomes [45]. There was a complex interaction between taping and the foot and ankle. The benefits of taping treatment shall integrate the effects of biomechanical, neurophysiological, and psychological considerations [14]. Further investigation is warranted to explore the underlying mechanism.
The results of this study should be interpreted in light of some limitations. First, generalisation of our research outcomes is weakened by the single-case design. Despite the advancements in computing power, batch processing of patient-specific models is still challenging for the foot–ankle complex owing to its multitude of components, highly complicated joint contact, and loading conditions [46]. Some studies chose to increase the sample size at the costs of oversimplifications on the foot structures and loading boundaries [46]. This is not applicable in the present study as the strength of our model was warranted by its complexity. In practice, researchers adopt a single-case design by selecting a typical or representative model participant with reasonable sets of loading conditions and assume that it could address the concern of external validity [19]. However, this approach still has the weakness in accounting for population variances. Second, the recruited runner was asymptomatic. Most finite element studies constructed the foot models using healthy participants and derived clinical implications theoretically or created the pathological identity by impoverishing some features of the normal foot model [46]. Although we endorsed the former approach to investigate the fascia strain of the normal foot, patients with plantar fasciitis may present different foot structures or loading patterns that may require further investigations. Third, the intrinsic foot muscles were modelled as string units in our foot model, which only yielded passive strength when elongated. The active part of the intrinsic foot muscle force was ignored owing to the technical difficulty in tracking its contraction.
Conclusion
The study investigated how different taping methods could affect loading on the plantar fascia in running through an approach of computational simulation. Our prediction showed that, compared with the control (nontaping), fascia taping reduced maximal strains on the fascia band and increased navicular height slightly during the stance phase, whereas Low-Dye taping did not cause obvious changes. Our results supported the application of taping treatments for plantar fascia suffering from overstraining. The relaxed fascia band by Fascia taping could be positive to relieve pain for runners who injure their plantar fascia from a mechanical cause. Future studies shall consider a patient-specific experiment for a firm conclusion.
Conflicts of interest statement
The authors have no conflicts of interest to disclose in relation to this article.
Funding
This work was supported by National Key R&D Program of China granted by the Ministry of Science and Technology of China (grant number: 2018YFB1107000), General Research Fund granted by the Hong Kong Research Grant Council (grant numbers: PolyU152065/17E, PolyU152002/15E), NSFC granted by the National Natural Science Foundation of China (grant number: 11732015).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jot.2019.06.006.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Jamali B., Walker M., Hoke B., Echternach J. Windlass taping technique for symptomatic relief of plantar fasciitis. J Sport Rehabil. 2004;13:228–243. [Google Scholar]
- 2.Riddle D.L., Pulisic M., Pidcoe P., Johnson R.E. Risk factors for Plantar fasciitis: a matched case-control study. J Bone Joint Surg Am. 2003;85-A doi: 10.2106/00004623-200305000-00015. 872–7. [DOI] [PubMed] [Google Scholar]
- 3.Buchbinder R. Clinical practice. Plantar fasciitis. N Engl J Med. 2004;350:2159–2166. doi: 10.1056/NEJMcp032745. [DOI] [PubMed] [Google Scholar]
- 4.Tong K.B., Furia J. Economic burden of plantar fasciitis treatment in the United States. Am J Orthoped. 2010;39:227–231. [PubMed] [Google Scholar]
- 5.Wearing S.C., Smeathers J.E., Urry S.R., Hennig E.M., Hills A.P. The pathomechanics of plantar fasciitis. Sport Med. 2006;36:585–611. doi: 10.2165/00007256-200636070-00004. [DOI] [PubMed] [Google Scholar]
- 6.Landorf K.B., Radford J.A., Keenan A.-M., Redmond A.C. Effectiveness of low-Dye taping for the short-term management of plantar fasciitis. J Am Podiatr Med Assoc. 2005;95:525–530. doi: 10.7547/0950525. [DOI] [PubMed] [Google Scholar]
- 7.Podolsky R., Kalichman L. Taping for plantar fasciitis. J Back Musculoskelet Rehabil. 2015;28:1–6. doi: 10.3233/BMR-140485. [DOI] [PubMed] [Google Scholar]
- 8.Hyland M.R., Webber-Gaffney A., Cohen L., Lichtman S.W. Randomized controlled trial of calcaneal taping, sham taping, and plantar fascia stretching for the short-term management of plantar heel pain. J Orthop Sport Phys Ther. 2006;36:364–371. doi: 10.2519/jospt.2006.2078. [DOI] [PubMed] [Google Scholar]
- 9.Donatelli R. F.A. Davis; 1996. The biomechanics of the foot and ankle. [Google Scholar]
- 10.Tsai C.-T., Chang W.-D., Lee J.-P. Effects of short-term treatment with kinesiotaping for plantar fasciitis. J Musculoskelet Pain. 2010;18:71–80. [Google Scholar]
- 11.Hicks J.H. The mechanics of the foot: II. The plantar aponeurosis and the arch. J Anat. 1954;88:25. [PMC free article] [PubMed] [Google Scholar]
- 12.Radford J.A., Burns J., Buchbinder R., Landorf K.B., Cook C. The effect of low-Dye taping on kinematic, kinetic, and electromyographic variables: a systematic review. J Orthop Sport Phys Ther. 2006;36:10. doi: 10.2519/jospt.2006.36.4.232. [DOI] [PubMed] [Google Scholar]
- 13.van de Water A.T.M., Speksnijder C.M. Efficacy of taping for the treatment of plantar fasciosis: a systematic review of controlled trials. J Am Podiatr Med Assoc. 2010;100:41–51. doi: 10.7547/1000041. [DOI] [PubMed] [Google Scholar]
- 14.Franettovich M., Chapman A., Blanch P., Vicenzino B. A physiological and psychological basis for anti-pronation taping from a critical review of the literature. Sport Med. 2008;38:617–631. doi: 10.2165/00007256-200838080-00001. [DOI] [PubMed] [Google Scholar]
- 15.Davis I.S., Rice H.M., Wearing S.C. Why forefoot striking in minimal shoes might positively change the course of running injuries. J Sport Health Sci. 2017;6:154–161. doi: 10.1016/j.jshs.2017.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cutts S., Obi N., Pasapula C., Chan W. Plantar fasciitis. Ann R Coll Surg Engl. 2012;94:539–542. doi: 10.1308/003588412X13171221592456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen T.L.-W., Agresta C.E., Lipps D.B., Provenzano S.G., Hafer J.F., Wong D.W.-C. Ultrasound elastographic assessment of plantar fascia in runners using rearfoot strike and forefoot strike. J Biomech. 2019;89:65–71. doi: 10.1016/j.jbiomech.2019.04.013. [DOI] [PubMed] [Google Scholar]
- 18.Chen T.L.-W., Wong D.W.-C., Wang Y., Lin J., Zhang M. Foot arch deformation and plantar fascia loading during running with rearfoot strike and forefoot strike: a dynamic finite element analysis. J Biomech. 2019;83:260–272. doi: 10.1016/j.jbiomech.2018.12.007. [DOI] [PubMed] [Google Scholar]
- 19.Wong D.W.-C., Wang Y., Leung A.K.-L., Yang M., Zhang M. Finite element simulation on posterior tibial tendinopathy: load transfer alteration and implications to the onset of pes planus. Clin Biomech. 2018;51:10–16. doi: 10.1016/j.clinbiomech.2017.11.001. [DOI] [PubMed] [Google Scholar]
- 20.Cavanagh P.R., Rodgers M.M. The arch index: a useful measure from footprints. J Biomech. 1987;20:547–551. doi: 10.1016/0021-9290(87)90255-7. [DOI] [PubMed] [Google Scholar]
- 21.John C.T., Anderson F.C., Higginson J.S., Delp S.L. Stabilisation of walking by intrinsic muscle properties revealed in a three-dimensional muscle-driven simulation. Comput Methods Biomech Biomed Eng. 2013;16:451–462. doi: 10.1080/10255842.2011.627560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gray S. Knopf Doubleday Publishing Group; 2011. Gray's anatomy. [Google Scholar]
- 23.Cheng H.-Y.K., Lin C.-L., Wang H.-W., Chou S.-W. Finite element analysis of plantar fascia under stretch—the relative contribution of windlass mechanism and Achilles tendon force. J Biomech. 2008;41:1937–1944. doi: 10.1016/j.jbiomech.2008.03.028. [DOI] [PubMed] [Google Scholar]
- 24.Boonkerd C., Limroongreungrat W. Elastic therapeutic tape: do they have the same material properties? J Phys Ther Sci. 2016;28:1303–1306. doi: 10.1589/jpts.28.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang M., Mak A.F. In vivo friction properties of human skin. Prosthet Orthot Int. 1999;23:135–141. doi: 10.3109/03093649909071625. [DOI] [PubMed] [Google Scholar]
- 26.Wu G., Siegler S., Allard P., Kirtley C., Leardini A., Rosenbaum D. ISB recommendation on definitions of joint coordinate system of various joints for the reporting of human joint motion—part I: ankle, hip, and spine. J Biomech. 2002;35:543–548. doi: 10.1016/s0021-9290(01)00222-6. [DOI] [PubMed] [Google Scholar]
- 27.Clark R.A., Franklyn-Miller A., Falvey E., Bryant A.L., Bartold S., McCrory P. Assessment of mechanical strain in the intact plantar fascia. Foot. 2009;19:161–164. doi: 10.1016/j.foot.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 28.Cohen J. 2 edition. Routledge; Hillsdale, N.J: 1988. Statistical power analysis for the behavioral sciences. [Google Scholar]
- 29.DeLeo A.T., Dierks T.A., Ferber R., Davis I.S. Lower extremity joint coupling during running: a current update. Clin Biomech. 2004;19:983–991. doi: 10.1016/j.clinbiomech.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 30.Harradine P., Herrington L., Wright R. The effect of low Dye taping upon rearfoot motion and position before and after exercise. Foot. 2001;11:57–60. [Google Scholar]
- 31.Keenan A.-M., Tanner C.M. The effect of high-Dye and low-Dye taping on rearfoot motion. J Am Podiatr Med Assoc. 2001;91:255–261. doi: 10.7547/87507315-91-5-255. [DOI] [PubMed] [Google Scholar]
- 32.Whitaker J.M., Augustus K., Ishii S. Effect of the low-Dye strap on pronation-sensitive mechanical attributes of the foot. J Am Podiatr Med Assoc. 2003;93:118–123. doi: 10.7547/87507315-93-2-118. [DOI] [PubMed] [Google Scholar]
- 33.Holmes C.F., Wilcox D., Fletcher J.P. Effect of a modified, low-Dye medial longitudinal arch taping procedure on the subtalar joint neutral position before and after light exercise. J Orthop Sport Phys Ther. 2002;32:194–201. doi: 10.2519/jospt.2002.32.5.194. [DOI] [PubMed] [Google Scholar]
- 34.Newell T, Simon J, Docherty CL. Arch-taping techniques for altering navicular height and plantar pressures during activity. J Athl Train. 2015;50:825–832. doi: 10.4085/1062-6050-50.5.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kirby K.A. Longitudinal arch load-sharing system of the foot. Revista Española de Podología. 2017;28:e18–26. [Google Scholar]
- 36.Ator R., Gunn K., McPoil T.G., Knecht H.C. The effect of adhesive strapping on medial longitudinal arch support before and after exercise. J Orthop Sport Phys Ther. 1991;14:18–23. doi: 10.2519/jospt.1991.14.1.18. [DOI] [PubMed] [Google Scholar]
- 37.McDonald K.A., Stearne S.M., Alderson J.A., North I., Pires N.J., Rubenson J. The role of arch compression and metatarsophalangeal joint dynamics in modulating plantar fascia strain in running. PLoS One. 2016;11 doi: 10.1371/journal.pone.0152602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Carlson R.E., Fleming L.L., Hutton W.C. The biomechanical relationship between the tendoachilles, plantar fascia and metatarsophalangeal joint dorsiflexion angle. Foot Ankle Int. 2000;21:18–25. doi: 10.1177/107110070002100104. [DOI] [PubMed] [Google Scholar]
- 39.Irving D.B., Cook J.L., Menz H.B. Factors associated with chronic plantar heel pain: a systematic review. J Sci Med Sport. 2006;9:11–22. doi: 10.1016/j.jsams.2006.02.004. [DOI] [PubMed] [Google Scholar]
- 40.Landorf K.B., Menz H.B. Plantar heel pain and fasciitis. BMJ Clin Evid. 2008;2008 [PMC free article] [PubMed] [Google Scholar]
- 41.Van Lunen B., Cortes N., Andrus T., Walker M., Pasquale M., Onate J. Immediate effects of a heel-pain orthosis and an augmented low-dye taping on plantar pressures and pain in subjects with plantar fasciitis. Clin J Sport Med. 2011;21:474–479. doi: 10.1097/JSM.0b013e3182340199. [DOI] [PubMed] [Google Scholar]
- 42.Abd El Salam M.S., Abd Elhafz Y.N. Low-dye taping versus medial arch support in managing pain and pain-related disability in patients with plantar fasciitis. Foot Ankle Spec. 2011;4:86–91. doi: 10.1177/1938640010387416. [DOI] [PubMed] [Google Scholar]
- 43.Radford J.A., Landorf K.B., Buchbinder R., Cook C. Effectiveness of low-Dye taping for the short-term treatment of plantar heel pain: a randomised trial. BMC Muscoskelet Disord. 2006;7 doi: 10.1186/1471-2474-7-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Orchard J. Plantar fasciitis. BMJ. 2012;345 doi: 10.1136/bmj.e6603. e6603–e6603. [DOI] [PubMed] [Google Scholar]
- 45.Van Tonder T., Allison G.T., Hopper D., Grisbrook T.L. Multidimensional impact of low-Dye taping on low-load hopping in individuals with and without plantar fasciitis. Phys Ther Sport. 2018;29:43–49. doi: 10.1016/j.ptsp.2017.11.001. [DOI] [PubMed] [Google Scholar]
- 46.Wang Y., Wong D.W.-C., Zhang M. Computational models of the foot and ankle for pathomechanics and clinical applications: a review. Ann Biomed Eng. 2016;44:213–221. doi: 10.1007/s10439-015-1359-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.