Abstract
Objective
The aim of this study was to investigate whether there is an increased risk of anterior knee pain (AKP) after total knee arthroplasty (TKA) without patellar resurfacing in patients with rheumatoid arthritis (RA) versus primary osteoarthritis (OA).
Methods
This study was a retrospective review of 388 patients (577 knees) who underwent TKA without patellar resurfacing between 2003 and 2011, with a minimum of 5 years of follow-up. Patients were divided into two groups: Group OA (273 knees of 206 patients; 83 males, 123 females; mean age: 64.4 (47–87) years) and Group RA (304 knees of 182 patients; 92 males, 90 females; mean age: 50.7 (21–72) years). In the clinical evaluation, the knee range of motion (ROM) and several outcome measures such as The Knee Society Score (KSS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) score, and International Knee Documentation Committee (IKDC) scores were used preoperatively and at the final follow-up visit. The quality of life was measured using Short Form (SF)-36 MCS and PCS scores. The primary outcome was the frequency and severity of patient-reported AKP. The AKP Scale was used to determine the severity of AKP.
Results
The IKDC raised from 21.62 (range, 13–29.9) preoperatively to 85.1 (range, 80–88) for group OA and from 21.8 (range, 13–29.9) to 85.2 (range, 81–88) for group RA (p < 0.001). The mean KSS improved from 28.35 (range, 22–38) preoperatively to 90.04 (range, 88–95) for group OA and from 21.9 (range, 18–35) preoperatively to 89.7 (range, 86–95) for group RA. The mean WOMAC increased from 20.61 (range, 17.4–24.2) preoperatively to 95.7 (range, 90.9–97.7) for group OA (p < 0.001) and from 20.2 (range, 16.7–24.2) preoperatively to 95.8 (range, 90.9–98.5) for group RA (p < 0.001). The mean ROM improved from 80.14° (range, 55°–130°) preoperatively to 113.17° (range, 95°–140°) in group OA (P = 0.003) and from 73.4° (range, 10°–130°) to 112.8° (range 90°–140°) in group RA (P = 0.003) postoperatively. The frequency of AKP was 8% in Group OA and 7% in Group RA (p = 0.27). For patients with AKP, the mean AKP Scale was 92.74 (range, 84–98) in Group OA and 93.39 (range, 82–98) in Group RA (p = 0.3).
Conclusion
After TKA without resurfacing the patella, patients with RA were determined to have a similar risk for AKP as those with OA.
Level of evidence
Level III, Therapeutic Study.
Keywords: Total knee arthroplasty, Anterior knee pain, Primary osteoarthritis, Rheumatoid arthritis, Patellar resurfacing, Patellar retention
Introduction
With a reported incidence ranging from 4% to 50%, anterior knee pain (AKP) has been cited as one of the most common causes of persistent pain following total knee arthroplasty (TKA), despite advancements in orthopedic implant architecture and the upward trend for minimally invasive surgery.1, 2 Although multifactorial etiology, AKP is considered to stem primarily from the patellofemoral joint.3, 4 Therefore, considerable research attention has been devoted to comparing patellar retention and patellar resurfacing regarding this issue,3, 5, 6 and there continues to be heated debate over whether or not resurfacing the patella has a role in minimizing the frequency of residual patellofemoral pain in the literature.7, 8
Another area of disagreement among researchers is the necessity to routinely resurface the patella in rheumatoid arthritis (RA).9, 10 Several authors regard patellar resurfacing as a necessary procedure for patients with RA since the retained patellar articular cartilage and bone stock may keep the antigenic feature active and lead to recurrence of anterior knee symptoms.11, 12, 13 In contrast, some authors inferred that routine resurfacing should be avoided in all cases because of the poor patellar bone stock caused by RA and its pertinent complications.9, 14, 15 In addition, despite the lower incidence of resurfacing complications in RA versus osteoarthritis (OA), most likely due to a lower level of activity, the patellar bone loss may pose a challenge to surgeons as demonstrated with a need for revision.11, 12
The present study aimed to investigate whether there is a difference in the rate of AKP after TKA without patellar resurfacing in patients with RA compared to patients with OA. Our hypothesis was that there may be no differences in terms of the rates of AKP between patients with either primary OA or RA who underwent TKA without patellar resurfacing.
Patients and methods
The study protocol
The study protocol involved as follows:
-
I)
to consider patients according to eligibility criteria (inclusion and exclusion) given in Table 1,
-
II)
to evaluate patellofemoral pain (anterior knee pain) and instability/functionality according to The AKP Scale as well as a visual analogue scale (VAS) of anterior knee pain at rest,
-
III)
to assess clinical outcome for total knee replacement according to different clinical scoring systems, measuring various domains, commonly function, consisting of The KSS, WOMAC score, and IKDC scores,
-
IV)
to measure the ROM of the knee.
-
V)
to measure the quality of life using SF-36 MCS and PCS scores.
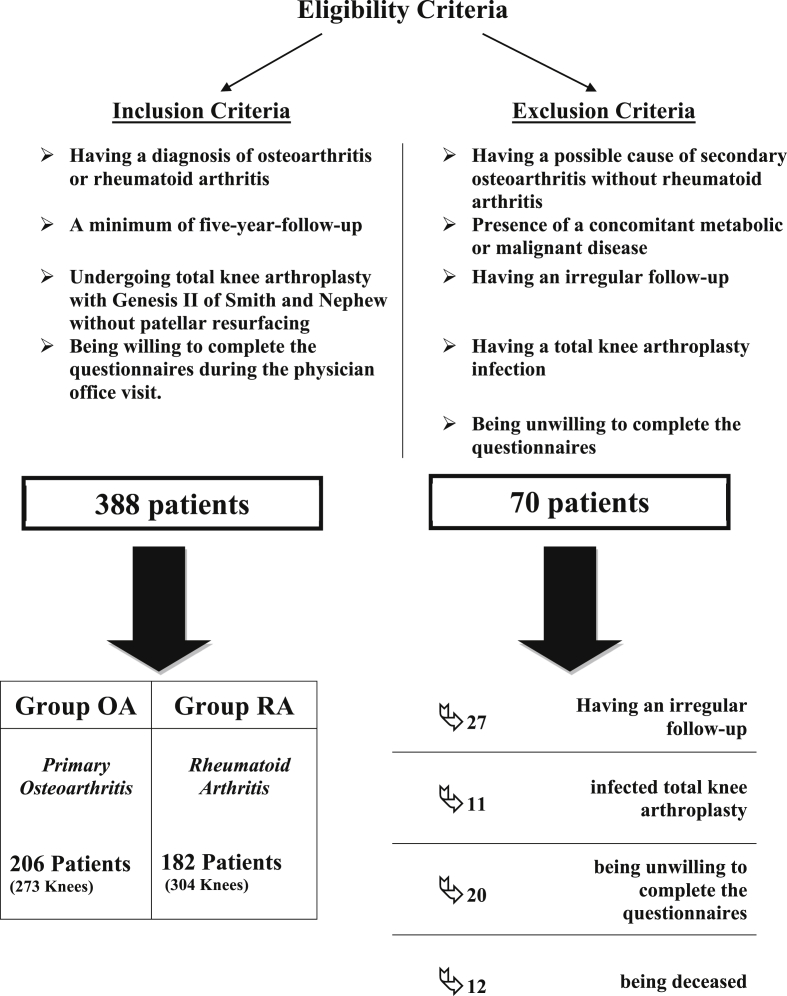
Table 1.
The flow chart of the study participants.
Approval of the institutional board review was obtained.
Patients
521 consecutive patients who underwent total knee arthroplasty with a diagnosis of OA or RA, between 2003 and 2011 were retrospectively reviewed. Of these, 458 patients (88%) could be contacted and invited to a final follow-up examination. Considering eligibility criteria, after excluding 70 patients (27 patients were unable to come to follow-up appointments, 11 patients (1.9%) underwent a revision surgery due to an infected total knee arthroplasty, 20 patients refused to fill in the questionnaires, 12 patients were deceased), remaining 388 patients (577 knees) who met the inclusion criteria were included in the study and were retrospectively reviewed based on our institution medical records including plain radiography, operative notes, information on demographic characteristics, discharge reports, progress notes and final follow-up radiological and physical examination.
Patients included in the study were divided into two groups: group OA and group RA. Group OA included 273 knees of 206 patients (123 female, 83 male) with OA, and group RA included 304 knees of 182 patients (90 females, 92 males) with RA.
The mean age of the patients was 64.4 years (range, 47–87) in group OA and 50.7 years (range, 21–72) in group RA. The average length of follow-up was 101.3 months (range, 60–152) in group OA and 102.6 months (range, 60–142) in group RA. Patients in either group were comparable in terms of the demographic data given in Table 2 (p > 0.05 for age, number, duration of follow-up).
Table 2.
Demographic characteristics of patient groups.
| Group OA | Group RA | |
|---|---|---|
| Number of patients | 206 | 182 |
| Number of knees investigated | 273 | 304 |
| Median age at time of surgery | 64.4 years (range, 47–87) | 50.7 years (range, 21–72) |
| Male/female | 83/123 | 92/90 |
| Mean follow-up | 101.3 months (range, 60–152) | 102.6 months (range, 60–142) |
Clinical evaluation and outcome measures
In the evaluation of clinical outcome for total knee replacement, in addition to measurement of the knee range of motion, The KSS,16 WOMAC score,17 and IKDC score16 were undertaken for each patient included in the present study preoperatively and at the final follow-up visit. ROM was measured with a universal standard goniometer by senior orthopaedic surgeons in our department. While the KSS was performed by senior orthopaedic surgeons, The WOMAC and IKDC scores were completed by patients.
The primary outcome of the present study comprised the frequency and severity of patient-reported AKP. At the final follow-up, in order to identify AKP with the origin of the patellofemoral joint, a specific quiz for the patella was rendered to each patient. The quiz contained the presence of AKP, an association of pain with stair ascending and rising from a chair, and the presence of patellar cracking or popping. It was regarded that the presence of only one element was sufficient to identify AKP. In patients with AKP who were determined by the quiz, the frequency of AKP was calculated. To estimate the severity of AKP, the AKP Scale18 was chosen as the primary outcome criterion and was applied to all the patients included in the study. Additionally, VAS, as a nonspecific test, was used to assess AKP at rest.
The AKP Scale, also called the Kujala Score, is a disease-specific, validated disability scale for patellofemoral problems. The self-administered questionnaire contains 13 items involving pain and functionality. Scores are obtained by summing all the items on a total scale of 0–100 (lower scores indicate greater pain and disability).16, 18
Surgical technique
The surgical schedule comprised a midline skin incision and standard medial parapatellar approach. All the patients in both groups underwent the GENESIS II™ cemented, fixed-bearing total knee endoprosthesis with ultra-high molecular weight polyethylene (Smith & Nephew, Memphis, TN, USA). While the posterior-cruciate-retaining design was preferred for all the patients in group OA, patients with RA mostly received posterior-cruciate-substituting design (298 of 304 knees). Case series of orthopedic surgeons (two senior surgeons predominantly) at the same institute, who had not preferred to resurface the patella, were used in the study. Patella was not replaced, and only removal of marginal osteophytes was applied to all patients included in the study.
Statistical analysis
Statistical software package SPSS 20.0 (IBM Corp, 2011, Armonk, New York) was used for analysis. Statistical significance was set at P < 0,05; results were considered statistically highly significant if p < 0,001. ANOVA, chi-square, Mann-Whitney-U Wilcoxon, and Fisher's exact tests with the application of Bonferroni's correction were used for the statistical analysis.
Results
The demographic data were parallel in the two groups (p > 0.05 for age, number, duration of follow-up). Table 3 demonstrates comparison of results of ROM and other outcome measures between patient groups.
Table 3.
Comparison of ROM and outcome measures between patient groups.
| Group OA |
Group RA |
||||
|---|---|---|---|---|---|
| Pre-operative | Post-operative | Pre-operative | Post-operative | ||
| IKDC score | 21.62 (13–29.9) | 85.1 (80–88) | 21.8 (range, 13–29.9) | 85.2 (81–88) | p < 0.001 |
| KSS | 28.35 (22–38) | 90.04 (88–95) | 21.9 (18–35) | 89.7 (86–95) | p < 0.001 |
| WOMAC | 20.61 (17.4–24.2) | 95.7 (90.9–97.7) | 20.2 (16.7–24.2) | 95.8 (90.9–98.5) | p < 0.001 |
| SF-36 PCS | 55.24 (51.9–57.4) | 55.19 (51.6–57.4) | p = 0.27 | ||
| SF-36 MCS | 54.55 (50.7–56.4) | 54.52 (50.5–56.4) | p = 0.30 | ||
| ROM | 80.14° (55°–130°) | 113.17° (95°-14°) | 73.4° (10°–130°) | 112.8° (90°–140°) | P = 0.003 |
| The AKP scale (Kujala Score) | 92.74 (84–98) | 93.39 (82–98) | P = 0.3 | ||
| VAS | 6.2 (5–8) | 0.49 (0–4) | 6.31 (5–8) | 0.46 (0–4) | P < 0.001 |
OA: Osteoarthritis, RA: Rheumatoid arthritis, IKDC score: International Knee Documentation Committee Score, KSS: Knee Society Score, WOMAC: Western Ontario and McMaster Universities Osteoarthritis Index, SF-36: Short-Form 36, ROM: Range of Motion, AKP (Anterior Knee Pain), VAS: Visual Analogue Scale.
Knee-specific outcome measures
The IKDC raised from 21.62 (range, 13–29.9) preoperatively to 85.1 (range, 80–88) for group OA and from 21.8 (range, 13–29.9) to 85.2 (range, 81–88) for group RA after a similar period of follow-up (p < 0.001).
Osteoarthritis-specific outcome measures
The mean KSS improved from 28.35 (range, 22–38) preoperatively to 90.04 (range, 88–95) for group OA and from 21.9 (range, 18–35) preoperatively to 89.7 (range, 86–95) for group RA at a minimum follow-up of 5 years. Similarly, the mean WOMAC increased from 20.61 (range, 17.4–24.2) preoperatively to 95.7 (range, 90.9–97.7) for group OA and from 20.2 (range, 16.7–24.2) preoperatively to 95.8 (range, 90.9–98.5) for group RA after a minimum follow-up of five years (p < 0.001 for both scores).
Assessment of ROM
Similarly, as in previous clinical outcomes, the mean ROM demonstrated an obvious increase in the two groups, which was elevated from 80.14° (range, 55°–130°) preoperatively to 113.17° (range, 95°-140°) in group OA (P = 0.003) and from 73.4° (range, 10°–130°) to 112.8° (range 90°–140°) in group RA (P = 0.003) postoperatively. No significant difference was found in the postoperative improvement of ROM between the two groups (p = 0.003).
Health-related quality of life measure
In group OA, the mean physical component score (PCS) was 55.24 (range, 51.9–57.4), and the mean mental component score (MCS) was 54.55 (range, 50.7–56.4). In group RA, the mean PCS was 55.19 (range, 51.6–57.4), and the mean MCS was 54.52 (range 50.5–56.4). In terms of SF-36 PCS and MCS, no statistically significant difference was observed between the two groups (p = 0.27 and p = 0.30, respectively).
Evaluation of patellofemoral joint
According to the patella-specific quiz, the frequency of AKP was 8% (22 of 273 knees) in group OA and 7% (21 of 304 knees) in group RA (p = 0.27).
For patients with AKP, the mean Anterior Knee Pain Scale (Kujala Score) was 92.74 (range, 84–98) in group OA and 93.39 (range, 82–98) in group RA (p = 0.3).
When compared preoperative with postoperative values, the mean AKP - VAS at rest showed a significant decrease in both groups, which dropped from 6.2 (range, 5–8) to 0.49 (range, 0–4) in group OA and from 6.31 (range, 5–8) to 0.46 (range, 0–4) (p < 0,001).
Discussion
A multitude of factors have been attributed to the contentious aetiology of AKP after TKA, including patellar instability; patellar maltracking; patellar fracture; inflammation of the tendon, bursa, or synovium around the patella; inappropriate soft tissue balancing; prosthetic design; and even patient characteristics.8, 9, 19, 20 However, there seems to be general agreement in the literature that patellofemoral articulation is the most common etiology. Therefore, numerous studies to date have investigated the association between AKP and patellar resurfacing in TKA.13, 21, 22, 23 Although most studies, including current meta-analyses, comprise mostly patients with primary OA,3, 6, 24, 25, 26 only a few studies have been conducted on patients with RA.8, 9, 12, 27
The present study compared the frequency and severity of anterior knee pain and the clinical and functional outcomes of TKAs without patellar resurfacing in patients with RA and OA. As in previous studies,12, 25, 28 the results of the current study have confirmed that TKA is effective in resolving chronic and debilitating knee pain as reported by most patients with OA and RA, with no significant difference between the two groups in terms of general or specific clinical rating systems.
We aimed to clarify whether there is an increased risk of AKP after TKA in patients with RA compared to patients with OA, as there is conflicting research about whether to resurface the patella in the rheumatoid knee or not. The main theoretical argument against routine patellar resurfacing for rheumatoid knees is the concern about antigens from the retained patellar articular cartilage and bone stock stimulating recurrent synovial inflammation.12, 13, 27 Proponents of this argument recommend routine resurfacing of the patella to avoid recurrence of the disease, thus minimizing the frequency of anterior knee pain and other patellofemoral complications.10, 27 However, it seems that the philosophy of surgeons regarding this problem is not in agreement with the facts of daily orthopaedic practice, as opponents of routine patellar resurfacing for rheumatoid knees have highlighted the risks of patellar fracture, avascular necrosis, bone loss for revision, and predictable deterioration of the extensor mechanism after resurfacing operations.27, 29 In the absence of patellar resurfacing, some authors have found lower rates of persistent AKP for rheumatoid patients.8, 15, 30
While there has been a great deal of research about the incidence of persistent AKP for OA patients,3, 24, 25, 31 a limited number of studies have focused on RA patients.8, 9, 12, 27 In a retrospective study that involved 1778 total knee replacements without patellar resurfacing, Metsna et al.8 reported the incidence of postoperative anterior knee pain as 20.5% (range 17.7–23.4) in patients with primary OA and as 15.1% (range 7.8–25.4) in patients with RA, with a mean follow-up of period of 69 months. They concluded that AKP was more prevalent among osteoarthritic knees compared to rheumatoid knees. However, the aforementioned study had a bias related to patient percentages, as it included 90.7% of OA patients and 8.2% of RA patients. In their study to determine the association between pre- and postoperative knee pain, Bhan et al.27 prospectively monitored 139 knees of 80 RA patients who underwent total knee replacement without patellar resurfacing. The study had satisfactory mid-term results (mean length of follow-up of 5.8 years) in terms of the incidence of anterior knee pain (approximately 8.5%) in addition to a lower rate of secondary resurfacing. Similarly, Holt et al.9 obtained satisfactory results with respect to pain relief and function by retaining the native patella in a total of 30 rheumatoid knees at a mean follow-up of 24 months, with an incidence of AKP of 13.3%. However, no comparative group was enrolled in the last two studies.9, 27 In a study similar to the present one, Deehan et al.12 attempted to compare the level of anterior knee function between OA and RA patients who underwent TKA without patellar resurfacing. More than 120 knee replacements were examined in each group, with a mean follow-up of 10 years. No significant difference with regard to anterior knee pain and function between the two groups was identified.
When it comes to advocating routine patellar resurfacing for RA, the studies are limited by poor study design and include relatively small and heterogeneous groups of OA and RA patients (some have no RA patients) to compare the frequency and severity of anterior knee pain.29, 31, 32 In the present study, we observed no difference in terms of the frequency and severity of anterior knee pain following TKA without patellar resurfacing at a minimum follow-up of 5 years when comparing the relatively large group of patients with either primary OA or RA. The incidence of anterior knee pain was 7% in the RA group and 8% in the primary OA group. The mean Anterior Knee Pain Scale score (the Kujala score) was 92.74 (range 84–98) in the OA group and 93.39 (range 82–98) in the RA group. Our findings support the current literature in that we observed lower rates of AKP for patients with RA compared to patients with OA. In addition, none of the patients in either group underwent secondary resurfacing of the patella for any reason, including anterior knee pain or instability.
The key strengths of this study were its relatively long follow-up period, having a comparative group of patients and the use of the Kujala score, a disease-specific, validated disability scale for patellofemoral problems. Furthermore, three surgeons performed all the operations using similar techniques, similar implants and a cruciate-retaining or a posterior-stabilized design, thus minimizing implant- and surgeon-related bias.
This study has some important limitations. The first is the retrospective nature of the study. The second is that it did not involve pre-operative Kujala scores because Kujala scores were not available for most of the patients included in the study at the time of surgery. However, many studies have also found no significant correlation between pre- and postoperative Kujala scores.26, 33 The third is that it did not include a group of patients who underwent TKA with patellar resurfacing. Finally, a cruciate-retaining TKA design was used for OA patients and a posterior-stabilized TKA design was used for RA patients. Although the prosthesis design has no marked impact on the issue of AKP, it may be considered a limitation.
Based on the existing literature and the results of this study, we disagree with the theoretical argument regarding anterior knee pain and patellar retention for patients with RA. We found a relatively lower incidence and decreased severity of AKP with the retention of the native patella in both groups of patients. Our study is a retrospective comparative study that includes a control group of patients with OA, thus allowing for a comparison in terms of the rate and severity of AKP after patellar retention in TKA between RA and non-RA patients. Moreover, we think it that more prospective, randomized, controlled studies including patients with RA and primary OA who underwent TKA with and without patellar resurfacing are needed to resolve the debate regarding patellar resurfacing and enlighten the true reason behind the multifactorial etiology in terms of AKP.
Conclusion
A significant improvement in terms of the clinical and functional status of patients with OA and patients with RA who underwent TKA without patellar resurfacing was observed. An amelioration of health-related quality of life was noticed in both groups. Overall, this study has provided additional evidence that after TKA without resurfacing the patella, patients with RA were detected to have a similar risk for AKP as those with OA.
Funding statement
IRB Approval: This study protocol was approved by the institutional board review of Istanbul University, Istanbul Faculty of Medicine. No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article. The authors declare that they have no competing interests.
Conflicts of interest
The authors “Tuna Pehlivanoğlu, Halil İbrahim Balcı, Mehmet Demirel, Mehmet Fevzi Çakmak, Önder Yazıcıoğlu, and Önder İ. Kılıçoğlu’’ individually declare that they have no conflict of interest, and no benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Footnotes
This study has not been published elsewhere before. It is not accepted for publication and under consideration by another publication.
Each author certifies that he or she has no commercial associations that might pose a conflict of interest in connection with the submitted article.
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
Contributor Information
Tuna Pehlivanoglu, Email: tunapehlivanoglu@gmail.com.
Halil Ibrahim Balci, Email: balcihalili@hotmail.com.
Mehmet Demirel, Email: dr88.mehmet.demirel@gmail.com.
Mehmet Fevzi Cakmak, Email: mehmetfevzicakmak@gmail.com.
Onder Yazicioglu, Email: oyazici@istanbul.edu.tr.
Onder Ismet Kilicoglu, Email: kilicoglu@istanbul.edu.tr.
References
- 1.Meftah M., Ranawat A.S., Ranawat C.S. The natural history of anterior knee pain in 2 posterior-stabilized, modular total knee arthroplasty designs. J Arthroplasty. 2011;26(8):1145–1148. doi: 10.1016/j.arth.2010.12.013. [DOI] [PubMed] [Google Scholar]
- 2.Indelli P., Aglietti P., Buzzi R., Baldini A. The Insall-Burstein II prosthesis: a 5-to 9-year follow-up study in osteoarthritic knees. J Arthroplasty. 2002;17(5):544–549. doi: 10.1054/arth.2002.32186. [DOI] [PubMed] [Google Scholar]
- 3.Li S., Chen Y., Su W., Zhao J., He S., Luo X. Systematic review of patellar resurfacing in total knee arthroplasty. Int Orthop. 2011;35(3):305–316. doi: 10.1007/s00264-010-1109-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pais-Brito J., Rafols-Urquiza B., Gonzalez-Massieu L., Herrera-Perez M., Aciego-De Mendoza M., De Bergua Domingo J. Reduced patellofemoral and walking pain with mobile-bearing vs. fixed-bearing total knee replacements: a mid-term prospective analytic study. Acta Orthop Traumatol Turc. 2015;49(4):375–381. doi: 10.3944/AOTT.2015.14.0299. [DOI] [PubMed] [Google Scholar]
- 5.Ranawat C. History of total knee replacement. J South Orthop Assoc. 2001;11(4):218–226. [PubMed] [Google Scholar]
- 6.Helmy N., Anglin C., Greidanus N.V., Masri B.A. To resurface or not to resurface the patella in total knee arthroplasty. Clin Orthop Relat Res. 2008;466(11):2775–2783. doi: 10.1007/s11999-008-0420-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Breeman S., Campbell M., Dakin H. Patellar resurfacing in total knee replacement: five-year clinical and economic results of a large randomized controlled trial. J Bone Joint Surg Am. 2011;93(16):1473–1481. doi: 10.2106/JBJS.J.00725. [DOI] [PubMed] [Google Scholar]
- 8.Metsna V., Vorobjov S., Martson A. Prevalence of anterior knee pain among patients following total knee arthroplasty with nonreplaced patella: a retrospective study of 1778 knees. Medicina (Kaunas, Lithuania) 2014;50(2):82–86. doi: 10.1016/j.medici.2014.06.001. [DOI] [PubMed] [Google Scholar]
- 9.Holt G., Miller N., Kelly M., Leach W. Retention of the patella in total knee arthroplasty for rheumatoid arthritis. Jt Bone Spine. 2006;73(5):523–526. doi: 10.1016/j.jbspin.2005.11.017. [DOI] [PubMed] [Google Scholar]
- 10.Robertsson O., Dunbar M., Pehrsson T., Knutson K., Lidgren L. Patient satisfaction after knee arthroplasty: a report on 27,372 knees operated on between 1981 and 1995 in Sweden. Acta Orthop Scand. 2000;71(3):262–267. doi: 10.1080/000164700317411852. [DOI] [PubMed] [Google Scholar]
- 11.Hanssen A.D. Bone-grafting for severe patellar bone loss during revision knee arthroplasty. J Bone Joint Surg Am. 2001;83(2):171. doi: 10.2106/00004623-200102000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Deehan D.J., Phaltankar P.M., Pinder I.M. Do we need to replace the patella in knee arthroplasty for rheumatoid disease? Acta Orthop Belg. 2008;74(4):478–482. [PubMed] [Google Scholar]
- 13.Parvizi J., Rapuri V.R., Saleh K.J., Kuskowski M.A., Sharkey P.F., Mont M.A. Failure to resurface the patella during total knee arthroplasty may result in more knee pain and secondary surgery. Clin Orthop Relat Res. 2005;438(1):191–196. doi: 10.1097/01.blo.0000166903.69075.8d. [DOI] [PubMed] [Google Scholar]
- 14.Feller J.A., Bartlett R.J., Lang D.M. Patellar resurfacing versus retention in total knee arthroplasty. J Bone Joint Surg Br. 1996;78(2):226–228. [PubMed] [Google Scholar]
- 15.Shoji H., Yoshino S., Kajino A. Patellar replacement in bilateral total knee arthroplasty. A study of patients who had rheumatoid arthritis and no gross deformity of the patella. J Bone Joint Surg Am. 1989;71(6):853–856. [PubMed] [Google Scholar]
- 16.Kon E., Altadonna G., Filardo G., Matteo B.D., Marcacci M. Knee scoring systems. In: Bentley G., editor. European Surgical Orthopaedics and Traumatology. Springer; Berlin: 2014. pp. 3371–3388. [Google Scholar]
- 17.Wolfe F., Kong S.X. Rasch analysis of the Western Ontario MacMaster questionnaire (WOMAC) in 2205 patients with osteoarthritis, rheumatoid arthritis, and fibromyalgia. Ann Rheum Dis. 1999;58(9):563–568. doi: 10.1136/ard.58.9.563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kujala U.M., Jaakkola L.H., Koskinen S.K., Taimela S., Hurme M., Nelimarkka O. Scoring of patellofemoral disorders. Arthroscopy. 1993;9(2):159–163. doi: 10.1016/s0749-8063(05)80366-4. [DOI] [PubMed] [Google Scholar]
- 19.Kramers-de Quervain I.A., Engel-Bicik I., Miehlke W., Drobny T., Munzinger U. Fat-pad impingement after total knee arthroplasty with the LCS A/P-Glide system. Knee Surg Sport Traumatol Arthrosc. 2005;13(3):174–178. doi: 10.1007/s00167-004-0492-x. [DOI] [PubMed] [Google Scholar]
- 20.Ma H.M., Lu Y.C., Kwok T.G., Ho F.Y., Huang C.Y., Huang C.H. The effect of the design of the femoral component on the conformity of the patellofemoral joint in total knee replacement. J Bone Joint Surg Br. 2007;89(3):408–412. doi: 10.1302/0301-620X.89B3.18276. [DOI] [PubMed] [Google Scholar]
- 21.Nizard R.S., Biau D., Porcher R. A meta-analysis of patellar replacement in total knee arthroplasty. Clin Orthop Relat Res. 2005;432(3):196–203. doi: 10.1097/01.blo.0000150348.17123.7f. [DOI] [PubMed] [Google Scholar]
- 22.Pakos E.E., Ntzani E.E., Trikalinos T.A. Patellar resurfacing in total knee arthroplasty. A meta-analysis. J Bone Joint Surg Am. 2005;87(7):1438–1445. doi: 10.2106/JBJS.D.02422. [DOI] [PubMed] [Google Scholar]
- 23.Pavlou G., Meyer C., Leonidou A., As-Sultany M., West R., Tsiridis E. Patellar resurfacing in total knee arthroplasty: does design matter? A meta-analysis of 7075 cases. J Bone Joint Surg Am. 2011;93(14):1301–1309. doi: 10.2106/JBJS.J.00594. [DOI] [PubMed] [Google Scholar]
- 24.Patel K., Raut V. Patella in total knee arthroplasty: to resurface or not to–a cohort study of staged bilateral total knee arthroplasty. Int Orthop. 2011;35(3):349–353. doi: 10.1007/s00264-010-1063-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.He J.Y., Jiang L.S., Dai L.Y. Is patellar resurfacing superior than nonresurfacing in total knee arthroplasty? A meta-analysis of randomized trials. Knee. 2011;18(3):137–144. doi: 10.1016/j.knee.2010.04.004. [DOI] [PubMed] [Google Scholar]
- 26.Swan J.D., Stoney J.D., Lim K., Dowsey M.M., Choong P.F. The need for patellar resurfacing in total knee arthroplasty: a literature review. ANZ J Surg. 2010;80(4):223–233. doi: 10.1111/j.1445-2197.2010.05242.x. [DOI] [PubMed] [Google Scholar]
- 27.Bhan S., Malhotra R., Eachempati K.K. Total knee arthroplasty without patellar resurfacing in patients with rheumatoid arthritis. Clin Orthop Relat Res. 2006;450(9):157–163. doi: 10.1097/01.blo.0000229277.74194.bf. [DOI] [PubMed] [Google Scholar]
- 28.Biau D., Mullins M.M., Judet T., Piriou P. Mobile versus fixed-bearing total knee arthroplasty: mid-term comparative clinical results of 216 prostheses. Knee Surg Sport Traumatol Arthrosc. 2006;14(10):927–933. doi: 10.1007/s00167-006-0070-5. [DOI] [PubMed] [Google Scholar]
- 29.Picetti G.d., McGann W., Welch R. The patellofemoral joint after total knee arthroplasty without patellar resurfacing. J Bone Joint Surg Am. 1990;72(9):1379–1382. [PubMed] [Google Scholar]
- 30.Fern E., Winson I., Getty C. Anterior knee pain in rheumatoid patients after total knee replacement. Possible selection criteria for patellar resurfacing. Bone Joint J. 1992;74(5):745–748. doi: 10.1302/0301-620X.74B5.1527126. [DOI] [PubMed] [Google Scholar]
- 31.Bourne R.B. To resurface the patella or not? Better assessments needed to address the benefits for total knee replacement: commentary on an article by George Pavlou, BSc, MRCS, et al.: “Patellar resurfacing in total knee arthroplasty: does design matter? A meta-analysis of 7075 cases”. J Bone Joint Surg Am. 2011;93(14):e82. doi: 10.2106/JBJS.K.00308. [DOI] [PubMed] [Google Scholar]
- 32.Levitsky K.A., Harris W.J., Mcmanus J., Scott R.D. Total knee arthroplasty without patellar resurfacing: clinical outcomes and long-term follow-up evaluation. Clin Orthop Relat Res. 1993;286:116–121. [PubMed] [Google Scholar]
- 33.Peng C.W., Tay B.K., Lee B.P. Prospective trial of resurfaced patellaversus non-resurfaced patella in simultaneous bilateral total knee replacement. Singapore Med J. 2003;44(7):347–351. [PubMed] [Google Scholar]