Abstract
Ageing population is now a global challenge, where physical deterioration is the common feature in elderly people. In addition, the diseases, such as spinal cord injury, stroke, and injury, could cause a partial or total loss of the ability of human locomotion. Thus, assistance is necessary for them to perform safe activities of daily living. Robotic hip exoskeletons are able to support ambulatory functions in elderly people and provide rehabilitation for the patients with gait impairments. They can also augment human performance during normal walking, loaded walking, and manual handling of heavy-duty tasks by providing assistive force/torque. In this article, a systematic review of robotic hip exoskeletons is presented, where biomechanics of the human hip joint, pathological gait pattern, and common approaches to the design of robotic hip exoskeletons are described. Finally, limitations of the available robotic hip exoskeletons and their possible future directions are discussed, which could serve a useful reference for the engineers and researchers to develop robotic hip exoskeletons with practical and plausible applications in geriatric orthopaedics.
The translational potential of this article
The past decade has witnessed a remarkable progress in research and development of robotic hip exoskeletons. Our aim is to summarize recent developments of robotic hip exoskeletons for the engineers, clinician scientists and rehabilitation personnel to develop efficient robotic hip exoskeletons for practical and plausible applications.
Keywords: Ageing population, Gait rehabilitation, Hip dysfunction, Human performance augmentation, Robotic hip exoskeletons
Introduction
Most countries are reported with rising life expectancy and therefore a rapid increase in ageing population worldwide. Elderly people normally have physical deterioration and frailty, which imposes a heavy burden on the social health care system. The decreased physical capabilities owing to deterioration of neuromusculoskeletal system makes elderly people walking with a changed gait pattern and more cautious [1]. They generally have increased step variability and metabolic cost of walking, lower walking speed, shorter step-length, and reduced range of motion of the ankle, knee, and hip joints [2,3]. In addition, the elderly people have difficulties in maintaining trunk stability and have a risk of falls [4]. The lower limbs dysfunction and gait impairments are also common in elderly people, which could cause unnatural gait patterns [5,6]. Nearly three-quarters of all strokes occur in people over the age of 65 years. All those could reduce the mobility of elderly people and lead them to fewer independent lives and poor quality of life.
In addition, the patients with neurological disorders caused by diseases or injuries such as a stroke and spinal cord injury generally have muscle weakness, which could lead to insufficient force/torque at the hip joints during human locomotion [7]. These individuals often have decreased capacities of self-balancing and increased falling risk [8]. Therefore, approaches that can help elderly people and these patients to maintain a good walking pattern are desirable [9]. The past decade has witnessed a remarkable progress in research and development (R&D) of wearable medical devices for the patients with gait impairments [10]. The use of wearable medical devices such as robotic exoskeletons [11] and active orthoses [12] have become one of the most promising approaches to assist the individuals with gait disorders. It is predicted by a researcher that robotic exoskeletons would be commonly used in the community by 2024 [13].
Robotic hip exoskeletons integrate the robot power and human intelligence, and they can provide controllable assistive force/torque at the wearers' hip joints with an anthropomorphic configuration. One application of robotic hip exoskeletons is on gait rehabilitation. They are able to train the wearers’ muscles and assist their movements for therapeutic exercise. The robot-assisted rehabilitation can release therapists from the heavy burden of rehabilitation training and provide long training sessions for the patients with good consistency. Human regular walking is able to reduce the risk of strokes and coronary heart disease, and hence to improve the physical and mental health [14]. Thus, it is promising to make human walking more efficient. Human effort is related to metabolic expenditure, and the other application of robotic hip exoskeletons is to augment human performance such as increasing the human strength and endurance.
By comparing with the human ankle joint, the hip joint needs higher metabolic cost for the generation of similar mechanical joint power owing to the differences in muscle characteristics [15]. Therefore, in addition to the robotic ankle exoskeletons developed for metabolic benefit [16], the hip joint actuating is also a promising strategy because large positive torque is provided by the human hip during the activities of daily living [17]. Robotic hip exoskeletons also have the potential to integrate into the factories. In warehouses and manufacturing environments, the workers often have to handle heavy goods, which could load their lumbar spine and increase the risk of physical injury such as low back pain and other work-related musculoskeletal disorders [18,19]. The work-related injuries could have a serious impact on the quality of life of these individuals. Robotic hip exoskeletons are able to assist these workers during manual handling of heavy-duty tasks.
The aim of this article is to review the aspects of engineering design and control strategies of robotic hip exoskeletons for the two applications, i.e., gait rehabilitation and human performance augmentation, and to discuss some possible future directions to improve the currently available robotic hip exoskeletons. We hope this review would provide useful information for the engineers and researchers to design desirable robotic hip exoskeletons, especially for those new to this field and would like to make contributions to this important multidisciplinary biomedical engineering and orthopaedic rehabilitation filed.
In this article, the biomechanics of the human hip joint and pathological gait of individuals with hip dysfunction are first presented before reviewing the mechanical structure, actuators, sensors, and control strategies of the existing robotic hip exoskeletons. Finally, this article discusses the limitations of the available robotic hip exoskeletons and their possible R&D directions with respect to clinical applications.
Biomechanics of human hip and pathological gait
To increase adaptability and achieve minimal interference, bioinspired design of robotic hip exoskeletons is required. This section presents a brief description of biomechanics of the human hip joint and the pathological gait pattern of individuals with hip dysfunction, which provides a basis for the design and control of robotic hip exoskeletons.
Biomechanics of normal human hip joint
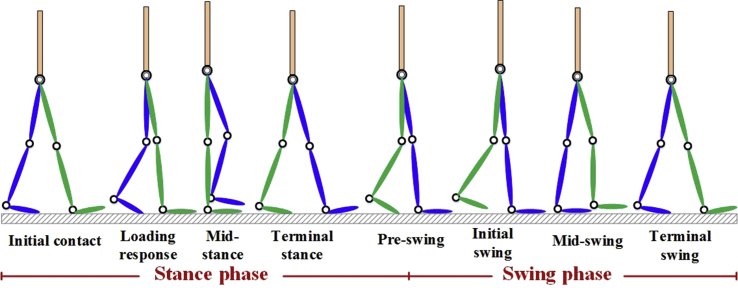
The human hip joint is a ball-and-socket joint and joins the pelvis to the femur. It is composed of the cup-shaped acetabulum and femoral head, which are connected and supported by several tissues and muscles [20,21]. In human locomotion analysis, the human hip behaves as a spherical joint with three degrees of freedom (DOFs), i.e., flexion/extension, abduction/adduction, and internal/external rotation. A human gait cycle is defined as a sequence of movements during walking and is basically composed of the alternating stance phase and swing phase [22], as shown in Fig. 1. According to the gait analysis of people with a normal gait pattern [23], the human hip joint will generate positive work to bear the body weight, propel the body forward, and stabilize the trunk during the period of 0–35% of a gait cycle. After this phase, the hip joint angle will cross the zero degree and the leg will become vertical.
Fig. 1.
Normal gait cycle. The green lines represent the right leg, and the blue lines represent the left leg. The gait cycle is composed of the alternating stance phase and swing phase, and it starts when one foot contacts the ground and ends when the same foot contacts the ground again.
Then, the tendons and muscle fascia of the hip joint will stretch and absorb and dissipate the energy by providing negative work. The significant negative work generated at terminal stance is for resisting gravity, raising the body centre of gravity, and propelling the body forward. At preswing, positive work will be generated from the hip joint to lift the leg and swing it forward. During the single-leg stance phase when the hip joint is loaded, the cup-shaped acetabulum will have some deformation to increase the contact area, which can reduce the pressure to protect the joint [24]. During the swing phase, the hip joint will provide large power to raise the leg and swing it forward. According to the clinical gait analysis results [23], the human hip joint angles and torques during a gait cycle with a normal gait pattern are shown in Fig. 2.
Fig. 2.
The human hip joint angles and torques during a gait cycle with a normal gait pattern. The stance phase is from 0% to 62% of a gait cycle, and the swing phase is from 62% to 100% of a gait cycle. (A) Hip joint angle; (B) hip joint torque.
Pathological gait pattern
Pathological gait patterns can be observed in elderly people and patients who have gait disorders. The gait of elderly people, especially those with lower limb disabilities such as osteoarthritis [25] and avascular necrosis of the hip [26], is different from a normal gait pattern. Elderly people normally have plantar flexor muscle weakness, which could lead to a reduction of the push-off power [27]. During the stance phase, a reduction of the push-off power of elderly people could affect trunk stabilization and trunk progression, which could cause a shorter step-length [28,29]. In addition, a low plantar flexor power-burst could affect the swing initiation. In general, the hip musculature of these people could increase the power output for compensation [30]. For the elderly people with muscle weakness at the hip joint or with hip joint stiffness, the human plantar flexors that can generate compensatory movements are significant important to realize a walking motion [31]. However, these compensatory movements could decrease the physical activity of these people, which have negative effects on their physical and mental health.
Metabolic cost is an important factor to evaluate human gait performance [32]. Elderly people normally have higher metabolic cost during walking as compared with that of young-to-middle-aged people [3]. Thus, it is essential to develop some strategies for the improvement of gait performance and metabolic efficiency of elderly people. Researches in [33,34] demonstrated that therapeutic exercises could benefit elderly people by improving their gait function and metabolic efficiency. Walking is a near-perfect locomotion [35], which is more attractive to elderly people than many other physical activities such as running and jumping because it is a familiar and convenient locomotion [36]. Robot-assisted therapy with high-dosage and high-intensity training is promising for compensating gait impairments. Therefore, robotic hip exoskeletons that can improve gait function and metabolic cost are desirable by and designed for the elderly people. In addition to elderly people, especially the individuals suffering from neurological disorders also need the assistance from robotic hip exoskeletons to compensate for the decreased muscle strength at the hip joints during human locomotion [37,38].
Category of robotic hip exoskeletons
A robotic hip exoskeleton is mainly composed of the mechanical structure, actuator, multisensor system, controller, and power source, as shown in Fig. 3. Robotic hip exoskeletons are primarily developed for two types of applications. One application is focused on gait rehabilitation for elderly people and individuals with gait impairments [37,38]. The other is on human performance augmentation, enhancing the physical abilities of healthy individuals during normal walking [21], loaded walking [39], and manual handling of heavy goods [40,41].
Fig. 3.
Essential components of a robotic hip exoskeleton. The essential components include the mechanical structure for transferring assistive force/torque, actuator for generating assistive force/torque, multisensor system for motion data collection, controller for controlling the exoskeleton, and power source for providing power for the exoskeleton.
Robotic hip exoskeletons for gait rehabilitation
Owing to the physical deterioration and frailty, the elderly people could have pathological gait patterns. In addition, the patients with a stroke, spinal cord injury, and other related diseases or injuries could have muscle weakness at the hip joints, which can seriously affect their gait performance. Robotic hip exoskeletons developed for therapeutic purposes are able to assist individuals with hip disabilities by providing controllable assistance at the wearers’ hip joints.
Lee et al [38,42] developed a robotic hip exoskeleton named GEMS for the rehabilitation of post-stroke patients and for the elderly people to improve their gait function and muscle effort. It has two active DOFs (flexion/extension) and two passive DOFs (abduction/adduction). The active DOFs are actuated by electric motors that can output a maximum torque of 12 Nm. Electric motors are the most commonly used actuators in robotic hip exoskeletons owing to their reliability, low noise, high efficiency, control precision, and torque-to-weight ratio. The electric components such as the embedded controller and battery are placed at the back of the exoskeleton. The GEMS has a weight of 2.8 kg in total. Experiments with 30 elderly persons were performed. The testing results showed that the exoskeleton could improve the wearer's gait function, decrease the muscle effort, and reduce the metabolic cost of walking.
An active pelvis orthosis named APO (Fig. 4A) was developed for the motion assistance of elderly people with gait impairments by Giovacchini et al [43]. Compliant elements have been introduced into the actuation system, and series elastic actuators (SEAs) have been developed for the APO. The SEA is composed of an electric motor, a custom torsional spring, a harmonic drive, and a four-bar mechanism. SEAs have the advantages of low intrinsic output impedance, high force fidelity and back-drivability, good force control bandwidth, and capability of storing energy in the flexible elements [44]. The APO has four DOFs in total. The DOFs in flexion/extension are active, and the DOFs in abduction/adduction are passive. The APO weighs about 4.2 kg, excluding the off-board components such as the control unit. The wearer's shoulder bears a part of the exoskeleton weight by two straps. Tests with a healthy individual was conducted, and the testing results demonstrated that a smooth assistive torque could be provided for the wearer's hip joints in flexion/extension by the exoskeleton.
Fig. 4.
Robotic hip exoskeletons for gait rehabilitation. (A) The robotic hip exoskeleton APO actuated by SEAs that comprise electric motors, custom torsional springs, harmonic drive, and a four-bar mechanism (Image credit: Elsevier); (B) the robotic hip exoskeleton actuated by electric motors through flexible Bowden cable transmission (Image credit: Professor Wang of the Southeast University, Nanjing, China).
Researchers in Honda R&D Corporation of Japan also developed a robotic hip exoskeleton named SAS for the patients with gait impairments and for the elderly people to improve the gait performance [[45], [46], [47]]. The exoskeleton weighs about 2.4 kg, and assistance in flexion/extension can be provided with electrical actuators. Experiments in 15 elderly individuals were conducted, and the experimental results demonstrated that the SAS could improve the walking performance and muscle activity efficiency of the elderly people. Wu et al [48] developed a robotic hip exoskeleton named PH-EXOS (Fig. 4B) to provide motion assistance for the individuals with walking impairments. The PH-EXOS weighs about 3.5 kg and has six DOFs in total. The active DOFs (flexion/extension) are actuated by electric motors through flexible Bowden cable transmission. The Bowden cable actuation has the advantages of simplicity, remote transmission, and dexterity [49]. The DOFs in internal/external rotation and abduction/adduction are passive. Experiments with a healthy individual were conducted, and the experimental results showed that the exoskeleton was able to provide walking assistance and reduce the wearer's muscular power consumption.
A robotic hip exoskeleton was developed to assist the patients with muscles weakness by Ryder [50]. The exoskeleton has one DOF in flexion/extension and is actuated by an SEA. The actuator is inherently cyclic and is composed of an electric motor, a worm gear, the scotch-yoke mechanism, and springs. It can output a peak active torque of 44 Nm. Zhang et al [51] developed a robotic hip exoskeleton named NREL-Exo that could provide walking and balance assistance in human locomotion for the individuals with muscular weakness. The NREL-Exo has a total of four DOFs, including hip flexion/extension and hip abduction/adduction. All the DOFs are active and are actuated by SEAs. The SEA is composed of an electric motor, a torsion spring, and a harmonic drive. It can output a continuous torque of 40 Nm. The exoskeleton weighs about 9.2 kg, excluding the power source.
Robotic hip exoskeletons for human performance augmentation
Researches have demonstrated that the human hip joint plays a significant role in the provision of high mechanical power during a gait cycle, which is up to 45% [52]. Thus, in addition to the robotic hip exoskeletons with rehabilitation application, they are also developed for the purposes of human performance augmentation.
A robotic hip exoskeleton was developed to increase the mobility of the wearers’ hip joints and reduce their metabolic cost during walking by van Wijdeven [21]. The exoskeleton is composed of the waist part, two thigh parts, and two leaf springs. It has four DOFs in total. The leaf springs are designed to be parallel to the human leg to capture the negative work that an individual does during a gait cycle. The exoskeleton has a weight of 4.15 kg. Treadmill gait trials with a healthy individual were conducted. The testing results validated the effectiveness of the exoskeleton to reduce the energetic cost of human walking.
A kinematically compatible hip exoskeleton was developed to reduce the wearer's metabolic consumption during the sit-to-stand motion by Junius et al [53,54]. The exoskeleton structure includes a misalignment compensation mechanism, a parallel spring mechanism, two hip joints, and torso and thigh braces. The misalignment compensation mechanism is able to compensate the misalignment between the exoskeleton and the wearer, and the parallel spring mechanism can provide a flexion/extension assistive torque for the wearers to reduce their metabolic consumption. The exoskeleton has six DOFs in total and allows hip flexion/extension, abduction/adduction, and internal/external rotation. It weighs about 5 kg. Sit-to-stand experiments were conducted in four healthy individuals, and the experimental results demonstrated the effectiveness of the exoskeleton to reduce the wearer's metabolic consumption.
Kang et al [55] developed a robotic hip exoskeleton (Fig. 5A) to reduce the metabolic cost of healthy individuals during walking. The exoskeleton weighs about 7 kg and is actuated by two SEAs. The SEA, which is able to provide a peak torque of 60 Nm, is composed of an electric motor, a timing belt transmission, a ball screw transmission, and a fiberglass leaf spring. Experiments were conducted in 10 able-bodied individuals. The results demonstrated a U-shaped trend between the exoskeleton assistance and the wearer's metabolic cost. Chen et al [40,41] developed a robotic hip exoskeleton (Fig. 5B) for assisting hip flexion and extension movements of individuals with heavy-duty tasks, especially for the assistance of lift movement. The exoskeleton is actuated by two SEAs that can generate a peak torque of 22 Nm. The control electronics of the exoskeleton are placed at the backpack. Experiments were conducted in 15 healthy individuals, and the experimental results showed that the exoskeleton could reduce the wearer's electromyography (EMG) activities of back muscles during the lift action.
Fig. 5.
Robotic hip exoskeletons for human performance augmentation. (A) The robotic hip exoskeleton developed for reducing the metabolic cost of healthy individuals during walking (Image credit: Professor Kang of the Georgia Institute of Technology, Atlanta, GA, USA); (B) the robotic hip exoskeleton developed for assisting individuals with heavy-duty tasks, especially for the assistance of lift movement (Image credit: Professor Chen of the BioRobotics Institute, Scuola Superiore Sant’Anna, Pisa, Italy).
Masood et al [56,57] developed a robotic hip exoskeleton for the able-bodied individuals with manual handling activities. The exoskeleton has a total of 12 DOFs. Among these DOFs, the hip flexion/extension is active, whereas the rest DOFs, including the hip abduction/adduction, hip elongation, and three DOFs in the thigh/torso attachment, are passive. The active DOFs are actuated by two parallel elastic actuators (PEAs) with a calculated output torque of about 53.76 Nm. Each PEA is comprised of an electric motor, a harmonic drive, and the parallel natural rubber elements. As compared with SEAs, PEAs have the advantages of reducing the peak power, energy, and torque [58]. The estimated weight of the exoskeleton is about 11.6 kg. Virtual testing was conducted, and the testing results demonstrated that the PEA increased the peak torque and peak power by 50% and 40% during the lowering and lifting scenarios, respectively.
Sensors selection of robotic hip exoskeletons
Motion data collection of the human–exoskeleton system is significantly important because it is essential for the feedback control and performance evaluation of robotic hip exoskeletons. Multiple sensors, including the kinematic, kinetic, and bioelectric sensors, are normally used in robotic hip exoskeletons to measure the motion data. Kinematic sensors are used to measure the kinematic data such as the joint angle and joint angular velocity; kinetic sensors are used to measure the kinetic data such as the joint torque and ground reaction forces; and bioelectric sensors are used to measure the bioelectric data such as the wearer's surface EMG signals.
Kinematic data collection
Most commonly, angular sensors such as encoders [43] and potentiometers [48] are used to measure the joint angles and angular velocity of robotic hip exoskeletons, which are basic information for the exoskeleton control. In Ryder's work [50], two rotary incremental encoders are used to measure the displacement between the link of the leg and the worm wheel, which can be used to calculate the interaction forces. Many, but not all, inertial measurement units (IMUs) are also used in the multisensor system of robotic hip exoskeletons to obtain more kinematic data of the human–exoskeleton system [40,55,57]. In the research of Lee et al [37], an IMU is placed at the back of the exoskeleton to estimate the wearer's walking speed.
Kinetic data collection
For robotic hip exoskeletons powered by SEAs, compliant elements such as springs [43,51] are generally implemented into the actuators. The compliant elements are able to reduce the exoskeleton mechanical impedance. Absolute encoder [43] and strain gauges [55] can be used to measure the deformation of the spring. With the information of the spring stiffness, the actuators output torque can be calculated. Other sensors such as the current sensor [46], Hall effect sensor [55], force sensing resistor (FSR) sensor [55], and torque sensor are used [51] in robotic hip exoskeletons. In the research of Shimada et al [46], the current sensors are used to measure the information of electric current, which can be used to calculate the generated torque. In the research of Wu et al [48], the FSR sensors are used to measure the human–exoskeleton interaction forces, and the wearer's motion intention can be recognized by measuring the pressure information on the thigh by the FSR sensors.
Metabolic cost measurement
To date, the standard for performance evaluation of the robotic hip exoskeletons with the application of augmenting human performance has not been established. Most researchers measure the wearer's metabolic cost of walking or loaded walking and use it as the metric to evaluate the performance of the exoskeletons. Therefore, the EMG sensors, cardiopulmonary metabolic system, and motion capture system are generally used to measure the wearer's muscle activity and oxygen consumption [37]. In the tests conducted by van Wijdeven [21], EMG signals from the individual's hip muscles are measured by a Delsys Bagnoli system and EMG electrodes. The individual's oxygen and carbon dioxide flow are measured to evaluate the metabolic cost by a mobile Oxycon open-circuit spirometry system. In addition, a Visualeyez system with two sets of cameras is used to measure the kinematic data, and a split-belt force-sensing treadmill is used to measure the kinetic data such as the ground reaction forces.
Control strategies of robotic hip exoskeletons
During the development of robotic hip exoskeletons, control strategy is a fundamental issue. With suitable control approaches, robotic hip exoskeletons can generate the assistive torques as needed for the wearers, and the hip joints of the human–exoskeleton system can share the same motions in a comfortable and safe mode. Up to now, different control strategies have been adopted for robotic hip exoskeletons.
Force/torque-based control
The force/torque control is one of the most common control approaches adopted in robotic hip exoskeletons. With this control strategy, the exoskeleton actuators are normally regulated to follow the desired torques so as to ensure the assistance of the wearers.
A hierarchical architecture control system is proposed for the robotic hip exoskeleton developed by Giovacchini et al [43], which includes a high-level controller and a low-level controller. The low-level controller is to regulate the actuator to follow a desired torque with proportional-integral-derivative (PID) regulator, and the high-level controller is responsible for generating the torque references. For the robotic hip exoskeleton developed by Young et al [55,59], the control system includes the high-, mid-, and low-level layers. The high-level is responsible for estimating the wearer's gait phases, the mid-level layer is to dictate the dynamic performance of the exoskeleton, and the low-level layer is to regulate the actuator to follow the desired torque. In their research, the best assistance timing of the exoskeleton to reduce the wearer's metabolic cost of walking is determined.
Impedance/admittance control
Physical interactions exist in the human–exoskeleton system, and it is essential to provide the assistive torque as needed for the wearers. The impedance/admittance control is another commonly used control approaches in robotic hip exoskeletons. It is an assist-as-needed control strategy that can generate the complementary part of the torque needed for the wearers to complete a movement.
In the research of Nagarajan et al [60], the integral admittance shaping algorithm was proposed to control the robotic hip exoskeleton. With this control method, a desired shape for the frequency response magnitude can be obtained and the desired dynamic response of the human–exoskeleton system can be achieved. Lee et al [61] proposed a switching admittance–position control method for the robotic hip exoskeleton, which took the advantages of both admittance and position control. The admittance control with feedforward models is used during the assistive phase of the exoskeleton, and the controller is switched to the position control during the nonassistive phase. To assist walking and maintain walking stability, an adaptive admittance controller is used to control the robotic hip exoskeleton NREL-Exo [62]. The admittance controller considers the interaction torque between the wearer and the exoskeleton, and it is able to provide adaptive assistance torque for the wearer as needed.
EMG signal–based control
Human bioelectric signals such as EMG signals are related to the muscle activities and human locomotion [63]. EMG signal–based control has also been used to control the robotic hip exoskeletons. The EMG signals can be used to establish a link between the exoskeleton torques and the phases of a gait cycle [64,65].
Grazi et al [66,67] developed an EMG-based assistive control strategy for the robotic hip exoskeleton. The wearer's motion intention can be recognized based on the EMG activity from the gastrocnemius medialis, which is measured by the pre-gelled bipolar Ag/AgCl surface electrodes. Then, the exoskeleton is accordingly controlled to provide the required assistive torque. In the research of Young et al [68], a proportional myoelectric controller was developed for the robotic hip exoskeleton, which used the EMG signals of the wearer's muscles to generate the proportional control signal. The EMG signals of rectus femoris are used for the activation of hip flexion assistance, and the hip extension assistance is activated based on the EMG signals of gluteus maximus.
Adaptive oscillator–based control
Based on the idea of the central pattern generator, the adaptive oscillator–based control has been developed for robotic hip exoskeletons, which can be conveniently implemented into robotic hip exoskeletons [69,70]. This controller makes the exoskeleton adjustable to different walking cadences and does not need additional sensors, estimation algorithms, or user-dependent calibration.
Giovacchini et al [43] proposed an adaptive assistive strategy for the robotic hip exoskeleton. The adaptive oscillators can track the periodicity characteristics such as amplitude and frequency of the input signals. The wearer's phase of a gait cycle can be learnt with the implementation of adaptive oscillators. Lenzi et al [65] proposed an assistive controller using adaptive frequency oscillators for the robotic hip exoskeleton. With this controller, the exoskeleton is able to estimate the wearer's walking cadence and the current percentage of stride in real-time, based on which the assistive torque can be provided at the wearer's hip joints. In the research of Lee et al [37,38], a particularly shaped adaptive oscillator was proposed for the robotic hip exoskeleton to estimate the gait state. The input of the controller is the hip joint angle, and the output is the assistive torque that is generated based on the walking speed, gait phase, and ground inclination.
Discussion
With the technological advancements of electronics, actuators, sensors, and batteries, remarkable progress has been achieved in the field of robotic hip exoskeletons in the past decade. Some of R&D has been made commercially available [71]. Table 1 summarizes the above-mentioned robotic hip exoskeletons. It can be seen that the actuators including electric motors, SEAs, PEAs, and Bowden cable actuation are designed and configured for robotic hip exoskeletons. Hydraulic servo rotary drive that can provide high power is also used in robotic hip exoskeletons [72]. To collect the motion data of the human–exoskeleton system for feedback control and performance evaluation, multiple sensors including the angle sensor, force sensor, torque sensor, IMU, current sensor, Hall effect sensor, EMG sensor, and some systems such as cardiopulmonary metabolic system, motion capture system, split-belt force-sensing treadmill, heart rate monitor have been used in robotic hip exoskeletons. Experimental studies [[37], [38], [39], [40], [41]] have demonstrated the effectiveness of gait rehabilitation and human performance augmentation of robotic hip exoskeletons.
Table 1.
Overview of the above-mentioned robotic hip exoskeletons.
| Devices | Application | Actuator | Maximum applied force/torque | Motion data collection | Control strategy | Weight, kg |
|---|---|---|---|---|---|---|
| GEMS [31,38] | Gait rehabilitation | Electric motor | 12 Nm | IMU, cardiopulmonary metabolic system, EMG sensor, motion capture system | Torque control + adaptive oscillator–based control | 2.8 |
| APO [43] | Gait rehabilitation | SEAs | NA | Encoders | Torque control + adaptive oscillator–based control | 4.2* |
| SAS [[45], [46], [47]] | Gait rehabilitation | Electric motor | NA | Angular sensor, current sensor | NA | 2.4 |
| PH-EXOS [48] | Gait rehabilitation | Bowden cable actuation | NA | Potentiometer, FSR sensor | NA | 3.5 |
| RHE by Ryder et al [50] | Gait rehabilitation | SEA | 44 Nm | Encoder | Torque control | NA |
| NREL-EXO [51] | Gait rehabilitation | SEA | 40 Nm | Encoders, force sensor, torque sensor | NA | 9.2* |
| RHE by van Wijdeven [21] | Human performance augmentation | NA | NA | EMG sensor, mobile Oxycon open-circuit spirometry system, Visualeyez system, split-belt force-sensing treadmill | NA | 4.15 |
| RHE by Junius et al [53,54] | Human performance augmentation | NA | NA | CORTEX METAMAX 3B breath-by-breath analysis system, heart rate monitor, EMG sensor, motion analysis system | NA | 5 |
| RHE by Kang et al [55] | Human performance augmentation | SEA | 60 Nm | Hall effect sensor, strain gauge, encoder, FSR sensor, IMU, Oxycon mobile system, split-belt instrumented treadmill | Torque control | 7 |
| RHE by Chen et al [40,41] | Human performance augmentation | SEA | 22 Nm | Encoder, IMU | Torque control | NA |
| RHE by Masood et al [56,57] | Human performance augmentation | PEA | 53.76 Nm | Encoder, IMU | NA | 11.6 |
*The weight of the RHE excluding the off-board components.
EMG = electromyography; IMU = inertial measurement unit; NA = the information is not available; PEA = parallel elastic actuator; RHE = robotic hip exoskeleton; SEA = series elastic actuator.
Limitations of existing robotic hip exoskeletons
The robotic hip exoskeletons still do not meet the desired applications, and various technological challenges should be met to address the limitations or overcome the technical barriers. Most currently available robotic hip exoskeletons have the disadvantages of bulk and complexity of learning to use them friendly. Some of them are tethered with off-board components such as power source, which could limit the wearers' areas of activity and are not suitable for daily use. In addition, the wearers have to perform activities of daily living within a certain area owing to the exoskeleton-limited operating-time, which is affected by the battery capacity and the energy efficiency of actuators. Owing to the deformations of the wearer's soft tissue, the robotic hip exoskeleton could slip during its operation, which could cause misalignment between the wearer and the exoskeleton. The misalignment could lead to additional constraints, and then it could cause discomfort and pain for the wearer. Another limitation of the existing robotic hip exoskeletons is related to the human trails. Regarding robotic hip exoskeletons for rehabilitation, the current researches predominantly adopt crossover trials to evaluate the immediate effects with a small sample size. Effects of long-term use of robotic hip exoskeleton has not yet investigated as well.
Possible R&D directions of robotic hip exoskeletons
For gait rehabilitation application, the ideal robotic hip exoskeletons are expected to provide therapeutic benefits for the elderly people and individuals with hip dysfunction, which is a sound strategy to lead them to better independent lives and improving their physiological health. For the application of human performance augmentation, the ideal robotic hip exoskeletons shall enhance the wearers’ physical abilities and/or reduce their metabolic cost. Robotic hip exoskeletons are also promising for orthopaedics application [73,74]. For individuals with injuries or diseases at the hip, the compensatory movements of the ankle and knee joints, which could decrease their physical activity, can be avoided by wearing robotic hip exoskeletons. In addition, robotic hip exoskeletons can activate the circulatory and increase the bone mineral density of these patients. They have the potential to reduce osteoarthritis and assist the treatment of avascular necrosis of the hip. As summarized in Table 2, interdisciplinary collective efforts from the engineers, physical therapists, and clinicians should be focused on the following aspects for potentially wide future applications of robotic hip exoskeletons.
-
1.
Weight: When wearing robotic hip exoskeletons, the added mass and inertia to the wearers would contribute to increase their metabolic cost [75]. Thus, the exoskeletons are expected to be as light and compact as possible. The mechanical structure is one of the main factors that limit the weight of robotic hip exoskeletons. The materials with low density and high stiffness/strength are desirable for the mechanical structure. Aluminium alloy is normally used for the frame design to realize lightweight and high stiffness. Compared with aluminium alloy, the material titanium would be better for the mechanical structure of robotic hip exoskeletons in terms of strength and weight. However, it is much more expensive. The fibre-reinforced plastic is another suitable material for the frame design of the exoskeletons, e.g., the carbon fibre is lighter than the aluminium alloy. In addition, some smart materials such as shape memory alloys and/or shape memory polymers also promise their use in robotic hip exoskeletons for weight reduction, customization, and cost-effective.
-
2.
Actuator: The actuation system plays a significant role during the development of robotic hip exoskeletons because it generally affects the portability, output speed and force/torque, and efficiency of the exoskeletons. The actuators shall have the characteristics of lightweight, small volume, and high power-to-weight ratio. Efficient transmission mechanism should be designed to improve the system energy efficiency so as to prolong the exoskeleton operating-time at one charge of the battery. Compliant elements shall be implemented into the actuators to lower down the exoskeleton mechanical impedance owing to the physical interactions among the wearer, exoskeleton, and the ground. In addition to electric motors, SEAs, PEAs, Bowden cable actuation, and hydraulic servo rotary drive, other actuators containing smart materials such as magneto-rheological SEA [76] and piezoelectric motor [77] also promise their use in robotic hip exoskeletons.
-
3.
Human--machine interface: Physical interactions exist between the wearer and the exoskeleton, thus a user-friendly human–machine interface shall be designed for robotic hip exoskeletons. The exoskeletons are expected to be ease of use with good appearances. Misalignment compensation mechanism shall be designed with a compact and lightweight structure, and the metal frame can be designed with a combination of materials to transmit the energy. It is reported that decreasing the DOFs could restrict the range of motion, which has a negative effect on gait performances and increases human metabolic cost [78]. Thus, robotic hip exoskeletons would be better to be designed with three DOFs at each hip joint. A smooth information exchange between the wearer and exoskeleton shall be achieved with the multisensor system. Then, the exoskeleton could obtain enough information for feedback control, and the wearer could acquire the information on the exoskeleton working status. With the development of machine vision technology, machine vision is potentially promising for use in future robotic hip exoskeletons. The exoskeletons equipped with cameras or infrared sensors can detect changes of the environment, and then the control parameters can be modified accordingly to improve the exoskeleton intelligence.
-
4.
Control: Control strategies have significant effects on the performances of robotic hip exoskeletons. The assistance magnitude, assistance duration, and onset timing of assistance of robotic hip exoskeletons are key factors for the controller, and the exoskeleton joint angles and torques shall be online modified according to the wearer's gait speed, step-length, and other conditions. Safety should also be considered during the development of control algorithms. In addition, bioelectric signals of the human body, such as the EMG and electroencephalogram signals, can be used for the exoskeleton feedback control. However, the EMG signals will change owing to the fatigue, sweat, and sensor placement. The intramuscular EMG electrodes that can be powered wirelessly and have stable properties could be another choice, but the electrodes have to be placed in the human body and reside within the muscle. EMG-based and electroencephalogram-based technologies are promising for the robotic hip exoskeletons control if the limitations can be addressed. By using the large number of the wearer's physiological signals, the adoption of big data algorithms and machine learning techniques would be another novel direction of the intelligent control of robotic hip exoskeletons.
-
5.
Human trials: The rehabilitation process of individuals with gait disorders with robotic hip exoskeletons can be divided into several stages according to the user's physical conditions. It is necessary to train them to use the exoskeletons before conducting clinical trials in the inertial stage and certified physiotherapists should be engaged in all stages of trials to ensure the safety. Once the user take off the robotic hip exoskeleton for rehabilitation, the user's gait function may be improved after a long-term use. However, it also has the possibility of returning to the previous conditions after its discontinuation. Thus, parallel-group randomized controlled trials shall be conducted to validate the immediate effects and long-term effects on individuals with gait impairments. Instead of small and selected samples, a large number of pragmatic samples shall be recruited in clinical trials to verify the clinical and functional effects of robotic hip exoskeletons. Some important effects of using the exoskeletons should also be explored, such as the users' confidence and the effects of robotic hip exoskeletons on prevention of falls.
Table 2.
Aspects of robotic hip exoskeletons for improvement.
| Aspects | Goals | Approaches |
|---|---|---|
| Weight | Light, compact | Materials: low density, high stiffness/strength, e.g., aluminium alloy, titanium, carbon fibre, shape memory alloys, shape memory polymers |
| Actuator | Lightweight, small volume, high power-to-weight ratio | Efficient transmission mechanism Introducing compliant elements Introducing smart materials |
| Human–machine interface | User-friendly, intuitive and flexible | Misalignment compensation mechanism A combination of materials for frame design Three DOFs at each hip joint Smooth information exchange Introducing machine vision technology |
| Control | Adaptive, intelligent | Manual control Flexible controller Minimized lag Bioelectric signal–based control Big data algorithms |
DOFs = degrees of freedom.
Conclusion
With population ageing and increased number of patients with gait disorders, especially seeing in geriatric orthopaedics, robotic hip exoskeletons are desirable to provide assistive force/torque for the wearers, and accordingly, to improve their physical and mental health. Robotic hip exoskeletons are also promising for human performance augmentation during human normal walking, loaded walking, and manual handling of heavy goods. This article presented the human hip biomechanics and the pathological gait pattern of individuals with walking impairments, followed by the description of mechanical design, actuator design and configuration, sensors selection, and control strategy of the available robotic hip exoskeletons. Limitations of the existing robotic hip exoskeletons and their future R&D directions are discussed. To propel the acceptance and wide consumer adoption of robotic hip exoskeletons, multidisciplinary collaborations among engineers, kinesiologists, clinician scientists and rehabilitation personnel as well as industry and academia shall work together to develop cost-effective, user-friendly, and efficient robotic hip exoskeletons for various clinical applications.
Conflict of interest
The authors have no conflicts of interest to disclose in relation to this article.
Funding/support
This work was supported by the National Natural Science Foundation of China (Project No. 51805132), the China Postdoctoral Science Foundation Funded Project (Project No. 2018M642512), and the Fundamental Research Funds for the Central Universities (Project No. JZ2019HGTB0084, JZ2018HGBZ0166).
References
- 1.Maki B.E. Gait changes in older adults: predictors of falls or indicators of fear. J Am Geriatr Soc. 1997;45(3):313–320. doi: 10.1111/j.1532-5415.1997.tb00946.x. [DOI] [PubMed] [Google Scholar]
- 2.Soares D.P., de Castro M.P., Mendes E., Machado L. Influence of wedges on lower limbs' kinematics and net joint moments during healthy elderly gait using principal component analysis. Hum Mov Sci. 2014;38:319–330. doi: 10.1016/j.humov.2014.09.007. [DOI] [PubMed] [Google Scholar]
- 3.Fiser W.M., Hays N.P., Rogers S.C., Kajkenova O., Williams A.E., Evans C.M. Energetics of walking in elderly people: factors related to gait speed. J Gerontol A, Biol Sci Med Sci. 2010;65(12):1332–1337. doi: 10.1093/gerona/glq137. [DOI] [PubMed] [Google Scholar]
- 4.Menz H.B., Lord S.R., Fitzpatrick R.C. Acceleration patterns of the head and pelvis when walking on level and irregular surfaces. Gait Posture. 2003;18(1):35–46. doi: 10.1016/s0966-6362(02)00159-5. [DOI] [PubMed] [Google Scholar]
- 5.Stolze H., Klebe S., Baecker C., Zechlin C., Friege L., Pohle S. Prevalence of gait disorders in hospitalized neurological patients. Mov Disord. 2010;20(1):89–94. doi: 10.1002/mds.20266. [DOI] [PubMed] [Google Scholar]
- 6.Snijders A.H., van de Warrenburg B.P., Giladi N., Bloem B.R. Neurological gait disorders in elderly people: clinical approach and classification. Lancet Neurol. 2007;6(1):63–74. doi: 10.1016/S1474-4422(06)70678-0. [DOI] [PubMed] [Google Scholar]
- 7.Olney S.J., Richards C. Hemiparetic gait following stroke. Part I: characteristics. Gait Posture. 1996;4(2):136–148. [Google Scholar]
- 8.Chen G., Patten C., Kothari D.H., Zajac F.E. Gait differences between individuals with post-stroke hemiparesis and non-disabled controls at matched speeds. Gait Posture. 2005;22(1):51–56. doi: 10.1016/j.gaitpost.2004.06.009. [DOI] [PubMed] [Google Scholar]
- 9.Potter J.M., Evans A.L., Duncan G. Gait speed and activities of daily living function in geriatric patients. Arch Phys Med Rehabil. 1995;76(11):997–999. doi: 10.1016/s0003-9993(95)81036-6. [DOI] [PubMed] [Google Scholar]
- 10.Chen B., Ma H., Qin L.Y., Gao F., Chan K.M., Law S.W. Recent developments and challenges of lower extremity exoskeletons. J Orthop Transl. 2016;5:26–37. doi: 10.1016/j.jot.2015.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen B., Zhong C.H., Zhao X., Ma H., Guan X., Li X. A wearable exoskeleton suit for motion assistance to paralysed patients. J Orthop Transl. 2017;11:7–18. doi: 10.1016/j.jot.2017.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen B., Zi B., Wang Z.Y., Qin L., Liao W.H. Knee exoskeletons for gait rehabilitation and human performance augmentation: a state-of-the-art. Mech Mach Theory. 2019;134:499–511. [Google Scholar]
- 13.Ferris D.P. The exoskeletons are here. J NeuroEng Rehabil. 2009;6:17. doi: 10.1186/1743-0003-6-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Manson J.E., Hu F.B., Rich-Edwards J.W., Colditz G.A., Stampfer M.J., Willett W.C. A prospective study of walking as compared with vigorous exercise in the prevention of coronary heart disease in women. N Engl J Med. 1999;341(9):650–658. doi: 10.1056/NEJM199908263410904. [DOI] [PubMed] [Google Scholar]
- 15.Umberger B.R., Rubenson J. Understanding muscle energetics in locomotion: new modeling and experimental approaches. Exerc Sport Sci Rev. 2011;39(2):59–67. doi: 10.1097/JES.0b013e31820d7bc5. [DOI] [PubMed] [Google Scholar]
- 16.Chen B., Zi B., Zeng Y.S., Qin L., Liao W.H. Ankle-foot orthoses for rehabilitation and reducing metabolic cost of walking: possibilities and challenges. Mechatronics. 2018;53:241–250. [Google Scholar]
- 17.Eng J.J., Winter D.A. Kinetic analysis of the lower limbs during walking: what information can be gained from a three-dimensional model? J Biomech. 1995;28(6):753–758. doi: 10.1016/0021-9290(94)00124-m. [DOI] [PubMed] [Google Scholar]
- 18.Punnett L., Prüss-Ütün A., Nelson D.I., Fingerhut M.A., Leigh J., Tak S. Estimating the global burden of low back pain attributable to combined occupational exposures. Am J Ind. 2005;48(6):459–469. doi: 10.1002/ajim.20232. [DOI] [PubMed] [Google Scholar]
- 19.da Costa B.R., Vieira E.R. Risk factors for work-related musculoskeletal disorders: a systematic review of recent longitudinal studies. Am J Ind. 2010;53(3):285–323. doi: 10.1002/ajim.20750. [DOI] [PubMed] [Google Scholar]
- 20.Forner-Cordero A., Pons J.L., Turowska E.A., Schiele A. John Wiley & Sons, Ltd; 2008. Kinematics and dynamics of wearable robots. Wearable robots: biomechatronic exoskeletons; pp. 47–85. [Google Scholar]
- 21.van Wijdeven M.A.P. 2016. Design and evaluation of a passive hip exoskeleton to reduce the energy cost of human walking. Master Thesis, Mechanical Engineering, Delft University of Technology; pp. 13–50. [Google Scholar]
- 22.Dicharry J. Kinematics and kinetics of gait: from lab to clinic. Clin Sports Med. 2010;29(3):347–364. doi: 10.1016/j.csm.2010.03.013. [DOI] [PubMed] [Google Scholar]
- 23.Winter D.A. 4th ed. John Wiley & Sons; Hoboken, NJ, USA: 2009. Biomechanics and motor control of human movement. [Google Scholar]
- 24.Radin E.L. Biomechanics of the human hip. Clin Orthop Relat Res. 1980;152:28–34. [PubMed] [Google Scholar]
- 25.Kong L., Zheng L.Z., Qin L., Ho K.W. Role of mesenchymal stem cells in osteoarthritis treatment. J Orthop Transl. 2017;9:89–103. doi: 10.1016/j.jot.2017.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cao H.J., Guan H.F., Lai Y.X., Qin L., Wang X.L. Review of various treatment options and potential therapies for osteonecrosis of the femoral head. J Orthop Transl. 2016;4:57–70. doi: 10.1016/j.jot.2015.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Winter D.A. Human balance and posture control during standing and walking. Gait Posture. 1995;3(4):193–214. [Google Scholar]
- 28.Winter D.A., Patla A.E., Frank J.S., Walt S.E. Biomechanical walking pattern changes in the fit and healthy elderly. Phys Ther. 1990;70:340–347. doi: 10.1093/ptj/70.6.340. [DOI] [PubMed] [Google Scholar]
- 29.Neptune R.R., Zajac F.E., Kautz S.A. Muscle force redistributes segmental power for body progression during walking. Gait Posture. 2004;19:194–205. doi: 10.1016/S0966-6362(03)00062-6. [DOI] [PubMed] [Google Scholar]
- 30.DeVita P., Hortobagyi T. Age causes a redistribution of joint torques and powers during gait. J Appl Physiol. 2000;88:1804–1811. doi: 10.1152/jappl.2000.88.5.1804. [DOI] [PubMed] [Google Scholar]
- 31.Goldberg E.J., Neptune R.R. Compensatory strategies during normal walking in response to muscle weakness and increased hip joint stiffness. Gait Posture. 2007;25:360–367. doi: 10.1016/j.gaitpost.2006.04.009. [DOI] [PubMed] [Google Scholar]
- 32.Kerr C., McDowell B.C., Parkes J., Stevenson M., Cosgrove A.P. Age-related changes in energy efficiency of gait, activity, and participation in children with cerebral palsy. Dev Med Child Neurol. 2011;53(1):61–67. doi: 10.1111/j.1469-8749.2010.03795.x. [DOI] [PubMed] [Google Scholar]
- 33.Chen M.S., Lin T.C., Jiang B.C. Aerobic and resistance exercise training program intervention for enhancing gait function in elderly and chronically ill Taiwanese patients. Public Health. 2015;129(8):1114–1124. doi: 10.1016/j.puhe.2015.04.018. [DOI] [PubMed] [Google Scholar]
- 34.Hvid L.G., Strotmeyer E.S., Skjodt M., Magnussen L.V., Andersen M., Caserotti P. Voluntary muscle activation improves with power training and is associated with changes in gait speed in mobility-limited older adults-A randomized controlled trial. Exp Gerontol. 2016;80:51–56. doi: 10.1016/j.exger.2016.03.018. [DOI] [PubMed] [Google Scholar]
- 35.Morris J.N., Hardman A.E. Walking to health. Sport Med. 1997;23:306–332. doi: 10.2165/00007256-199723050-00004. [DOI] [PubMed] [Google Scholar]
- 36.Mutrie N., Hannah M.-K. Some work hard while others play hard: the achievement of current recommendations for physical activity levels at work, at home, and in leisure time in the West of Scotland. Int J Health Promot Educ. 2004;42:109–117. [Google Scholar]
- 37.Lee H.J., Lee S., Chang W.H., Seo K., Shim Y., Choi B.O. A wearable hip assist robot can improve gait function and cardiopulmonary metabolic efficiency in elderly adults. IEEE Trans Neural Syst Rehabil Eng. 2017;25(9):1549–1557. doi: 10.1109/TNSRE.2017.2664801. [DOI] [PubMed] [Google Scholar]
- 38.Seo K., Lee J., Park Y.J. IEEE; London, UK: 2017. Autonomous hip exoskeleton saves metabolic cost of walking uphill. International Conference on Rehabilitation Robotics; pp. 246–251. [DOI] [PubMed] [Google Scholar]
- 39.Ding Y., Panizzolo F.A., Siviy C., Malcolm P., Galiana I., Holt K.G. Effect of timing of hip extension assistance during loaded walking with a soft exosuit. J NeuroEng Rehabil. 2016;13:1–10. doi: 10.1186/s12984-016-0196-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chen B., Grazi L., Lanotte F., Vitiello N., Crea S. A real-time lift detection strategy for a hip exoskeleton. Front Neurorob. 2018;12(17):1–11. doi: 10.3389/fnbot.2018.00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chen B., Lanotte F., Grazi L., Vitiello N., Crea S. Classification of lifting techniques for application of a robotic hip exoskeleton. Sensors. 2019;19(963):1–13. doi: 10.3390/s19040963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jang J., Kim K., Lee J., Lim B., Shim Y. IEEE; Daejeon, Korea: 2016. Assistance strategy for stair ascent with a robotic hip exoskeleton. IEEE/RSJ International Conference on Intelligent Robots & Systems; pp. 5658–5663. [Google Scholar]
- 43.Giovacchini F., Vannetti F., Fantozzi M., Cempini M., Cortese M., Parri A. A light-weight active orthosis for hip movement assistance. Robot Auton Syst. 2015;73:123–134. [Google Scholar]
- 44.Kong K., Bae J., Tomizuka M. A compact rotary series elastic actuator for human assistive systems. IEEE ASME Trans Mechatron. 2012;17(2):288–297. [Google Scholar]
- 45.Shimada H., Kimura Y., Suzuki T., Hirata T., Sugiura M., Endo Y. The use of positron emission tomography and [18F]fluorodeoxyglucose for functional imaging of muscular activity during exercise with a stride assistance system. IEEE Trans Neural Syst Rehabil Eng. 2007;15(3):442–448. doi: 10.1109/TNSRE.2007.903978. [DOI] [PubMed] [Google Scholar]
- 46.Shimada H., Hirata T., Kimura Y., Naka T., Kikuchi K., Oda K. Effects of a robotic walking exercise on walking performance in community-dwelling elderly adults. Geriatr Gerontol Int. 2010;9(4):372–381. doi: 10.1111/j.1447-0594.2009.00546.x. [DOI] [PubMed] [Google Scholar]
- 47.Buesing C., Fisch G., O'Donnell M., Shahidi I., Thomas L., Mummidisetty C.K. Effects of a wearable exoskeleton stride management assist system (SMA®) on spatiotemporal gait characteristics in individuals after stroke: a randomized controlled trial. J NeuroEng Rehabil. 2015;12:1–14. doi: 10.1186/s12984-015-0062-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wu Q.C., Wang X.S., Du F.P., Zhang X.B. Design and control of a powered hip exoskeleton for walking assistance. Int J Adv Robot Syst. 2015;12:1–11. [Google Scholar]
- 49.Chen L., Wang X.S., Xu W.L. Inverse transmission model and compensation control of a single-tendon-sheath actuator. IEEE Trans Ind Electron. 2014;61(3):1424–1433. [Google Scholar]
- 50.Ryder M.C. 2015. A continuous rotary actuation mechanism for a powered hip exoskeleton. Masters Thesis, Department of Mechanical and Industrial Engineering, University of Massachusetts Amherst. [Google Scholar]
- 51.Zhang T., Tran M., Huang H. IEEE/RSJ International Conference on Intelligent Robots and Systems (IROS), Vancouver, BC, Canada, 2017. 2017. NREL-Exo: a 4-DoFs wearable hip exoskeleton for walking and balance assistance in locomotion; pp. 508–513. [Google Scholar]
- 52.Sawicki G.S., Lewis C.L., Ferris D.P. It pays to have a spring in your step. Exerc Sport Sci Rev. 2009;37(3):1–19. doi: 10.1097/JES.0b013e31819c2df6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Junius K., Degelaen M., Lefeber N., Swinnen E., Vanderborght B., Lefeber D. Bilateral, misalignment-compensating, full-DOF hip exoskeleton: design and kinematic validation. Appl Bionics Biomechanics. 2017;2017(5):1–14. doi: 10.1155/2017/5813154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Junius K., Lefeber N., Swinnen E., Vanderborght B., Lefeber D. Metabolic effects induced by a kinematically compatible hip exoskeleton during STS. IEEE Trans Biomed Eng. 2018;65(6):1399–1409. doi: 10.1109/TBME.2017.2754922. [DOI] [PubMed] [Google Scholar]
- 55.Kang I., Hsu H., Young A. The effect of hip assistance levels on human energetic cost using robotic hip exoskeletons. IEEE Robot Autom Lett. 2019;4(2):430–437. [Google Scholar]
- 56.Toxiri S., Ortiz J., Masood J., Fernandez J., Mateos L.A., Caldwell D.G. IEEE; Zhuhai, China: 2015. A wearable device for reducing spinal loads during lifting tasks: biomechanics and design concepts. IEEE International Conference on Robotics and Biomimetics; pp. 2295–2300. [Google Scholar]
- 57.Masood J., Ortiz J., Fernández J., Mateos L.A., Caldwell D.G. IEEE International Conference on Biomedical Robotics and Biomechatronics. IEEE, UTown, Singapore. 2016. Mechanical design and analysis of light weight hip joint parallel elastic actuator for industrial exoskeleton; pp. 631–636. [Google Scholar]
- 58.Mettin U., La Hera P.X., Freidovich L.B., Shiriaev A.S. Parallel elastic actuators as a control tool for preplanned trajectories of underactuated mechanical systems. Int J Robot Res. 2010;29(9):1186–1198. [Google Scholar]
- 59.Young A.J., Foss J., Gannon H., Ferris D.P. Influence of power delivery timing on the energetics and biomechanics of humans wearing a hip exoskeleton. Front Bioeng Biotechnol. 2017;5(4):1–11. doi: 10.3389/fbioe.2017.00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Nagarajan U., Aguirreollinger G., Goswami A. Integral admittance shaping: a unified framework for active exoskeleton control. Robot Auton Syst. 2016;75:310–324. [Google Scholar]
- 61.Lee G., Ding Y., Bujanda I.G., Karavas N., Zhou Y.M., Walsh C.J. IEEE/RSJ International Conference on Intelligent Robots and Systems, Vancouver, Canada, 2017. 2017. Improved assistive profile tracking of soft exosuits for walking and jogging with off-board actuation; pp. 1–8. [Google Scholar]
- 62.Zhang T., Tran M., Huang H. Design and experimental verification of hip exoskeleton with balance capacities for walking assistance. IEEE/ASME Trans Mechatron. 2018;23(1):274–285. [Google Scholar]
- 63.Cè E., Rampichini R., Monti E., Venturelli M., Limonta E., Esposito F. Changes in the electromechanical delay components during a fatiguing stimulation in human skeletal muscle: an EMG, MMG and force combined approach. Eur J Appl Physiol. 2017;117:95–107. doi: 10.1007/s00421-016-3502-z. [DOI] [PubMed] [Google Scholar]
- 64.Lewis C., Ferris D. Invariant hip moment pattern while walking with a robotic hip exoskeleton. J Biomech. 2011;44(5):789–793. doi: 10.1016/j.jbiomech.2011.01.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lenzi T., Carrozza M., Agrawal S. Powered hip exoskeletons can reduce the user's hip and ankle muscle activations during walking. IEEE Trans Neural Syst Rehabil Eng. 2013;21(6):938–948. doi: 10.1109/TNSRE.2013.2248749. [DOI] [PubMed] [Google Scholar]
- 66.Grazi L., Crea S., Parri A., Yan T.F., Cortese M., Giovacchini F. Conf. Proc. IEEE. Eng. Med. Biol. Soc. Milan, Italy. 2015. Gastrocnemius myoelectric control of a robotic hip exoskeleton; pp. 3881–3884. [DOI] [PubMed] [Google Scholar]
- 67.Grazi L., Crea S., Parri A., Lova R.M., Micera S., Vitiello N. Gastrocnemius myoelectric control of a robotic hip exoskeleton can reduce the user's lower-limb muscle activities at push off. Front Neurosci. 2018;12:1–11. doi: 10.3389/fnins.2018.00071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Young A.J., Hannah G., Ferris D.P. A biomechanical comparison of proportional electromyography control to biological torque control using a powered hip exoskeleton. Front Bioeng Biotechnol. 2017;5:1–18. doi: 10.3389/fbioe.2017.00037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Yan T., Parri A., Garate V.R., Cempini M., Ronsse R., Vitiello N. An oscillator-based smooth real-time estimate of gait phase for wearable robotics. Aut Robots. 2017;41(3):759–774. [Google Scholar]
- 70.Sugar T.G., Fernandez E., Kinney D., Hollander K.W., Redkar S. Springer; 2017. HeSA, Hip exoskeleton for superior assistance. Wearable robotics: challenges and trends; pp. 319–323. [Google Scholar]
- 71.Davies C. 2013. Honda walking assist device goes into broad hospital trial. Slash Gear.www.slashgear.com/honda-walking-assist-device-goes-into-broad-hospital-trial-29284034 [Online]. Available at: [Google Scholar]
- 72.Yang M.X., Zhu Q., Xi R.R., Wang X.S., Han Y.L. 23rd International Conference on mechatronics and Machine Vision in practice (M2VIP), Nanjing, China, IEEE, 2016. 2016. Design of the power-assisted hip exoskeleton robot with hydraulic servo rotary drive; pp. 1–5. [Google Scholar]
- 73.Li Z.R., Cheng L.M., Wang K.Z., Yang N.P., Yang S.H., He W. XLGB herbal Fufang prevents corticosteroid-induced osteonecrosis of the femoral head - a multicenter, randomized, double-blind, placebo-controlled clinical trial. J Orthop Transl. 2018;12:36–44. doi: 10.1016/j.jot.2017.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Tian L., Tang N., Ngai T., Wu C., Ruan Y.C., Huang L. Hybrid fracture fixation systems developed for orthopaedic applications, A general review. J Orthop Transl. 2019;16:1–13. doi: 10.1016/j.jot.2018.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Waters R.L., Mulroy S. The energy expenditure of normal and pathologic gait. Gait Posture. 1999;9(3):207–231. doi: 10.1016/s0966-6362(99)00009-0. [DOI] [PubMed] [Google Scholar]
- 76.Chen B., Zhao X., Ma H., Qin L., Liao W.H. Design and characterization of a magneto-rheological series elastic actuator for a lower extremity exoskeleton. Smart Mater Struct. 2017;26(10):1–17. [Google Scholar]
- 77.Pan Q.S., Huang F.S., Chen J., He L.G., Li W., Feng Z.H. High-speed low-friction piezoelectric motors based on centrifugal force. IEEE Trans Ind Electron. 2017;64(3):2158–2167. [Google Scholar]
- 78.Hanada E., Kerrigan D.C. Energy consumption during level walking with arm and knee immobilized. Arch PM&R (Phys Med Rehabil) 2001;82:1251–1254. doi: 10.1053/apmr.2001.24902. [DOI] [PubMed] [Google Scholar]