Abstract
Objective
To analyse the 6 degrees of freedom of the knee and gait data of patients with medial knee osteoarthritis before and after fixed-bearing (FB) and mobile-bearing (MB) total knee arthroplasty (TKA) and examine the influence of TKA on gait characteristics and the difference between FB and MB prosthesis. We also sought to explore the prosthesis options available for TKA in these patients.
Methods
Thirty patients who underwent TKA at the Department of Orthopedics at our hospital from June to October 2017 were included. All patients had a lower limb mechanical axis (hip-knee-ankle angle) of less than 180° which were regarded as genu varum knees and had medial knee osteoarthritis. Patients were randomised divided into the FB group and the MB group according to the knee prosthesis implanted. An infrared navigation three-dimensional portable knee motion analysis system (Opti-Knee®, Shanghai Innomotion, Inc.) was used to acquire data on the 6 degrees of freedom of both knees when walking on flat ground before and after surgery (angle of tibia relative to femur parameters: flexion-extension, internal rotation–external rotation, abduction–adduction; displacement parameters: anterior–posterior, proximal–distal, medial–lateral). Postoperative follow-up efficacy was assessed using the Oxford Knee Score system.
Results
There were significant differences in the maximum values of the internal/external rotation and flexion/extension angle between patients post-TKA and the healthy population, p values were 0.007 and <0.001,respectively. The postoperative maximum values of genu varum and internal rotation in both FB [(−9.49 ± 5.99°), (−5.77 ± 3.42°), respectively] and MB [(−9.64 ± 4.83°), (−7.54 ± 4.51°), respectively] groups were lower than the preoperative ones [FB (−15.13 ± 6.78°), (−8.28 ± 4.83°); MB (−13.28 ± 3.98°), (−9.46 ± 4.99°), respectively] (p ≤ 0.001), while the postoperative maximum values of flexion angle and anterior displacement in both FB [(46.11 ± 4.14°), (0.71 ± 0.35 cm), respectively] and MB [(49.33 ± 3.98°), (0.75 ± 0.89 cm), respectively] groups were larger than the preoperative ones [FB (43.15 ± 3.77°), (0.26 ± 0.74 cm); MB (44.62 ± 5.92°), (0.33 ± 0.79°), respectively] (p ≤ 0.001). The postoperative range of flexion/extension angle in both FB (40.13 ± 4.14°) and MB (45.82 ± 3.76°) groups was significantly larger than the preoperative one [FB (36.17 ± 6.07°), MB (37.09 ± 3.93°), respectively] (p ≤ 0.001). There were also significant increases in range of anterior–posterior displacement in the FB group (0.85 ± 0.32 cm) postoperatively compared with the preoperative one (0.71 ± 0.92 cm) (p = 0.016) and significant increases in range of medial-lateral displacement (0.64 ± 0.73 cm) in the MB group postoperatively compared with the preoperative one (0.52 ± 0.91 cm) (p = 0.025). The mean flexion/extension angle of the MB group was significantly greater than the FB group after surgery in both the stance phase and the swing phase (p < 0.001). There were significant differences in postoperative knee axial rotation during the gait cycle between the MB and FB groups (p = 0.028) and that postoperative internal rotation of the tibia relative to the femur increased in the MB group. The Oxford Knee Score at the last follow-up visit about 7.5 months after surgery was 15.6 ± 1.3 and 15.1 ± 1.1 points for FB and MB groups, respectively. This difference was not significant (p = 0.428).
Conclusions
TKA can make the parameters of knee gait characteristics closer to the normal population. Medial knee osteoarthritis patients who received a MB prosthesis in TKA had better joint flexion function and axial rotation than the FB one. However, there is insufficient evidence to suggest that the MB prosthesis is a better option for patients with medial knee osteoarthritis.
The translational potential of this article
To date, no consensus for prosthesis selection in TKA has been established. This study found significant differences in joint flexion/extension angle and internal/external rotation during gait post-TKA surgery in medial knee osteoarthritis patients who received different prostheses. This will provide some references for prosthesis selection for a large number of genu varum patients in clinical practice.
Keywords: Fixed-bearing, Gait analysis, Kinematic, Prosthesis implantation, Mobile-bearing, Total knee arthroplasty
Introduction
Knee osteoarthritis is a common cause of adult knee disability, of which medial knee osteoarthritis accounts for 60%–80% [1]. Total knee arthroplasty (TKA) is widely used in clinical practice for treating severe advanced knee osteoarthritis, and effective medial knee osteoarthritis TKA surgeries can enable most patients to achieve satisfactory mobility. The long-term efficacy of TKA is determined by recovery of normal kinematic function of the knees [2], [3]. Prosthesis selection for optimising joint geometry can result in better long-term recovery of joint kinematic function [4]. The latest national study by Liu Q demonstrated that the number of elderly osteoarthritis patients and patients living with knee dysfunction are increasing in China, along with various associated burdens [5]. A study by Osmani et al. reported that the majority of the cost of TKA is that of the prosthesis, which has demonstrated an accelerated increase [6]. However, a consensus for prosthesis selection, both in China and abroad, remains to be established. Mobile-bearing (MB) TKA prostheses have been widely used today because of its moderate price and advanced design. The first TKA surgery to use a MB prosthesis was carried out in 1980 [7]. Comparison of the designs of the mobile-bearing prosthesis and fixed-bearing prosthesis revealed that the former's insert enable the longitudinal rotation of the tibia (MB) or allow for anterior-posterior displacement between the insert and tibia. Owing to the rotation and displacement effects between the mobile insert and tibial prosthesis, the tibial prosthesis can fit the femoral prosthesis better, without sacrificing the natural rotation and displacement between the tibia and femur [8]. In theory, this has advantages such as reducing insert friction, lower risk of loosening, lower revision rate, and better clinical efficacy.
In the last 5 years, several studies have compared the efficacy between MB and fixed-bearing (FB) or TKA surgery. Although MB knee prostheses have been regarded as successful with low contact stress, they did not demonstrate better maximum knee flexion, range of motion, posterior condylar translation, tibial axial rotation, knee function score, and durability compared with FB [9], [10], [11], [12]. While some in vivo kinematic studies reported that MB had significant advantages in the axial surface rotation between the tibia and femur over FB [8], [13], [14], other studies did not observe such advantages [15], [16], [17]. In recent years, few studies have reported on the use of gait analysis to assess the differences in walking between MB and FB [4], [18], [19]. Although some differences were observed in gait data variables, there were no significant differences in postoperative higher functions, polyethylene wear, and prosthesis survival rates. Chinese researchers have used the VICON three-dimensional gait analyser to compare early gait post-TKA between the high flexion FB and MB and did not find any differences. However, they only measured the step length, step speed, and step frequency in gait and did not assess the 6 degrees of freedom of the knee [20]. Other Chinese studies have compared the prognoses between FB and MB through post-TKA joint function scores and X-ray and also did not find any differences [21], [22]. In summary, to date, there have been no reports on the use of 6 degrees of freedom of the knee joint data to compare different prosthesis options for specific patients with medial knee osteoarthritis.
The aim of the present study was two-fold: (1) to employ a novel portable three-dimensional knee movement analysis system (Opti-Knee®, Shanghai Innomotion Inc.) to acquire the preoperative and postoperative 6 degrees of freedom of the knee joint data from medial knee osteoarthritis patients who underwent FB or MB TKA surgery and (2) to examine whether TKA can restore the gait characteristics to normal and compare the differences in postoperative gait between the FB and MB groups. We hypothesised that (1) TKA can make the gait characteristics of patients closer to normal and (2) MB have better joint flexion function and axial rotation than the FB in total knee arthroplasty. The results may provide some references for the selection of the type of prosthesis for patients with medial knee osteoarthritis.
Materials and methods
Subjects
Thirty patients who underwent TKA from June to October 2017 at the Department of Orthopedics at our hospital were selected. Grading and classification of these patients were carried out according to the preoperative full-length X-ray image of the lower limbs at standing position. All patients had a medial knee osteoarthritis grade of Kellgren–Lawrence Grade III or above with medial articular surface “bone to bone” and severe patellofemoral joint degeneration, which fulfilled the indications for TKA. All patients had a lower limb mechanical axis (hip-knee-ankle angle) less than 180° which were regarded as genu varum knees and had medial knee osteoarthritis. Patients who participated in the gait analysis experiment did so voluntarily and fully understood the clinical trial protocol. Informed consent was obtained in all patients. The patients and investigators were both blinded for the types of implanted prosthesis. Patients were completely randomised grouping into FB (n = 15) and MB (n = 15) implants. Data of the healthy control group were provided by Shanghai Innomotion, Inc. The study protocol was approved by the ethics committee of the hospital. The ethical approval statement number was 2016-96-C23.
Exclusion criteria were as follows: (1) tuberculous arthritis, rheumatoid arthritis, traumatic arthritis, and other nonosteoarthritis patients; (2) severe osteoporosis in the joint or bone defects requiring special prosthesis; and (3) genu varum exceeding 30° or patients with concurrent severe flexion contracture deformities.
Surgical method and prosthesis implantation
All TKA surgeries were carried out by highly experienced surgeons from the same department. A pneumatic tourniquet (inflation pressure twice that of the patient's baseline blood pressure) was attached to the proximal end of the ipsilateral thigh. A 12-cm median longitudinal skin incision was made in front of the knee, and the skin and subcutaneous tissues were cut. The supporting ligament and joint capsule were cut along the medial edge of the patella, followed by patellar eversion and exposure of the joint cavity. The fat pads were removed. Soft tissue release was not carried out. Cruciate ligaments were excised for joint dislocation. The meniscus and some congestive synovial tissues were excised. Osteotomy of the distal end of the femur and the proximal end of the tibia were carried out based on preoperative measurements and prosthesis option. Measurement osteotomy was used for rotary osteotomy of the femur. After completion of osteotomy, a dummy prosthesis was inserted to assess whether the size of the prosthesis is suitable, the lower limb mechanical axis is restored to normal, and the tension between the flexion and extension gaps was adjusted. Following that, the dummy prosthesis was removed, and the joint cavity was completely flushed. A cocktail analgesic injection (195 mg ropivacaine + 0.5 mL adrenaline + 10 mg morphine + physiological saline topped up to 60 mL) was injected at the posterior joint capsule, periosteum, and surrounding soft tissues. The prostheses (SIGMA prosthesis from Depuy, Inc.) were then implanted. Fifteen patients received the PFC FB prosthesis, while 15 patients received the RP MB prosthesis. All prostheses were fixed using bone cement. Excess bone cement was removed before the joint cavity was flushed again. Joint mobility was 0°–120°. All patients underwent patellar replacement, sealing of the incision, compression bandaging, and loose tourniquets. No drainage tube was retained. Patients initiated routine walking 1 day after surgery. All patients had an active maximum knee flexion angle of 90° in 3 days after surgery. At the time of gait data collection about 7.5 months after surgery, patients have recovered and could walk like ‘Forgotten knee’.
Gait analysis device, knee imaging, and functional assessment
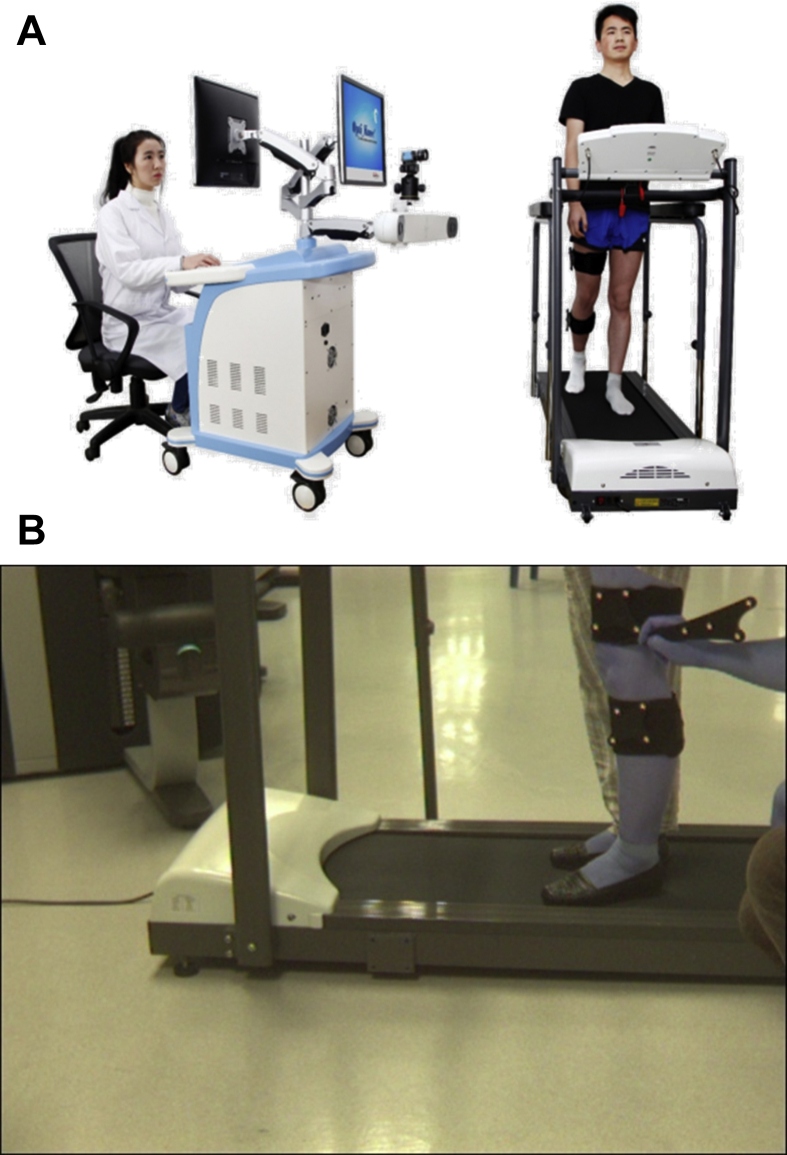
An in vivo infrared navigation three-dimensional knee joint movement analysis system (Opti-Knee®, Shanghai Innomotion, Inc.) was used to acquire data on the 6 degrees of freedom of both knees 2 days before surgery and about 7.5 months after surgery (angle of tibia relative to femur parameters: flexion–extension, internal rotation–external rotation, abduction–adduction; displacement parameters: anterior–posterior, proximal–distal, and medial–lateral) (Fig. 1A). The Opti-Knee® three-dimensional knee joint movement analysis system integrates infrared navigation technology and movement capture technology to track and record movement trajectories, and synchronously photograph moving images. This system exhibits dynamic, real-time, three-dimensional, and objective quantitation characteristics and accounts for an area of only 1.1 m × 0.6 m × 0.4 m.
Figure 1.
(A) Opti-Knee in vivo infrared navigation three-dimensional knee joint movement analysis system. (B) Infrared sensor markers based on bony markers.
Measurement method: Before walking, bony markers were located on every subject. A set of eight reflective markers were used according to a standardised protocol provided by the developer. Two sets of markers on two rigid bandages which were fixed 8 cm above the lateral epicondyle of femur and 3 cm below the fibular head were attached on the test limb according to premade grids, with each set consisting of four infrared sensors in corresponding markers (OK_Marquer®,Shanghai Innomotion, Inc.). After fixing the markers, calibration was performed by marking specified body landmarks with the use of a pointer fixed with four reflective markers. Body landmarks included the trochanter major, condylus lateralis, condylus medialis, medial tibial plateau, lateral tibial plateau, medial malleolus, and lateral malleolus (Fig. 1B).Three points on the ground were also captured. The three-dimensional trajectory of the infrared sensor was tracked at a frequency of 60 Hz using an integrated dual stereo infrared camera with an accuracy of 0.3 mm root mean square and 0.2° [23]. The subjects walked on a treadmill without aid for 3 min before official data collection. When the subjects were able to walk freely and normally, an integrated synchronous high-speed camera was used to collect walking videos and gait data at a frequency of 60 frames per second for 15 s. Collection was carried out twice. Knee kinematics, including rotations and translations, were calculated for each frame using the geometric relationships between the reflective markers under the femur and tibia coordinate systems that were established during calibration. A default software automatically outputs the gait data of the knee joints at every side of each subject. The maximum and minimum values of each degree of freedom data were collected; the difference between the two values constitutes the range of motion.
Weight-bearing full-length X-ray images of the ipsilateral limb were taken in all subjects who underwent TKA during the outpatient visit about 7.5 months after surgery. The X-ray images were used to assess the lower limb mechanical axis recovery status and presence/absence of prosthesis loosening or infection, as well as polyethylene insert displacement, among others.
Knee function was assessed using the Oxford Knee Score (OKS) about 7.5 months after surgery. This system is composed of 12 constituent items, including five pain markers and seven functional markers. The pain markers include self-description of pain and joint pain under specific situations. The functional markers include joint function when walking up and down a flight of stairs, washing and drying, getting in and out of cars, walking, and squatting/standing up. Each item is scored 1–5 points, where 1 = best and 5 = worst outcomes. The scores of the 12 items were summed up to obtain a total score of 12–60 points. This evaluation system has been shown to demonstrate good results in evaluating post-TKA joint function [24].
Statistical analysis
The Microsoft Office Excel 2010 software was used for statistical processing. One-way analysis of variance was used to compare age, body mass index (BMI), postoperative maximum values of the 6 degrees of freedom, and range of motion of the knee joint across FB, MB, and health control groups. The paired samples t-test was conducted to compare the maximum value of the 6 degrees of freedom of the knee joint presurgery/postsurgery in the FB and MB group, respectively. The difference in postoperative OKS score, flexion/extension angles, and internal/external rotation between FB and MB groups were compared using Student t-test. A difference of p < 0.05 was considered to be statistically significant.
Results
General information
Table 1 showed the mean age, sex, BMI, preoperative hip-knee-ankle angle, and postoperative follow-up duration in two groups. Patients in the FB group were older than the MB group, while the mean BMI of the FB group was lower than the MB group, p values were 0.014 and 0.002, respectively. There was no statistically significant difference in sex (p = 0.393), preoperative lower limb mechanical axis (hip-knee-ankle angle) (p = 0.107), and postoperative follow-up duration (p = 0.582) between the two groups. X-rays taken at the last postoperative follow-up visit about 7.5 months after surgery in both groups demonstrated that the lower limb mechanical axis recovery and position of the prostheses were satisfactory. The mean HKA angle post-TKA was 179.5° in FB group and 179.3° in MB group (p = 0.581). No prosthesis loosening, infection, or polyethylene insert displacement occurred.
Table 1.
General information of patients.
| Group | n | Age |
Sex |
Body mass index |
Hip-knee-ankle angle |
Follow-up duration |
|---|---|---|---|---|---|---|
| (years, ±s) | (n, Male/Female) | (㎏/㎡,±s) | (degrees, ±s) | (Months, ±s) | ||
| FB group | 15 | 69 ± 5.3 | 6/9 | 24.8 ± 2.8 | 176.7 ± 1.2 | 7.5 ± 0.5 |
| MB group | 15 | 67 ± 4.2 | 7/8 | 26.8 ± 1.6 | 177.3 ± 1.5 | 7.7 ± 0.6 |
| p value | 0.014 | 0.393 | 0.002 | 0.107 | 0.582 |
FB = fixed-bearing prosthesis group; MB = mobile-bearing prosthesis group.
Gait characteristics and joint function
The mean values of the maximum value and range of motion (maximum value − minimum value) for the 6 degrees of freedom of the knee joint during the gait cycle were used for comparison (Table 2). There were significant differences in the maximum values of the internal/external rotation and flexion/extension angle between patients post-TKA and the healthy population, p values were 0.007 and <0.001, respectively. The maximum values of the internal rotation in MB group (−7.54 ± 4.51°) were larger than those in the healthy population (−5.93 ±3.56°),while these values in FB group (−5.77 ± 3.42°) were lower than those in the healthy population (−5.93 ± 3.56°).The maximum flexion angles of FB (46.11 ± 4.14°) and MB (−49.33 ± 3.98°) groups were lower than the healthy control group (55.91 ± 3.36°). The range of flexion/extension angles and various displacements in both FB and MB groups post-TKA was significantly lower than those in the healthy population (p ≤ 0.001).
Table 2.
Comparison of the maximum value and range of motion of the 6 degrees of freedom of the knee joint in the FB and MB groups of patients after surgery and the healthy control group.
| Group |
Healthy control group |
FB group |
MB group |
p1 | p2 |
|---|---|---|---|---|---|
| N | 15 | 15 | 15 | ||
| Varus/valgus angle | −10.36 ± 2.17/5.97 ± 1.50 | −9.49 ± 5.99/5.43 ± 1.01 | −9.64 ± 4.83/5.01 ± 1.93 | 0.096 | 0.052 |
| Internal/external rotation | −5.93 ± 3.56/11.74 ± 2.69 | −5.77 ± 3.42/10.75 ± 3.03 | −7.54 ± 4.51/11.48 ± 4.38 | 0.007 | 0.081 |
| Flexion/extension angle | 55.91 ± 3.36/50.82 ± 4.35 | 46.11 ± 4.14/40.13 ± 4.14 | 49.33 ± 3.98/45.82 ± 3.76 | ≤0.001 | ≤0.001 |
| Anterior-posterior displacement | 0.78 ± 0.57/1.36 ± 0.37 | 0.71 ± 0.35/0.85 ± 0.32 | 0.75 ± 0.89/0.72 ± 0.64 | 0.359 | 0.001 |
| Superior-inferior displacement | 1.37 ± 0.31/1.68 ± 0.32 | 1.31 ± 0.37/0.78 ± 0.43 | 1.28 ± 0.43/0.84 ± 0.21 | 0.430 | ≤0.001 |
| Medial-lateral displacement | 0.43 ± 0.31/1.07 ± 0.37 | 0.41 ± 0.13/0.41 ± 0.13 | 0.46 ± 0.47/0.64 ± 0.73 | 0.643 | ≤0.001 |
FB = fixed-bearing prosthesis group; MB = mobile-bearing prosthesis group.
Motion angle (°,±s), displacement (cm,±s); degrees of freedom data: maximum value/range of motion; varus-valgus angle:negative value-positive value; internal rotation-external rotation: negative value-positive value; anterior-posterior displacement:positive value-negative value; superior-inferior displacement:positive value-negative value; medial-lateral displacement:negative value-positive value; p1: intergroup difference in maximum value, <0.05 indicates statistical significance; p2: intergroup difference in range of motion, <0.05 indicates statistical significance
The postoperative maximum values of genu varum and internal rotation in both FB [(−9.49 ± 5.99°), (−5.77 ± 3.42°), respectively] and MB [(−9.64 ± 4.83°), (−7.54 ± 4.51°), respectively] groups were lower than the preoperative ones [FB (−15.13 ± 6.78°), (−8.28 ± 4.83°); MB (−13.28 ± 3.98°), (−9.46 ± 4.99°); respectively] (p ≤ 0.001),while the postoperative maximum values of flexion angle and anterior displacement in both FB [(46.11 ± 4.14°), (0.71 ± 0.35 cm), respectively] and MB [(49.33 ± 3.98°), (0.75 ± 0.89 cm), respectively] groups were larger than the preoperative ones [FB (43.15 ± 3.77°), (0.26 ± 0.74 cm); MB (44.62 ± 5.92°), (0.33 ± 0.79°); respectively] (p ≤ 0.001) (Table 3).
Table 3.
Comparison of the maximum value of the 6 degrees of freedom of the knee joint in the FB and MB groups before and after surgery.
| Group |
FB group |
MB group |
p1 | p2 | ||
|---|---|---|---|---|---|---|
| Status | Before surgery | After surgery | Before surgery | After surgery | ||
| Varus/valgus angle | −15.13 ± 6.78 | −9.49 ± 5.99 | −13.28 ± 3.98 | −9.64 ± 4.83 | ≤0.001 | ≤0.001 |
| Internal/external rotation | −8.28 ± 4.83 | −5.77 ± 3.42 | −9.46 ± 4.99 | −7.54 ± 4.51 | ≤0.001 | ≤0.001 |
| Flexion/extension angle | 43.15 ± 3.77 | 46.11 ± 4.14 | 44.62 ± 5.92 | 49.33 ± 3.98 | ≤0.001 | ≤0.001 |
| Anterior-posterior displacement | 0.26 ± 0.74 | 0.71 ± 0.35 | 0.33 ± 0.79 | 0.75 ± 0.89 | ≤0.001 | ≤0.001 |
| Superior-inferior displacement | 1.21 ± 0.67 | 1.31 ± 0.37 | 1.31 ± 0.61 | 1.28 ± 0.43 | 0.177 | 0.137 |
| Medial-lateral displacement | 0.44 ± 0.24 | 0.41 ± 0.13 | 0.39 ± 0.26 | 0.46 ± 0.47 | 0.792 | 0.534 |
FB = fixed-bearing prosthesis group; MB = mobile-bearing prosthesis group.
Motion angle (°,±s), displacement (cm,±s); degrees of freedom data: maximum value; Varus-valgus angle: negative value-positive value; internal rotation-external rotation: negative value-positive value; anterior-posterior displacement:positive value-negative value; superior-inferior displacement:positive value-negative value; medial-lateral displacement: negative value-positive value; p1: differences before and after surgery in the FB group, <0.05 indicates statistical significance; p2: differences before and after surgery in the MB group, <0.05 indicates statistical significance
The postoperative range of internal/external rotation in FB group (10.75 ± 3.03°) was significantly lower than the preoperative one (12.05 ± 3.88°) (p = 0.037), while this range in MB group (11.48 ± 4.38°) was significantly larger than the preoperative one (9.06 ± 5.75°) (p ≤ 0.001). The postoperative range of flexion/extension angle in both FB (40.13 ± 4.14°) and MB (45.82 ± 3.76°) groups was significantly larger than the preoperative one [FB (36.17 ± 6.07°), MB (37.09 ± 3.93°), respectively] (p ≤ 0.001). There were also significant increases in range of anterior–posterior displacement in the FB group (0.85 ± 0.32 cm) postoperatively compared with the preoperative one (0.71 ± 0.92 cm) (p = 0.016) and significant increases in range of medial–lateral displacement (0.64 ± 0.73 cm) in the MB group postoperatively compared with the preoperative one (0.52 ± 0.91 cm) (p = 0.025) (Table 4).
Table 4.
Comparison of the range of motion of the 6 degrees of freedom of the knee joint in the FB and MB groups before and after surgery.
| Group |
FB group |
MB group |
p1 | p2 | ||
|---|---|---|---|---|---|---|
| Status | Before surgery | After surgery | Before surgery | After surgery | ||
| Varus/valgus angle | 4.91 ± 1.34 | 5.43 ± 1.01 | 4.79 ± 1.72 | 5.01 ± 1.93 | 0.083 | 0.118 |
| Internal/external rotation | 12.05 ± 3.88 | 10.75 ± 3.03 | 9.06 ± 5.75 | 11.48 ± 4.38 | 0.037 | ≤0.001 |
| Flexion/extension angle | 36.17 ± 6.07 | 40.13 ± 4.14 | 37.09 ± 3.93 | 45.82 ± 3.76 | ≤0.001 | ≤0.001 |
| Anterior-posterior displacement | 0.71 ± 0.92 | 0.85 ± 0.32 | 0.66 ± 0.39 | 0.72 ± 0.64 | 0.016 | 0.055 |
| Superior-inferior displacement | 0.81 ± 0.74 | 0.78 ± 0.43 | 0.88 ± 0.21 | 0.84 ± 0.21 | 0.727 | 0.694 |
| Medial-lateral displacement | 0.45 ± 0.21 | 0.41 ± 0.13 | 0.52 ± 0.91 | 0.64 ± 0.73 | 0.287 | 0.025 |
FB = fixed-bearing prosthesis group; MB = mobile-bearing prosthesis group.
Motion angle (°,±s), displacement (cm,±s); degrees of freedom data: range of motion; p1: differences before and after surgery in the FB group, <0.05 indicates statistical significance; p2: differences before and after surgery in the MB group, <0.05 indicates statistical significance
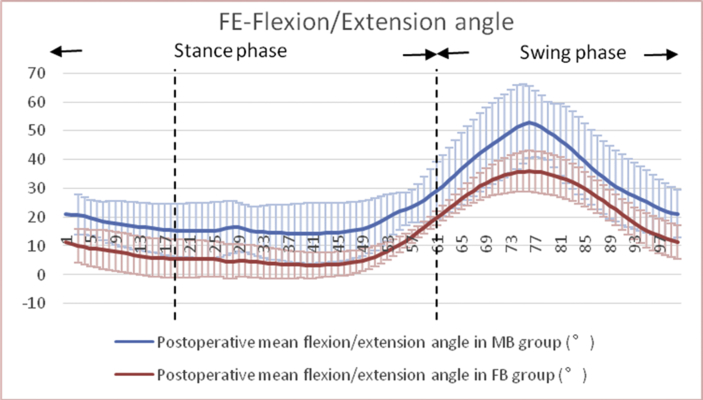
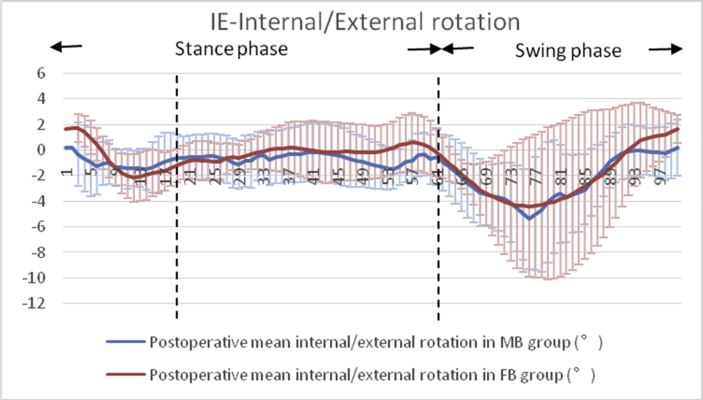
The mean flexion/extension angle of the MB group was significantly greater than the FB group after surgery in both the stance phase and the swing phase (p < 0.001). There were significant differences in postoperative knee axial rotation during the gait cycle between the MB and FB groups (p = 0.028) and that postoperative internal rotation of the tibia relative to the femur increased in the MB group (Figure 2, Figure 3).
Figure 2.
Significant differences in the mean flexion/extension angles were observed between the MB and FB groups after surgery (p < 0.001). FB = fixed-bearing; MB = mobile-bearing.
Figure 3.
Significant differences in mean internal/external rotation were observed between the MB and FB groups after surgery (p = 0.028). FB = fixed-bearing; MB = mobile-bearing.
TKA outcomes
The OKS scores at the last follow-up visit about 7.5 months after surgery was 15.6 ± 1.3 and 15.1 ± 1.1 points for FB and MB groups, respectively. This difference was not significant (p = 0.428).
Discussion
The most important finding in this study was that MB have better joint flexion function and axial rotation than the FB in total knee arthroplasty for specific medial knee osteoarthritis patients. This provided some references for prosthesis selection of a large number of genu varum patients in clinical practice. Mockel et al. found that the MB prosthesis group had greater knee flexion angle at the gait stance phase compared with the FB prosthesis group during walking while bearing weights [25]. Meanwhile, Kramers-de Quervain et al. reported that the MB prosthesis group had a greater maximum knee flexion angle at the gait cycle compared with the FB group [26].Recent systematic reviews and meta-analyses demonstrated that there were no significant differences in postoperative kinematics, gait analysis, joint function scores, and pain scores between the rotating MB and FB prosthesis [9], [27].But, the current study found that the mean flexion/extension angle of the MB group was significantly greater than the FB group after surgery in both the stance phase and the swing phase (P < 0.001), and this results were in line with the results of the two aforementioned studies. Okamoto et al. found that the MB group demonstrated a greater range of axial rotation during step-up activity compared with the FB group and attributed this phenomenon to the mobility of the implanted inserts [28]. Zurcher et al. reported that when patients carry out more demanding tasks after TKA, the MB can provide better axial rotation function for the knee joint during gait and can better adapt to the functional requirements of demanding tasks [19]. The current study demonstrated that there were significant differences in postoperative knee axial rotation between the MB and FB groups (p = 0.028) and that postoperative internal rotation of the tibia relative to the femur increased in the MB group. In theory, the MB group should have better flexion/extension angle and axial rotation mobility compared with the FB group. On the other hand, tibial varus deformity is the main cause of genu varum knee. It is not easy to determine the rotation of tibial prosthesis in TKA for medial knee osteoarthritis patients. The MB can compensate for the poor rotation of the tibial prosthesis by the mobility of insert and tibial prosthesis to reduce the dismatching of the prosthesis and the postcam wear. However, the postoperative OKS scores of the two groups in the present study did not demonstrate any significant differences. In summary, although MB had shown a few advantages over FB in some gait characteristics and joint functions after surgery, there was no sufficient evidences to show that the MB prosthesis is superior for medial knee osteoarthritis patients.
TKA is currently the most effective treatment for end-stage knee osteoarthritis, and its efficacy is generally acknowledged. According to the latest survey on end-stage osteoarthritis in China, the proportion of patients with medial knee osteoarthritis accounted for 91.7% of patients [29]. Therefore, the vast majority of patients who underwent TKA in clinical practice are patients with severe degeneration of the medial knee compartment, with lower limb mechanical axis of less than 180°. It is thus especially important for surgeons to select prostheses with high ‘cost-effective’ for large numbers of patients with genu varum. Compared with ordinary prostheses, ‘high-demand’ prosthesis designs include greater flexion, better kinematic design, the use of zirconia materials, highly cross-linked polyethylene, and MB platforms [6]. The rotating mobile platform which is regarded as the ‘high-demand’ prosthesis is designed to simulate the kinematic characteristics of the knee, reduce polyethylene wear, and increase knee mobility without affecting joint stability and increasing the activity between the insert and tibial prosthesis. However, it is slightly costlier than the fixed platform insert which is considered as an ordinary design, and its postoperative efficacy, long-term survival, and other theoretical advantages remain controversial. The present study also did not show that MB was obviously better than FB in gait characteristics and joint function. The high ‘cost-effective’ prosthesis is still in the exploration.
Assessment of post-TKA efficacy includes X-ray evaluation, various joint function and pain scores, and joint kinematic analysis, among others. Powell et al. supported that the MB had better OKS, SF-12 PCS, and KOOS (Sport/Rec) scores than the FB at 10-year follow-up. But no difference was found in X-ray evaluation. They used a cruciate-retaining prosthesis, which was different from ours [30].Kim et al. compared the posterior cruciate-substituting high-flexion NexGen LPS-Flex MB and NexGen LPS-Flex FB in the same younger patients by long-term clinical, radiographic, and computed tomography scanning. They found no significant difference between these two groups with regard to functional outcome, knee motion, prevalence of osteolysis, or survivorship at 13 year follow-up [31].In the current study, postoperative follow-up X-rays demonstrated the proximity of the lower limb mechanical axis to the physiological mechanical axis, good prosthesis positioning, as well as absence of polyethylene insert displacement and prosthesis loosening or infection. In addition, there were no significant differences in the postoperative OKS scores between the two patient groups. The two aforementioned evaluation methods might be unable to assess the postoperative differences between the MB and FB prostheses. However, joint kinematics analysis may detect the differences between two groups. So, it may be a more reliable evaluation indicator. In the present study, we used the Opti-Knee® three-dimensional knee joint movement analysis system to employ gait analysis as an evaluation method for joint kinematics. Currently, this technology is used in research on articular structural damage, joint mobility analysis, and comparative studies on postoperative efficacy, among others [32], [33].
In this study, patients in the FB group were older and demonstrated lower BMI than patients in the MB group. In addition, the BMI/age ratio of the FB group was significantly lower than the MB group (p < 0.05). Osmani et al. reported that the BMI/age ratio can be used as a reference standard for selecting prosthesis and proposed that there is no need to use ‘higher demand’ prostheses for patients with a low BMI/age ratio [6].Young people need higher-demand activities, and heavier patients may need to use ‘high-demand’ prosthesis to reduce the components' wear during walking. MB might be recommended for the high BMI/age ratio patients. Amaro et al.'s study concluded that MB TKA allowed a higher degree of axial tibiofemoral rotation when walking, stepping up stair steps, and standing up from a chair and had higher functional outcomes compared with FB TKA at 1-year follow-up by knee kinematics analysis. But, they did not compare with the healthy group [34]. Zürcher et al. supported that MB had significant more axial femorotibial rotation versus FB TKA during gait, sit to walk straight, and sit to walk turning [19]. But the present study only tested the gait characteristics when walking on flat ground. MB may be more suitable for these high-demand activities at all events.
Various parameters of knee gait characteristics postoperatively in the present study were closer to the healthy control group compared with the preoperative ones. With regards to angles of motion, the maximum value and range of mobility of the flexion/extension angle in the FB and MB groups increased after surgery compared with before surgery, while the maximum genu varum and internal rotation of the two groups decreased after surgery. TKA plays a positive role in improving the gait characteristics and joint function of patients. But, these parameters of both the FB and MB groups postoperatively were still lower than the healthy control group, except for the maximum internal rotation of the MB group increased significantly compared with the healthy control group (p = 0.007). Meanwhile, the range of motion of internal/external rotation in the MB group increased postsurgery but lower than the healthy one. Bytyqi et al. studied joint kinematic characteristics during gait in medial knee osteoarthritis patients who underwent TKA and received posterior-stabilising prostheses. They concluded that the range of flexion/extension was improved significantly after TKA, but it still remained lower than control group. The range of motion in internal–external rotation did not change prearthroplasty and postarthroplasty but remained lower than the matched control group [35].Their results were partly the same as ours. Urwin et al. compared three-dimensional spatiotemporal, kinematic, and kinetic parameters during walking to examine whether MBs offer functional advantages over FB designs. They did not find any differences between two groups in the spatiotemporal parameters, with both groups indicative of similar differences when compared with normal knee biomechanics at 9 months postsurgery [18].The new findings in the present study which were different from the above literatures were that the maximum internal rotation of the MB group after TKA was even larger than the healthy group. The MB might be a better choice for the poor rotation of the tibial prosthesis placement in TKA. This design could compensate for the rotational mismatch of femur and tibia during walking. With regards to displacement, the anterior displacement of the tibia in two groups increased after surgery. The range of anterior–posterior displacement in the FB group also increased significantly after surgery (p = 0.016), as did the range of medial–lateral displacement in the MB group, significantly (p = 0.025). Bytyqi et al. concluded in their study that posterior displacement of the tibia after posterior-stabilising TKA was greater than the healthy control population [35].In the present study, we found that the postoperative anterior displacement of the tibia in both groups significantly increased postoperatively, which contradicted the results of Bytyqi et al. Uvehammer et al. found that the anterior displacement of the femur during low flexion gait increased after surgery compared with the normal population, regardless of the type of prostheses. However, they were unable to demonstrate the differences among concave prostheses, posterior cruciate ligament-retaining prosthesis, and alternative prostheses [36]. Another study found that the rotating MB prosthesis can improve the anteroposterior stability of the joint in the mid-flexion range [2].The current study found that the range of anterior–posterior displacement in both groups increased postoperatively, although this range in MB group was not statistically significant. It was still lower than that of the healthy control group. In general, anterior–posterior displacements should be stabilised in posterior-stabilising TKA because of cruciate ligament-substituting. Based on the above literatures, the anterior–posterior displacements both increased after surgery, which was consistent with ours. In addition, these results did not exceed the normal range, the anterior-posterior stability after TKA was still excellent. Unfortunately, MB did not have an advantage over FB in terms of anterior–posterior displacement in the present study. Therefore, the knee joint displacement cannot be used as a reliable reference marker for prosthesis selection.
In summary, although there was insufficient evidence to suggest that the MB prosthesis is a better option for patients with medial knee osteoarthritis, the MB prosthesis might be a desirable choice for patients who are young, obese, have high-performance activity requirements, or have the malrotation of the tibial prosthesis placement.
This study has several limitations. First, the three-dimensional knee joint gait movement analysis system employed in this study uses 7 body surface markers to label the knee movement trajectory. Compared with conventional VICON gait analysis, the accuracy of this system in assessing axial rotation is poorer. During examination, we only collected gait data when walking on flat ground and did not collect gait data for upslope walking, downslope walking, standing up, and other higher functional activities. In addition, the follow-up duration is relatively short, and gait data were collected only once in about 7.5 months after surgery. Therefore, measurement errors and selection bias may be present.
Conclusion
In summary, the current study demonstrated that TKA can make the parameters of knee gait characteristics closer to the normal population. Medial knee osteoarthritis patients who received a MB prosthesis in total knee arthroplasty had better joint flexion function and axial rotation than the FB one. However, there is insufficient evidence to suggest that the MB prosthesis is a better option for patients with medial knee osteoarthritis. The MB prosthesis might be a desirable choice for patients who are young, obese, have high-performance activity requirements, or have the malrotation of the tibial prosthesis placement.
Conflicts of interest statement
The author(s) have no conflicts of interest relevant to this article.
Funding statement
This research received the grant from funding “Development and application of Internet + shoulder arthroscopy registration system” (YG2017MS05) and “Shanghai Clinical Medical Center (2017ZZ01023), Shanghai Municipal Key Clinical Specialty.
Acknowledgements
The authors thank the staff members of Shanghai Innomotion, Inc, for their kind assistance with our study.
Contributor Information
Jun Zhang, Email: jeferry717717@163.com.
You Wang, Email: drwangyou@163.com.
References
- 1.Chang A., Hurwitz D., Dunlop D., Song J., Cahue S., Hayes K. The relationship between toe-out angle during gait and progression of medial tibiofemoral osteoarthritis. Ann Rheum Dis. 2007;66(10):1271–1275. doi: 10.1136/ard.2006.062927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Minoda Y., Ikebuchi M., Mizokawa S., Ohta Y., Nakamura H. Mobile-bearing TKA improved the anteroposterior joint stability in mid-flexion range comparing to fixed-bearing TKA. Arch Orthop Trauma Surg. 2016;136(11):1601–1606. doi: 10.1007/s00402-016-2567-9. [DOI] [PubMed] [Google Scholar]
- 3.Vahtrik D., Ereline J., Gapeyeva H., Paasuke M. Postural stability in relation to anthropometric and functional characteristics in women with knee osteoarthritis following total knee arthroplasty. Arch Orthop Trauma Surg. 2014;134(5):685–692. doi: 10.1007/s00402-014-1940-9. [DOI] [PubMed] [Google Scholar]
- 4.Papagiannis G.I., Roumpelakis I.M., Triantafyllou A.I., Makris I.N., Babis G.C. No differences identified in transverse plane biomechanics between medial pivot and rotating platform total knee implant designs. J Arthroplast. 2016;31(8):1814–1820. doi: 10.1016/j.arth.2016.01.050. [DOI] [PubMed] [Google Scholar]
- 5.Liu Q., Wang S., Lin J., Zhang Y. The burden for knee osteoarthritis among Chinese elderly: estimates from a nationally representative study. Osteoarthr Cartil. 2018;26(12):1636–1642. doi: 10.1016/j.joca.2018.07.019. [DOI] [PubMed] [Google Scholar]
- 6.Osmani F.A., Bolz N., Odeh K., Bearison C., Schwarzkopf R., Iorio R. The ratio of patient body mass index to age: a cost-effective implant selection guideline for total knee arthroplasty. Arthroplasty today. 2018;4(1):94–98. doi: 10.1016/j.artd.2017.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Buechel F.F., Pappas M.J. The New Jersey Low-Contact-Stress Knee Replacement System: biomechanical rationale and review of the first 123 cemented cases. Arch Orthop Trauma Surg. 1986;105(4):197–204. doi: 10.1007/BF00435480. [DOI] [PubMed] [Google Scholar]
- 8.Ranawat C.S., Komistek R.D., Rodriguez J.A., Dennis D.A., Anderle M. In vivo kinematics for fixed and mobile-bearing posterior stabilized knee prostheses. Clin Orthop Relat Res. 2004;(418):184–190. doi: 10.1097/00003086-200401000-00030. [DOI] [PubMed] [Google Scholar]
- 9.Abdel M.P., Tibbo M.E., Stuart M.J., Trousdale R.T., Hanssen A.D., Pagnano M.W. A randomized controlled trial of fixed- versus mobile-bearing total knee arthroplasty. The bone & joint journal. 2018;100-B(7):925–929. doi: 10.1302/0301-620X.100B7.BJJ-2017-1473.R1. [DOI] [PubMed] [Google Scholar]
- 10.Ferguson K.B., Bailey O., Anthony I., James P.J., Stother I.G., B M.J.G. A prospective randomised study comparing rotating platform and fixed bearing total knee arthroplasty in a cruciate substituting design--outcomes at two year follow-up. The Knee. 2014;21(1):151–155. doi: 10.1016/j.knee.2013.09.007. [DOI] [PubMed] [Google Scholar]
- 11.Schotanus M.G.M., Pilot P., Kaptein B.L., Draijer W.F., Tilman P.B.J., Vos R. No difference in terms of radiostereometric analysis between fixed- and mobile-bearing total knee arthroplasty: a randomized, single-blind, controlled trial. Knee Surg Sports Traumatol Arthrosc. 2017;25(9):2978–2985. doi: 10.1007/s00167-016-4138-6. [DOI] [PubMed] [Google Scholar]
- 12.Shi X., Shen B., Yang J., Kang P., Zhou Z., Pei F. In vivo kinematics comparison of fixed- and mobile-bearing total knee arthroplasty during deep knee bending motion. Knee Surg Sports Traumatol Arthrosc. 2014;22(7):1612–1618. doi: 10.1007/s00167-012-2333-7. [DOI] [PubMed] [Google Scholar]
- 13.Delport H.P., Banks S.A., De Schepper J., Bellemans J. A kinematic comparison of fixed- and mobile-bearing knee replacements. J Bone Joint Surg Br Vol. 2006;88(8):1016–1021. doi: 10.1302/0301-620X.88B8.17529. [DOI] [PubMed] [Google Scholar]
- 14.Shi K., Hayashida K., Umeda N., Yamamoto K., Kawai H. Kinematic comparison between mobile-bearing and fixed-bearing inserts in NexGen legacy posterior stabilized flex total knee arthroplasty. J Arthroplast. 2008;23(2):164–169. doi: 10.1016/j.arth.2007.01.009. [DOI] [PubMed] [Google Scholar]
- 15.Dennis D.A., Komistek R.D., Mahfouz M.R., Walker S.A., Tucker A. A multicenter analysis of axial femorotibial rotation after total knee arthroplasty. Clin Orthop Relat Res. 2004;(428):180–189. doi: 10.1097/01.blo.0000148777.98244.84. [DOI] [PubMed] [Google Scholar]
- 16.Liu F., Ohdera T., Miyamoto H., Wasielewski R.C., Komistek R.D., Mahfouz M.R. In vivo kinematic determination of total knee arthroplasty from squatting to standing. The Knee. 2009;16(2):116–120. doi: 10.1016/j.knee.2008.10.011. [DOI] [PubMed] [Google Scholar]
- 17.Wolterbeek N., Nelissen R.G., Valstar E.R. No differences in in vivo kinematics between six different types of knee prostheses. Knee Surg Sports Traumatol Arthrosc. 2012;20(3):559–564. doi: 10.1007/s00167-011-1605-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Urwin S.G., Kader D.F., Caplan N., St Clair Gibson A., Stewart S. Gait analysis of fixed bearing and mobile bearing total knee prostheses during walking: do mobile bearings offer functional advantages? The Knee. 2014;21(2):391–395. doi: 10.1016/j.knee.2013.10.007. [DOI] [PubMed] [Google Scholar]
- 19.Zurcher A.W., van Hutten K., Harlaar J., Terwee C.B., Rob Albers G.H., Poll R.G. Mobile-bearing total knee arthroplasty: more rotation is evident during more demanding tasks. The Knee. 2014;21(5):960–963. doi: 10.1016/j.knee.2014.05.007. [DOI] [PubMed] [Google Scholar]
- 20.周欣, 韦民, 王伟 高屈曲度固定平台和高屈曲度旋转平台膝关节假体置换后的早期步态比较. 中国组织工程研究. 2011;15(43):8023–8026. [Google Scholar]
- 21.马成才, 刘冰, 李小娜, 廖中亚 固定平台与旋转平台假体全膝关节表面置换术治疗膝关节骨性关节炎的早期疗效观察. 中国基层医药. 2014;21(8):1159–1161. [Google Scholar]
- 22.肖俊, 张朝贵, 唐广满, 许科峰, 刘卫峰 汪建良. 活动平台与固定平台全膝关节置换的比较研究. 实用骨科杂志. 2013;19(12):1075–1077. [Google Scholar]
- 23.Guler O., Perwog M., Kral F., Schwarm F., Bardosi Z.R., Gobel G. Quantitative error analysis for computer assisted navigation: a feasibility study. Med Phys. 2013;40(2) doi: 10.1118/1.4773871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Whitehouse S.L., Blom A.W., Taylor A.H., Pattison G.T., Bannister G.C. The Oxford knee score; problems and pitfalls. The Knee. 2005;12(4):287–291. doi: 10.1016/j.knee.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 25.Mockel G., Perka C., Gabler J., Zippel H. Early postoperative functional differences between total knee arthroplasties supplied with mobile-bearing platform or fixed-bearing system--an analysis of gait pattern. Zeitschrift fur Orthopadie und ihre Grenzgebiete. 2004;142(1):40–45. doi: 10.1055/s-2004-818028. [DOI] [PubMed] [Google Scholar]
- 26.Kramers-de Quervain I.A., Stussi E., Muller R., Drobny T., Munzinger U., Gschwend N. Quantitative gait analysis after bilateral total knee arthroplasty with two different systems within each subject. J Arthroplast. 1997;12(2):168–179. doi: 10.1016/s0883-5403(97)90063-2. [DOI] [PubMed] [Google Scholar]
- 27.Fransen B.L., van Duijvenbode D.C., Hoozemans M.J.M., Burger B.J. No differences between fixed- and mobile-bearing total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2017;25(6):1757–1777. doi: 10.1007/s00167-016-4195-x. [DOI] [PubMed] [Google Scholar]
- 28.Okamoto N., Nakamura E., Nishioka H., Karasugi T., Okada T., Mizuta H. In vivo kinematic comparison between mobile-bearing and fixed-bearing total knee arthroplasty during step-up activity. J Arthroplast. 2014;29(12):2393–2396. doi: 10.1016/j.arth.2014.02.022. [DOI] [PubMed] [Google Scholar]
- 29.Wang W.J., Sun M.H., Palmer J., Liu F., Bottomley N., Jackson W. Patterns of compartment involvement in end-stage knee osteoarthritis in a Chinese orthopedic center: implications for implant choice. Orthop Surg. 2018;10(3):227–234. doi: 10.1111/os.12395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Powell A.J., Crua E., Chong B.C., Gordon R., McAuslan A., Pitto R.P. A randomized prospective study comparing mobile-bearing against fixed-bearing PFC Sigma cruciate-retaining total knee arthroplasties with ten-year minimum follow-up. Bone Joint J. 2018;100-B(10):1336–1344. doi: 10.1302/0301-620X.100B10.BJJ-2017-1450.R1. [DOI] [PubMed] [Google Scholar]
- 31.Kim Y.H., Park J.W., Kim J.S. The long-term results of simultaneous high-flexion mobile-bearing and fixed-bearing total knee arthroplasties performed in the same patients. J Arthroplast. 2019;34(3):501–507. doi: 10.1016/j.arth.2018.11.007. [DOI] [PubMed] [Google Scholar]
- 32.翟永喜, 叶劲, 陈艺, 白波, 卢伟杰, 姚咏嫦 单髁与全膝关节置换术治疗膝内侧骨关节炎术后步态对比研究. 中华关节外科杂志(电子版) 2017;11(1):9–16. [Google Scholar]
- 33.Yao Z.L., Wang S.B., Zhang Y., Huang W.H., Shen H.Y., Ma L.M. Clinical significance of a novel knee joint stability assessment system for evaluating anterior cruciate ligament deficient knees. Orthop Surg. 2016;8(1):75–80. doi: 10.1111/os.12225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Amaro J.T., Novaretti J.V., Astur D.C., Cavalcante E.L.B., Rodrigues Junior A.G., Debieux P. Higher axial tibiofemoral rotation and functional outcomes with mobile-bearing compared with fixed-bearing total knee arthroplasty at 1- but not at 2-year follow-up - a randomized clinical trial. J Knee Surg. 2019 doi: 10.1055/s-0039-1678675. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 35.Bytyqi D., Shabani B., Cheze L., Neyret P., Lustig S. Does a third condyle TKA restore normal gait kinematics in varus knees? In vivo knee kinematic analysis. Arch Orthop Trauma Surg. 2017;137(3):409–416. doi: 10.1007/s00402-017-2629-7. [DOI] [PubMed] [Google Scholar]
- 36.Uvehammer J., Karrholm J., Brandsson S. In vivo kinematics of total knee arthroplasty. Concave versus posterior-stabilised tibial joint surface. J Bone Joint Surg Br Vol. 2000;82(4):499–505. doi: 10.1302/0301-620x.82b4.10651. [DOI] [PubMed] [Google Scholar]