Abstract
Background and objective
Existing orthopaedic robotic systems are almost restricted to provide guidance for trajectory direction. In the present study, a novel spinal robotic system with automatic drilling power was introduced. The aim of this study is to evaluate the feasibility and safety in pedicle screw insertion of posterior lumbar interbody fusion assisted by this novel robotic system.
Methods and materials
A randomised controlled trial was conducted for 17 participants who were required posterior lumbar interbody fusion process. Seven (3 M/4 F) were randomly assigned to the robot-assisted group (RA group), and the other ten (4 M/6 F) were assigned to the conventional technique group (FH group). A novel robotic system was used in the RA group. All measurements were based on postoperative computed tomography (CT) data. Accuracy of screw insertion was determined using the Gertzbein and Robbins Scale. Precision was measured by the entry point deviation distance and the trajectory rotation. Other variables included operation time, radiation time, length of stay, and screw-related complications.
Result
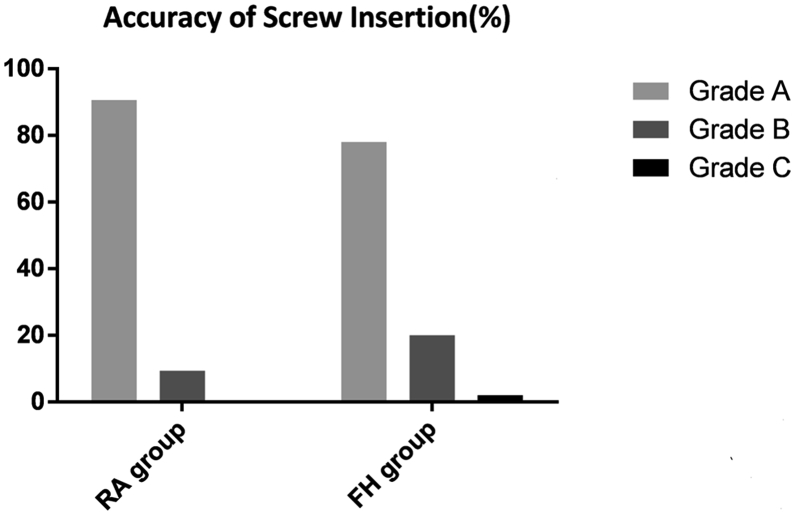
A total of 82 pedicle screws were placed in the 17 participants. In the RA group, 90.6% of screws placed were Grade A, and 9.4% were Grade B. In the FH group, 78.0% of screws were Grade A, 20.0% were Grade B, and 2.0% were Grade C. No statistical difference was found in the operation time, radiation time per case, and length of stay between both groups. The radiation time per screw is significantly lower in the RA group. No screw-related complications or revision occurred in the present study.
Conclusion
The outcome of screw accuracy of this robotic system was comparable with that of experienced surgeons, and no screw-related complication was found in the RA group during hospitalisation. In addition, radiation time per screw in the robotic group was significantly lower than that in the conventional group, which shows the potential to reduce radiation exposure of pedicle screw fixation assisted by this robotic system.
Translational potential
Our study shows that pedicle screw fixation assisted by “Orthbot” system is accurate and safe. It is concluded that this novel robotic system offers a new option for internal implantation in spine surgery.
Keywords: Robotic system, Pedicle screw fixation, Posterior lumbar interbody fusion, Preoperative planning, Accurcay
Background
Pedicle screw insertion is widely used in posterior lumbar fusion for spinal stabilisation. Conventional internal fixation procedure, with free-hand tools, is based on anatomical landmarks and intraoperative fluoroscopic images [1]. Although this method has been shown to be safe and used worldwide, screw misplacement rates vary greatly among previous research studies [2], [3], [4], [5], [6]. Malposition of the screw may result in severe surgical complications, such as vascular or visceral damage, neurological deficit, and dural tearing [3], [7]. To acquire higher accuracy in pedicle screw placement, several techniques have been introduced. Computer-assisted system [8], [9] or three-dimensional (3D) fluoroscopy–based system [10] seems to be effective to improve screw position in earlier literature. The robotic system, developed as a newer navigation technique with high intrinsic precision and stability, has obtained popularity in a multitude of spinal internal fixation procedures [11]. Current research tends to pay close attention to Renaissance (Mazor Robotics Ltd, Caesarea, Israel) [12], SpineAssist (Mazor Robotics Ltd, Caesarea, Israel) [13], ROSA spine (Zimmer Biomet, Warsaw, Indiana) [14], and the TiRobot system (TINAVI Medical Technologies Co. Ltd, Beijing, China) [15]. However, these robotic systems seem to be limited to provide the position of trajectory guiding surgeons to insert K-wires and screw manually. In the present study, a novel spinal robotic system with automatic drilling power is introduced. The aim of this study is to evaluate the feasibility and safety in the insertion of pedicle screws for posterior lumbar interbody fusion assisted by this robotic technique.
Methods and materials
Approved by the Southern Medical University Ethics Committee, the patient recruitment for this randomised controlled trial was performed from August 2018 to December 2018 in our single medical centre. Informed consent was obtained from each individual participant in our study. Those who do not have any mental disorders were enrolled, and all of them signed the informed consent form in a clear-conscious situation without any temptation. Patients who required lumbar interbody fusion and pedicle screw fixation treatments for degenerative lumbar disc disease were prospectively included in the study and randomly divided into two groups. Patients in the “Orthbot” group were consecutively treated under robotic assistance (RA group), while the other patients in the conventional technique group were treated with free-hand approach assisted by intraoperative fluoroscopy equipment (FH group).
Patients
Inclusion criteria were as follows: (1) age between 18 and 65 years; (2) indication of posterior fusion for degenerative lumbar disc disease or lumbar spinal stenosis; (3) signed informed consent to accept the subsequent randomised trial process. Exclusion criteria were as follows: (1) patients with severe degenerative spinal deformity; (2) patients with a previous surgery on the lumbar spine; (3) patients with coagulopathy or metal allergy; (4) pregnant or lactating women; (5) patients who participated in relevant clinical trials of other drugs or medical devices in the past 3 months. We prospectively enrolled 17 participants, 7 males and 10 females, aged 23–63 years. Seven (3 males and 4 females) were randomly assigned to the RA group, and the other 10 (4 males and 6 females) were assigned to the FH group.
Robotic procedure
Based on machine vision tracking algorithm, the “Orthbot” system (Fig. 1), which is comprised of a robotic workstation, coordinate position plate, tracking camera (Fig.2a) and a 6-degree of freedom (6-DOF) robotic arm with an automatic bone drill (Fig. 2b), can finish inserting a K-wire autonomously by following the preoperative planning of screw trajectory. The working procedure is as follows.
Figure 1.
Main composition of the “Orthbot” system: a robotic arm with a tracking camera and an automatic bone drill, a surgical planning workstation, and a coordinate position plate.
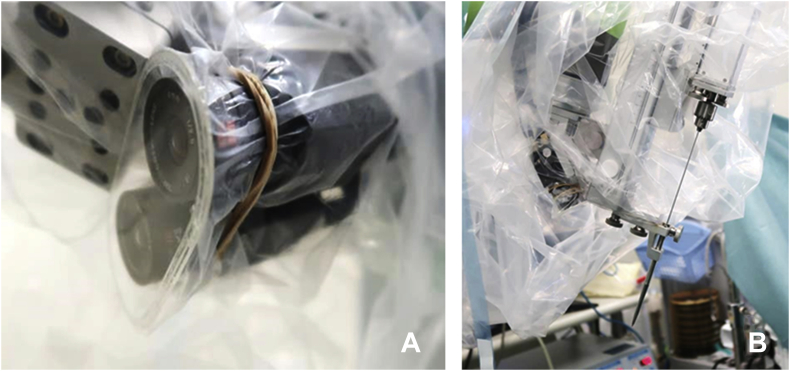
Figure 2.
Photographs of the (A) tracking camera and (B) the automatic bone drill set on the robotic arm.
Preoperative planning
A thin-cut (1 mm) computed tomography (CT) scan was performed for each patient before surgery. The CT images were saved in the digital imaging and communications in medicine (DICOM) file format and transferred to the “Orthbot” system's proprietary software in the planning workstation. The workstation was used to integrate preoperative planning, image acquisition and registration, kinematic calculations, and supervisory control. After the reconstruction of CT data into a 3D model, surgeons could formulate and modify the preoperative plan with appropriate screw sizes and optimal trajectory position in coronal, sagittal, and axial planes (Fig. 3).
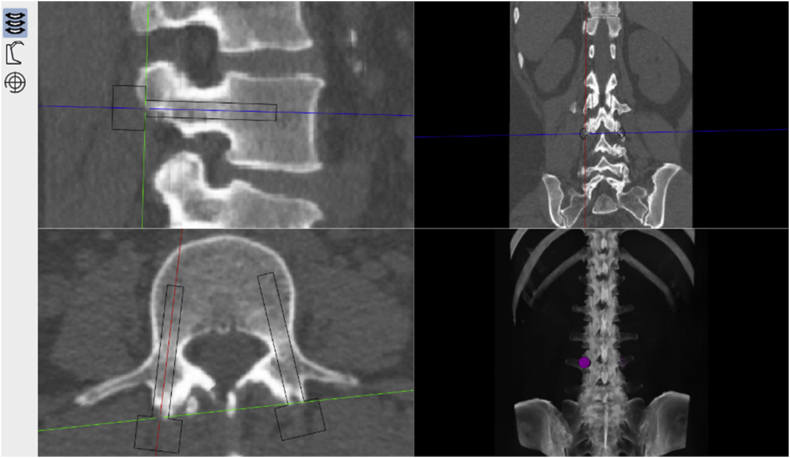
Figure 3.
Screw planning performed in the workstation based on the preoperative CT reconstruction data. CT = computed tomography.
Registration
Patients, after receiving general anaesthesia, were placed in prone position. Surgeons assembled the coordinate position plate and set it up above the surgical area. Anteroposterior and lateral fluoroscopic images were required by the C-arm to match with the preoperative CT data for registration. Surgeons’ inspection for registration outcomes was of utmost importance to ensure that the surgical plan had been precisely imported into the robotic system.
Robotic position and drilling procedure
In the RA group, first, the “Orthbot” system was passively positioned alongside the surgical table. The tracking camera then guided the robotic arm into the surgical site by recognising the marker sign set on the coordinate position plate. The automatic bone drill thereafter began to make a channel into the target pedicle, and a K-wire was placed subsequently by following the trajectory in the surgical planning. After all K-wires were inserted, the surgical arm is cleared off the region. Surgeons finally finished inserting screws over each K-wire. The primary surgical procedures in the RA group are shown in Fig. 4.
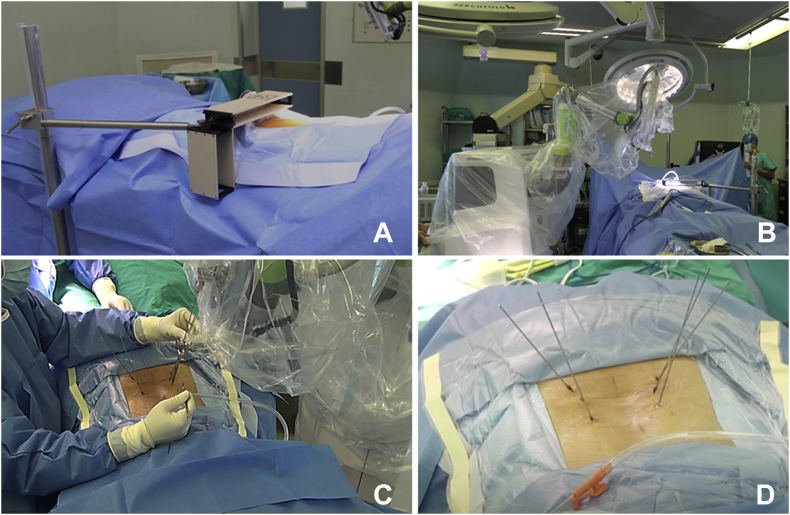
Figure 4.
(A) The coordinate position plate was assembled by fellows and set up above the surgical area for registration; (B) the robotic arm of the “Orthbot” system was passively positioned alongside the surgical table; (C) supervised by surgeons, k-wires were placed by the “Orthbot” system automatically during the operation; (D) K-wires were finished inserting, and the robotic system was cleared off the surgical field.
Conventional surgical procedure
In the conventional technique group, experienced surgeons insert K-wires and screws according to routine processes by a fluoroscopy-guided technique.
Evaluation and data collection
All patients required postoperative CT scans. The CT reconstructed images with actual screws position were also loaded on to the workstation to compare the deviation from the planned trajectories. Precision assessment of the “Orthbot” system depended on two parameters—the deviation distance of the entry point and the rotation angle of the trajectory. Based on the 3D surgical space coordinate system constructed in the robotic workstation, entry point position and trajectory location were transformed to numerical parameters with X-value, Y-value, and Z-value. Three-dimensional measurements of these two parameters were also performed in the proprietary software (Fig. 5). Meanwhile, each screw position was appraised by the Gertzbein and Robbins Classification Scale to obtain the evaluation of accuracy. In the Gertzbein and Robbins Scale [16], Grade A indicated no perforation of the pedicle; Grade B indicated<2 mm of perforation of the pedicle; Grade C indicated 2–4 mm of perforation of the pedicle; and Grade D indicated >4 mm of perforation. Grades A and B were considered clinically satisfactory. All of the evaluation was assessed by an independent author who was blinded to patients’ allocation after receiving the postoperative CT data. Other perioperative variables collected included operation time, blood loss, radiation time (radiation time per case and per screw), length of stay, and screw-related complications (e.g., neurologic deficit, vital vascular injury, and revision surgery).
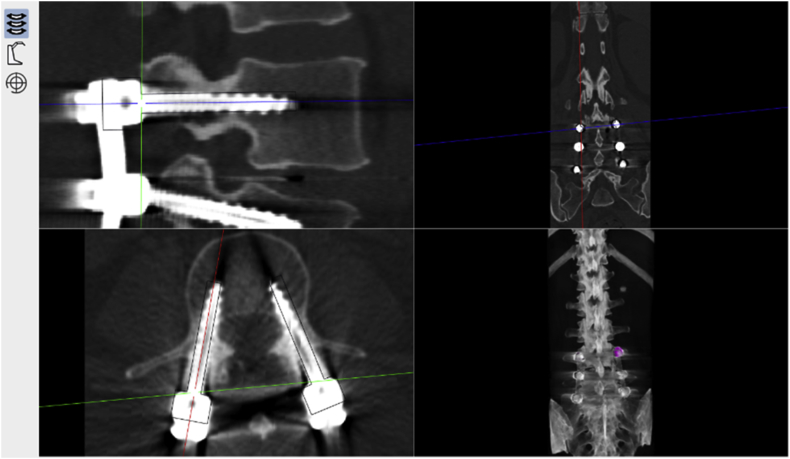
Figure 5.
Screw accuracy and precision (based on the entry point and trajectory) were evaluated on the postoperative CT images (one of the robot-assisted groups). CT = computed tomography.
Statistical analysis
Quantitative data were expressed as mean ± standard deviation (SD). The two-sample t test was used to compare continuous variables between the two groups, and the Fisher exact test was used for ranked variables. Alpha was set at 0.05, while P-values<0.05 was considered statistically significant.
Result
There were 17 participants enrolled in the randomised controlled trial for treatment by posterior lumbar interbody fusion. The median age of these patients was 50.0 years, and the confidence interval was 48.9 ± 11.4 years (ranging from 23 to 63 years). The median body mass index was 24.3 kg/m2, and the confidence interval was 24.5 ± 2.3 kg/m2 (ranging from 20.7 to 30.5 kg/m2). Demographic data collected are shown in Table 1. A total of 82 pedicle screws were placed in the study. In the RA group, according to the Gertzbein and Robbins Scale, 29 of 32 screws placed were Grade A, and 3 were Grade B. In the FH group, 39 of 50 screws were Grade A, 10 were Grade B, and 1 was Grade C (p>0.05) (Table 2, Table 3). A comparison of the screw position according to the Gertzbein and Robbins Classification Scale in each group is presented in Fig. 6. However, the deviation distance of entry point (p<0.001) and the rotation angle of the trajectory (p<0.001) were both significantly lower in the RA group (Table 4). There were no statistical differences in the operation time (p = 0.620), blood loss (p = 0.878), radiation time per operation (p = 0.291), and length of stay (p = 0.811) between both groups. But radiation time per screw is significantly lower in the RA group (0.56 s in the RA group and 1.04 s in the FH group, p<0.05) (Table 5). No screw-related complications occurred, and no intraoperative or postoperative revision was necessary for either group.
Table 1.
Demographic data of the study cohort.
| Characteristic | RAG (n = 7) | FHG (n = 10) | P-value |
|---|---|---|---|
| Gender (male/female) | 3/4 | 4/6 | 1.000 |
| Age (median; M ± SD) (y) | 48.0; 47.4 ± 12.9 | 51.5; 49.9 ± 10.9 | 0.675 |
| BMI (median; M ± SD) (kg/m2) | 24.3; 24.3 ± 1.8 | 24.0; 24.6 ± 2.6 | 0.773 |
| Diagnosis (no. patients, percentage) | |||
| Degenerative disc disease | 5 (71.4%) | 6 (60.0%) | |
| Lumbar spinal stenosis | 2 (28.6%) | 4 (40.0%) | |
FHG = free-hand technique group (conventional group); M = mean; RAG = “Orthbot”-assisted group; SD = standard deviation.
Table 2.
Grading assessment for screw position of each patient.
| Patient | Group | Screw (n) | Grade of screw |
||
|---|---|---|---|---|---|
| A | B | C | |||
| 1 | FHG | 4 | 4 | 0 | 0 |
| 2 | FHG | 6 | 4 | 2 | 0 |
| 3 | RAG | 4 | 3 | 1 | 0 |
| 4 | RAG | 6 | 6 | 0 | 0 |
| 5 | RAG | 4 | 3 | 1 | 0 |
| 6 | FHG | 4 | 4 | 0 | 0 |
| 7 | FHG | 6 | 5 | 1 | 0 |
| 8 | FHG | 4 | 2 | 2 | 0 |
| 9 | FHG | 4 | 3 | 1 | 0 |
| 10 | RAG | 4 | 4 | 0 | 0 |
| 11 | RAG | 4 | 4 | 0 | 0 |
| 12 | FHG | 4 | 1 | 2 | 1 |
| 13 | RAG | 4 | 3 | 1 | 0 |
| 14 | RAG | 6 | 6 | 0 | 0 |
| 15 | FHG | 4 | 3 | 1 | 0 |
| 16 | FHG | 8 | 8 | 0 | 0 |
| 17 | FHG | 6 | 5 | 1 | 0 |
RAG = “Orthbot”-assisted group; FHG = free-hand technique group (conventional group).
No Grade D was evaluated in both the two groups.
Table 3.
Grading assessment for screw position of each group.
| Grade | RAG (n = 32) | FHG (n = 50) | Total (n = 82) | P-value |
|---|---|---|---|---|
| A | 29 (90.6%) | 39 (78.0%) | 68 (82.9%) | 0.138 |
| B | 3 (9.4%) | 10 (20.0%) | 13 (15.9%) | 0.199 |
| A + B | 32 (100.0%) | 49 (98.0%) | 81 (98.8%) | 1.000 |
| C | 0 | 1 (2.0%) | 1 (1.2%) | 1.000 |
RAG = “Orthbot”-assisted group; FHG = free-hand technique group (conventional group).
No Grade D was evaluated in both the two groups.
Figure 6.
A bar graph of comparison of the percentage for the accuracy on screw insertion between two groups in the study. Grades were determined by the Gertzbein and Robbins Classification Scale.
Table 4.
Precision parameters measurement of each study group.
| Parameters | RAG | FHG | P-value |
|---|---|---|---|
| EPD (M ± SD) (mm) | 0.70 ± 0.33 | 4.16 ± 2.21 | 0.000 |
| TRA (M ± SD) (°) | 1.3 ± 0.8 | 11.9 ± 5.6 | 0.000 |
EPD = entry point deviation; FHG = free-hand technique group (conventional group); M = mean; RAG = “Orthbot”-assisted group; SD = standard deviation; TRA = trajectory rotation angle.
Table 5.
Perioperative variables of each study group.
| Variables | RAG | FHG | P-value |
|---|---|---|---|
| ORT (M ± SD) (min) | 289 ± 87 | 266 ± 92 | 0.620 |
| BL (M ± SD) (ml) | 257 ± 181 | 245 ± 140 | 0.878 |
| RTC (M ± SD) (s) | 7.29 ± 1.80 | 9.00 ± 3.83 | 0.291 |
| RTS (M ± SD) (s) | 0.56 ± 0.20 | 1.04 ± 0.62 | 0.000 |
| LOS (M ± SD) (days) | 13.1 ± 2.8 | 12.8 ± 3.2 | 0.811 |
BL = blood loss; FHG = free-hand technique group (conventional group); LOS = length of stay; M = mean; ORT = operation time; RAG = “Orthbot”-assisted group; RTC = radiation time per case; RTS = radiation time per screw; SD = standard deviation.
Discussion
Commonly, procedures of spinal surgery require meticulous manipulation to avoid complications due to screw misplacement. Spinal surgeons, currently, depend on the visualisation of anatomical landmarks and guidance of two-dimensional fluoroscopy technique to determine screw position. However, the length of the spinal surgery may often lead to performance fatigue, which potentially affects the screw position. With high intrinsic precision and stability, a robotic system can significantly improve surgical dexterity and show its advantages on assisting spinal procedures [17]. In the meantime, several pieces of research have shown that elimination of the reliance on hand–eye coordination and continuous concentration can effectively increase the accuracy of implant insertion and reduce the incidence of screw-related complications when using robotic systems [18], [19], [20]. However, existing robotic systems almost guide the direction of the trajectory by a cannula and surgeons insert K-wires and screws manually. In the present study, we introduce a novel robotic platform with automatic drilling power. To our knowledge, this is the first report of the series for medical robotic technology.
Accuracy and precision
The accuracy of pedicle screw fixation with the conventional technique has been studied in several earlier research studies. Karapinar et al. [21] evaluated 640 transpedicular screws in the thoracolumbar spine and showed the percentage of pedicle violated reach 5.8%. Jutte and Castelein [3] found a similar result on screw misplacement rate (6.5%) in 105 consecutive primary operations. When assisted by a navigation system, screw position turned better. A meta-analysis had been conducted to study the accuracy of pedicle screw placement with navigation. It found 11% increase in accuracy in inserting a lumbar pedicle screw in the navigation-assisted group, compared with no-navigation group [6].
The robotic system was developed as a high-precision technique to improve the outcome of implant placement. These years, a large number of studies report the affirmative effect on robot-assisted screw fixation. Schatlo et al. [22] observed 83.6% of screws were evaluated as perfect trajectories (Grade A) and 7.8% of screws were Grade B, based on the Gertzbein and Robbins Scale. There was no difference between the robot-assisted group and fluoroscopy-guided group on comparison on “clinically acceptable” (screws in Grades A and B). A similar result was later confirmed by Solomiichuk et al. [23], who found 84.4% of trajectories were Grade A or B in their study with robotic guidance provided by the SpineAssist system. On the contrary, the opposite result came out in a randomised comparison conducted by Ringel et al. [24]. In their study, 93% of screws had acceptable positions in the free-hand group, while 85% in the robotic group. Attachment of the robot to the spine seemed like a potential risk factor giving rise to screw malposition. In addition, Han et al. [25] designed an experiment to assess the precision of the “TiRobot” system by measuring the deviations of both the entry points and the end point. They found out the average deviations were 1.4 ± 0.9 mm for the entry point and 1.6 ± 1.0 mm for the end point.
In our study, we enrolled 17 participants into the prospective randomised controlled trial. Seven patients were randomly assigned to the RA group, and the other 10 were assigned to the FH group. Accuracy evaluation depended on the Gertzbein and Robbins Scale, and precision measurement followed 3D measurements of the entry point deviation and the trajectory rotation angle. Comparing with the FH group, the RA group showed no statistical difference in the rate of acceptable trajectories (Grade A and B). But we achieved a significant reduction on the entry point deviation (p<0.001) and the trajectory rotation angle (p<0.001) in the RA group. It indicated that the “Orthbot” system could definitely follow the preoperative plan to drill k-wires precisely for assisting pedicle screw fixation. Meanwhile, without using the axial and sagittal views, it is possible to measure precision parameters on the 3D surgical space coordinate system constructed by the “Orthbot” system, which is a newer concept we came up with in the present study.
Operation time
Operation time is an important variable to assess the effectiveness of a novel surgical technique. Theoretically, the robotic system is able to remarkably shorten the duration of the operation because it can directly finish a point-to-point task without overmuch adjustment. Schatlo et al. [22], however, found equal operation time between the robot-assisted group and the fluoroscopy-guided group, and Khan et al. [26] obtained the consistent finding when comparing robotic assistance and 3D CT navigation. Similar to several previous research studies, this study also detected a similar outcome in this part for these two groups during the experiment. In our opinion, the lack of a record on time-per-screw placement may be responsible for this situation. Different from the matched cohort study, it is difficult to restrictively equal the quantities of screw inserted in two randomised groups. Taking time-per-screw placement into account is compensation to correctly assess the impact on operation time of the robotic technique.
Radiation
It is widely concerned that radiation exposure is an exact hazard for the patient and the operating room personnel, especially orthopaedists [27]. Some articles confirmed the use of the robotic technique seems to reduce trajectory verification by fluoroscopic images after screw fixation [28], [29]. In the present study, average radiation time was 7.29 s per case in the robot-assisted group compared with 9.00 s per operation in the conventional technique group. But we detected average radiation time per screw was significantly lower in the robotic group (p<0.05). The main reason might be that overmuch C-arm exposure was used to inspect the accuracy of registration in the RA group because of inexperience in this new technique. In general, the radiation time per screw in the robotic group was significantly lower, which shows the potential to reduce radiation exposure of pedicle screw fixation assisted by this robotic system when more robot-assisted surgeries were conducted.
Complication
Pedicle screw malposition always increases the rate of complication. The major screw-related complications including vascular or visceral damages, neurologic deficits, and cerebrospinal fluid leakage are identified [7]. More attention had been paid on neurologic deficits in previous experiments of free-hand screw insertion technique. Davne and Myers [30] reported the rate of neural injury reached 1.1% in lumbar spine fusion, and Faraj and Webb [31] found a similar result (1.09%). A reduction to 0.7% was observed by Devito et al. [32] assisted by the robotic system. In the present experiment, we encountered 1 case of cerebrospinal fluid leakage in the robotic cohort. Because all the screws in this case were placed inside the pedicle cortex, other reasons were needed to explain for this complication. No vascular damage or neurologic injury occurred. In the meantime, no revision surgery was required in both two groups.
Limitation and expectation
There are some inherent limitations to our study. First, it is not enough to obtain generalizability of the results of our study with a small sample size. A primary reason is that we restrict indications involved in our study to obtain a preliminary evaluation of this robotic system. Deep research with a wider range of indications including cervical spondylosis, thoracic disease, and scoliosis will be required. Furthermore, time-per-screw placement was not documented, which made us fail to accurately estimate the influence on the operation time of this robotic platform. The study was a preliminary assessment of this novel robotic system which performs the pedicle screw insertion with high precision and stability. To our knowledge, this was the first clinical assessment about the accuracy and safety of this novel robotic technique. The unique automatic bone drilling system exhibits a new technology improving the operative technique compared with the conventional robotic system, which brought a new concept for surgical robotic technology changing it to an operative technique more than a guidance machine. Further studies with more cases performed are required to verify the accuracy of this novel system. With new applications or capabilities updated, in the future, the use of this system in spinal surgery clearly offers great promise.
Conclusion
We concluded that pedicle screw fixation procedure assisted by the “Orthbot” system was accurate and safe. All screws in the robotic group, with no complication, were determined to be of a clinically acceptable level, and screw accuracy of this robotic system was comparable with the outcomes intervened by experienced surgeons. Furthermore, the execution of the “Orthbot” system following the preoperative planning was more precise than surgeons, and we also found this robotic system has potential to reduce radiation exposure of pedicle screw fixation.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the 1964 Helsinki declaration, and the protocol was approved by the Institutional Review Board of Nanfang Hospital, Southern Medical University (IRB no. NFEC-2018-082).
Conflict of interest
The study was conducted under the cooperation of the Department of Spinal Surgery, Nanfang Hospital, and Xinjunte Smart Medical Equipment Co. Ltd, Shenzhen. All authors declared that they have no conflict of interests.
Acknowledgements
The study was supported by the Science and Technology Planning Project of Guangdong Province, China [2017B010110012].
References
- 1.Kuntz C., Maher P.C., Levine N.B., Kurokawa R. Prospective evaluation of thoracic pedicle screw placement using fluoroscopic imaging. J Spinal Disord Tech. 2004;17(3):206–214. doi: 10.1097/00024720-200406000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Carbone J.J., Tortolani P.J., Quartararo L.G. Fluoroscopically assisted pedicle screw fixation for thoracic and thoracolumbar injuries: technique and short-term complications. Spine (Phila Pa 1976) 2003;28(3):91–97. doi: 10.1097/00007632-200301010-00021. [DOI] [PubMed] [Google Scholar]
- 3.Jutte P.C., Castelein R.M. Complications of pedicle screws in lumbar and lumbosacral fusions in 105 consecutive primary operations. Eur Spine J. 2002;11(6):594–598. doi: 10.1007/s00586-002-0469-8. [DOI] [PubMed] [Google Scholar]
- 4.Castro W.H., Halm H., Jerosch J., Malms J., Steinbeck J., Blasius S. Accuracy of pedicle screw placement in lumbar vertebrae. Spine (Phila Pa 1976) 1996;21(11):1320–1324. doi: 10.1097/00007632-199606010-00008. [DOI] [PubMed] [Google Scholar]
- 5.Lonstein J.E., Denis F., Perra J.H., Pinto M.R., Smith M.D., Winter R.B. Complications associated with pedicle screws. J Bone Jt Surg Am. 1999;81(11):1519–1528. doi: 10.2106/00004623-199911000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Kosmopoulos V., Schizas C. Pedicle screw placement accuracy: a meta-analysis. Spine (Phila Pa 1976) 2007;32(3):E111–E120. doi: 10.1097/01.brs.0000254048.79024.8b. [DOI] [PubMed] [Google Scholar]
- 7.Lieber A.M., Kirchner G.J., Kerbel Y.E., Khalsa A.S. Robotic-assisted pedicle screw placement fails to reduce overall postoperative complications in fusion surgery. Spine J. 2019;19(2):212–217. doi: 10.1016/j.spinee.2018.07.004. [DOI] [PubMed] [Google Scholar]
- 8.Kotani Y., Abumi K., Ito M., Minami A. Improved accuracy of computer-assisted cervical pedicle screw insertion. J Neurosurg. 2003;99(3 Suppl):257–263. doi: 10.3171/spi.2003.99.3.0257. [DOI] [PubMed] [Google Scholar]
- 9.Wang H.C., Yang Y.L., Lin W.C., Chen W.F., Yang T.M., Lin Y.J. Computer-assisted pedicle screw placement for thoracolumbar spine fracture with separate spinal reference clamp placement and registration. Surg Neurol. 2008;69(6):597–601. doi: 10.1016/j.surneu.2007.04.006. discussion 601. [DOI] [PubMed] [Google Scholar]
- 10.Du J.P., Fan Y., Wu Q.N., Wang D.H., Zhang J., Hao D.J. Accuracy of pedicle screw insertion among 3 image-guided navigation systems: systematic review and meta-analysis. World Neurosurg. 2018;109:24–30. doi: 10.1016/j.wneu.2017.07.154. [DOI] [PubMed] [Google Scholar]
- 11.Bertelsen A., Melo J., Sánchez E., Borro D. A review of surgical robots for spinal interventions. Int J Med Robot. 2013;9(4):407–422. doi: 10.1002/rcs.1469. [DOI] [PubMed] [Google Scholar]
- 12.Urakov T.M., Chang K.H., Burks S.S., Wang M.Y. Initial academic experience and learning curve with robotic spine instrumentation. Neurosurg Focus. 2017;42(5):E4. doi: 10.3171/2017.2.FOCUS175. [DOI] [PubMed] [Google Scholar]
- 13.Sukovich W., Brink-Danan S., Hardenbrook M. Miniature robotic guidance for pedicle screw placement in posterior spinal fusion: early clinical experience with the SpineAssist. Int J Med Robot. 2006;2(2):114–122. doi: 10.1002/rcs.86. [DOI] [PubMed] [Google Scholar]
- 14.Lonjon N., Chan-Seng E., Costalat V., Bonnafoux B., Vassal M., Boetto J. Robot-assisted spine surgery: feasibility study through a prospective case-matched analysis. Eur Spine J. 2016;25(3):947–955. doi: 10.1007/s00586-015-3758-8. [DOI] [PubMed] [Google Scholar]
- 15.Le X., Tian W., Shi Z., Han X., Liu Y., Liu B. Robot-assisted versus fluoroscopy-assisted cortical bone trajectory screw instrumentation in lumbar spinal surgery: a matched-cohort comparison. World Neurosurg. 2018;120:E745–E751. doi: 10.1016/j.wneu.2018.08.157. [DOI] [PubMed] [Google Scholar]
- 16.Gertzbein S.D., Robbins S.E. Accuracy of pedicular screw placement in vivo. Spine (Phila Pa 1976) 1990;15(1):11–14. doi: 10.1097/00007632-199001000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Louw D.F., Fielding T., McBeth P.B., Gregoris D., Newhook P., Sutherland G.R. Surgical robotics: a review and neurosurgical prototype development, Neurosurgery. 2004;54(3):525–536. doi: 10.1227/01.neu.0000108638.05274.e9. discussion 536–7. [DOI] [PubMed] [Google Scholar]
- 18.Keric N., Doenitz C., Haj A., Rachwal-Czyzewicz I., Renovanz M., Wesp D.M.A. Evaluation of robot-guided minimally invasive implantation of 2067 pedicle screws. Neurosurg Focus. 2017;42(5):E11. doi: 10.3171/2017.2.FOCUS16552. [DOI] [PubMed] [Google Scholar]
- 19.Roser F., Tatagiba M., Maier G. Spinal robotics: current applications and future perspectives, Neurosurgery. 72. 2013;(Suppl 1):12–18. doi: 10.1227/NEU.0b013e318270d02c. [DOI] [PubMed] [Google Scholar]
- 20.Schröder M.L., Staartjes V.E. Revisions for screw malposition and clinical outcomes after robot-guided lumbar fusion for spondylolisthesis. Neurosurg Focus. 2017;42(5):E12. doi: 10.3171/2017.3.FOCUS16534. [DOI] [PubMed] [Google Scholar]
- 21.Karapinar L., Erel N., Ozturk H., Altay T., Kaya A. Pedicle screw placement with a free hand technique in thoracolumbar spine: is it safe. J Spinal Disord Tech. 2008;21(1):63–67. doi: 10.1097/BSD.0b013e3181453dc6. [DOI] [PubMed] [Google Scholar]
- 22.Schatlo B., Molliqaj G., Cuvinciuc V., Kotowski M., Schaller K., Tessitore E. Safety and accuracy of robot-assisted versus fluoroscopy-guided pedicle screw insertion for degenerative diseases of the lumbar spine: a matched cohort comparison. J Neurosurg Spine. 2014;20(6):636–643. doi: 10.3171/2014.3.SPINE13714. [DOI] [PubMed] [Google Scholar]
- 23.Solomiichuk V., Fleischhammer J., Molliqaj G., Warda J., Alaid A., von Eckardstein K. Robotic versus fluoroscopy-guided pedicle screw insertion for metastatic spinal disease: a matched-cohort comparison. Neurosurg Focus. 2017;42(5):E13. doi: 10.3171/2017.3.FOCUS1710. [DOI] [PubMed] [Google Scholar]
- 24.Ringel F., Stüer C., Reinke A., Preuss A., Behr M., Auer F. Accuracy of robot-assisted placement of lumbar and sacral pedicle screws: a prospective randomised comparison to conventional freehand screw implantation. Spine (Phila Pa 1976) 2012;37(8):E496–E501. doi: 10.1097/BRS.0b013e31824b7767. [DOI] [PubMed] [Google Scholar]
- 25.Han X., Tian W., Liu Y., Liu B., He D., Sun Y. Safety and accuracy of robot-assisted versus fluoroscopy-assisted pedicle screw insertion in thoracolumbar spinal surgery: a prospective randomised controlled trial. J Neurosurg Spine. 2019:1–8. doi: 10.3171/2018.10.SPINE18487. [DOI] [PubMed] [Google Scholar]
- 26.Khan A., Meyers J.E., Yavorek S., 'Connor T.E.O., Siasios I., Mullin J.P. Comparing next-generation robotic technology with 3-dimensional computed tomography navigation technology for the insertion of posterior pedicle screws. World Neurosurg. 2019;123:E474–E481. doi: 10.1016/j.wneu.2018.11.190. [DOI] [PubMed] [Google Scholar]
- 27.Mastrangelo G., Fedeli U., Fadda E., Giovanazzi A., Scoizzato L., Saia B. Increased cancer risk among surgeons in an orthopaedic hospital. Occup Med (Lond. 2005;55(6):498–500. doi: 10.1093/occmed/kqi048. [DOI] [PubMed] [Google Scholar]
- 28.Kantelhardt S.R., Martinez R., Baerwinkel S., Burger R., Giese A., Rohde V. Perioperative course and accuracy of screw positioning in conventional, open robotic-guided and percutaneous robotic-guided, pedicle screw placement. Eur Spine J. 2011;20(6):860–868. doi: 10.1007/s00586-011-1729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liu H.S., Duan S.J., Liu S.D., Jia F.S., Zhu L.M., Liu M.C. Robot-assisted percutaneous screw placement combined with pelvic internal fixator for minimally invasive treatment of unstable pelvic ring fractures. Int J Med Robot. 2018;14(5):e1927. doi: 10.1002/rcs.1927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Davne S.H., Myers D.L. Complications of lumbar spinal fusion with transpedicular instrumentation. Spine (Phila Pa 1976) 1992;17(6 Suppl):S184–S189. doi: 10.1097/00007632-199206001-00021. [DOI] [PubMed] [Google Scholar]
- 31.Faraj A.A., Webb J.K. Early complications of spinal pedicle screw. Eur Spine J. 1997;6(5):324–326. doi: 10.1007/BF01142678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Devito D.P., Kaplan L., Dietl R., Pfeiffer M., Horne D., Silberstein B. Clinical acceptance and accuracy assessment of spinal implants guided with SpineAssist surgical robot: retrospective study. Spine (Phila Pa 1976) 2010;35(24):2109–2115. doi: 10.1097/BRS.0b013e3181d323ab. [DOI] [PubMed] [Google Scholar]