Abstract
Objective
Day type II crescent fracture–dislocation is a subtype of pelvic lateral compression injury. At present, there is still a controversy on the operative approach and fixation technique. We have put forward closed reduction and percutaneous crossed screws fixation for treating type-II crescent fracture–dislocation. Finite element analysis is used to compare the biomechanical properties between percutaneous crossed screws and other internal fixations.
Methods
A three-dimensional finite element model of Day type-II crescent fracture–dislocation was simulated using 5 implants, including double anterior plates (Model A), one posterior plate and one iliac screw (Model B), one sacroiliac joint screw (Model C), crossed one iliac screw and one sacroiliac joint screw (Model D), and crossed two iliac screws and one sacroiliac joint screw (Model E). 600-N stress was applied to S1 vertebral end-plate. To evaluate the biomechanical properties, the stress distribution and displacement distribution of the pelvis, stress distribution of the crescent fragment and stress distribution of plate and cannulated screw were recorded and analyzed.
Results
Under the loading of 600N, the maximum pelvic displacements in the finite element model were compared as follows: model E (0.070 mm), model D (0.071 mm), model A (0.080 mm), model C (0.096 mm), and model B (0.112 mm). The maximum displacements of crescent fragment were compared as follows: model E (0.018 mm), model B (0.022 mm), model D (0.023 mm), model A (0.030 mm), and model C (0.043 mm). The maximum stress of all implants were compared as follows: model D (90.01 Mpa), model E (81.60 Mpa), model C (69.07 Mpa), model A (56.51 Mpa), model B (18.29 Mpa). Model E and model D could provide better mechanical support for whole pelvic.
Conclusions
With sufficient biomechanical stability and minimally invasive advantage, percutaneous crossed screw fixation is a recommended treatment for Day Type-II Crescent Fracture–dislocation. It is recommended to fix crescent fracture fragment and sacroiliac joint simultaneously during the operation. If it is difficult to fix the both position, the sacroiliac joint is preferentially fixed.
The translational potential of this article
There is a controversy on the operative approach and fixation technique of Day type-II crescent fracture–dislocation. This article proves that percutaneous crossed screw fixation is a recommended treatment for Day type-II crescent fracture–dislocation by finite element analysis.
Keywords: Crescent fracture-dislocation, Day type, Finite element analysis, Internal fixation, Pelvic fracture
Abbreviations: FEA, Finite element analysis; ORIF, open reductions and internal fixations; CT, Computed Tomography; DICOM, Digital Imaging and Communications in Medicine
Introduction
Pelvic ring injuries are classified into 3 main groups in the Young–Burgess classification system [1]. A subtype of lateral compression injury, crescent fracture–dislocation, which accounts for approximately 12% of pelvic ring injuries [2], is originally defined as a fracture–dislocation of the sacroiliac joint. Day et al. [2] divided crescent fracture–dislocation into 3 main types: type I fractures involve less than one-third of the sacroiliac joint, resulting in a large and stable fragment of the posterior crescent-shaped iliac; type II fractures involve one-third of the sacroiliac joint, resulting in a moderate and stable fragment; and type III fractures involve more than one-third of the sacroiliac joint, resulting in a small and stable fragment. Posterior iliac crescent fracture–dislocation involves the sacroiliac joint, which is a major weight-bearing articulation. If it is not appropriately treated, the potential for posttraumatic arthritis and chronic instability is considerable [3]. For the treatment of type II fracture, the previous literatures report that there are mainly two methods of open reductions and internal fixations (ORIFs) with anterior [4], [5] or posterior [6] approaching. However, there is still a big controversy about this subject.
Accurate reduction with stable fixation diminishes pain permits early patient mobility and allows the pelvic ring to heal in an anatomic location [2], [7]. ORIF could achieve the effect of accurate reduction. However, ORIF is delayed routinely for fear of entering the pelvic haematoma, thereby causing additional haemorrhage [7]. Delayed operative intervention allows maturation of the haematoma but diminishes the success of closed manipulative reduction. What is more, ORIF of posterior pelvic injuries, in particular, was associated with high wound complication rates in one clinical series [8]. Early and accurate closed reduction in conjunction with stable fixation using percutaneous insertion techniques should be ideal treatment for certain pelvic fracture, especially in patients with polytrauma [9], [10]. Percutaneous pelvic fixation provides a stable skeletal frame to support the viable local soft tissues while avoiding large operative exposures.
Since 2005, our team had started a series of basic and clinical research on minimally invasive treatment of pelvic fractures [11]. Close reduction and minimally invasive percutaneous crossed screw fixation was used for the treatment of Day II pelvic crescent fracture–dislocation (Fig. 1). It was the first report in which the crossed iliac screw and sacroiliac joint screw were used for the treatment of Day type II crescent fracture–dislocation. Calafi et al. [12] identified 129 crescents in 128 patients during a 7-year time period. They also recommended the majority of crescent fracture–dislocation were amenable to closed reduction and percutaneous iliosacral screw fixation. Both studies have shown that percutaneous screw fixation for Day type II crescent fracture–dislocation can achieve good clinical results. But is there more biomechanical advantageous for percutaneous crossed screw fixation compare to traditional percutaneous screw fixation? Moreover, is it possible to provide sufficient biomechanical stability for Day II crescent fracture–dislocation with percutaneous crossed screws? Current studies provide little information regarding the stability of different fixations.
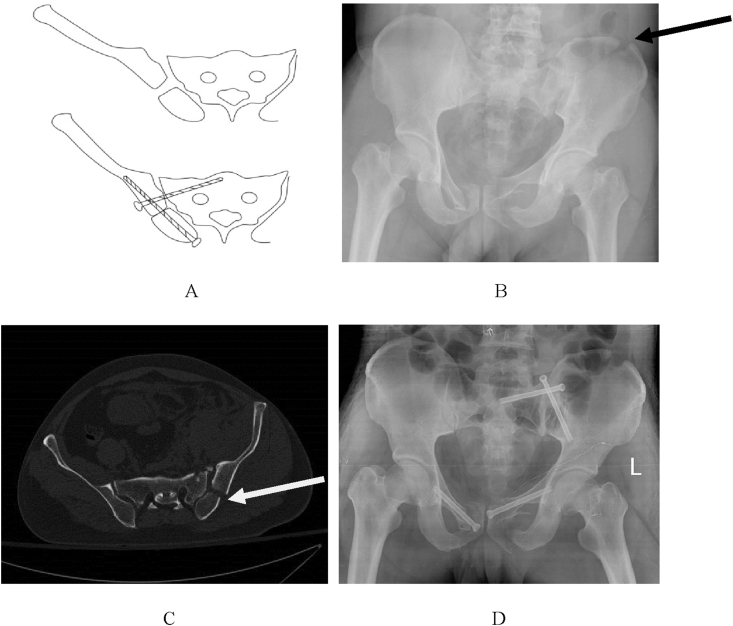
Figure 1.
(A): The schematic diagram of percutaneous crossed screw fixation; (B): A typical Day type-II pelvic crescent fracture-dislocation accrding to anteroposterior pelvic radiograph and CT scan, the black arrow shows the crescent fracture fragment; (C) preoperatively, the white arrow shows the crescent fracture line,. D: Closed reduction and percutaneous crossed fixation with one posterior iliac screw and one sacroiliac joint screw, pelvic X-ray postoperatively is satisfactory.
In this study, a three-dimensional finite element model of the pelvis including cartilage, peripheral ligaments, and other structures was constructed. The model of the typical type II pelvic crescent fracture–dislocation was used to analyze the application of percutaneous crossed cannulated screw and the remaining traditional internal fixations. The effect of fixed type II pelvic crescent fracture–dislocation on pelvic stress distribution and displacement distribution was compared. To the best of our knowledge, it was the first study to compare the biomechanical stability of percutaneous crossed screw fixation and other fixations in treatment of Day type II crescent fracture–dislocation.
Materials and methods
Finite element models and implants
After reviewing published literature, there is no established model for reference for this type of injury. Therefore, among the many Day type II crescent fracture–dislocation cases, a patient with typical Day type II crescent fracture–dislocation of the sacroiliac joint was selected randomly (male, 32-year-old, 172-cm height and 72-kg weight). Authors had obtained patient consent before enrolling participants in this study. The Hospital Ethics Committee licenced this study. The computed tomography (CT) scan data in the Digital Imaging and Communications in Medicine format of the typical patients was imported into Mimics V10.0 for three-dimensional reconstructions and to simulate the reduction of Day type II crescent fracture–dislocation [10], [13]. Cannulated screw, cortical screw, reconstruction plate, and fixation models were established on SolidWorks software. There were five different internal fixation models which were established via the Boolean Operation: (1) double plates model (model A): a 4-hole reconstruction plate for the anterior part of the sacroiliac joint; another 5-hole reconstruction plate for the anterior iliac fracture. (2) One posterior plate and one iliac screw (model B): one 5-hole reconstruction plate for the posterior iliac fracture; the iliac fracture was fixed by a cannulated screw; the sacroiliac joint was not fixed. (3) One sacroiliac joint screw (model C): the dislocated sacroiliac joint was fixed by a cannulated screw. The iliac was not fixed. (4) Crossed one iliac screw and one sacroiliac joint screw (model D): the dislocated sacroiliac joint was fixed by a cannulated screw. The iliac fracture was fixed by another cannulated screw. (5) Crossed two iliac screws and one sacroiliac joint screw (model E). The dislocated sacroiliac joint was fixed by a cannulated screw. The iliac fracture was fixed by another two cannulated screws.
All of the parts were imported into ANSYS 14.5 for assembling and meshing. The pelvic ligament reconstruction was achieved through the spring link, and the Poisson's ratio, elastic modulus, and spring number of each ligament were set according to the parameter shown in Table 1. The material properties involved in the model were assigned in combination with the material properties commonly used in references [14], [15] and the research purposes of this article (Table 2). The five finite element models were divided into different tetrahedral mesh structures (nodes and element number in Table 3). Finally, five different three-dimensional finite element models with internal fixation were completed (Fig. 2A–E).
Table 1.
Different elastic modulus parameters and numbers of pelvic ligaments.
| Ligaments | K (N/mm) | Number of springs |
|---|---|---|
| Anterior sacroiliac | 700 | 27 |
| Posterior sacroiliac | 1400 | 15 |
| Interosseous sacroiliac | 2800 | 8 |
| Sacrotuberous | 1500 | 15 |
| Sacrospinous | 1400 | 10 |
| Superior pubic | 500 | 24 |
| Arcuate pubic | 500 | 24 |
Table 2.
Material properties of series of FE models.
| Materials | Elastic modulus/MPa | Poisson ratio | Friction coefficient |
|---|---|---|---|
| Titanium plate | 110 000 | 0.30 | — |
| Titanium screw | 110 000 | 0.30 | — |
| Cortical bone | 17 000 | 0.3 | 0.4 |
| Cancellous bone | 129 | 0.2 | 0.4 |
| Articular cartilage | 11.9 | 0.4 | 0.0024 ~ 0.24 |
| Interpubic disc | 5 | 0.45 | — |
| Capsule, ligament matrix | 3.22 ~ 4.29 | 0.49 | — |
| Joint capsule fibre | 105 | 0.3 | — |
Table 3.
The nodes and elements of 5 kinds of FE models.
| Finite element model | Nodes | Element number |
|---|---|---|
| A | 298521 | 183660 |
| B | 295642 | 183450 |
| C | 281024 | 180245 |
| D | 275460 | 178903 |
| E | 280456 | 180032 |
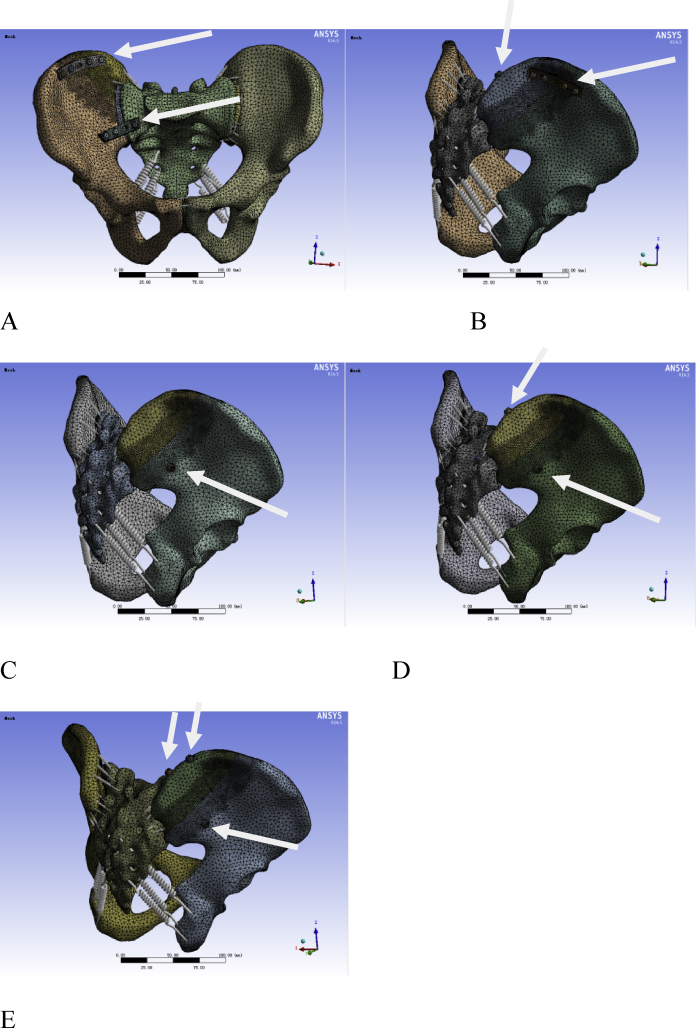
Figure 2.
Five different internal fixation after assembly of 3D model. A: Double plates model, white arrow show the two plates; B: One reconstruction plate and one posterior iliac screw fixed model, as indicated by the white arrow; C: One canulated screw fixed sacroiliac joint model, as indicated by the white arrow; D: Crossed fixation with one posterior iliac screw and one sacroiliac joint screw model, as indicated by the white arrow; E: Crossed fixation with two posterior iliac screw and one sacroiliac joint screw model, as indicated by the white arrow.
Contact, constraint, and load of three-dimensional finite element model
In the research, the contact relation between the iliac, sacrum, and SI joint was set as binding constraints, as same as the contact relation between screw and bones. The contact relation between plate and bone was set as sliding friction. In reference to previous studies [16], [17], in the boundary and loading conditions, a standing posture with a double-leg stance was considered in the present study, a vertical (S1) downward load of 600 N was imposed on the surface of the sacrum to simulate the gravity of the upper part of the body (Fig. 3).
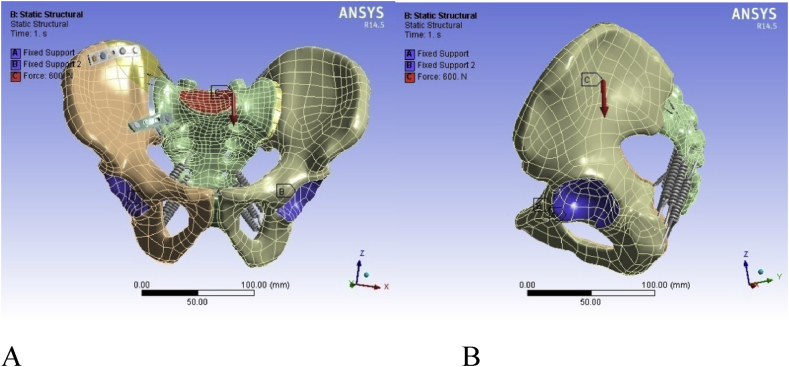
Figure 3.
Location of the constraints and add load (model A, for example), the red arrow indicates the direction of force loading. A: anterioposterior side; B: lateral side.
The mechanical properties of five different internal fixation methods were comprehensively analyzed by the following indicators: (1) maximum displacement of the pelvis, maximum von Mises stress of the pelvis; (2) stress distribution of the posterior crescent fragment; (3) stress distribution of plate and cannulated screws.
Results
Displacement and stress analysis of the whole pelvis
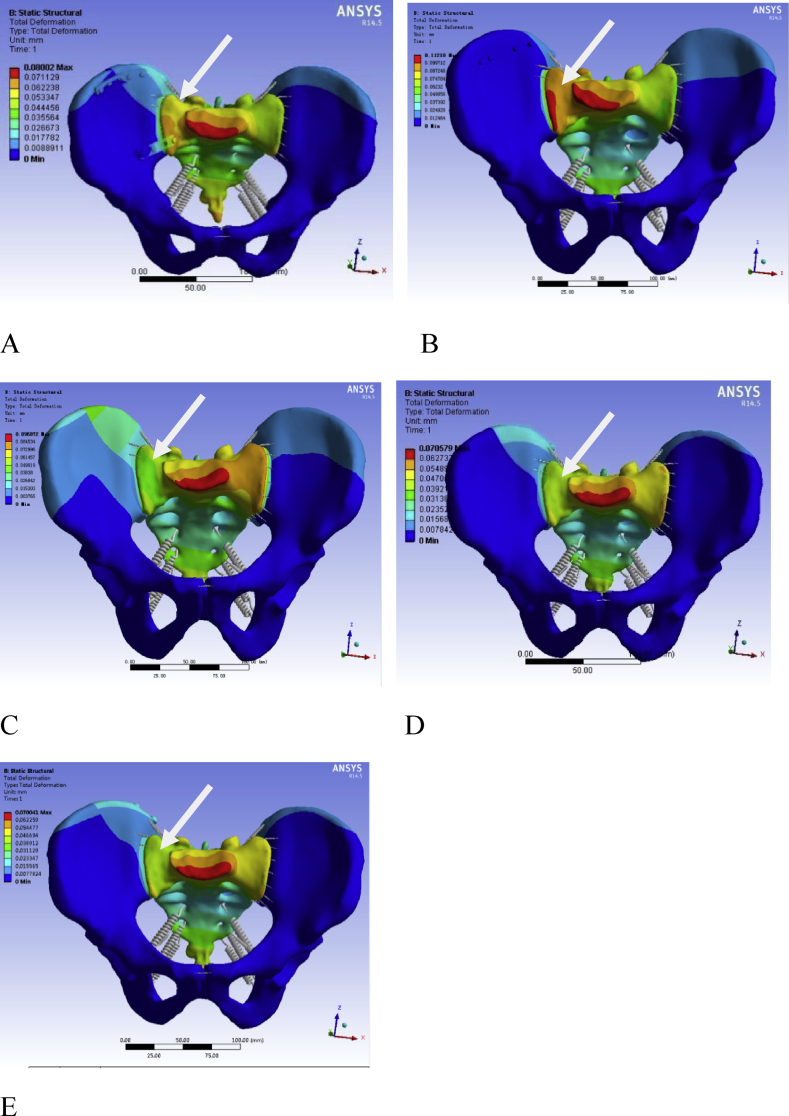
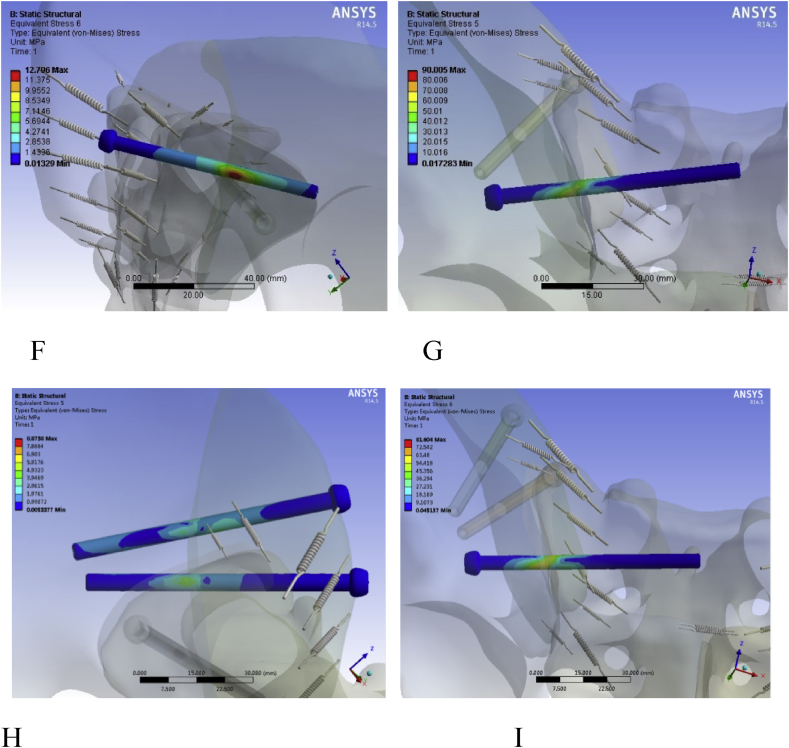
Under the loading of 600N, the maximum pelvic displacement in the finite element model is as follows: model A (0.080 mm, Fig. 4A), model B (0.112 mm, Fig. 4B), model C (0.096 mm, Fig. 4C), model D (0.071 mm, Fig. 4D), model E (0.070 mm, Fig. 4E). As shown in Table 4, the maximum pelvic displacements of the five models are compared as follows: model E < model D < model A < model C < model B.
Figure 4.
The pelvic displacement distribution diagram of the five models. A: model A; B: model B; C: model C; D: model D; E: model E. The white arrow shows the color change at pelvic displacement, indicating the displacement distribution. As shown in the figure, the color is more reddish, the pelvic is with the greater the displacement distribution. In A and B, the color of the pelvic is orange and red, indicating a large displacement distribution; while, in C, D and E, the color of the pelvic is green, indicating that the displacement distribution is smaller than A and B.
Table 4.
The maximum displacement (MD) and maximum stress (MS) of different finite element model and the maximum displacement of crescent fracture-dislocation (MDCFS) after loading the pelvis.
| Model | MD (mm) | MS (Mpa) | MDCFS (mm) |
|---|---|---|---|
| A | 0.080 | 56.51 | 0.030 |
| B | 0.112 | 18.29 | 0.022 |
| C | 0.096 | 69.07 | 0.043 |
| D | 0.071 | 90.01 | 0.023 |
| E | 0.070 | 81.60 | 0.018 |
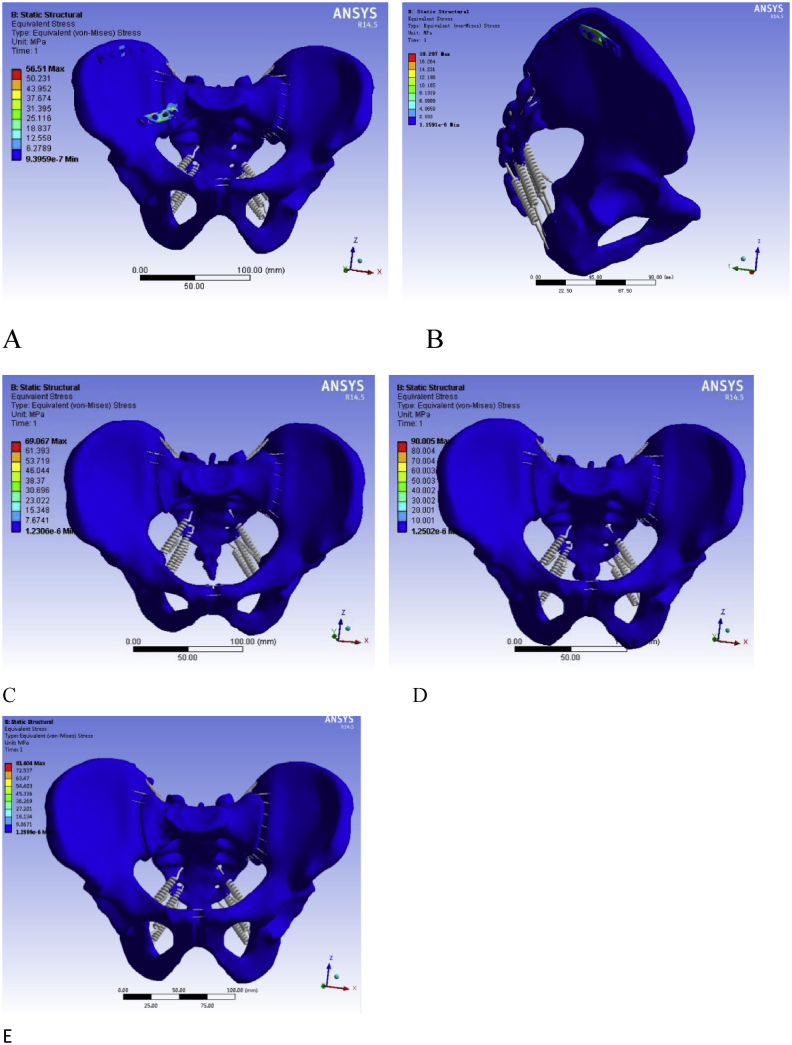
The maximum von Mises stress of the pelvic in model A is 56.51Mpa (Fig. 5A), which is located in the middle of the reconstruction plate; model B is 18.29Mpa (Fig. 5B), which is located above the middle hole of the reconstruction plate. The maximum stress of the pelvis in model C is 69.07Mpa (Fig. 5C), model D is 90.01Mpa (Fig. 5D), model E is 81.60Mpa (Fig. 5E), which are all located in the area of cannulated screw through the sacroiliac joint. Model E and model D could provide better mechanical support for whole pelvic (Table 4).
Figure 5.
The pelvic stress distribution diagram of the five models. A: model A, the maximum stress of the pelvic (56.51 Mpa) was located in the middle of reconstruction plate; B: model B, the maximum stress of the pelvic (18.297 Mpa) was located above the middle hole of the reconstruction plate; C: model C; D: model D; E: model E. The maximum stress of the pelvic (69.07 Mpa, 90.01 Mpa, 81.60 Mpa) was all located in the area of cannulated screw through the sacroiliac joint. Compared to plate, SI screw can withstand greater stress and reduce stress distribution in the pelvis.
Displacement distribution of the crescent fracture fragment
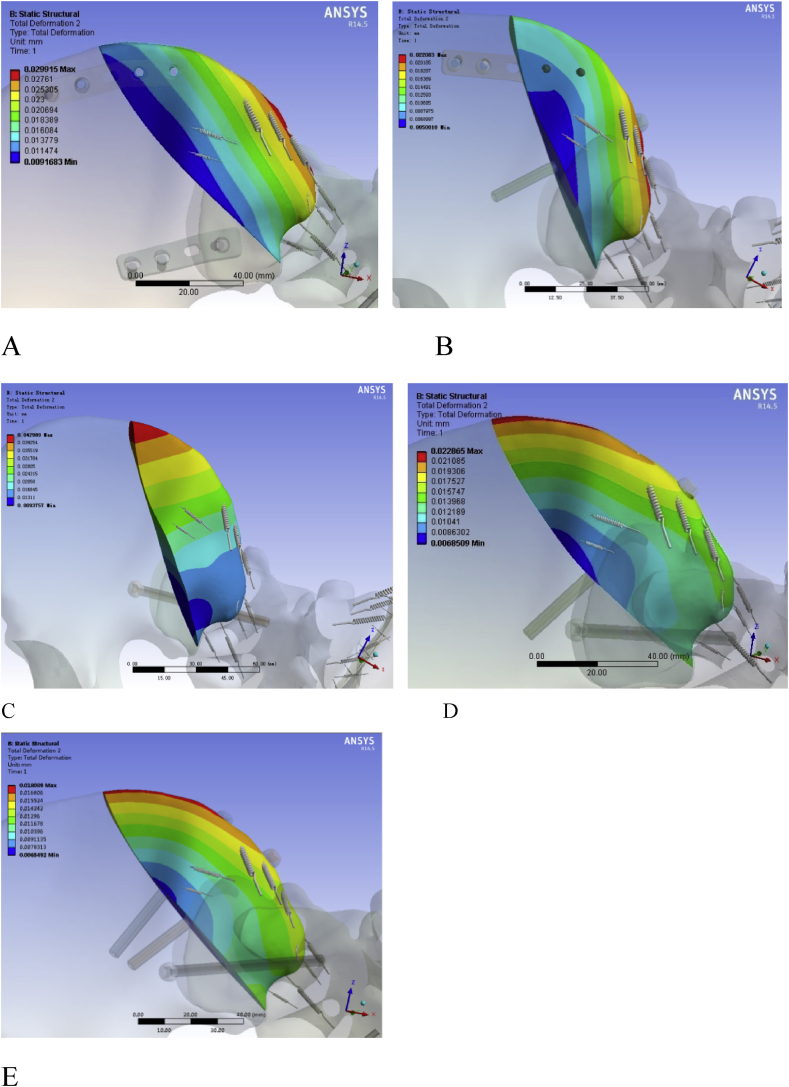
Under the loading of 600N, the maximum displacement of crescent fragment is as follows: model A (0.030 mm, Fig. 6A), model B (0.022 mm, Fig. 6B), model C (0.043 mm, Fig. 6C), model D (0.023 mm, Fig. 6D), model E (0.018 mm, Fig. 6E). As shown in Table 4, the maximum displacements of crescent fragment are compared as follows: model E< model B< model D< model A< model C. Compared with model E, B, and D, the values of model A and C are significantly increased. So, model E, model B, and model D could provide better mechanical support for the crescent fracture fragment.
Figure 6.
Displacement distribution of crescent fragment of the five models. A: model A; B: model B; C: model C; D: model D; E: model E. The color change at the crescent fragment, indicates the displacement distribution. As shown in the figure, the color is more reddish, the crescent fragment is with the greater the displacement distribution. In C (0.043 mm), there is most red part in the five models, because the crescent fragment is not fixed. The second red part is A (0.030 mm), in which the crescent fragment is fixed with plate. The B (0.022 mm), D (0.023 mm) and E (0.018 mm), are with the similar value. They are all fixed with cannulated screw. Compared to plate, cannulated screw can withstand more stress.
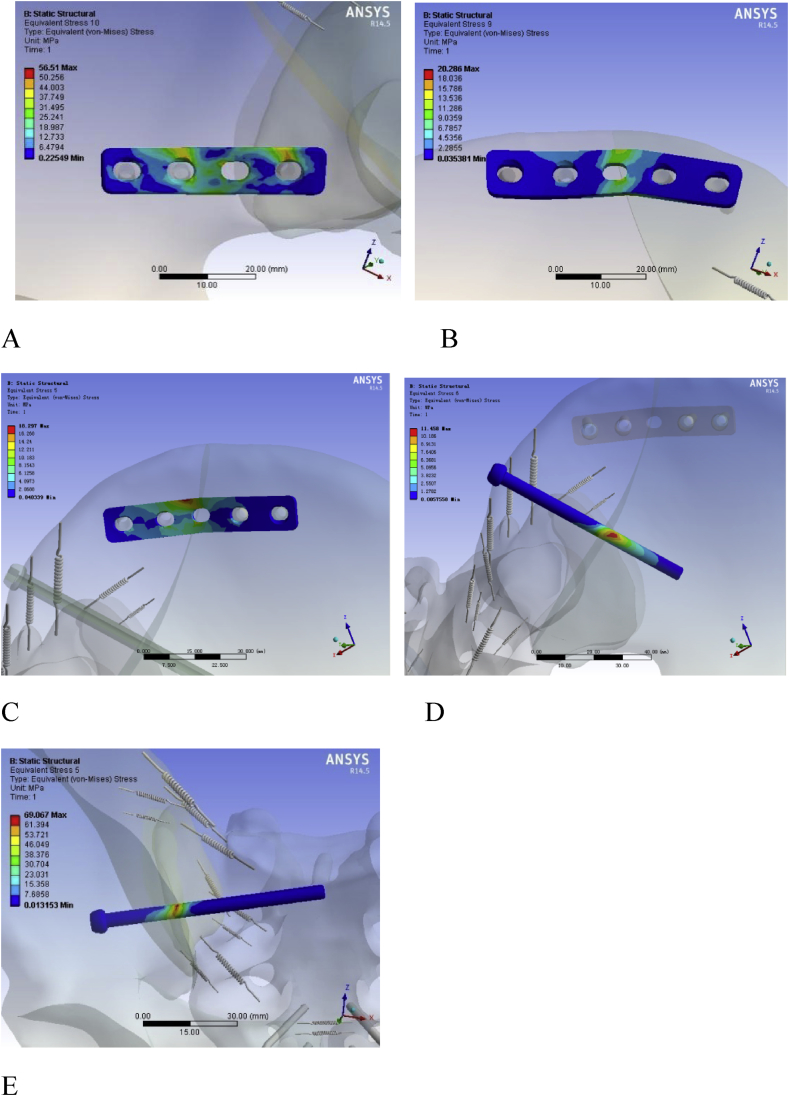
Stress analysis of the implants
In model A, the maximum stress of the plate which fixed the sacroiliac joint is 56.51 Mpa (Fig. 7A), the maximum stress of the plate which fixed crescent fragment is 20.29 Mpa (Fig. 7B). In model B, the maximum stress of the plate is 18.29Mpa (Fig. 7C), the maximum stress of the cannulated screw is 11.458 Mpa (Fig. 7D). In model C, the maximum stress of the cannulated screw is 69.07 Mpa (Fig. 7E). In model D, the maximum stress of the cannulated screw which fixed the crescent fragment is 12.80 Mpa (Fig. 7F) and the maximum stress of the cannulated screw which fixed sacroiliac joint is 90.01 Mpa (Fig. 7G). In model E, the maximum stress of the cannulated screw which fixed the crescent fragment is 8.87 Mpa (Fig. 7H) and the maximum stress of the cannulated screw which fixed sacroiliac joint is 81.604 Mpa (Fig. 7I). Compared with the plate, the percutaneous cannulated screw could provide better stability for sacroiliac joint fixation.
Figure 7.
Stress analysis of the fixation in the five models. A:Distribution diagram of plate stress fixed sacroiliac joint in model A; B: Distribution diagram of plate stress fixed crescent fragment in model A; C: Distribution diagram of plate stress fixed crescent fragment in model B; D: Distribution diagram of canulated screw stress fixed crescent fragment in model B; E: Distribution diagram of canulated screw stress fixed sacroiliac joint in model C; F: Distribution diagram of canulated screw stress fixed crescent fragment in model D; G: Distribution diagram of canulated screw stress fixed sacroiliac joint in model D; H:Distribution diagram of the two canulated screw stress fixed crescent fragment in model E; I:Distribution diagram of canulated screw stress fixed sacroiliac joint in model E. Whether it is the fixation of the crescent fragment or the SI joint, the cannulated screw can withstand more stress and is more evenly distributed than the plate, and the two cannulated screws are more advantageous.
Discussion
Crescent fracture–dislocation of the sacroiliac joint is a relatively uncommon type of lateral compression injury [2], [3]. The main purpose of surgical intervention is to achieve early reduction and fixation of the associated fracture or dislocation of the pelvic ring. A number of surgical techniques have been described for the reduction and fixation of sacroiliac fracture–dislocations [2], [4], [6]. Day et al. [2] described the crescent fracture–dislocation classification system based on the extent and location of sacroiliac joint involvement. Type II fractures involving the middle third of the joint are generally addressed through a posterior approach with open reduction and plate fixation. Another study [6] argued that the lateral window of an ilioinguinal approach offers the best chance of accurate reduction with stable anterior plate fixation, while our team proposed close reduction and minimally invasive percutaneous crossed screw fixation for the treatment of Day II pelvic crescent fracture–dislocation [11]. However, there is no conclusion whether it could provide sufficient biomechanical stability for Day II crescent fracture–dislocation. So this research was carried out.
In the five internal fixation models, the maximum displacement of the pelvis in model E was 0.070 mm and the maximum displacement of the crescent fracture fragment was 0.018 mm, the value being the smallest of all models. The maximal displacement of the pelvis in model D was 0.071 mm, which was the second smallest; and the maximum displacement of the crescent fracture fragment is 0.023 mm, which was only larger than the crescent in model E and model B. This suggested that for the overall stability of the pelvis, models D and E had better biomechanical stability than the other three models. This also indicated that it was necessary to fix the crescent fracture fragment and sacroiliac joint for treating type II crescent fracture–dislocation. This could also be verified from model A. The crescent fracture fragment and sacroiliac joint were fixed by the double anterior plates in model A. The maximum displacement of the pelvis was 0.080 mm and the biomechanical stability was only subsequent to models D and E, significantly better than models B and C. In model B and model C, the crescent fracture fragment and sacroiliac joint were not fixed at the same time.
For the maximum stress of the pelvic, model D and model E provided better mechanical support for whole pelvic than other three models. This also indicated that it was necessary to fix the crescent fracture fragment and sacroiliac joint for treating type-II crescent fracture–dislocation. Although the crescent fracture fragment and sacroiliac joint were all fixed by plates in model A, the maximum stress was less than model C, in which just the sacroiliac joint fixed by cannulated screw. It mean that cannulated screw provide more mechanical stability than plates. The reason may be that the cannulated screw is intramedullary fixation and the plate is eccentrically fixation [18]. The value of model B was far less than the other four models. This indicated that the fixation of the sacroiliac joint played a more important role in the mechanical stability than the crescent fracture fragment of the whole pelvis in type II crescent fracture–dislocation [19].
For the posterior crescent fracture, the displacement in model E and model D were almost equal and the smallest of the five models, which indicated that the models with two cannulated screws had the best stability. It also showed that the intramedullary fixation of the cannulated screw had good biomechanical properties. Meanwhile, the displacement in the D and B models was not much different, which suggested that we use a cannulated screw or a reconstruction plate combined with a cannulated screw to fix the crescent fracture, and the biomechanical stability was not much different.
For the maximum stress of the different implants, the maximum stress of the cannulated screw which fixed sacroiliac joint in model D and E was more than the plate which fixed the sacroiliac joint in model A. Compared with the plate, the cannulated screw could provide better stability for sacroiliac joint fixation. A study by Li [20] showed percutaneous sacroiliac screw internal fixation in the treatment of pelvic fractures has less injury, less bleeding, less pain, and rapid recovery which is a safe and effective minimally invasive operation method. So, it was better than anterior plate fixation for the treatment of sacroiliac joint.
Scores demonstrating the highest overall level of dysfunction in this series relate to type II fracture–dislocation patients with failure of fixation, multiple injuries, and malunion following nonoperative management [2]. The minimally invasive effect of percutaneous crossed screw fixation of type II fracture–dislocation was not only in the minimally invasive surgery [21] but also in the protection of pelvic-related affiliated structures. Therefore, there is a greater impact on the patient's recovery and functional rehabilitation exercise because of the soft tissue injury caused by ORIF [22]. With sufficient biomechanical stability and minimally invasive advantage, percutaneous crossed screw fixation is a recommended treatment for Day type II crescent fracture–dislocation. But this technique requires specific training and regular surgical experience, which requires a learning curve [23].
There are some limitations of the present study. First, the pelvic model was set as a homogeneous isotropic elastic material, which was different from the real bone. In the human bone tissue, the elastic modulus is different in directional elastic modulus, and the Poisson's ratio is also different. Second, the overall structure of the pelvis is very complicated. The finite element models are based on skeleton–ligament system, and the muscle forces were neglected, similarly to other finite element studies [24], [25]. Third, there is a limitation about the biomechanical tests: only one male patient for the finite element analysis. After reviewing published literature, there is no established model for reference for this type of injury. Therefore, among the many Day type II crescent fracture–dislocation cases, we randomly selected a typical case for establishing finite element for this type of injury. Of cause, such one male patient choice is insufficient. In the future, more patients and at least a female patient will be included. Although the established model had certain defects, it was basically a comprehensive three-dimensional finite element model of the type II pelvis crescent fracture–dislocation with different internal fixations. This study would lay a foundation for the clinical research of pelvic crescent fracture–dislocation in the future.
Conclusion
In conclusion, with sufficient biomechanical stability and minimally invasive advantage, percutaneous crossed screw fixation is a recommended treatment for Day type II crescent fracture–dislocation. It is recommended to fix crescent fracture fragment and sacroiliac joint simultaneously during the operation. If it is difficult to fix the both position, the sacroiliac joint is preferentially fixed.
Conflicts of interest
The authors have no conflicts of interest to disclose in relation to this article.
Acknowledgements
This research was supported by Wenzhou Basic Scientific Research project funding (No. Y20180321), Zhejiang Natural Science Fund project funding (No. LY19H060003), and the National Natural Science Foundation of China (81701928). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Contributor Information
Leyi Cai, Email: caileyi@wmu.edu.cn.
Yingying Zhang, Email: alma55@yeah.net.
Wenhao Zheng, Email: zhengwenhao@wmu.edu.cn.
Jianshun Wang, Email: wjszdl@aliyun.com.
Xiaoshan Guo, Email: guoxiaoshan666@163.com.
Yongzeng Feng, Email: 13858878561@163.com.
References
- 1.Burgess A.R., Eastridge B.J., Young J.W., Ellison T.S., Ellison P.S., Jr., Poka A. Pelvic ring disruptions: effective classification system and treatment protocols. J Trauma. 1990;30(7):848–856. [PubMed] [Google Scholar]
- 2.Day A.C., Kinmont C., Bircher M.D., Kumar S. Crescent fracture-dislocation of the sacroiliac joint. J Bone Joint Surg Br. 2007;89(5):651–658. doi: 10.1302/0301-620X.89B5.18129. [DOI] [PubMed] [Google Scholar]
- 3.Zong Z., Chen S., Jia M., Shen Y., Hua X., Liu D. Posterior iliac crescent fracture-dislocation: is it only rotationally unstable? Orthopedics. 2014;37(5):e435–e440. doi: 10.3928/01477447-20140430-53. [DOI] [PubMed] [Google Scholar]
- 4.Borrelli J., Koval K.J., Helfet D.L. The crescent fracture:a posterior fracture dislocation of the sacroiliac joint. J Oahop Trauma. 1996;10(3):165–170. doi: 10.1097/00005131-199604000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Borrelli J., Koval K.J., Helfet D.L. Operative stabilization of fracture dislocations of the sacroiliac joint. Clin Orthop Relat Res. 1996;(329):141–146. doi: 10.1097/00003086-199608000-00017. [DOI] [PubMed] [Google Scholar]
- 6.Schildhauer T.A., Josten Ch, Muhr G. Triangular osteosynthesis of vertically unstable sacrum fractures: a new concept allowing early weight bearing. J Orthop Trauma. 2006;20(1 Suppl):S44–S51. [PubMed] [Google Scholar]
- 7.Routt M.L., Jr., Nork S.E., Mills W.J. Percutaneous fixation of pelvic ring disruptions. Clin Orthop Relat Res. 2000;375:15–29. doi: 10.1097/00003086-200006000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Elzohairy M.M., Salama A.M. Open reduction internal fixation versus percutaneous iliosacral screw fixation for unstable posterior pelvic ring disruptions. Orthop Traumatol Surg Res. 2017;103(2):223–227. doi: 10.1016/j.otsr.2016.12.002. [DOI] [PubMed] [Google Scholar]
- 9.Eckardt H., Egger A., Hasler R.M., Zech C.J., Vach W., Suhm N. Good functional outcome in patients suffering fragility fractures of the pelvis treated with percutaneous screw stabilisation: assessment of complications and factors influencing failure. Injury. 2017;48(12):2717–2723. doi: 10.1016/j.injury.2017.11.002. [DOI] [PubMed] [Google Scholar]
- 10.Cai L., Zhang Y., Chen C., Lou Y., Guo X., Wang J. 3D printing-based minimally invasive cannulated screw treatment of unstable pelvic fracture. J Orthop Surg Res. 2018;13(1):71. doi: 10.1186/s13018-018-0778-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shui X., Ying X., Mao C., Feng Y., Chen L., Kong J. Percutaneous screw fixation of crescent fracture-dislocation of the sacroiliac joint. Orthopedics. 2015;38(11):e976–e982. doi: 10.3928/01477447-20151020-05. [DOI] [PubMed] [Google Scholar]
- 12.Calafi L.A., Routt M.L., Jr. Posterior iliac crescent fracture-dislocation: what morphological variations are amenable to iliosacral screw fixation? Injury. 2013;44(2):194–198. doi: 10.1016/j.injury.2012.10.028. [DOI] [PubMed] [Google Scholar]
- 13.Chen D., Chen C.H., Tang L., Wang K., Li Y.Z., Phan K. Three-dimensional reconstructions in spine and screw trajectory simulation on 3D digital images: a step by step approach by using Mimics software. J Spine Surg. 2017;3(4):650–656. doi: 10.21037/jss.2017.10.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen L., Zhang G., Song D., Guo X., Yuan W. A comparison of percutaneous reduction and screw fixation versus open reduction and plate fixation of traumatic symphysis pubis diastasis. Arch Orthop Trauma Surg. 2012;132(2):265–270. doi: 10.1007/s00402-011-1414-2. [DOI] [PubMed] [Google Scholar]
- 15.Zuo Z. Shandong University; Jinan, China: 2006. Three-dimensional finite element analysis and biomechanics of sacroiliac complex. Medical Doctorship Thesis. [Google Scholar]
- 16.Eberle S., Gerber C., von Oldenburg G., Augat P. Stronger implant does not cause stress-shielding in the fixation of hip fractures - validated finite element analysis and cadaver tests. World Congress on Medical Physics and Biomedical Engineering. 2010;25(4):224–226. [Google Scholar]
- 17.Muller R., Kampschulte M., Khassawna T.E., Schlewitz G., Hürter B., Böcker W. Change of mechanical vertebrae properties due to progressive osteoporosis: combined biomechanical and finite-element analysis within a rat model. Med Biol Eng Comput. 2014;52(4):405–414. doi: 10.1007/s11517-014-1140-3. [DOI] [PubMed] [Google Scholar]
- 18.Lázaro Gonzálvez A., Martínez Reina J., Cano Luis P., Jiménez Baquero J., Sueiro Fernández J., Giráldez Sánchez M.A. Is cannulated-screw fixation an alternative to plate osteosynthesis in open book fractures? A biomechanical analysis. Injury. 2016;47(Suppl 3):S72–S77. doi: 10.1016/S0020-1383(16)30610-6. [DOI] [PubMed] [Google Scholar]
- 19.Vleeming A., Schuenke M.D., Masi A.T., Carreiro J.E., Danneels L., Willard F.H. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. J Anat. 2012 Dec;221(6):537–567. doi: 10.1111/j.1469-7580.2012.01564.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li C.L. Clinical comparative analysis on unstable pelvic fractures in the treatment with percutaneous sacroiliac screws and sacroiliac joint anterior plate fixation. Eur Rev Med Pharmacol Sci. 2014;18(18):2704–2708. [PubMed] [Google Scholar]
- 21.Starr A.J., Walter J.C., Harris R.W., Reinert C.M., Jones A.L. Percutaneous screw fixation of fractures of the iliac wing and fracture-dislocations of the sacro-iliac joint (OTA Types 61-B2.2 and 61-B2.3, or Young-Burgess "lateral compression type II" pelvic fractures) J Orthop Trauma. 2002;16(2):116–123. doi: 10.1097/00005131-200202000-00008. [DOI] [PubMed] [Google Scholar]
- 22.Kim J.W., Kim H.U., Oh C.W., Kim J.W., Park K.C. A prospective randomized study on operative treatment for simple distal tibial fractures-minimally invasive plate osteosynthesis versus minimal open reduction and internal fixation. J Orthop Trauma. 2018;32(1):e19–e24. doi: 10.1097/BOT.0000000000001007. [DOI] [PubMed] [Google Scholar]
- 23.Rysavý M., Pavelka T., Khayarin M., Dzupa V. Iliosacral screw fixation of the unstable pelvic ring injuries. Acta Chir Orthop Traumatol Cech. 2010;77(3):209–214. [PubMed] [Google Scholar]
- 24.He Y., He J., Wang F., Zhou D., Wang Y., Wang B. Application of additional medial plate in treatment of proximal humeral fractures with unstable medial column: a finite element study and clinical practice. Medicine. 2015;94:e1775. doi: 10.1097/MD.0000000000001775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhao Y., Li J., Wang D., Liu Y., Tan J., Zhang S. Comparison of stability of two kinds of sacro-iliac screws in the fixation of bilateral sacral fractures in a finite element model. Injury. 2012;43:490–494. doi: 10.1016/j.injury.2011.12.023. [DOI] [PubMed] [Google Scholar]