Abstract
Objective
The objective of this study is to compare the clinical efficacy of O-arm navigation and microscope-assisted minimally invasive transforaminal lumbar interbody fusion (modified MIS-TLIF) versus conventional TLIF in the lumbar isthmic spondylolisthesis.
Materials and methods
Forty patients with 1-level lumbar isthmic spondylolisthesis were enrolled in the study. Perioperative indexes including operation time, intraoperative bleeding, bed rest time, time of hospitalisation stay and the accuracy rate of screw placement were analysed. Preoperative and postoperative visual analogue scale (VAS) and Oswestry disability index (ODI) were assessed.
Results
The operation time in the modified MIS-TLIF group was longer than the conventional TLIF group (p < 0.05). However, intraoperative blood loss in the modified MIS-TLIF group was less than the comparative group (p < 0.05). The average bed rest time and hospitalisation stay in the modified MIS-TLIF group was shorter than conventional TLIF group (p < 0.05). The screw placement in the modified MIS-TLIF group was more precisely than that in the conventional TLIF group (p < 0.05). Meanwhile, the improvement of VAS and ODI in the modified MIS-TLIF group were lower than that in the conventional TLIF group 1 and 6 months after operation (p < 0.05). There was no difference in the VAS and ODI score between the two group at the last follow-up (p > 0.05).
Conclusion
Navigation and microscope-assisted MIS-TLIF is safe and reliable for treatment of lumbar isthmic spondylolisthesis (Meyerding degree I or II) with potential advantages including less injury, less blood loss, higher screw accuracy and faster recovery after operation.
The translational potential of this article
Compared with conventional transforaminal lumbar interbody fusion, O-arm navigation and microscope-assisted minimally invasive transforaminal lumbar interbody fusion has a huge advantage in surgery treatment of lumbar isthmic spondylolisthesis. Hence, this article provided a better surgery method to deal with lumbar isthmic spondylolisthesis, and robot-assisted minimally invasive transforaminal lumbar interbody fusion will be adopted in the future.
Keywords: Microscope, O-arm, Transforaminal lumbar interbody fusion, Navigation, Minimally invasive transforaminal lumbar interbody fusion, Lumbar isthmic spondylolisthesis
Introduction
Lumbar isthmic spondylolisthesis is an usual low back pain disease with morbidity of 4–6% in the population [1,2]. The character of this disease is the upper vertebrae slips over the subjacent vertebrae because of a defect in the isthmus in adolescence or adulthood [3]. The main symptoms of lumbar isthmic spondylolisthesis are low back pain, paresthesia in lower limbs, weakness of the legs and even impaired ambulation, intermittent claudication, etc [4]. Surgeries are necessary for patients with serious symptom and conservative treatment fail. Transforaminal lumbar interbody fusion (TLIF) had been widely used to treat lumbosacral isthmic spondylolisthesis [5]. This surgery makes satisfying nerve root decompression and intervertebral fusion by a single posterior approach and decreases the risk of neurological complications as well [6]. To complete the conventional TLIF, a long incision, excessive muscle stripping and massive blood loss are unavoidable [[7], [8], [9]]. With the situation of enhanced recovery after surgery (ERAS) and minimally invasive surgeries becoming prevalent [10], the conventional TLIF is becoming less enough to meet the requirements of both surgeons and patients. The principle of ERAS is to improve patient outcome and reduce complications to help them recover fast [11,12]Figure 1, Figure 2, Figure 3.
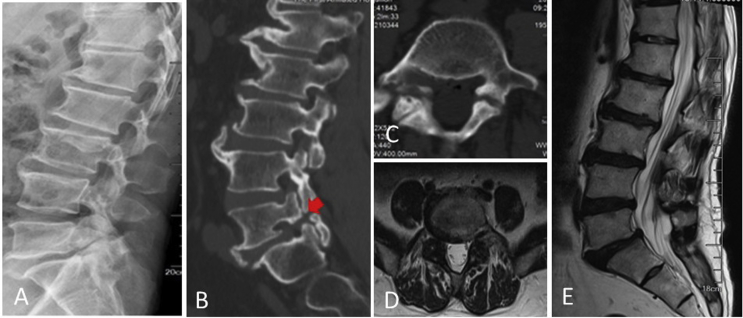
Figure 1.
Lateral (A) radiograph of a 59-year-old male with L5 isthmic spondylolisthesis. The sagittal view (B) and transverse views(C) of preoperative CT and MRI (D, E) showed isthmic spondylolisthesis of L5 (Meyerding Grade I). CT = computed tomography; MRI = magnetic resonance imaging.
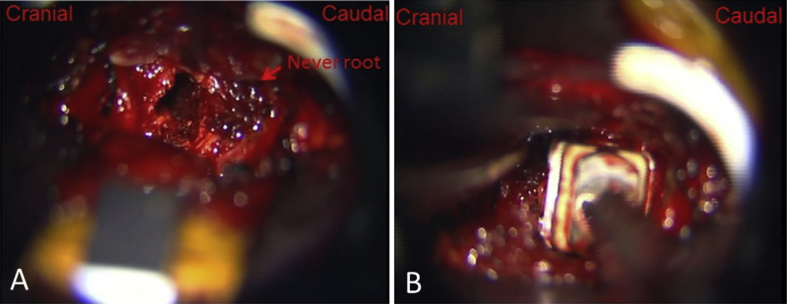
Figure 2.
With the help of microscope, (A) the dural sac and nerve roots were exposed clearly; (B) the cage filled with bone fragments was inserted into the disc space.
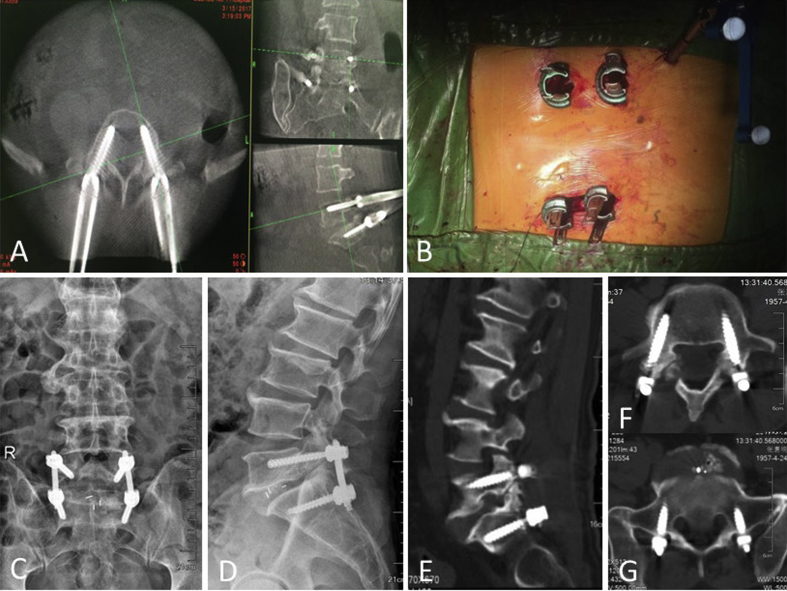
Figure 3.
Intraoperative images (A) showed that navigation based on O-arm device could provide real-time and precise virtual trajectory. (B) The operative incision is small. (C) Anteroposterior and (D) lateral views after novel MIS-TLIF and postoperative CT (E–G) showed the screws remained a satisfactory position. MIS-TLIF = minimally invasive transforaminal lumbar interbody fusion.
Minimally invasive TLIF (MIS-TLIF), as a novel operation, was firstly described by Foley in 2002 [13], with less complications such as blood loss and soft tissue injury [9,14]. Comparing with open TLIF, this minimally invasive procedure had some advantages in terms of amount of bleeding, operation time, hospitalisation time and fusion rates [3,12]. As a novel technology, O-arm navigation has the advancement by providing real-time intraoperative images of the key operating area to assist surgeons improve the performing accuracy. Meanwhile, this new technology can also reduce the radiation exposure [15]. Some facts were revealed that in the O-arm navigation system, pedicle screws placement accuracy was higher than that in the conventional screw insertion with C-arm system [16]. Furthermore, microscope has the advantages of better magnification and illumination, which makes the operative view clearer [17]. Therefore, O-arm navigation and microscope-assisted MIS-TLIF has a very promising blue print, which can not only improve the accuracy in the operation but also help the surgeons gain more confidence [18]. This retrospective study aims to compare the clinical outcomes of O-arm navigation and microscope-assisted MIS-TLIF (modified MIS-TLIF) and conventional TLIF in the treatment of lumbar isthmic spondylolisthesis.
Materials and methods
Clinical data
In this retrospective study, 40 patients suffered from lumbar isthmic spondylolisthesis treated with surgeries between January 2016 and December 2017 in our hospital were enrolled. Eighteen of them were treated with O-arm navigation and microscope-assisted accepted MIS-TLIF (modified MIS-TLIF group), and 22 patients were treated with conventional TLIF (conventional TLIF group). We drew up inclusion criteria as follows: (1) patients had been diagnosed as mild isthmic spondylolisthesis (Meyerding grade I or II) before the operation by X-ray, computed tomography or magnetic resonance imaging; (2) patients had symptoms such as low back pain and/or radiating pain, neurological troubles, impaired ambulation or a combination of above symptoms; (3) patients received conservative therapy for at least 3 months while the symptoms had no significant improvement and none of them had surgery at the responsible segment and (4) 1-level fusion was performed between L4 and S1. The exclusion standards were (1) patients have had spinal surgeries previously; (2) active infection, severe osteoporosis or spinal deformity required surgical intervention; (3) severe internal medical diseases or psychological problems; (4) inability to finish preoperative and postoperative questionnaires or refuse to participate in the follow-up study because of medical or other problems. According to the Meyerding grading system, which divided into four degrees by assess the slippage of the vertebra, Grade I, up to 25%; Grade II, up to 50%; Grade III, up to 75% and Grade IV, up to 100% [19]. The operations were performed by the same surgical team. Except for different surgical methods, the two groups were given the same ERAS-related measurements, including preventive analgesia, prevention of thrombosis, intraoperative temperature control, controlling intravenous fluid infusion, etc.
Surgical techniques
O-arm navigation and microscope-assisted MIS-TLIF
The patient was placed in prone position after general anaesthesia. The first scan was performed by O-arm (Medtronic, Inc., Dublin, Ireland) to acquire three-dimensional images. Then a 3 cm incision was made lateral to the midline on the decompression side. Through the incision, dilator was placed and fixed. An operating microscope (Carl Zeiss, Inc., Oberkochen, Germany) was used during laminectomy and discectomy. The facet joints and the ligamentum flavum were removed by oesteotome and laminectomy rongeur, and the traversing nerve roots, exiting nerve roots and the lateral edge of the dura were exposed and decompressed. The posterolateral annulus was incised, and discectomy was acted completely. After confirming the spacer size, a polyetheretherketone (PEEK) cage filled with autologous cancellous bone was inserted accurately. The homolateral pedicle screw implantation was performed through the decompression incision. Posterior fixation on the contralateral side was done using percutaneous pedicle screws through two 1 cm incisions. A bended rod was place to connect the pedicle screws, and then, the intervertebral space was moderately compressed to make sure the cage was very solid. O-arm scan was acted again to make sure the position of the pedical screws. Then, we sutured incisions, and a drainage tube was placed underneath the fascia.
Conventional TLIF
Conventional TLIF approach was performed using a midline open approach as previously described in the literatures. The process of decompression had no microscope, and all procedures were acted by our naked eyes. The pedicle screws in conventional TLIF group were placed under C-arm fluoroscopy.
Clinical and radiological measurement
Clinical evaluation including patients’ age, gender, operation segment, operation time, intraoperative bleeding, amount of postoperative drainage, bed rest time and length of hospitalisation stay were collected by the surgeons for analysis. All the followed participants were invited to finish clinical evaluation, and the data were obtained at 1, 3, 6 months after the surgery and semiannually until the end. The follow-up time was at least 12 months. Visual analogue scale (VAS) and Oswestry disability index (ODI) were evaluated at every follow-up time. Postoperatively, the position of pedicle screws was evaluated by computed tomography scans (Toshiba, Inc., Minato, Tokyo, Japan) with cross-sectional images of the instrumented pedicle screws. According to the classification used by the study of Laine T et al., screw position was staged as inside pedicle screws (screw inside the pedicle); minor misplacement (perforation of the pedicle cortex by up to 2 mm); moderate misplacement (perforation of the pedicle cortex from 2 to 4 mm); severe misplacement (perforation of the pedicle cortex from 4 to 6 mm, or by more than 6 mm) [6]. The definition of failure screw insertion included pedicle screw misplacement, pedicle screw rupture and bending or loosening and pedicle fracture. Magnetic resonance imaging (Siemens, Inc.) was used to evaluate the nerve root status. All analyses were made in the PACS (Picture Archiving and Communication Systems, Neusoft, Inc., Shenyang, China) independently and objectively to decrease bias.
Statistical analysis
The statistical data were analysed by using SPSS 17.0 (SPSS Inc, Chicago, IL, USA). Student t tests or Wilcoxon rank–sum tests were used to compare the continuous variables. Chi-square test was used to compare the categorical variables between these two groups. A p < 0.05 was considered statistically significant.
Results
Patients’ information from the two groups was shown in Table 1. In the aspect of the age, gender, surgical segment and Meyerding grade, there was no obvious difference. The operating time in the modified MIS-TLIF group (201.67 ± 29.15 min) was significantly longer than that in the conventional TLIF group (132.27 ± 23.64 min) (p < 0.05). The intraoperative bleeding volume in the modified MIS-TLIF group was dramatically less than in the conventional TLIF group (88.33 ± 23.57 ml vs. 255.91 ± 50.95 ml) (p < 0.05). Meanwhile, compared with that in the conventional TLIF group, patients in the modified MIS-TLIF group had less postoperative drainage (p < 0.05). In terms of bed rest time and length of hospital stay, the modified MIS-TLIF group takes less time than the conventional group (p < 0.05). These data have been shown in Table 2. Furthermore, 72 pedicle screws were inserted in the modified MIS-TLIF group, and 88 pedicle screws were inserted in the conventional TLIF group. The precision rate of screw insertion was 95.8%–85.2% (p < 0.05), respectively. The screw position data have been shown in Table 3. No pedicle screw rupture, bending or loosening and pedicle fracture were observed in these two groups. An example case was shown in Figure 1, Figure 2, Figure 3.
Table 1.
The demographic data of the patients in two groups.
| Variable | Modified MIS-TLIF group (n = 18) | Conventional TLIF group (n = 22) | p |
|---|---|---|---|
| Age (years) | 55.61 ± 9.29 | 56.59 ± 7.13 | 0.716 |
| Gender (female/male) | 13/5 | 17/5 | 0.731 |
| Segment [n (%)] | 0.750 | ||
| L4 | 9 (50%) | 9 (40.9%) | |
| L5 | 9 (50%) | 13 (59.1%) | |
| Meyerding grade [n (%)] | 0.427 | ||
| I | 16 (88.9%) | 17 (77.3%) | |
| II | 2 (11.1%) | 5 (22.7%) |
MIS-TLIF = minimally invasive transforaminal lumbar interbody fusion.
Table 2.
Comparison of perioperative data between the modified MIS-TLIF and conventional TLIF groups.
| Parameters | Modified MIS-TLIF group | Conventional TLIF group | p value |
|---|---|---|---|
| Operating time (min) | 201.67 ± 29.15 | 132.27 ± 23.64 | 0.000* |
| Intraoperative blood loss (ml) | 88.33 ± 23.57 | 255.91 ± 50.95 | 0.000* |
| Postoperative drainage (ml) | 42.22 ± 13.52 | 230.45 ± 50.94 | 0.000* |
| Bed rest time (days) | 2.05 ± 0.63 | 4.09 ± 0.68 | 0.000* |
| Hospitalisation stay (days) | 10.33 ± 2.47 | 13.64 ± 3.91 | 0.004* |
*p < 0.05
MIS-TLIF = minimally invasive transforaminal lumbar interbody fusion.
Table 3.
Comparison of the pedicle screw position and accuracy between two groups.
| Parameters | Group |
p | |
|---|---|---|---|
| Modified MIS-TLIF group (n = 18) | Conventional TLIF group (n = 22) | ||
| Screw position | |||
| Inside pedicle screws | 69 | 75 | |
| Minor misplacement | 2 | 9 | |
| Moderate misplacement | 1 | 4 | |
| Severe misplacement | 0 | 0 | |
| Accuracy rated | 95.8% (69/72) | 85.2% (75/88) | 0.012 |
MIS-TLIF = minimally invasive transforaminal lumbar interbody fusion.
VAS and ODI score of all the patients in the two groups were demonstrated to decrease postoperation. However, compared with the conventional TLIF group, the VAS and the ODI score significantly reduced first and sixth month postsurgery in the modified MIS-TLIF group (Table 4). No difference of VAS and the ODI score were found between the two groups at the last follow-up (p > 0.05).
Table 4.
Postoperative VAS and ODI scores of the modified MIS-TLIF and conventional TLIF groups.
| Variable | Modified MIS-TLIF group (n = 18) | Conventional TLIF group (n = 22) | p |
|---|---|---|---|
| VAS for back pain | |||
| Preoperative | 5.94 ± 1.16 | 5.63 ± 0.95 | 0.373 |
| 1 m postsurgerya | 2.61 ± 0.50 | 3.27 ± 0.88 | 0.008* |
| 6 m postsurgery | 1.67 ± 0.68 | 2.27 ± 0.88 | 0.019* |
| Last follow-up | 0.61 ± 0.50 | 0.86 ± 0.63 | 0.180 |
| ODI (%) | |||
| Preoperative | 41.88 ± 2.96 | 41.31 ± 2.14 | 0.485 |
| 1 m postsurgery | 21.67 ± 1.74 | 24.95 ± 1.49 | 0.000* |
| 6 m postsurgery | 15.83 ± 1.42 | 17.13 ± 1.21 | 0.005* |
| Last follow-up | 12.94 ± 1.58 | 13.41 ± 0.96 | 0.286 |
VAS = visual analogue scale; ODI = Oswestry disability index; MIS-TLIF = minimally invasive transforaminal lumbar interbody fusion.
m represents month, *p < 0.05.
The common complications of this surgery including leakage of cerebrospinal fluid, wrong-level surgery, probe and pedicle screws fracture, radiation exposure injure, postoperative infection, etc. No complications were occurred in these two groups. No case in the modified MIS-TLIF group was converted to open surgery.
Discussion
Lumbar isthmic spondylolisthesis is a common disease resulted from the stress or fatigue fracture of pars interaricularis located between the upper and lower vertebra [1]. With the great experience, surgical procedure is necessary after the failure of long conservative treatment such as posterior lumbar interbody fusion, posterolateral fusion, TLIF, etc. These operations are proved successful in the past decades. However, the introoperative extensive detachment of paraspinal muscles and continuous muscle retraction may lead to the muscle necrosis and fibrous scarring, resulting in chronic back pain, stiffness and unsatisfied outcome after surgery [20]. With the development of minimally invasive technology and instrument, patients desire less iatrogenic injury during and after the surgery. TLIF was first described by Harms et al., and it was widely used to treat lumbar disease up to now [5]. The incision of TLIF was different which was in the lateral portion of the vertebral foramen. Through the small incision, we can finish the nerve roots decompression. Clinical curative effect has proved that TLIF had less epidural scarring, intraoperative bleeding and postoperative pain than posterior lumbar interbody fusion. MIS-TLIF was the minimally invasive procedure of TLIF, and Brodano et al. retrospectively analysed 30 patients who accepted surgery (TLIF and MIS-TLIF), and they found that these two operations had same results while MIS-TLIF has smaller incisions, less blood loss and soft tissue trauma, quicker recovery and shorter hospital stays compared with the conventional TLIF [21]. It is reported by Sulaiman and Singh that compared with open TLIF, MIS-TLIF was demonstrated a more appropriate operation in the treatment of degenerative Grade I-II spondylolisthesis [22].
With the development of medical career, the invasive operation became more and more minimal. Therefore, MIS-TLIF assisted by O-arm navigation and microscope was adopted to treat lumbosacral isthmic spondylolisthesis. O-Arm navigation, as the novel navigation technology, it can provide real-time intraoperative 3D images of the operative area to improve pedicle screws accuracy [18]. There is a few studies performed to evaluate the precision of pedicle screw placement assisted by O-arm navigation, but some facts were revealed that O-arm navigation can improve the precision of screw placement since the 1990s [23,24]. According to the study of Laine T, the free-hand pedicle perforation rate (13.4%) was significantly higher than computer-assisted pedicle perforation rate (4.6%) [25]. The study of Jin M et al. revealed that the accuracy of pedicle screw insertion assisted by O-arm navigation was 79% [26], and some prior reports point out that the malposition of free-hand screws insertion is 20–41% [23]. In our study, the accuracy rate of screw implanting in the modified MIS-TLIF group was higher than the conventional TLIF (95.8% vs. 85.2%). At the same time, percutaneous pedicle screw placement which is actually a minimally invasive insertion type can tremendously reduce muscle traction and detachment to avoid muscle damage. Skilled percutaneous pedicle screw fixation in minimal invasive surgery could decrease blood loss, reoperation rate and operative incision. Percutaneous pedicle screw fixation reflexed less muscle atrophy and stronger back muscle strength than the conventional pedicle screw fixation.
The microscope has the advantages of better magnification and illumination in the surgical field. In this study, we combined O-arm navigation and microscope with MIS-TLIF to serve as a novel method to treat lumbar isthmic spondylolisthesis and compared its surgical and clinical outcomes with conventional open TLIF. The microscope can provide a clearer visual field to make the operation more accurate and less traumatic [17]. The adoption of the microscope makes surgeons and assistants share the same visual field of the operation at the same time, which can unite participants to improve efficiency. The microscope system has favourable features such as adjustable magnification according to the requirement, clear image with a good sense of depth and high resolution [17]. These advantages can reduce the risk of nerve injury and clearly identify the bleeding vessels and is conducive to the timely and accurate electric coagulation. It has been reported that the channel created in microscope surgery enables the operators to have a clear enough field of vision through a small incision, which makes the operation safer and more effective [27].
According to our studies, the modified MIS-TLIF group had significantly less intraoperative blood loss, postoperative drainage and less venous transfusion. Furthermore, bed rest time and hospitalisation stay were shortened than conventional MIS-TLIF group. Although the modified MIS-TLIF takes a longer operating time than the conventional MIS-TLIF, it is more conducive to enhance recovery after surgery [12,28].
No serious complication intraoperation and postoperation occurred in all patients. The radiation exposure to the medical staffs was significantly reduced with the modified MIS-TLIF operation, while no data in our study indicated. The O-arm need only one scan before surgery, while the C-arm system need repeat shoot because we need adjust the C-arm to obtain the ideal picture to make sure the screw insertion accurate. Although the operation time of the modified MIS-TLIF was longer than conventional TLIF group, this novel procedure was promoted by our team in the initial stage, and the surgeons need more time to learn and practice. After the long learning curve, we have the confidence that this technique could be modified to become more suitable to the surgical treatment of lumbar isthmic spondylolisthesis.
The study had some limitations such as small sample size, short follow-up and lack of multiple factors analysis. In general, the results demonstrated that MIS-TLIF assisted by O-arm navigation and microscope was safe and effective for the treatment of lumbar isthmic spondylolisthesis. This proposed modified MIS-TLIF operation may have the advantages of less operative trauma, less blood loss and satisfactory short-term curative effect. Further prospective randomised clinical studies should be performed to investigate if this modified MIS-TLIF can provide an advantage for lumbar isthmic spondylolisthesis.
Funding
National Nature Science Foundation of China (grant no. 81802682 and 81802132), Natural Science Foundation of Jiangsu Province (grant no. BK20180199) and Suzhou Science and Technology Program for People's Livelihood (SS201858).
Ethical approval
This study received approval from the local Institutional Ethics Committee. Informed consent was obtained from all patients.
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jot.2019.10.001.
Contributor Information
Peng Peng, Email: smdzw1314@163.com.
Kangwu Chen, Email: chenkangwu@suda.edu.cn.
Hao Chen, Email: haochen0329@126.com.
Kai Zhang, Email: zhangkaimessi@163.com.
Jiajia Sun, Email: orthopaedicvit@163.com.
Peng Yang, Email: ypspine@163.com.
Feng Zhou, Email: 854700065@qq.com.
Yu Liu, Email: 20165232096@stu.suda.edu.cn.
Huilin Yang, Email: sdfyyyhl@163.com.
Haiqing Mao, Email: maohq@suda.edu.cn.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Barbagallo G.M., Piccini M., Alobaid A., Al-Mutair A., Albanese V., Certo F. Bilateral tubular minimally invasive surgery for low-dysplastic lumbosacral lytic spondylolisthesis (LDLLS): analysis of a series focusing on postoperative sagittal balance and review of the literature. Eur Spine J. 2014;23(6):705–713. doi: 10.1007/s00586-014-3543-0. [DOI] [PubMed] [Google Scholar]
- 2.Barbagallo G.M., Certo F., Sciacca G., Albanese V. Bilateral tubular minimally invasive approach for decompression, reduction and fixation in lumbosacral lythic spondylolisthesis. Neurosurg Focus. 2013;35(3) doi: 10.3171/2013.V2.FOCUS13196. Video 9. [DOI] [PubMed] [Google Scholar]
- 3.Chen Y.C., Zhang L., Li E.N., Ding L.X., Zhang G.A., Hou Y. Comparison of posterolateral fusion and posterior lumbar interbody fusion in the treatment of lumbar spondylolithesis: a meta-analysis. J Investig Surg. 2018;5:1–8. doi: 10.1080/08941939.2017.1411543. [DOI] [PubMed] [Google Scholar]
- 4.Petraco D.M., Spivak J.M., Cappadona J.G., Kummer F.J., Neuwirth M.G. An anatomic evaluation of L5 nerve stretch in spondylolisthesis reduction. Spine (Phila Pa 1976) 1996;21(10):1133–1138. doi: 10.1097/00007632-199605150-00002. [DOI] [PubMed] [Google Scholar]
- 5.Harms J., Rolinger H. A one-stager procedure in operative treatment of spondylolistheses: dorsal traction-reposition and anterior fusion (author's transl) Z Orthop Ihre Grenzgeb. 1982;120(3):343–347. doi: 10.1055/s-2008-1051624. [DOI] [PubMed] [Google Scholar]
- 6.Wang Y., Chen K., Chen H., Zhang K., Lu J., Mao H. Comparison between free-hand and O-arm-based navigated posterior lumbar interbody fusion in elderly cohorts with three-level lumbar degenerative disease. Int Orthop. 2019;43(2):351–357. doi: 10.1007/s00264-018-4005-9. [DOI] [PubMed] [Google Scholar]
- 7.Qu J.T., Yu T., Mei W., Tang X.D., Zhang T.J., Shi G.H. Comparison of MIS vs. open PLIF/TLIF with regard to clinical improvement, fusion rate, and incidence of major complication: a meta-analysis. Eur Spine J. 2015;24(5):1058–1065. doi: 10.1007/s00586-015-3890-5. [DOI] [PubMed] [Google Scholar]
- 8.Lee K.H., Yue W.M., Yeo W., Soeharno H., Tan S.B. Clinical and radiological outcomes of open versus minimally invasive transforaminal lumbar interbody fusion. Eur Spine J. 2012;21(11):2265–2270. doi: 10.1007/s00586-012-2281-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Seng C., Siddiqui M.A., Wong K.P., Zhang K., Yeo W., Tan S.B. Five-year outcomes of minimally invasive versus open transforaminal lumbar interbody fusion: a matched-pair comparison study. Spine (Phila Pa 1976) 2013;38(23):2049–2055. doi: 10.1097/BRS.0b013e3182a8212d. [DOI] [PubMed] [Google Scholar]
- 10.Wang M.Y., Chang H.K., Grossman J. Reduced acute care costs with the ERAS® minimally invasive transforaminal lumbar interbody fusion compared with conventional minimally invasive transforaminal lumbar interbody fusion. Neurosurgery. 2018;83(4):827–834. doi: 10.1093/neuros/nyx400. [DOI] [PubMed] [Google Scholar]
- 11.Soeters P.B. The Enhanced Recovery after Surgery (ERAS) program: benefit and concerns. Am J Clin Nutr. 2017;106(1):10–11. doi: 10.3945/ajcn.117.159897. [DOI] [PubMed] [Google Scholar]
- 12.Wang M.Y., Chang P.Y., Grossman J. Development of an Enhanced Recovery after Surgery (ERAS) approach for lumbar spinal fusion. J Neurosurg Spine. 2017;26(4):411–418. doi: 10.3171/2016.9.SPINE16375. [DOI] [PubMed] [Google Scholar]
- 13.Foley K.T., Lefkowitz M.A. Advances in minimally invasive spine surgery. Clin Neurosurg. 2002;49:499–517. [PubMed] [Google Scholar]
- 14.Eleftherios A., Mario C.Y.N. Comparison of minimally invasive fusion and instrumentation versus open surgery for severe stenotic spondylolisthesis with high-grade facet joint osteoarthritis. Eur Spine J. 2013;22(8):1731–1740. doi: 10.1007/s00586-013-2732-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Boon Tow B.P., Yue W.M., Srivastava A., Lai J.M., Guo C.M., Wearn Peng B.C. Does navigation improve accuracy of placement of pedicle screws in single-level lumbar degenerative spondylolisthesis? A comparison between free-hand and three-dimensional O-arm navigation techniques. J Spinal Disord Tech. 2015;28(8):E472–E477. doi: 10.1097/BSD.0b013e3182a9435e. [DOI] [PubMed] [Google Scholar]
- 16.Parker S.L., Mcgirt M.J., Farber S.H., Amin A.G., Rick A.M. Accuracy of free-hand pedicle screws in the thoracic and lumbar spine: analysis of 6816 consecutive screws. Neurosurgery. 2011;68(1):170–178. doi: 10.1227/NEU.0b013e3181fdfaf4. [DOI] [PubMed] [Google Scholar]
- 17.Basques B.A., Golinvaux N.S., Bohl D.D., Alem Y., Toy J.O., Varthi A.G. Use of an operating microscope during spine surgery is associated with minor increases in operating room times and no increased risk of infection. Spine (Phila Pa 1976) 2014;39(22):1910–1916. doi: 10.1097/BRS.0000000000000558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kleck C.J., Johnson C., Akiyama M., Burger E.L., Cain C.J., Patel V.V. One-step minimally invasive pedicle screw instrumentation using O-arm and stealth navigation. Clin Spine Surg. 2018;31(5):197–202. doi: 10.1097/BSD.0000000000000616. [DOI] [PubMed] [Google Scholar]
- 19.Niggemann P., Kuchta J., Grosskurth D., Beyer H.K., Hoeffer J., Delank K.S. Spondylolysis and isthmic spondylolisthesis: impact of vertebral hypoplasia on the use of the Meyerding classification. Br J Radiol. 2012;85(1012):358–362. doi: 10.1259/bjr/60355971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gu G., Zhang H., Fan G., He S., Cai X., Shen X. Comparison of minimally invasive versus open transforaminal lumbar interbody fusion in two-level degenerative lumbar disease. Int Orthop. 2014;38(4):817–824. doi: 10.1007/s00264-013-2169-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brodano G.B., Martikos K., Lolli F., Gasbarrini A., Cioni A., Bandiera S. Transforaminal lumbar interbody fusion in degenerative disc disease and spondylolisthesis grade I: minimally invasive versus open surgery. J Spinal Disord Tech. 2015;28(10):E559–E564. doi: 10.1097/BSD.0000000000000034. [DOI] [PubMed] [Google Scholar]
- 22.Sulaiman W.A., Singh M. Minimally invasive versus open transforaminal lumbar interbody fusion for degenerative spondylolisthesis grades 1-2: patient-reported clinical outcomes and cost-utility analysis. Ochsner J. 2014;14(1):32–37. [PMC free article] [PubMed] [Google Scholar]
- 23.Jin M., Liu Z., Qiu Y., Yan H., Han X., Zhu Z. Incidence and risk factors for the misplacement of pedicle screws in scoliosis surgery assisted by O-arm navigation-analysis of a large series of one thousand, one hundred and forty five screws. Int Orthop. 2017;41(4):773–780. doi: 10.1007/s00264-016-3353-6. [DOI] [PubMed] [Google Scholar]
- 24.Kosmopoulos V., Schizas C. Pedicle screw placement accuracy: a meta-analysis. Spine (Phila Pa 1976) 2007;32(3):E111–E120. doi: 10.1097/01.brs.0000254048.79024.8b. [DOI] [PubMed] [Google Scholar]
- 25.Laine T., Lund T., Ylikoski M., Lohikoski J., Schlenzka D. Accuracy of pedicle screw insertion with and without computer assistance: a randomised controlled clinical study in 100 consecutive patients. Eur Spine J. 2000;9(3):235–240. doi: 10.1007/s005860000146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jin M., Liu Z., Liu X., Yan H., Han X., Qiu Y. Does intraoperative navigation improve the accuracy of pedicle screw placement in the apical region of dystrophic scoliosis secondary to neurofibromatosis type I: comparison between O-arm navigation and free-hand technique. Eur Spine J. 2016;25(6):1729–1737. doi: 10.1007/s00586-015-4012-0. [DOI] [PubMed] [Google Scholar]
- 27.Tian W., Xu Y.F., Liu B., Liu Y.J., He D., Yuan Q. Computer-assisted minimally invasive transforaminal lumbar interbody fusion may Be better than open surgery for treating degenerative lumbar disease. Clin Spine Surg. 2017;30(6):237–242. doi: 10.1097/BSD.0000000000000165. [DOI] [PubMed] [Google Scholar]
- 28.Soffin E.M., Vaishnav A.S., Wetmore D., Barber L., Hill P., Gang C.H. Design and implementation of an enhanced recovery after surgery (ERAS) program for minimally invasive lumbar decompression spine surgery: initial experience. Spine (Phila Pa 1976) 2019;44(9):E561–E570. doi: 10.1097/BRS.0000000000002905. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.