Abstract
Background:
Tobacco remains the leading cause of preventable death in the United States, with 41,000 deaths attributable to secondhand smoke (SHS) exposure. On July 30, 2018, the U.S. Department of Housing and Urban Development passed a rule requiring public housing authorities to implement smoke-free housing (SFH) policies.
Objectives:
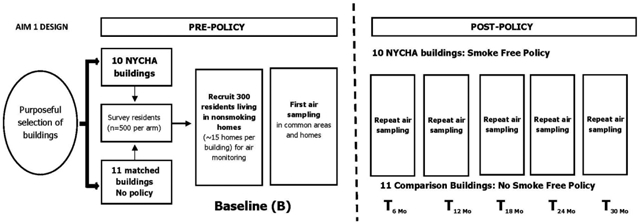
Prior to SFH policy implementation, we measured self-reported and objective SHS incursions in a purposeful sample of 21 high-rise buildings (>15 floors) in New York City (NYC): 10 public housing and 11 private sector buildings where most residents receive federal housing subsidies (herein ‘Section 8’ buildings).
Methods:
We conducted a baseline telephone survey targeting all residents living on the 3rd floor or higher of selected buildings: NYC Housing Authority (NYCHA) residents were surveyed in April-July 2018 (n=559), and residents in ‘Section 8’ buildings in August-November 2018 (n=471). We invited nonsmoking household participants to enroll into a longitudinal air monitoring study to track SHS exposure using: (1) nicotine concentration from passive, bisulfate-coated nicotine filters and (2) particulate matter (PM2.5) from low-cost particle monitors. SHS was measured for 7-days in non-smoking households (NYCHA n=157, Section 8 n=118 households) and in building common areas (n=91 hallways and stairwells).
Results:
Smoking prevalence among residents in the 21 buildings was 15.5%. Two-thirds of residents reported seeing people smoke in common areas in the past year (67%) and 60% reported smelling smoke in their apartments coming from elsewhere. Most stairwells (88%) and hallways (74%) had detectable nicotine levels, but nicotine was detected in only 9.9% of non-smoking apartments. Substantial variation in nicotine and PM2.5 was observed between and within buildings; on average nicotine concentrations were higher in NYCHA apartments and hallways than in Section 8 buildings (p<0.05), and NYCHA residents reported seeing smokers in common areas more frequently.
Conclusions:
SFH policies may help in successfully reducing SHS exposure in public housing, but widespread pre-policy incursions suggest achieving SFH will be challenging.
Keywords: smoke-free housing, secondhand smoke, multiunit housing, policy, public housing authority, air quality, air nicotine, PM2.5
Graphical Abstract
Introduction:
Tobacco remains the leading cause of preventable death in the United States, responsible for more than 440,000 deaths annually, of which 41,000 deaths are attributable to secondhand smoke (SHS) exposure.1,2
Low-income residents in urban settings, including residents in public housing, are at high risk for SHS exposure compared to the general population for two reasons.3-6 First, despite overall declines in smoking in the past 30 years, smoking rates among low-income residents and residents living in public housing developments tend to be higher than in the general population.3-6 Second, urban low-income and public housing residents also more likely than higher income residents to live in multiunit housing, an environment that places all residents at elevated risk for involuntary SHS exposure due to smoke accumulation compared to residents living in detached housing.7-9 Numerous air quality studies have demonstrated that that SHS accumulates in shared areas of MUH buildings such as hallways and stairwells and transfers between apartments, placing non-smokers at risk for SHS exposure.7,10-12
Beginning July 30th, 2018, per a rule passed by the federal Department of Urban Development (HUD), all public housing authorities (PHAs) were required to implement smoke free policies in their developments.13 While previous studies have examined implementation impacts of smoke-free housing (SFH) policies on self-reported SHS exposure, 14-17 only a small number of studies have evaluated the impacts of SFH policies on objectively measured SHS exposure metrics such as airborne nicotine concentrations or particulate matter concentrations less than 2.5 micrometers in diameter (PM2.5).10,18-20 Results have been mostly inconclusive, with most studies documenting a modest post-policy reduction in SHS in common areas, but studies have had limited sample size and follow up duration.
As part of a larger natural experiment study to assess the impact of the SFH policy on health outcomes, we completed a pre-policy baseline examination of self-reported SHS incursions and objective air quality measures in a large sample of non-smoking households and common areas in 21 select public and private sector high-rise developments comprised predominantly of low-income residents in New York City (NYC). Currently, the NYC Housing Authority (NYCHA) is the largest housing authority in the United States, with more than 400,000 residents.13,21 Nearly 100,000 additional NYC households receive rental assistance in the form of housing vouchers, through a program known as Section 8, to subsidize their rental costs for apartments in private sector buildings.22
We report here our pre-policy baseline findings on levels of SHS exposure in both public and private sector multi-unit housing environments serving lower income residents. These findings not only provide empirical evidence regarding the context in which the policy is being introduced and thus the potential public health impacts of the policy if effectively enforced, but also characterize the extent to which SHS exposure will continue to affect lower-income residents living in private sector multi-unit housing. The current rule only applies to public housing, leaving millions of residents nationwide residing in multi-unit housing in the private sector, Section 8, and other voucher programs without policies prohibiting indoor smoking. Precisely because smoke-free policies in public housing settings have strong potential for further reducing SHS exposure disparities, they require rigorous evaluation to establish effectiveness and health impact to inform future smoke-free housing policy development and practice for a wider array of residential settings.
Methods:
Study Population and Procedures
We selected a purposeful sample of 21 high-rise buildings located in Manhattan and the Bronx—10 public housing developments operated by NYCHA and 11 developments operated by private building managers, in which most residents receive Section 8 housing subsidy vouchers (herein ‘Section 8 buildings’). The following building eligibility criteria were established to ensure homogeneity across buildings: (1) high-rise (> 15 floors); (2) large resident population (>150 families); (3) 80% or greater of resident population black or Hispanic (mirroring racial/ethnic distribution found in most NYCHA buildings); and (4) 20% or greater of resident population under the age of 18. Detailed information on the study population and procedures has been described elsewhere.23
Resident Survey
We conducted a baseline resident survey by telephone, with ‘mop-up’ door-to-door enrollment in the 10 selected NYCHA buildings in April-July 2018, immediately prior to the federal SFH rule going into effect, and in the 11 selected private-sector buildings in August-November 2018. We targeted all households in selected buildings with telephone numbers above the third floor to avoid the biasing influence of ambient outdoor PM2.5 and SHS. Adults aged 18 and older who spoke English or Spanish were eligible for participation; we invited one member per household to participate. The telephone survey was 15 minutes in length and included questions about demographics, cigarette smoking behavior, SHS incursions, knowledge about SHS, and support of smoke-free policies. Self-reports of SHS incursions were obtained by asking the following questions: “During the past 12 months, have you smelled cigarette smoke in your home that comes from another apartment or from outside? [yes/no]” and “Do people currently smoke in common areas such as lobbies, stairwells, hallways and elevators? [yes/no]”.2,8,13,24,25 The survey yielded 1,030 responses, for a response rate of 35.3% among NYCHA residents (n=559) and 32.1% among Section 8 residents (n=471). Detailed information on the resident survey is described elsewhere.23
Objective Air Quality and Secondhand Smoke Measures
Following survey completion, we invited survey participants from non-smoking households to participate in a longitudinal air monitoring study. A volunteer sample of residents from 275 non-smoking households enrolled (NYCHA n=157, Section 8 buildings n=118). Non-smoking households were defined as having no household members who, at the time of enrollment, were known to smoke cigarettes or use other tobacco products including cigars, cigarillos or e-cigarettes. Detailed information on objective air quality and SHS measures are described elsewhere.23 Briefly, we placed passive, bisulfate-coated nicotine filters prepared by the Secondhand Smoke Exposure Assessment Laboratory at Johns Hopkins University (http://www.shsmonitoring.org/analysis/lab/ ) in resident living rooms to measure airborne nicotine concentration over a 7-day sampling period. The detection limit for the 7-day samples was 0.017 μg/m3. Alongside the nicotine filters, we also placed AirBeam monitors, novel low-cost particle sensors 26 that have been shown to be successful and reproducible in monitoring ambient PM 27 , in order to measure airborne PM concentrations over the same 7-day period. AirBeam monitors were individually calibrated with cigarette smoke in a dynamic exposure chamber against a DataRam PDR 1500 instrument—a more advanced, manufacturer-calibrated light scattering PM2.5 monitoring instrument (Thermo Scientific).28 Linear calibration curves were generated, creating best fit and regression equations to apply to the PM2.5 values in our sample. In addition to air monitoring in non-smoking households, we also placed passive nicotine filters in 2 randomly selected hallways and 2 randomly selected stairwells (target of n=20 each in NYCHA and n=22 each in Section 8) per building to assess the presence of nicotine in common areas.
Data Analysis:
From survey responses, we estimated the percentage of self-reported smokers and prevalence of SHS incursions in NYCHA and Section 8 buildings, and we compared differences using a Chi-Square test. Although non-smoking households were defined as having no household members known to smoke cigarettes or use other tobacco products at the time of the survey, during air monitoring data collection, we identified some evidence of indoor smoking (by a resident or guest) in 8 households, and their data were excluded. In addition, we excluded 7 households from analysis where there was evidence of AirBeam monitor malfunction. In common areas, additional air filters were placed in hallways when hallways contained a central common area (5 additional filters in NYCHA and 2 in Section 8). Nine common area observations were excluded from analysis due to equipment tampering. Our final effective baseline sample for common area dwellings was 39 stairwells (n=20 for NYCHA and n=19 for Section 8) and 42 hallways (n=19 for NYCHA and n=23 for Section 8). We calculated the geometric means for airborne nicotine concentrations in NYCHA and Section 8 buildings and compared differences using Wilcoxon Rank Sum Test. We estimated the percentage of detectable nicotine in NYCHA and Section 8 buildings (defining non-smoking apartments and building common areas as above the level of detection if their nicotine concentration was >0.017 μg/m3)23 and compared differences using a Chi-Square test. All estimates were computed separately for common areas (stairwells and hallways) and non-smoking apartments. We calculated the means for PM2.5 in NYCHA and Section 8 non-smoking apartments and compared differences using independent t-tests. Lastly, we estimated the percentage of non-smoking apartments in NYCHA and Section 8 buildings with PM2.5 levels above the Environmental Protection Agency (EPA) annual standard of 12.0 μg/m3, and compared differences using a Chi-Square test.29 All estimates were considered statistically significant if their p-value from a two-tailed test was ≤0.05. Previous studies have assessed the validity of self-reported SHS exposure against nicotine and cotinine levels and have found good agreement between the measures.30 All analysis were performed using SAS 9.4 software.
Results:
In part reflecting building eligibility criteria, the demographic composition and prevalence of smoking among residents living in NYCHA and Section 8 buildings were highly comparable (p>0.05) (Table 1). Detailed information on socio-demographic characteristics for non-smoking households enrolled into the longitudinal air monitoring study is described elsewhere.23 Overall smoking prevalence among residents in the 21 selected buildings was 15.5%. Nearly three quarters (73.5%) of residents had smoke-free policies in their homes, two-thirds (67.4%) of residents reported seeing smoke in the common areas, and more than half (60.0%) of residents reported smelling cigarette smoke in their home over the past year, coming from the outside (Table 1). Smoking habits and personal smoke-free housing policies were largely comparable between NYCHA and Section 8 building residents. However, residents of NYCHA reported seeing smoking in common areas with higher frequency than residents of Section 8 buildings (77.3% NYCHA, 55.6% Section 8, p<0.0001).
Table 1.
Smoking Prevalence and Second-Hand Smoke Incursions across NYC Residents living in Low-Income, Subsidized Housing, New York City, 2018
| Overall (n=1030) |
NYC Housing Authority Residents (n=559) |
Comparison “Section 8” Residents (n=471) |
||
|---|---|---|---|---|
| % | % | % | p-value | |
| Demographic Characteristics | ||||
| Children in home (under the age of 18) | 37.8 | 37.4 | 38.3 | 0.768a |
| Education Level (< High School) | 22.7 | 24.3 | 20.7 | 0.031a |
| Spanish Language | 28.4 | 28.5 | 28.3 | 0.852a |
| Self-Reported Cigarette Smoking Behaviors | ||||
| Current smoker | 15.5 | 15.7 | 15.2 | 0.829a |
| Smokers in the home | 10.4 | 9.9 | 11.0 | 0.573a |
| Smoke-free policy in the home | 73.5 | 74.6 | 72.2 | 0.368a |
| Self-Reported Secondhand Smoke Incursions | ||||
| Seeing smoke in common areas | 67.4 | 77.3 | 55.6 | <0.0001a |
| Smelling cigarette smoke, past year | 60.0 | 62.3 | 57.2 | 0.095a |
*p-values based on Chi-Square Test for Independence
Air quality monitoring results indicated evidence of widespread cigarette smoking in indoor common areas such as stairwells and hallways (Table 2). More than three quarters of common areas (87.5% of stairwells and 73.8% of hallways) had levels of detectable nicotine. Compared to hallways in Section 8 buildings, hallways in NYCHA buildings had a significantly higher mean (SD) airborne nicotine concentrations (NYCHA = 0.45 (0.16) μg/m3, Section 8 = 0.09 (0.03) μg/m3, p=0.004) and higher percentages of detectable nicotine (NYCHA = 89.5%, Section 8 = 60.9%, p=0.036). Compared to stairwells in Section 8 buildings, stairwells in NYCHA buildings had slightly higher mean (SD) airborne nicotine concentrations, but differences were not statistically significant (NYCHA = 0.43 (0.11) μg/m3, Section 8 = 0.24 (0.10) μg/m3, p=0.371). The overall airborne nicotine concentration for non-smoking households in public and private sector high-rise buildings was 0.021 μg/m3. 9.9% of non-smoking households had levels of nicotine above the detection limit of 0.017 μg/m3.23 Compared to non-smoking Section 8 households, a higher proportion of non-smoking NYCHA households had detectable nicotine levels (NYCHA = 13.1%, Section 8 = 5.5%, p=0.041).
Table 2.
Pre-Policy Air Quality Findings in the Longitudinal Study for those Enrolled in the Baseline Air Sampling Study
| Overall | NYC Housing Authority Residents |
Comparison “Section 8” Residents |
|||||
|---|---|---|---|---|---|---|---|
| N | Mean (SD) or % |
N | Mean (SD) or % |
N | Mean (SD) or % |
p-value | |
| Stairwell | 39 | 20 | 19 | ||||
| Nicotine Geomean | 0.32 (0.08) | 0.43 (0.11) | 0.24 (0.10) | 0.371b | |||
| % above LODd,e | 87.5 | 94.7 | 81.0 | 0.188a | |||
| Hallway | 42 | 19 | 23 | ||||
| Nicotine Geomean | 0.19 (0.05) | 0.45 (0.16) | 0.09 (0.03) | 0.004b | |||
| % above LODd,e | 73.8 | 89.5 | 60.9 | 0.036a | |||
| Apartment | |||||||
| Airborne Nicotine Level | 263 | 153 | 110 | ||||
| Nicotine Geomean | 0.021 (0.001) | 0.023 (0.002) | 0.019 (0.001) | 0.049b | |||
| % above LODd,e | 9.9 | 13.1 | 5.5 | 0.041a | |||
| Particulate Matter 2.5 Level | 242 | 137 | 105 | ||||
| PM 2.5 Mean | 20.96 (10.73) | 22.10 (10.80) | 19.48 (10.49) | 0.059c | |||
| % above EPA Standard | 83.1 | 89.8 | 74.3 | 0.001a | |||
*p-values based on Chi-Square Test for Independence
*p-values based on Wilcoxon Rank Sum Test
*p-values based on Independent T-Test
*Nicotine levels were calculated using ½ L.O.D. for any values below the detection limit of 0.017 μg/m3
*PM2.5 levels were calculated using the EPA standard of 12 μg/m3
More than half (83.1%) of non-smoking households in our sample had PM2.5 measurements above the EPA annual standard of 12 μg/m3. The mean (SD) household PM2.5 concentration was 20.96 (10.73) μg/m3 for all households. Compared to households in Section 8 buildings, a higher proportion of households in NYCHA buildings had elevated (i.e., above 12 μg/m3) PM2.5 levels (NYCHA = 89.8%; Section 8 = 74.3%, p =0.001).
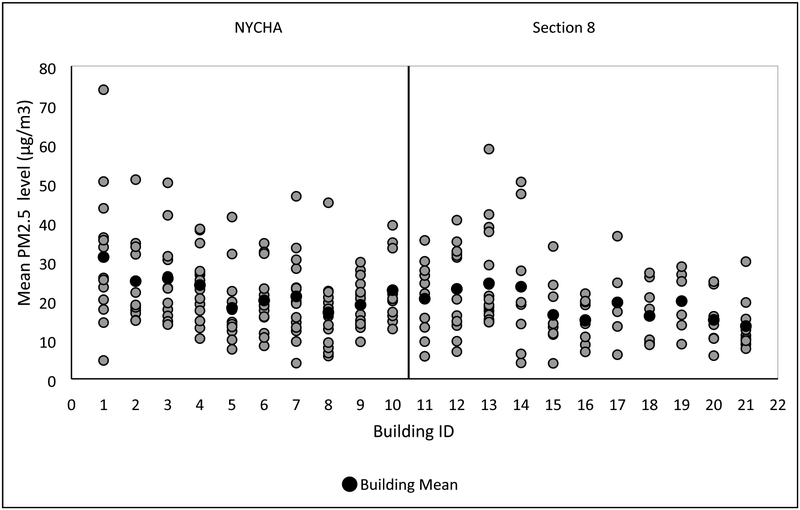
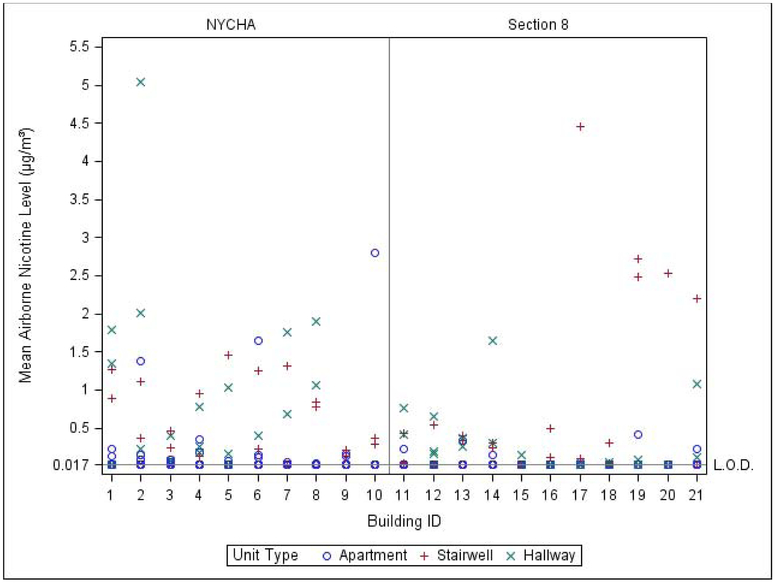
Air quality monitoring results showed substantial between- and within-building variability across our sample of 21 buildings (Figures 1a and 1b). Across the 275 enrolled non-smoking households, airborne nicotine concentrations ranged from 0.017 μg/m3 to 2.798 μg/m3, and PM2.5 concentrations ranged from 3.96 μg/m3 to 73.95 μg/m3. Airborne nicotine concentrations measured in building common areas (n=91) ranged from 0.017 μg/m3 to 5.04 μg/m3. More notably, building-level variation appeared greater across stairwells of Section 8 buildings compared to stairwells in NYCHA buildings.
Figure 1a.
Particulate Matter 2.5 Levels, Between-and-Within Building Variability for Low-Income MUH in NYC
*N=242 (NYCHA= 137, Section 8=105)
* PM2.5 levels were calculated using the EPA standard of 12 μg/m3
Figure 1b.
Airborne Nicotine Levels, Between-and-Within-Building Variability for Low-Income MUH in NYC
*Apartments n=263 (NYCHA= 153, Section 8=110); Stairwells n=39 (NYCHA=20, Section 8=19); Hallways n=42 (NYCHA= 19, Section 8=23)
*Nicotine levels were calculated using ½ L.O.D. for any values below the detection limit of 0.017 μg/m3
Discussion:
In this large-sample assessment of SHS exposure in low-income, subsidized housing in NYC, conducted prior to implementation of the nationwide smoke-free housing policy for PHAs, we found a high prevalence of SHS exposure in both public and private sector high-rise buildings. While all 21 buildings in our sample had policies banning smoking in common areas prior to policy implementation, most residents reported seeing people smoke in indoor common areas and we found high levels of detectable nicotine in stairwells and hallways, confirming that widespread indoor cigarette smoking occurs in low-income, subsidized housing in NYC.
Airborne nicotine concentrations were significantly greater in hallways in NYCHA buildings compared to Section-8 buildings, as were percentages of detectable nicotine, suggesting a greater propensity for cigarette smoking in the NYCHA building indoor common areas, at least in our sample of buildings, yet both building settings had extensive documentation of SHS exposure, particularly in common areas. We also identified that a majority non-smoking households in our sample had average PM2.5 levels above the EPA’s annual standard of 12 μg/m3, although the source of indoor PM in our measurements was unclear. Previous research has demonstrated a strong correlation between fine particles and tobacco smoke8,11,12, yet only 9.9% of homes had detectable nicotine levels. Overall, our air quality measures, in combination with the residents’ self-reported measures of SHS exposure, provide evidence of widespread indoor cigarette smoking in low-income, subsidized MUH in NYC.
To our knowledge, this study includes the largest sample of non-smoking households and building common areas (stairwells and hallways) to measure SHS incursions residential high-rise developments, with plans to measure incursions longitudinally for up to 2.5 years post-policy. Previous studies have measured objective SHS incursions prior to SFH policy implementation in smaller sample of households and building common areas8,10,19,20. One previous study conducted across five Boston Housing Authority (BHA) developments recruited 40 households, comprised of smoking and non-smoking households, as well as 10 common building areas to objectively measure SHS incursions prior to the implementation of federal SFH policies.10,19 Another study recruited 49 low-income MUH residences in the greater Boston area to objectively measure nicotine concentrations among smoking and non-smoking households.8 A third study recruited 172 households across Philadelphia public housing developments to objectively measure airborne nicotine concentrations in non-smoking households.20 Importantly, it also prospectively measures SHS incursions in private sector multi-unit housing serving other lower-income residents not affected by the SFH policy, allowing for a sustained investigation into policy approaches to reduce disparities in two settings that have disproportionately been affected by SHS and other poor housing quality exposures.
For building-wide smoke-free policies to be effective, PHA agencies will need to provide consistent support to help residents develop a culture of adherence.31,32 Prior to the implementation of SFH policy, residents expressed how PHAs needed to communicate the benefits of the policy in an effective manner, and provide smokers with alternatives to smoking, i.e. smoking cessation resources to maximize implementation effectiveness.33-35 Achieving the goal of smoke-free housing will be challenging given the high volume of residents in NYC living in public housing and the limited number of resources available. Thus, as part of our larger natural experiment study to measure health outcomes, we also aim to study the post-implementation process in order to better understand challenges PHAs face during implementation and to offer guidance to optimize implementation effectiveness.33 Broadly, evaluating the HUD policy presents an important opportunity to elucidate the health and health equity benefits and effectiveness of SFH policies in residential settings. In the past 30 years, a large body of evidence has documented health hazards from SHS exposure, including elevated risk for cancers, coronary artery disease, stroke, and serious respiratory problems in adults, and congenital defects, sudden infant death syndrome, lower respiratory infections, middle ear infections, and asthma among children.36,37 While the potential for health benefits from smoke-free housing regulations is clear, the actual short- and long-term health impacts of such a policy at improving health and health equity are as yet unknown. Findings of pervasive high SHS exposure in this baseline study are an important reminder of the importance of policy strategies to remediate and improve housing quality in disadvantaged neighborhoods. However, to achieve health equity in housing, additional strategies to will be needed to also address housing affordability, and residential stability.
Strengths and Limitations
Our study had a number of strengths. We engaged a very large and diverse sample of low-income residents living in high-rise multiunit housing in NYC to collect self-reported and objective air quality data on 275 nonsmoking households and more than 90 common areas (stairwells and hallways). Previous studies have found good agreement between self-reported SHS exposure and nicotine levels.30 By sampling public housing and private sector buildings, we were able to contrast SHS exposures between the two settings. A key attribute of the study is that we collected data prior to implementation of a nationwide HUD smoke-free housing policy for PHAs. These findings thus provide a robust baseline assessment of SHS, both in a setting where the policy will be implemented and in a setting in which it will not. At the same time, our study had a number of limitations. First, AirBeam monitors used for our study continuously measured PM in one-minute intervals using light scattering techniques,38 a method that can be subject to error. To improve the accuracy of our data and minimize error, we systematically applied calibration curves to our PM data. While prior studies have found strong correlation between fine particles and tobacco smoke, 8,11,12 fine particles are not specific to tobacco smoke and can result from other sources. Second, our study consists of 21 purposefully selected public and private sector high-rise buildings in NYC; therefore, our findings may not be generalizable to all MUH settings. The narrow focus of this study provides an important starting point for further investigations. While achieving complete SFH goals may be challenging, reducing SHS exposure for low-income residents in urban settings, where most residents require public housing, may improve short-and-long term health quality, creating a more equitable health environment.
Conclusion:
Our findings confirm that residents living in low-income, subsidized housing in NYC are at elevated risk of exposure to SHS. Implementation of smoke-free policies may help in successfully reducing exposure to SHS in low-income MUH. To better understand the impact of the HUD smoke-free housing policy on reducing SHS exposure, longitudinal objective air monitoring studies are needed.
Highlights:
SFH policies have been implemented across PHAs nationwide
We measured self-reported and objective SHS incursions in low-income MUH in NYC
Most stairwells (88%) and hallways (74%) had detectable levels of nicotine
Substantial variation in nicotine and PM2.5 was observed between and within buildings
SFH policies may help in successfully reducing SHS exposure in public housing
Acknowledgements:
The authors of this manuscript would like to acknowledge the contributions made by Andrea Mata and Anne-Marie Flatley from the New York City Housing Authority, Health Initiatives Department. Additionally, the PM measurements were supported by the Inhalation Facility Core of NYU’s National Institute of Environmental Health Sciences Center and Excellence (ES000260).
Funding
This manuscript describes the SHS exposure assessment component of a larger study. The work reported in this publication was supported by the National Cancer Institute of the National Institute of Health under Award Number R01CA220591. The content is solely the responsibility of the authors and does not necessarily represent the official news of the National Institutes of Health.
Abbreviation:
- SHS
Secondhand Smoke
- HUD
Department of Housing and Urban Development
- PHA
Public Housing Authority
- SFH
Smoke-Free Housing
- PM 2.5
Particulate Matter 2.5
- NYCHA
New York City Housing Authority
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Ethics Approval and Consent to Participate
The study protocol and procedures were approved by the Institutional Review Board at the New York University School of Medicine on July 20, 2017; IRB number: i17-00968. Written informed consent is obtained from study participants by trained field staff and Memorandums of Understanding were signed by all institutions involved for the appropriate exchange of data following good clinical practice and HIPAA compliance. The study provides participants’ households with information on the aggregate results of the air monitoring in their respective buildings.
Conflict of interest statement
At this time, all contributing authors of this manuscript have no competing financial interests to disclose.
References:
- 1.California Environmental Protection Agency. Proposed Identification of Environmental Tobacco Smoke as a Toxic Air Contaminant. Sacramento (CA)2005. [Google Scholar]
- 2.Office on Smoking and Health (US). The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. Atlanta (GA): Centers for Disease Control and Prevention (US);2006. [PubMed] [Google Scholar]
- 3.King BA, Peck RM, Babb SD. National and state cost savings associated with prohibiting smoking in subsidized and public housing in the United States. Prev Chronic Dis. 2014;11:E171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jamal A, Homa DM, O'Connor E, et al. Current cigarette smoking among adults - United States, 2005-2014. MMWR Morb Mortal Wkly Rep. 2015;64(44):1233–1240. [DOI] [PubMed] [Google Scholar]
- 5.Lopez PM, Islam N, Feinberg A, et al. A Place-Based Community Health Worker Program: Feasibility and Early Outcomes, New York City, 2015. Am J Prev Med. 2017;52(3S3):S284–S289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Helms VE, King BA, Ashley PJ. Cigarette smoking and adverse health outcomes among adults receiving federal housing assistance. Prev Med. 2017;99:171–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.King BA, Cummings KM, Mahoney MC, Juster HR, Hyland AJ. Multiunit housing residents' experiences and attitudes toward smoke-free policies. Nicotine Tob Res. 2010;12(6):598–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kraev TA, Adamkiewicz G, Hammond SK, Spengler JD. Indoor concentrations of nicotine in low-income, multi-unit housing: associations with smoking behaviours and housing characteristics. Tob Control. 2009;18(6):438–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nguyen KH, Gomez Y, Homa DM, King BA. Tobacco Use, Secondhand Smoke, and Smoke-Free Home Rules in Multiunit Housing. Am J Prev Med. 2016;51(5):682–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.MacNaughton P, Adamkiewicz G, Arku RE, Vallarino J, Levy DE. The impact of a smoke-free policy on environmental tobacco smoke exposure in public housing developments. Sci Total Environ. 2016;557-558:676–680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Arku RE, Adamkiewicz G, Vallarino J, Spengler JD, Levy DE. Seasonal variability in environmental tobacco smoke exposure in public housing developments. Indoor Air. 2015;25(1):13–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.King BA, Travers MJ, Cummings KM, Mahoney MC, Hyland AJ. Secondhand smoke transfer in multiunit housing. Nicotine Tob Res. 2010;12(11):1133–1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.US Department of Housing and Urban Development. Instituting Smoke-Free Public Housing: A Proposed Rule by the Housing and Urban Development Department. HUD; website. 2015; http://portal.hud.gov/hudportal/documents/huddoc?id=smoke-freepublichousing.pdf. [Google Scholar]
- 14.Young W, Karp S, Bialick P, et al. Health, Secondhand Smoke Exposure, and Smoking Behavior Impacts of No-Smoking Policies in Public Housing, Colorado, 2014-2015. Prev Chronic Dis. 2016;13:E148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pizacani BA, Maher JE, Rohde K, Drach L, Stark MJ. Implementation of a smoke-free policy in subsidized multiunit housing: effects on smoking cessation and secondhand smoke exposure. Nicotine Tob Res. 2012;14(9):1027–1034. [DOI] [PubMed] [Google Scholar]
- 16.Kingsbury JH, Reckinger D. Clearing the Air: Smoke-Free Housing Policies, Smoking, and Secondhand Smoke Exposure Among Affordable Housing Residents in Minnesota, 2014-2015. Prev Chronic Dis. 2016;13:E111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hollar TL, Cook N, Quinn D, Phillips T, DeLucca M. Smoke-Free Multi-unit Housing Policies Show Promise in Reducing Secondhand Smoke Exposure Among Racially and Ethnically Diverse, Low-Income Seniors. J Immigr Minor Health. 2016:1–9. [DOI] [PubMed] [Google Scholar]
- 18.Phillips K, Bentley MC, Howard DA, Alvan G. Assessment of environmental tobacco smoke and respirable suspended particle exposures for nonsmokers in Prague using personal monitoring. Int Arch Occup Environ Health. 1998;71(6):379–390. [DOI] [PubMed] [Google Scholar]
- 19.Russo ET, Hulse TE, Adamkiewicz G, et al. Comparison of indoor air quality in smoke-permitted and smoke-free multiunit housing: findings from the Boston Housing Authority. Nicotine Tob Res. 2015;17(3):316–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Klassen AC, Lee NL, Pankiewicz A, et al. Secondhand Smoke Exposure and Smoke-free Policy in Philadelphia Public Housing. Tob Regul Sci. 2017;3(2):192–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.New York City Housing Authority (NYCHA). Facts About NYCHA. [http://www1.nyc.gov/assets/nycha/downloads/pdf/factsheet.pdf].
- 22.New York City Housing Authority (NYCHA). Facts About Section 8. [https://www1.nyc.gov/site/nycha/section-8/about-section-8.page].
- 23.Cardozo RA, Feinberg A, Tovar A, et al. A protocol for measuring the impact of a smoke-free housing policy on indoor tobacco smoke exposure. BMC Public Health. 2019;19(1):666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wilson KM, Klein JD, Blumkin AK, Gottlieb M, Winickoff JP. Tobacco-smoke exposure in children who live in multiunit housing. Pediatrics. 2011;127(1):85–92. [DOI] [PubMed] [Google Scholar]
- 25.Levy DE, Adams IF, Adamkiewicz G. Delivering on the Promise of Smoke-Free Public Housing. American journal of public health. 2017;107(3):380–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Palmes ED, Burton RM Jr., Ravishankar K, Solomon JJ. A simple mathematical model for diffusional sampler operation. Am Ind Hyg Assoc J. 1986;47(7):418–420. [DOI] [PubMed] [Google Scholar]
- 27.Jiao W, Hagler G, Williams R, et al. Community Air Sensor Network (CAIRSENSE) project: evaluation of low-cost sensor performance in a suburban environment in the southeastern United States. Atmospheric Measurement Techniques. 2016;9(11):5281–5292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Maciejczyk P, Chen LC. Effects of subchronic exposures to concentrated ambient particles (CAPs) in mice. VIII. Source-related daily variations in in vitro responses to CAPs. Inhal Toxicol. 2005;17(4-5):243–253. [DOI] [PubMed] [Google Scholar]
- 29.Environmental Protection Agency (US). National Ambient Air Quality Standards for Particulate Matter. Federal Resigster (US): Rules and Regulations. 2013;78(10): 3086–3287; https://www3.epa.gov/ttnamti1/. [Google Scholar]
- 30.Fang SC, Chen S, Trachtenberg F, Rokicki S, Adamkiewicz G, Levy DE. Validity of Self-Reported Tobacco Smoke Exposure among Non-Smoking Adult Public Housing Residents. PLoS One. 2016;11(5):e0155024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rokicki S, Adamkiewicz G, Fang SC, Rigotti NA, Winickoff JP, Levy DE. Assessment of Residents' Attitudes and Satisfaction Before and After Implementation of a Smoke-Free Policy in Boston Multiunit Housing. Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco. 2016;18(5):1282–1289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Anthony J, Goldman R, Rees VW, et al. Qualitative Assessment of Smoke-Free Policy Implementation in Low-Income Housing: Enhancing Resident Compliance. Am J Health Promot. 2019;33(1):107–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jiang N, Thorpe L, Kaplan S, Shelley D. Perceptions about the Federally Mandated Smoke-Free Housing Policy among Residents Living in Public Housing in New York City. Int J Environ Res Public Health. 2018;15(10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Twyman L, Bonevski B, Paul C, Bryant J. Perceived barriers to smoking cessation in selected vulnerable groups: a systematic review of the qualitative and quantitative literature. BMJ Open. 2014;4(12):e006414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Murray RL, Bauld L, Hackshaw LE, McNeill A. Improving access to smoking cessation services for disadvantaged groups: a systematic review. J Public Health (Oxf). 2009;31(2):258–277. [DOI] [PubMed] [Google Scholar]
- 36.U.S. Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. [Google Scholar]
- 37.U.S. Department of Health and Human Services. The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2006. [Google Scholar]
- 38.H M, Besser A. AirBeam Technical Specifications, Operation & Performance. Taking space 2014; http://www.takingspace.org/airbeam-technical-specifications-operation-performance/. [Google Scholar]