Abstract
Objective:
To examine racial/ethnic disparities in 30-day all-cause readmission after stroke.
Methods:
Thirty-day all-cause readmission was compared by race/ethnicity among Medicare fee-for-service beneficiaries discharged for ischemic stroke from hospitals in the Florida Stroke Registry from 2010-2013. We fit a Cox proportional hazards model that censored for death and adjusted for age, sex, length of stay, discharge home, and comorbidities to assess racial/ethnic differences in readmission.
Results:
Among 16,952 stroke patients (54% women, 75% white, 8% black, 15% Hispanic), 30-day all-cause readmission was 15% (17.2% for blacks, 16.7% for Hispanics, 14.4% for whites, and 14.7% for others; p=0.003). There was a median of 11 days between discharge and first readmission. In adjusted analyses, there was no significant difference in readmission for blacks (hazard ratio 1.15, 95% confidence interval 0.99-1.33), Hispanics (1.00, 0.90-1.13), and those of other race/ethnicity (0.91, 0.71-1.16) compared with whites. Nearly 1 in 4 readmissions were attributable to acute cerebrovascular events: 16.6% ischemic stroke or transient ischemic attack, 1.5% hemorrhagic stroke, and 5.2% cerebral artery interventions. Interventions were more common among whites and those of other race than blacks and Hispanics (p=0.029). Readmission due to pneumonia or urinary tract infection was 8.2%.
Conclusions:
Readmissions attributable to acute cerebrovascular events were common and generally occurred within two weeks of hospital discharge. Racial/ethnic disparities were present in readmissions for arterial interventions. Our results underscore the importance of post-discharge transitional care and the need for better secondary prevention strategies after ischemic stroke, particularly among minority populations.
Keywords: Race-ethnicity, disparities, rehospitalization, stroke
INTRODUCTION
Stroke is a leading cause of morbidity and long-term disability in the US, and a greater burden of stroke and stroke risk factors is seen in minority groups, including blacks and Hispanics (1,2). Recent evidence suggests disparities in acute stroke care (3-5), which could contribute to disparities in outcomes. Elucidating and eliminating racial/ethnic disparities in stroke care and outcomes remain public health priorities. Early hospital readmission after stroke is an important outcome that reflects the quality and efficiency of hospital-level care (6). Readmission rates are high at 30 days (17%), with major causes being infection, coronary artery disease, and recurrent stroke (7). Whether racial/ethnic disparities exist in 30-day readmission after stroke is not well-understood. A better understanding of differences in the timing, rates, and causes of readmission after stroke between racial/ethnic groups is needed to inform clinical approaches, improve transition of care, and reduce potentially preventable readmissions (6). The primary goal of this study is to identify the rate of all-cause 30-day readmission after stroke and potential racial/ethnic differences among fee-for-service Medicare beneficiaries in the Florida Stroke Registry. In addition, the secondary goal is to describe the reasons for 30-day readmissions.
METHODS
Standard Protocol Approvals, Registrations, Patient Consents
Medicare data were obtained under a data use agreement with the Centers for Medicare & Medicaid Services, and the study was approved by the institutional review boards of University of Miami and Yale University.
Florida Stroke Registry
The Florida Stroke Registry is a voluntary stroke registry of hospitals in Florida participating in the ongoing American Heart Association Get With The Guidelines-Stroke (GWTG-S) data collection system. The registry grew out of the Florida-Puerto Rico Collaboration to Reduce Stroke Disparities (CReSD), which has been described previously (3). CReSD adds several questions to the GWTG-S data collection, including self-reported ethnicity, language, and education. As of March 2015, the registry included 65 hospitals in Florida.
Study Population
The population included fee-for-service Medicare beneficiaries aged ≥65 years who were discharged from a Florida Stroke Registry hospital in 2010-2013 with a principal diagnosis of ischemic stroke (International Classification of Diseases, 9th revision, Clinical Modification codes 433, 434, or 436). Individual admissions in CReSD, from which the Florida Stroke Registry originated, were matched to Medicare claims by identifying unique identifier combinations, including hospital identification number, admission and discharge dates, date of birth, and sex. This matching process is depicted in Figure 1. We identified 33,888 fee-for-service Medicare ischemic stroke cases potentially eligible for matching and matched 21,630 (64%) of the Medicare ischemic stroke cases to registry cases. The match process and achieved rate is comparable to that achieved for national GWTG-S (8).
Figure 1.
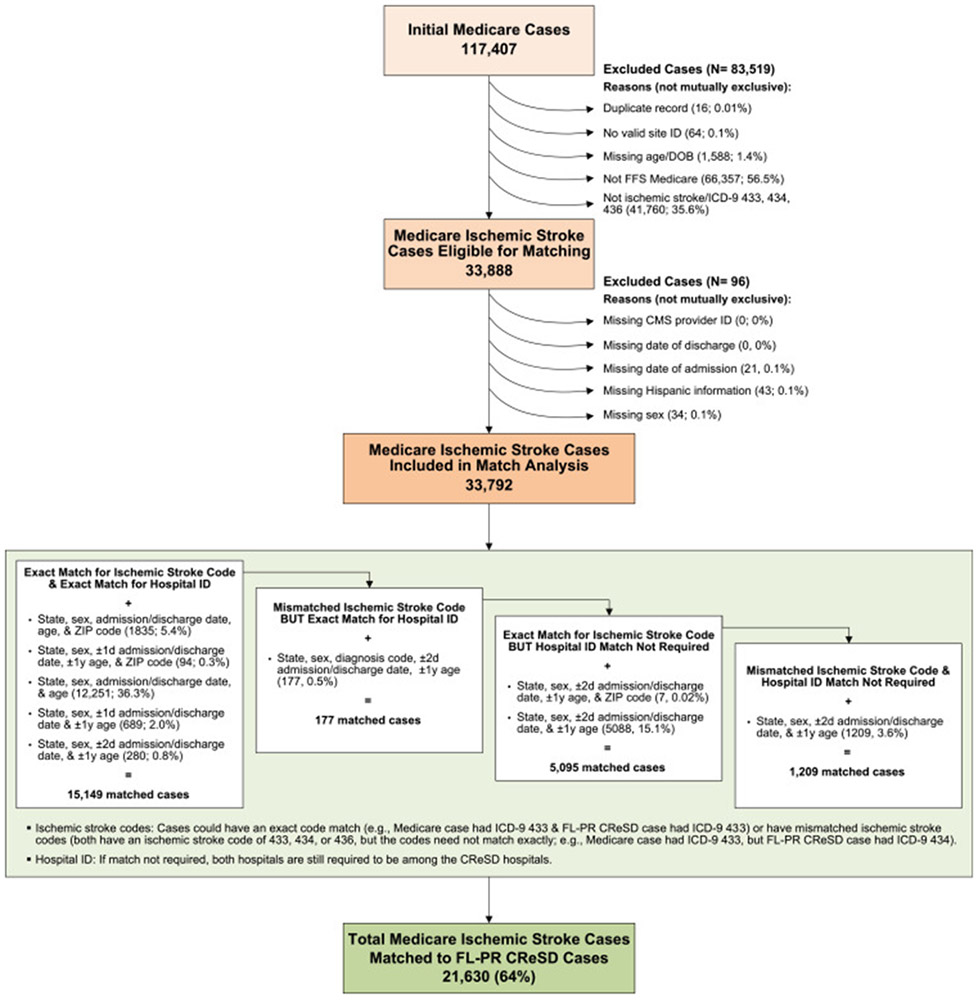
Match of Medicare data with CReSD data.
Variables
The primary outcome was 30-day all-cause readmission to an acute-care hospital from the date of discharge in the Medicare database. The cause of readmission was based on ICD-9 codes. Additional data included age, sex, length of stay, discharge destination, and clinical variables (e.g., hypertension, diabetes) derived from the index admission secondary diagnoses and diagnosis and procedure codes from the 12-month pre-index Inpatient claims. Race/ethnicity was defined based on self-report as recorded in the CReSD-enhanced GWTG-S database and categorized as Hispanic, non-Hispanic white, and non-Hispanic black.
The data are privately owned by CMS and GWTG, and the authors are not authorized to make them publicly available.
Statistical Analysis
We compared overall rates and causes of readmission by race/ethnicity and constructed a Cox proportional hazards model with death as a censoring event to evaluate the relationship between 30-day all-cause readmission and race/ethnicity, adjusting for age, sex, length of stay, discharge to home, and the medical history/comorbidity variables in Table 1. A sensitivity analysis additionally adjusted for stroke severity among patients with an available National Institutes of Health Stroke Scale (NIHSS) score in the Florida Stroke Registry/GWTG-S database. Analyses were conducted using SAS v9.4 (SAS Institute, Cary, NC), and statistical tests were two-sided with alpha=0.05.
Table 1.
Patient Characteristics and Outcomes*
| White (n=12666) |
Black (n=1428) |
Hispanic (n=2562) |
Other (n=296) |
|
|---|---|---|---|---|
| Demographic characteristics | ||||
| Age, mean (SD), y | 79.5 (8.1) | 76.0 (7.8) | 79.1 (7.9) | 76.2 (7.7) |
| Female, n (%) | 6787 (53.6) | 802 (56.2) | 1434 (56.0) | 135 (45.6) |
| Medical history/co-morbid conditions, n (%) | ||||
| Congestive heart failure | 1303 (10.3) | 196 (13.7) | 354 (13.8) | 22 (7.4) |
| Myocardial infarction | 315 (2.5) | 36 (2.5) | 83 (3.2) | <11 (<3.7) |
| Unstable angina | 157 (1.2) | <11 (<0.8) | 31 (1.2) | <11 (<3.7) |
| Chronic atherosclerosis | 4510 (35.6) | 385 (27.0) | 994 (38.8) | 98 (33.1) |
| Respiratory failure | 357 (2.8) | 41 (2.9) | 133 (5.2) | <11 (<3.7) |
| Hypertension | 10028 (79.2) | 1164 (81.5) | 2067 (80.7) | 231 (78.0) |
| Cerebrovascular disease | 1478 (11.7) | 199 (13.9) | 322 (12.6) | 37 (12.5) |
| Renal failure | 1265 (10.0) | 238 (16.7) | 330 (12.9) | 24 (8.1) |
| COPD | 1969 (15.5) | 129 (9.0) | 435 (17.0) | 27 (9.1) |
| Pneumonia | 931 (7.4) | 114 (8.0) | 245 (9.6) | 14 (4.7) |
| Protein-calorie malnutrition | 513 (4.1) | 79 (5.5) | 105 (4.1) | 13 (4.4) |
| Dementia | 1556 (12.3) | 224 (15.7) | 475 (18.5) | 31 (10.5) |
| Functional disability | 648 (5.1) | 134 (9.4) | 184 (7.2) | 14 (4.7) |
| Peripheral vascular disease | 840 (6.6) | 90 (6.3) | 182 (7.1) | 16 (5.4) |
| Cancer | 877 (6.9) | 100 (7.0) | 193 (7.5) | <11 (<3.7) |
| Trauma | 1152 (9.1) | 72 (5.0) | 206 (8.0) | 21 (7.1) |
| Psychiatric disorder | 378 (3.0) | 50 (3.5) | 138 (5.4) | <11 (<3.7) |
| Liver disease | 53 (0.4) | 11 (0.8) | 19 (0.7) | <11 (<3.7) |
| Depression | 1032 (8.1) | 56 (3.9) | 217 (8.5) | 14 (4.7) |
| Diabetes | 3742 (29.5) | 703 (49.2) | 1059 (41.3) | 135 (45.6) |
| Hospital stay, mean (SD) | ||||
| CMS payment, $ | 7871 (7710) | 9837 (11350) | 9282 (8998) | 8284 (6697) |
| Length of stay, d | 4.4 (4.0) | 5.8 (5.7) | 5.1 (4.3) | 4.7 (5.0) |
| Discharge disposition, % (95% CI) | ||||
| Home without home care | 35.0 (34.1-35.8) | 24.2 (22.0-26.5) | 29.2 (27.4-31.0) | 37.5 (32.0-43.3) |
| Home with home care | 14.0 (13.4-14.6) | 15.4 (13.6-17.4) | 16.2 (14.8-17.6) | 17.6 (13.4-22.4) |
| ICF/SNF | 23.8 (23.1-24.6) | 30.0 (27.7-32.5) | 22.6 (21.0-24.2) | 23.3 (18.6-28.6) |
| Outcome, % (95% CI) | ||||
| 30-day all-cause readmission | 14.4 (13.8-15.1) | 17.2 (15.2-19.3) | 16.7 (15.1-18.2) | 14.7 (10.5-18.9) |
CI, confidence interval; CMS, Centers for Medicare and Medicaid Services; COPD, chronic obstructive pulmonary disease; ICF, intermediate care facility; SD, standard deviation; SNF, skilled nursing facility.
The Centers for Medicare and Medicaid Services cell suppression policy prohibits the direct reporting of values between 1 and 10. In accordance with our data use agreement, we coarsened these data and report as <11 in the table.
RESULTS
Among 16,952 unique ischemic stroke patients in Florida (54% women, 75% identified as white, 8% black, 15% Hispanic), the 30-day all-cause readmission was 15%, and the median time between discharge and first readmission was 11 days.
All-cause readmission rates were 17.2% for blacks, 16.7% for Hispanics, 14.4% for whites, and 14.7% for others (unadjusted p=0.003; Table 1). After risk-adjustment, there was no significant difference in 30-day readmission for blacks (hazard ratio [HR]=1.15, 95% confidence interval [CI]=0.99-1.33), Hispanics (1.00, 0.89-1.13), and other race/ethnicity (0.91, 0.71-1.16), compared with whites. Results remained consistent with further adjustment for stroke severity among the 58% for whom data were available (blacks: HR=1.19, 95% CI=0.99-1.44; Hispanics: 1.02, 0.87-1.20; other race/ethnicity: 1.03, 0.72-1.46, vs whites). There were no racial/ethnic differences in the number of days between discharge and first readmission.
Nearly one-fourth of readmissions were attributable to an acute cerebrovascular event: 16.6% ischemic stroke or transient ischemic attack, 1.5% hemorrhagic stroke, and 5.2% cerebral artery intervention (carotid endarterectomy, stenting, or endovascular procedure; Table 2). Readmission due to pneumonia or urinary tract infection, conditions often considered complications or preventable readmissions, was 8.2% overall. Carotid and endovascular interventions were more common among whites and those of other race/ethnicity than among blacks and Hispanics (p=0.029; Table 2).
Table 2.
Readmission Within 30 Days*
| White | Black | Hispanic | Other | |
|---|---|---|---|---|
| Number readmitted within 30 days | 1621 | 220 | 372 | 40 |
| Time to 1st readmission, median (IQR), d | 11 (5-19) | 10 (4-18) | 11 (5-19) | 8.5 (2.5-18.5) |
| Reason for readmission, n (%) | ||||
| Ischemic stroke, hemorrhagic stroke, or TIA | 299 (18.4) | 30 (13.6) | 68 (18.3) | 11 (27.5) |
| Any cerebral artery intervention† | 97 (6.0) | <11 (<5.0) | 14 (3.8) | <11 (<27.5) |
| UTI or pneumonia | 132 (8.1) | 24 (10.9) | 31 (8.3) | <11 (<27.5) |
IQR, interquartile range; TIA, transient ischemic attack; UTI, urinary tract infection.
The Centers for Medicare and Medicaid Services cell suppression policy prohibits the direct reporting of values between 1 and 10. In accordance with our data use agreement, we coarsened these data and report <11 in the table.
Defined as carotid endarterectomy, carotid artery stenting, or endovascular procedure.
DISCUSSION
In the Florida Stroke Registry, post-stroke 30-day readmissions generally occurred within two weeks post-discharge, and almost one-fourth were due to an acute cerebrovascular event. All-cause readmission did not vary significantly by race/ethnicity after multivariable adjustment, but blacks and Hispanics were less likely to be readmitted for cerebral artery interventions. The findings reinforce the continued need to critically evaluate healthcare approaches to transitions of care after stroke and identify opportunities to eliminate disparities in acute stroke care.
A nationwide sample of Medicare patients treated at GWTG-S hospitals reported that the rehospitalization rate within the first year after stroke was higher among blacks and Hispanics as compared with whites for all-cause rehospitalizations and rehospitalizations due to stroke, cardiovascular disease, and myocardial infarction (9). A more recent analysis of Medicare beneficiaries with ischemic stroke in the nationwide GWTG-S registry showed an overall adjusted mean 30-day readmission rate of 13.1%, which was slightly lower than that observed in the current study (10). The latter study reported significant regional variation in readmission, ranging from 10.1% to 20.8%, and their national map indicated that Florida was on the higher end of that range, consistent with our findings. The authors also reported that regions with a higher percentage of black patients had higher readmission, again consistent with our results. A study of national trends in carotid endarterectomy and carotid stenting from 1999-2014 reported higher rates of carotid revascularization procedures in the Medicare population for whites compared with blacks and patients of other race/ethnicity, but the study did not report results for Hispanic patients or identify determinants of these patterns (11).
Our study has several limitations. The study was restricted to fee-for-service Medicare patients in the Florida Stroke Registry, and findings may not be representative of all stroke patients. We lacked data on stroke severity for the entire study population; however, the unadjusted racial/ethnic trends were similar among those with and without NIHSS scores. Administrative CMS data do not include information on psychosocial factors that may contribute to potential disparities in care. Because our study population includes elderly fee-for-service beneficiaries who have equal access to health care in the United States, health insurance type, which was associated with post-stroke care in prior studies, is unlikely to be an issue in our study (12, 13). It is recognized that some of the endarterectomies may have been planned elected surgeries, but we are unable to distinguish those in the CMS database. Administrative Medicare data do not include clinical information on the degree of carotid stenosis or the decision-making process to perform carotid procedures (14). Lastly, Hispanic ethnicity was defined based on the CReSD/GWTG-S category term, with the understanding that Latinos and Hispanics represent a heterogeneous population. Because this study was conducted in Florida, the Hispanic participants were primarily of Cuban, Caribbean, and Central American descent.
The frequency of readmissions within two weeks after hospital discharge underscores the need for improved secondary prevention strategies early after ischemic stroke. Racial/ethnic disparities in rehospitalization after stroke can have multiple interacting causes, including differences in stroke pathologies, pre-stroke risk factor profiles, acute care, discharge recommendations, rehabilitation, and medical follow-up. Effective transition of care after hospitalization may reduce preventable readmissions, especially among minority populations who may be particularly disadvantaged in receiving post-hospital interventions.
Post-discharge stroke care is fragmented and often inadequate. To limit early hospital readmissions, previous studies have suggested that careful discharge planning and effective transitional care may be particularly important for stroke survivors with higher NIHSS scores, coronary artery disease, renal disease, respiratory conditions, and diabetes (7). Stroke survivors may require enhanced transitional care, including discharge navigators, frequent follow-up with medical providers (e.g., community caregivers), monitored medication adherence, and lifestyle modification therapy. We have previously shown racial/ethnic disparities in acute stroke care (3), which can impact both in-hospital and long-term outcomes. Future research is needed to examine whether observed disparities in quality of care among Medicare stroke patients explain observed variability in hospital readmissions, and to determine whether racial/ethnic disparities in hospital-to-home transition of stroke care impact hospital readmission rates.
Acknowledgments
Funding: National Institute of Neurological Disorders and Stroke grant U54-NS081763 and National Institute on Minority Health and Health Disparities grant 1R01MD012467
Footnotes
Disclosures: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Hannah Gardener, Department of Neurology, University of Miami Miller School of Medicine.
Erica C. Leifheit, Department of Epidemiology, Yale School of Public Health.
Judith H Lichtman, Department of Epidemiology, Yale School of Public Health.
Kefeng Wang, Department of Neurology, University of Miami Miller School of Medicine.
Yun Wang, Department of Epidemiology, Yale School of Public Health.
Carolina M. Gutierrez, Department of Neurology, University of Miami Miller School of Medicine.
Maria A. Ciliberti-Vargas, Department of Neurology, University of Miami Miller School of Medicine.
Chuanhui Dong, Department of Neurology, University of Miami Miller School of Medicine.
Mary Robichaux, Department of Neurology, University of Miami Miller School of Medicine.
Jose G. Romano, Department of Neurology, University of Miami Miller School of Medicine.
Ralph L. Sacco, Department of Neurology, University of Miami Miller School of Medicine.
Tatjana Rundek, Department of Neurology, University of Miami Miller School of Medicine.
REFERENCES
- 1.Sacco RL, Boden-Albala B, Gan R, Chen X, Kargman DE, Shea S, et al. Stroke incidence among white, black, and Hispanic residents of an urban community: the Northern Manhattan Stroke Study. Am J Epidemiol. 1998;147:259–68. [DOI] [PubMed] [Google Scholar]
- 2.White H, Boden-Albala B, Wang C, Elkind MS, Rundek T, Wright CB, et al. Ischemic stroke subtype incidence among whites, blacks, and Hispanics: the Northern Manhattan Study. Circulation. 2005;111:1327–31. [DOI] [PubMed] [Google Scholar]
- 3.Sacco RL, Gardener H, Wang K, Dong C, Ciliberti-Vargas MA, Gutierrez CM, et al. Racial-Ethnic Disparities in Acute Stroke Care in the Florida-Puerto Rico Collaboration to Reduce Stroke Disparities Study. J Am Heart Assoc. 2017;6 pii: e004073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cruz-Flores S, Rabinstein A, Biller J, Elkind MS, Griffith P, Gorelick PB, et al. Racial-ethnic disparities in stroke care: the American experience: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42:2091–116. [DOI] [PubMed] [Google Scholar]
- 5.Oluwole SA, Wang K, Dong C, Ciliberti-Vargas MA, Gutierrez CM, Yi L, et al. Disparities and Trends in Door-to-Needle Time: The FL-PR CReSD Study (Florida-Puerto Rico Collaboration to Reduce Stroke Disparities). Stroke. 2017;48:2192–2197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lichtman JH, Leifheit-Limson EC, Jones SB, Wang Y, Goldstein LB. Preventable readmissions within 30 days of ischemic stroke among Medicare beneficiaries. Stroke. 2013;44:3429–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhong W, Geng N, Wang P, Li Z, Cao L. Prevalence, causes and risk factors of hospital readmissions after acute stroke and transient ischemic attack: a systematic review and meta-analysis. Neurol Sci. 2016;37:1195–202. [DOI] [PubMed] [Google Scholar]
- 8.Fonarow GC, Pan W, Saver JL, Smith EE, Reeves MJ, Broderick JP, et al. Comparison of 30-day mortality models for profiling hospital performance in acute ischemic stroke with vs without adjustment for stroke severity. JAMA. 2012;308:257–64. [DOI] [PubMed] [Google Scholar]
- 9.Qian F, Fonarow GC, Smith EE, Xian Y, Pan W, Hannan EL, et al. Racial and ethnic differences in outcomes in older patients with acute ischemic stroke. Circ Cardiovasc Qual Outcomes. 2013;6:284–92. [DOI] [PubMed] [Google Scholar]
- 10.Thompson MP, Zhao X, Bekelis K, Gottlieb DJ, Fonarow GC, Schulte PJ, et al. Regional Variation in 30-Day Ischemic Stroke Outcomes for Medicare Beneficiaries Treated in Get With The Guidelines-Stroke Hospitals. Circ Cardiovasc Qual Outcomes. 2017;10 pii: e003604. [DOI] [PubMed] [Google Scholar]
- 11.Lichtman JH, Jones MR, Leifheit EC, Sheffet AJ, Howard G, Lai BK, et al. Carotid Endarterectomy and Carotid Artery Stenting in the US Medicare Population, 1999–2014. JAMA. 2017;318:1035–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Skolarus LE, Muerer WJ, Burke JF, Prvu Bettger J, Lisabeth LD. Effect of insurance status on postacute care among working age stroke survivors. Neurology. 2012;78:1590–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lichtman JH, Leifheit-Limson EC, Jones SB, Watanabe E, Bernheim SM, Phipps MS, et al. Predictors of hospital readmission after stroke: a systematic review. Stroke. 2010;41:2525–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Martin KD, Naert L, Goldstein LB, Kasl S, Molinaro AM, Lichtman JH. Comparing the use of diagnostic imaging and receipt of carotid endarterectomy in elderly black and white stroke patients. J Stroke Cebrovas Dis. 2012;21:600–6. [DOI] [PMC free article] [PubMed] [Google Scholar]


