Abstract
Background
The incidence of skin and soft-tissue infections (SSTIs), for which human immunodeficiency virus (HIV) is a significant risk factor, in United States emergency departments (EDs) increased dramatically after 2000 with the emergence of community-associated methicillin-resistant Staphylococcus aureus. Few studies have examined SSTI incidence among HIV-infected and non–HIV-infected patients in the United States after 2010.
Methods
Data were obtained for patient encounters at all academic medical center EDs affiliated with the Vizient clinical data warehouse assigned an SSTI-associated code based on the International Classification of Diseases, Ninth Revision, between 1 January 2009 and 31 December 2014. The rate was calculated per 1000 ED encounters by year and stratified by SSTI, HIV infection, or both, and by age group, race, payer type, and region of care. Poisson regression was used to assess temporal change over the study period.
Results
In 2009–2014, a total of 47317 HIV-associated and 820440 SSTI-associated encounters were recorded among 25239781 ED patient encounters. The rate of SSTIs decreased by 8% among all patients and by 14.6%, among those with HIV infection. The SSTI incidence overall decreased from 32.0 to 29.7 per 1000 ED encounters between 2009 and 2014. HIV-infected patients had a significantly higher rate of SSTIs than HIV-uninfected patients (adjusted rate ratio, 1.91; 95% confidence interval, 1.84–1.99).
Conclusions
The decline in SSTI incidence in US EDs between 2009 and 2014 is a remarkable epidemiologic shift from the increase in SSTIs after 2000, and further research is necessary to assess reasons for this decrease.
Keywords: SSTI, HIV, emergency department, incidence
In 2009–2014, 820 440 skin and soft-tissue infection (SSTI)–associated encounters were recorded among 25239781 encounters in 86 US emergency departments (EDs); the SSTI rate decreased by 8%, from 32.0 to 29.7 per 1000 ED patient encounters.
The incidence of skin and soft-tissue infections (SSTIs) in the United States increased sharply in the hospital setting and among outpatients after 2000 [1–4]. SSTIs include a range of conditions from uncomplicated folliculitis, skin abscess, or cellulitis to severe, life-threatening infections, such as necrotizing fasciitis. In the period 1993–2005, US emergency department (ED) visits related to SSTIs increased dramatically [5], particularly in urban EDs [6]. This increase coincided with, and is often attributed to, a sharp increase in community-associated (CA) methicillin-resistant Staphylococcus aureus (MRSA) infections [7–10]. Compounding this increase, among patients who present with a CA-MRSA SSTI, >30% have a recurrent infection diagnosed within 1 year [11–13]. In 2004 and 2008, MRSA was the most common cause of purulent SSTIs among patients treated at 12 US urban EDs [14].
Data from the National Hospital Ambulatory Medical Care Survey demonstrated that approximately 6.8 million ED visits for SSTIs occurred in the United States in 2007–2009 [15], and that the number of ED visits for SSTIs increased from 3.55 million in 2007 to 4.21 million in 2010 [16]. Although several studies have suggested that the incidence of MRSA infections has decreased in the United States after 2005 [17, 18], and we demonstrated a decreasing overall trend in the rate of SSTIs at the University of Chicago in 2006–2013 [19], few published data are now available about the epidemiology of SSTIs in US EDs after 2010.
Furthermore, although human immunodeficiency virus (HIV) infection is a risk factor for MRSA SSTIs [20, 21], few large studies have examined the recent incidence of SSTIs among persons with HIV infection. In particular, the longitudinal trends on SSTI incidence in ED patients with HIV infection are not known, despite the fact that many HIV-infected patients receive their urgent care in EDs.
We noticed that there was a decline in the number of patients visiting our ED with uncomplicated SSTIs after 2012. We therefore examined temporal trends in SSTI rates among ED patients in 2009–2014 at 86 US academic medical centers. We hypothesized that the incidence of SSTIs overall and among patients with HIV infection decreased significantly.
METHODS
Study Design
Data were obtained from the Vizient Clinical Data Warehouse (formerly University HealthSystems Consortium), which collects clinical and administrative data related to patient encounters at member academic medical centers in the United States. Data were obtained for all ED encounters at 86 academic medical centers between 1 January 2009 and 31 December 2014, and, among them, the cohort of encounters with a diagnosis of SSTI. SSTI encounters were defined as having, in administrative records, at least a single SSTI-associated International Classification of Diseases, Ninth Revision (ICD-9) code (see Supplementary Table 1). An encounter was considered an ED encounter if a subject visited an ED and was not admitted to the hospital. We included only the first ED encounter for an SSTI for each individual subject in a calendar year. The University of Chicago Biological Sciences Division Institutional Review Board approved the study.
Demographic Characteristics
In this retrospective cohort study, variables collected for each patient encounter included age, ethnicity, race, insurance payer type, region of the United States, HIV status (defined as having a primary or secondary diagnosis ICD-9 code of 042), and all other comorbid conditions noted in ICD-9–coded data. Patients were categorized as either pediatric (<18 years of age) or adult (≥18 years of age). Hispanic, African American, white, or other race (a category that included those reported >1 race, those who declined to answer, and unknown) was self-reported by each patient. Payer type was defined as low socioeconomic status (SES) (a category that included Medicaid, charity care, county medical indigent, and self-pay uninsured), commercial (purchased through a for-profit insurance provider), Medicare, or other (a category that included, but was not limited to, workers compensation, auto insurance, federal employee coverage, self-pay cash, unknown, state insurance programs, and criminal justice coverage). A region of care assigned to each patient was defined by medical center location: West, Midwest, Northeast, or South in the United States (Supplementary Figure 1). A patient was considered to have a comorbid condition if he or she had an ICD-9 code for any medical problem other than the SSTI.
Analysis
Incidence densities (hereafter referred to as “rates”) of both HIV infection and SSTIs were calculated by year. The SSTI rates were calculated separately for all encounters and then among those with and those without an HIV ICD-9 code. We first performed individual unadjusted Poisson regression analyses for each year, age group (pediatric or adult), ethnicity/race, payer type, and region of residence. Multivariable Poisson regression models, controlling for covariates, were then used to assess (1) the change in SSTI incidence over time among all patients, (2) the change over time in those with an HIV encounter, (2) the differential rate of SSTIs in those with versus those without HIV infection, and (3) the differential rate of SSTIs in those with versus those without comorbid conditions. All covariates identified as statistically significant at the P ≤ .05 level, using the Wald test statistic, were included in the multivariable regression model (including comorbid conditions, age, race, payer type, and region of residence). Analyses were performed using Stata 14.0 software (StataCorp) [22].
RESULTS
During the study period, from January 2009 through December 2014, data were collected for 25838647 ED patient encounters across 86 academic medical centers. Among all ED patient encounters, 820441 (3.18%) had an ICD-9 code for SSTI as a primary or secondary diagnosis, with a rate of 31.8 SSTI-associated encounters per 1000 ED patient encounters. In the study cohort, 47317 patient encounters (0.18%) had an ICD-9 code for HIV, with a rate of 1.9 HIV-associated encounters per 1000 patient encounters. Nearly half of SSTI encounters involved white patients (49.3%), and about one-third involved African American patients (29.1%). Commercial insurance covered 27.5% of all ED encounters, but only 24.1% of SSTI ED encounters. Among 4966652 pediatric ED encounters, 113222 (2.2%) were for SSTIs. The total number of ED encounters increased in each year. Data on the demographics of patients with ED encounters overall and the number of SSTI ED encounters, as well as the distribution of ED encounters by region of the United States and by year, are shown in Table 1.
Table 1.
Patient Characteristics for Emergency Department (ED) Encounters With or Without an ICD-9 Diagnosis Code for an Skin and Soft-tissue Infection at 86 US EDs, 2009–2014
| Characteristic | ED Patient Encounters, No. (%) | |||
|---|---|---|---|---|
| Total (N = 25838647) | SSTI ICD-9 Code (n = 820441) | No SSTI ICD-9 Code (n = 25018206) | P Value (χ2 Test) | |
| Pediatric age group (<18 y) | 4966652 (19.2) | 113222(13.8) | 4853430 (19.4) | <.001 |
| Female sex | …a | 397106 (48.4) | … | … |
| Race | ||||
| African American | 7556399 (29.2) | 265698 (32.4) | 7290701 (29.1) |
<.001 |
| Hispanic | 3070216 (11.9) | 85426 (10.4) | 2984790 (11.9) | |
| Other | 2486626 (9.6) | 64467 (7.9) | 2422159 (9.7) | |
| White | 12725406 (29.3) | 404850 (49.4) | 12320556 (49.3) | |
| Payer type | ||||
| Commercial | 7084645 (27.5) | 198011(24.1) | 6886634 (27.5) | <.001 |
| Low SES | 12842335 (49.7) | 460258 (56.1) | 12382077 (49.5) | |
| Medicare | 3744652 (14.5) | 105248 (12.8) | 3639404 (14.6) | |
| Other | 2167015 (8.4) | 56924 (6.9) | 2110091 (8.4) | |
| US region | ||||
| Midwest | 7170812 (27.8) | 232229 (28.3) | 6938583 (27.7) | <.001 |
| Northeast | 9540835 (36.9) | 297807 (36.3) | 9243028 (37.0) | |
| South | 5084045 (19.7) | 169937 (20.7) | 4914108 (19.6) | |
| West | 4042955 (15.7) | 120468 (14.7) | 3922487 (15.7) | |
| Year | ||||
| 2009 | 4057552 (15.7) | 131336 (16.0) | 3926216 (15.7) | <.001 |
| 2010 | 4072286 (15.8) | 132823 (16.2) | 3939463 (15.8) | |
| 2011 | 4167171 (16.1) | 135805 (16.6) | 4031366 (16.1) | |
| 2012 | 4471092 (17.3) | 142960 (17.4) | 4328132 (17.3) | |
| 2013 | 4491725 (17.4) | 141326 (17.2) | 4350399 (17.4) | |
| 2014 | 4578821 (17.72) | 136191 (16.6) | 4442630 (17.8) | |
Abbreviations: ED, emergency department; ICD-9, International Classification of Diseases, Ninth Revision; SES, socioeconomic status; SSTI, skin and soft-tissue infection.
aSex was only available for those with an SSTI-associated code.
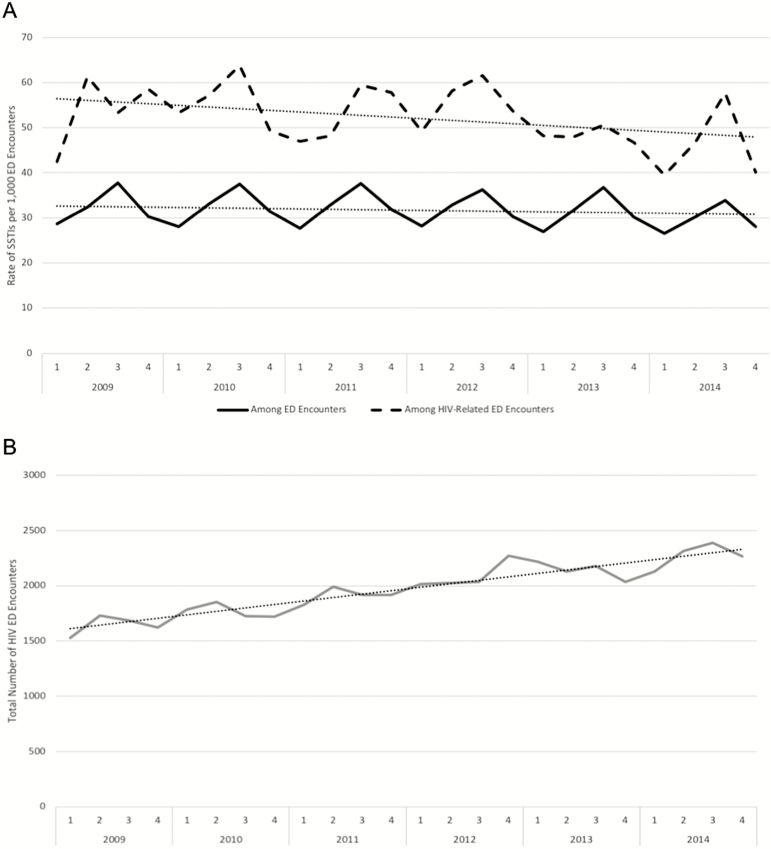
The overall rate of SSTIs decreased significantly, from 32.8 per 1000 encounters in 2009 to 29.7 per 1000 ED encounters in 2014 (rate ratio [RR], 0.98; 95% confidence interval [CI], .98–.98) (Figure 1). The rate decreased significantly in adults (RR, 0.98; 95% CI, .98–.98) while increasing slightly in children (1.005; 1.001–1.008). When stratified by race, the SSTI rates decreased in African American (RR, 0.97; 95% CI, .97–.97), Hispanic (0.99; .98–.99), and white (0.99; .99–.99) patients. Patients whose payer was commercial (RR, .99; 95% CI, .99–1.00), low SES (0.98; .98–.98), or Medicare (0.99; .98–.99) had significantly reduced SSTI rates, whereas those with another payer type had a significantly increased rate (1.01; 1.01–1.02). It was also observed that the SSTI rates decreased across all regions of the United States (Table 2).
Figure 1.
A, Rates of skin and soft-tissue infections (SSTIs), per 1000 emergency department (ED) patient encounters, from 2009 to 2014, for all ED encounters and human immunodeficiency virus (HIV)–associated encounters. B, Total numbers of HIV-associated ED encounters from 2009 to 2014. Dotted lines in each graph represent the trend line. Numbers above each year represent the quarter in which data were collected.
Table 2.
Annual Change in Skin and Soft-tissue Infection (SSTI) Incidence Stratified by Demographic Groups and Change in Number of SSTI Encounters Adjusted by Demographic Characteristics in Univariate and Multivariate Poisson Regression Models
| Characteristic | RR (95% CI) | ||
|---|---|---|---|
| Stratifieda | Univariate Model | Multivariate Model | |
| Year | 0.98 (.98–.99)b | 0.98 (.98–.99)b | 0.98 (.98–.98)b |
| Age group | |||
| Adult (≥18 y) | 0.98 (.98–.98)b | Reference | Reference |
| Pediatric (<18 y) | 1.005 (1.001–1.008)b | 0.67 (.67–.68)b | 0.65 (.64–.65)b |
| Race | |||
| African American | 0.97 (.97–.97)b | Reference | Reference |
| Hispanic | 0.99 (.98–.99)b | 0.79 (.79–.80)b | 0.79 (.79–.80)b |
| Other | 1.00 (1.00–1.00) | 0.74 (.73–.74)b | 0.78 (.77–.79)b |
| White | 0.99 (.99–.99)c | 0.90 (.90–.91)b | 0.97 (.96–.97)b |
| Payer | |||
| Commercial | 0.99 (.99–1.00)b | 0.78 (.78–.78)b | 0.76 (.76–.77)b |
| Low SES | 0.98 (.98–.98)b | Reference | Reference |
| Medicare | 0.99 (.98–.99)b | 0.78 (.78–.79)b | 0.70 (.69–.70)b |
| Other | 1.01 (1.01–1.02)b | 0.73 (.73–.74)b | 0.69 (.69–.70)b |
| US region | |||
| Midwest | 0.98 (.98–.98)b | 1.09 (1.08–1.09)b | 1.04 (1.02–1.03)b |
| Northeast | 0.99 (.99–.99)b | 1.05 (1.04–1.05)b | 1.06 (1.05–1.06)b |
| South | 0.998 (.98–.99)b | 1.12 (1.11–1.13)b | 1.08 (1.07–1.09)b |
| West | 0.98 (.98–.98)b | Reference | Reference |
Abbreviations: CI, confidence interval; RR, rate ratio; SES, socioeconomic status.
aEach RR represents an individual model.
b P < .005.
c P < .05.
SSTI rates differed between patients with and those without HIV infection, with 32.5 SSTI-associated encounters per 1000 ED encounters in HIV-uninfected patients, compared with 51.9 SSTI-associated encounters per 1000 ED encounters in HIV-infected patients. This pattern was observed across the study period, with SSTI rates among those with HIV infection consistently higher than among all ED encounters (Figure 1). Furthermore, among all ED encounters there was a consistent and strong seasonal peak in the second quarter of each year.
In separate sensitivity analyses, we examined SSTI rates in those with versus those without additional comorbid conditions among (1) the entire sample, (2) adults only, and (3) pediatric patients only. We observed a significant decrease in the SSTI rate in both those with (RR, 0.99; 95% CI, .99–.995) and those without (0.99; .98–.99) other comorbid conditions. In adults, we continued to observe a significant decrease in those with (RR, 0.99; 95% .99–.996) and those without (0.98; .98–.98) comorbid conditions. In pediatric patients, however, we observed a significant decrease in those with comorbid conditions (RR, 0.98; 95% CI, .97–.99) and a significant increase in those without any comorbid conditions (1.01; 1.004–1.01).
Among HIV-associated ED encounters, the majority of patients (Table 3) did not have an SSTI-associated encounter (94.8%), were adults (98.7%), were African American (56.2%), and had a payer type of low SES (55.3%). The greatest proportion received care in the South (34.0%). The overall rate of SSTIs in HIV-infected patients, per 1000 ED patient encounters, decreased significantly, from 54.2 in 2009 to 46.3 in 2014 (RR, 0.97; 95% CI, .94–.99). Examining only patients with an HIV-associated encounter, the incidence of SSTIs decreased significantly in adults (RR, 0.96; 95% CI, .94–.99), African Americans (0.94; .91–.97), those with low SES payer type (0.97;.94–1.00), and those who received care in the West (0.94; .89–1.00) or Midwest (0.95; .91–1.00) regions.
Table 3.
Characteristics of Patients With Emergency Department Encounters, Comparing Human Immunodeficiency Virus (HIV)-associated and Non–HIV-associated Encounters, at 86 US EDs, 2009–2014a
| Characteristic | ED Patient Encounters, No. (%) | P Value (χ2 Test) | ||
|---|---|---|---|---|
| Total (N = 25 239 781) | HIV ICD-9 Code (n = 47317) | No HIV ICD-9 Code (n = 25 192 464) | ||
| SSTI | 820440 (3.3) | 2458 (5.2) | 817982 (3.3) | <.001 |
| Pediatric age group (<18 y) | 4749933 (18.8) | 618 (1.3) | 4749315 (18.9) | <.001 |
| Race | ||||
| African American | 7362029 (29.2) | 26595 (56.2) | 7335434 (29.1) | <.001 |
| Hispanic | 3007203 (11.9) | 3725 (7.9) | 3003478 (11.9) | |
| Other | 2431409 (9.6) | 2425 (5.1) | 2428984 (9.6) | |
| White | 12439140 (49.3) | 14572 (30.8) | 12424568 (49.3) | |
| Payer type | ||||
| Commercial | 6922892 (27.4) | 5125 (10.8) | 6917767 (27.5) | <.001 |
| Low SES | 12493731 (49.5) | 26186 (55.3) | 12467545 (49.5) | |
| Medicare | 3698344 (14.7) | 12636 (26.7) | 3685708 (14.6) | |
| Other | 2124814 (8.4) | 3370 (7.1) | 2121444 (8.4) | |
| Region | ||||
| Midwest | 7109670 (28.2) | 14953 (31.6) | 7094717 (28.2) | <.001 |
| Northeast | 9475927 (37.5) | 8750 (18.5) | 9467187 (37.5) | |
| South | 4680267 (18.5) | 16094 (34.0) | 4664173 (18.5) | |
| West | 3973907 (15.7) | 7520 (15.9) | 3966387 (15.7) | |
| Year | ||||
| 2009 | 3907331 (15.5) | 6567 (13.9) | 3900764 (15.5) | <.001 |
| 2010 | 3899709 (15.5) | 7087 (15.0) | 3892622 (15.5) | |
| 2011 | 4059627 (16.1) | 7658 (16.2) | 4051969 (16.1) | |
| 2012 | 4344140 (17.2) | 8345 (17.6) | 4335795 (17.2) | |
| 2013 | 4473754 (17.7) | 8559 (18.1) | 4465195 (17.7) | |
| 2014 | 4555220 (18.1) | 9101 (19.2) | 4546119 (18.1) | |
Abbreviations: ED, emergency department; HIV, human immunodeficiency virus; ICD-9, International Classification of Diseases, Ninth Revision; SES, socioeconomic status; SSTI, skin and soft-tissue infection.
aHIV-associated encounters were defined as those with a primary or secondary HIV-associated ICD-9 code.
The rate of SSTI ED encounters in patients with HIV infection was significantly higher than in those without HIV infection, not only for adults (RR, 1.51; 95% CI, 1.45–1.57) but also for children (1.56; 1.04–2.35). Compared with patients without HIV infection, the rate in HIV-infected patients was also significantly higher in African Americans (RR, 1.36; 1.28–1.43), Hispanics (1.73; 1.50–2.00), those with race categorized as “other” (2.11; 1.79–2.51), and whites (1.77; 1.66–1.90). Significantly higher SSTI rates among those with HIV infection were also identified in patients with commercial (RR, 1.84; 95% CI, 1.64–2.07), low SES (1.52; 1.44–1.60), Medicare (1.47; 1.34–1.60), or other (2.23; 1.94–2.56) payer types. Patients with HIV infection had higher SSTI rates in all 4 geographic regions of care.
In adjusted Poisson analyses (Supplementary Table 2), accounting for age, race, payer type, and region, we found that the rate of SSTIs in ED patients with HIV infection decreased significantly (adjusted RR, 0.96; 95% CI, .94–.99). Furthermore, we found in adjusted analyses (Table 4) that patients with HIV infection had a significantly higher SSTI rate than other patients (adjusted RR, 1.91; 95% CI, 1.84–1.99).
Table 4.
Multivariate Poisson Regression Analyses for Numbers of Human Immunodeficiency Virus (HIV)-associated and Skin and Soft-tissue Infection-associated Emergency Department (ED) Encounters Among HIV-infected Patients, by Selected Patient Characteristics at 86 US EDs, 2009–2014
| Characteristic | ARR (95% CI) | |
|---|---|---|
| All HIV-Associated ED Encounters (N = 25 239 781) | SSTIs Among HIV-Associated ED Encounters (n = 47 317) |
|
| Year of encounter | 1.02 (1.01–1.02)a | 0.96 (.94–.99)a |
| Age group | ||
| Adult (≥18 y) | Reference | Reference |
| Pediatric (<18 y) | 0.07 (.06–.07)a | 0.68 (.45–1.03) |
| Race | ||
| African American | Reference | Reference |
| Hispanic | 0.37 (.36–.39)a | 0.99 (.84–1.16) |
| Other | 0.39 (.37–.40)a | 1.18 (.99–1.42) |
| White | 0.39 (.38–.40)a | 1.21 (1.10–1.32)a |
| Payer type | ||
| Low SES | Reference | Reference |
| Commercial | 0.78 (.46–.49)a | 0.92 (.81–1.05) |
| Medicare | 1.51 (1.47–1.54)a | 0.74 (.67–.82)a |
| Other | 0.72 (.69–.75)a | 1.05 (.90–1.21) |
| US region | ||
| West | Reference | Reference |
| Midwest | 0.85 (.83–.89)a | 0.93 (.82–1.05) |
| Northeast | 0.48 (.46–.49)a | 0.85 (.74–.98)b |
| South | 1.34 (1.31–1.38)a | 1.01 (.90–1.14) |
Abbreviations: ARR, adjusted rate ratio; CI, confidence interval; ED, emergency department; HIV, human immunodeficiency virus; SES, socioeconomic status; SSTI, skin and soft-tissue infection.
a P < .005.
b P < .05.
DISCUSSION
We studied >25 million ED patient encounters across 86 academic medical centers to assess our research questions. We found that during 2009–2014, the rate of all ED SSTI encounters decreased by 8.0%. HIV-associated ED SSTI encounters also decreased significantly, by 14.6%. This is a major reversal of the great increase in SSTI incidence in the United States in outpatient and inpatient care settings after the year 2000, with the emergence of the USA300 MRSA strain [5–10, 14]. We observed a significant decrease in SSTI rates in the following groups: adult patients with HIV-associated encounters; all adults; African American, Hispanic, and white patients; patients whose payer was commercial, low SES, or Medicare; and patients in all regions of the United States. We also observed significantly higher SSTI rates in HIV-infected patients than in those with non–HIV-associated encounters, adjusting for demographic group, payer type, and region.
Recent research examining temporal trends in the incidence of both MRSA infections and SSTIs has demonstrated a decline in both after approximately 2005 [17, 19, 23]. In the current study, we observed a significant decrease in the rate of SSTIs in many demographic risk groups. Children were the only demographic group in which we observed an increase in SSTI rate, but further analyses demonstrated that this increase occurred only in children without other comorbid conditions. These results suggest that the rising rate in this cohort is most likely to due to community-associated infections, not healthcare-associated infections. We also observed that, compared with non–HIV-associated encounters, HIV-associated encounters had a significantly higher SSTI rate. Past research has demonstrated a high prevalence of SSTIs in men who have sex with men (MSM) caused by multidrug-resistant USA300 [24], and physicians should be aware of CA-MRSA as a potential cause of SSTI in HIV-infected individuals [25].
More generally, SSTIs have been shown to be common in HIV-infected patients [26]. A high rate of SSTI recurrence (71%) has also been found in the primary care setting among HIV-infected patients in San Francisco [27] and HIV-infected patients in Chicago [28]. Although an overall decline in the rate of SSTIs was observed in this sample, we continued to observe a higher rate in those who were HIV-infected. It is possible that there are differing incidence rates of SSTIs in MSM or other HIV transmission risk groups, independent of HIV infection status. Future research is necessary to define the reasons for the observed trends in SSTI incidence in these high-risk groups and the role of recurrent infections in the epidemiology of SSTIs.
Overall in the United States, the rate of new HIV diagnoses has decreased 19% over the past decade, although this rate varies by both demographic and risk groups [29]. Although the rate of new HIV diagnoses has decreased in both men and women, MSM and African American men and women continue to be disproportionately affected by HIV [29]. Furthermore, both Hispanic and African American MSM are among the only demographic and risk groups to have experienced an increase in the incidence of new HIV infections in 2009–2014, with younger Hispanic and African American MSM (those aged 13–24 years) experiencing the steepest increases in the rate of new diagnoses [29].
This study should be viewed in the context of its limitations. We used administrative data and ICD-9 codes to identify both HIV- and SSTI-associated ED patient encounters. Since the study period, the International Classification of Diseases, Tenth Revision (ICD-10), has replaced ICD-9, and future studies must account for changes that will result from coding practices with ICD-10. Our study was performed with data only from academic medical centers, and thus trends that we identified may not be true of all US medical facilities. Although these data have high sensitivity, they have a lower specificity for identifying subjects with an SSTI or HIV infection than do medical records. In addition, though we used a large and robust data set, we are missing data that would be useful in exploring trends in SSTI infections among HIV-infected patients, particularly transmission risk group characteristics.
In our study, we demonstrated an overall decrease in the incidence of SSTIs among all patients at US academic medical centers, a trend that reverses a massive increase in SSTI incidence after 2000. Patients with HIV-associated ED encounters similarly showed a decrease in SSTI incidence. We also observed higher SSTI rates among those who were HIV infected, compared with those who were not, across all demographic groups, payer types, and regions of the United States. The higher incidence of SSTIs in HIV-infected patients represents a substantial burden of disease, and this should be addressed in future, prospective studies on the prevention of SSTIs in this population.
Supplementary Data
Supplementary materials are available at Clinical Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Notes
Financial support. This work was supported by the National Institute of Allergy and Infectious Diseases, National Institutes of Health (grant K23 AI095361 to M. Z. D.)
Potential conflicts of interest. J. R. reports grants from Gilead and GlaxoSmithKline outside the submitted work. M. Z. D. reports grants from GlaxoSmithKline outside the submitted work. All other authors report no potential conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Gutierrez K, Halpern MS, Sarnquist C, Soni S, Arroyo AC, Maldonado Y. Staphylococcal infections in children, California, USA, 1985–2009. Emerg Infect Dis 2013; 19:10–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hersh AL, Chambers HF, Maselli JH, Gonzales R. National trends in ambulatory visits and antibiotic prescribing for skin and soft-tissue infections. Arch Intern Med 2008; 168:1585–91. [DOI] [PubMed] [Google Scholar]
- 3. Klein E, Smith DL, Laxminarayan R. Community-associated methicillin-resistant Staphylococcus aureus in outpatients, United States, 1999–2006. Emerg Infect Dis 2009; 15:1925–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Tracy LA, Furuno JP, Harris AD, Singer M, Langenberg P, Roghmann MC. Staphylococcus aureus infections in US veterans, Maryland, USA, 1999–2008. Emerg Infect Dis 2011; 17:441–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Pallin DJ, Egan DJ, Pelletier AJ, Espinola JA, Hooper DC, Camargo CA Jr. Increased US emergency department visits for skin and soft tissue infections, and changes in antibiotic choices, during the emergence of community-associated methicillin-resistant Staphylococcus aureus. Ann Emerg Med 2008; 51:291–8. [DOI] [PubMed] [Google Scholar]
- 6. Frazee BW, Lynn J, Charlebois ED, Lambert L, Lowery D, Perdreau-Remington F. High prevalence of methicillin-resistant Staphylococcus aureus in emergency department skin and soft tissue infections. Ann Emerg Med 2005; 45:311–20. [DOI] [PubMed] [Google Scholar]
- 7. Kaplan SL, Hulten KG, Gonzalez BE, et al. Three-year surveillance of community-acquired Staphylococcus aureus infections in children. Clin Infect Dis 2005; 40:1785–91. [DOI] [PubMed] [Google Scholar]
- 8. David MZ, Daum RS. Community-associated methicillin-resistant Staphylococcus aureus: epidemiology and clinical consequences of an emerging epidemic. Clin Microbiol Rev 2010; 23:616–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dukic VM, Lauderdale DS, Wilder J, Daum RS, David MZ. Epidemics of community-associated methicillin-resistant Staphylococcus aureus in the United States: a meta-analysis. PLoS One 2013; 8:e52722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. McCaig LF, McDonald LC, Mandal S, Jernigan DB. Staphylococcus aureus-associated skin and soft tissue infections in ambulatory care. Emerg Infect Dis 2006; 12:1715–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fritz SA, Camins BC, Eisenstein KA, et al. Effectiveness of measures to eradicate Staphylococcus aureus carriage in patients with community-associated skin and soft-tissue infections: a randomized trial. Infect Control Hosp Epidemiol 2011; 32:872–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Duong M, Markwell S, Peter J, Barenkamp S. Randomized, controlled trial of antibiotics in the management of community-acquired skin abscesses in the pediatric patient. Ann Emerg Med 2010; 55:401–7. [DOI] [PubMed] [Google Scholar]
- 13. Kaplan SL, Forbes A, Hammerman WA, et al. Randomized trial of “bleach baths” plus routine hygienic measures vs routine hygienic measures alone for prevention of recurrent infections. Clin Infect Dis 2014; 58:679–82. [DOI] [PubMed] [Google Scholar]
- 14. Talan DA, Krishnadasan A, Gorwitz RJ, et al. Comparison of Staphylococcus aureus from skin and soft-tissue infections in US emergency department patients, 2004 and 2008. Clin Infect Dis 2011; 53:144–9. [DOI] [PubMed] [Google Scholar]
- 15. Mistry RD, Shapiro DJ, Goyal MK, et al. Clinical management of skin and soft tissue infections in the U.S. emergency departments. West J Emerg Med 2014; 15:491–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Prusakowski MK, Kuehl DR. Trends in emergency department management of skin abscesses. Am J Infect Control 2015; 43:336–40. [DOI] [PubMed] [Google Scholar]
- 17. Dantes R, Mu Y, Belflower R, et al. national burden of invasive methicillin-resistant Staphylococcus aureus infections, United States, 2011. JAMA Intern Med 2013; 173:1970–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Stenehjem E, Stafford C, Rimland D. Reduction of methicillin-resistant Staphylococcus aureus infection among veterans in Atlanta. Infect Control Hosp Epidemiol 2013; 34:62–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Morgan E, Daum RS, David MZ. Decreasing incidence of skin and soft tissue infections with a seasonal pattern at an academic medical center, 2006–2014. Open Forum Infect Dis 2016; 3:ofw179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Charlebois ED, Bangsberg DR, Moss NJ, et al. Population-based community prevalence of methicillin-resistant Staphylococcus aureus in the urban poor of San Francisco. Clin Infect Dis 2002; 34:425–33. [DOI] [PubMed] [Google Scholar]
- 21. Crum-Cianflone NF, Grandits G, Weintrob A, Ganesan A, Agan B, Landrum M. Skin and soft tissue infections among HIV-infected persons in the late combination antiretroviral therapy era. Int J STD AIDS 2012; 23:507–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. StataCorp. Stata Statistical Software: release 14. College Stations, TX: StataCorp, 2015. [Google Scholar]
- 23. Landrum ML, Neumann C, Cook C, et al. Epidemiology of Staphylococcus aureus blood and skin and soft tissue infections in the US military health system, 2005–2010. JAMA 2012; 308:50–9. [DOI] [PubMed] [Google Scholar]
- 24. Diep BA, Chambers HF, Graber CJ, et al. Emergence of multidrug-resistant, community-associated, methicillin-resistant Staphylococcus aureus clone USA300 in men who have sex with men. Ann Intern Med 2008; 148:249–57. [DOI] [PubMed] [Google Scholar]
- 25. Anderson E, Hawkins C, Bolon M, Palella F Jr. A series of skin and soft tissue infections due to methicillin-resistant Staphylococcus aureus in HIV-infected patients. J Acquir Immune Defic Syndr 2008; 48:567–71. [DOI] [PubMed] [Google Scholar]
- 26. Hemmige V, McNulty M, Silverman E, David MZ. Predictors of skin and soft tissue infections in HIV-infected outpatients in the community-associated methicillin-resistant Staphylococcus aureus era. Eur J Clin Microbiol Infect Dis 2015; 34:339–47. [DOI] [PubMed] [Google Scholar]
- 27. Graber CJ, Jacobson MA, Perdreau-Remington F, Chambers HF, Diep BA. Recurrence of skin and soft tissue infection caused by methicillin-resistant Staphylococcus aureus in a HIV primary care clinic. J Acquir Immune Defic Syndr 2008; 49:231–3. [DOI] [PubMed] [Google Scholar]
- 28. Hemmige V, McNulty M, Silverman E, David MZ. Recurrent skin and soft tissue infections in HIV-infected patients during a 5-year period: incidence and risk factors in a retrospective cohort study. BMC Infect Dis 2015; 15:455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Centers for Disease Control and Prevention. Trends in U.S. HIV diagnoses, 2005–2014. Available at:https://www.cdc.gov/nchhstp/newsroom/docs/factsheets/hiv-data-trends-fact-sheet-508.pdf. Accessed 27 February 2017. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.