Abstract
Background:
Clinicians play an important role in containing pharmaceutical spending at the patient level, as well as ensuring efficacy and quality outcomes, yet little research has examined how to achieve this goal.
Measures:
Using auditing and feedback (A&F) as part of a Pharmacy and Therapeutics (P&T) Committee, we evaluated our community-based hospice program’s prescribing habits for opioids, antipsychotics, and antidepressants and calculated oral pharmaceutical prescription costs per-patient-day (PPD). Quality of care was reflected by patient pain scores in electronic medical records.
Interventions:
Our P&T Committee adopted an A&F approach to monitor and assess provider prescribing habits and cost. An already-existing pain quality improvement program assessed care quality.
Outcomes:
Pain relief either improved or was maintained while medication costs were reduced by over $1.00 PPD from 2010 to 2011.
Conclusions/Lessons Learned:
An active, hospice P&T Committee featuring A&F can significantly affect medication costs for a hospice program while maintaining or improving patient outcomes.
Keywords: auditing and feedback, hospice, pharmacy and therapeutics, expenditures
Background
Pain relief is central tenant of quality hospice and palliative care, making it a reasonable target of quality improvement efforts. Recently, we described outcomes from an electronic medical records-based quality improvement pain monitoring and treatment initiative in a large hospice and palliative care provider (1). This program resulted in numerous statistically significant and clinically meaningful improvements in the documentation of patient-reported pain scores and decreases in the incidence of problematic pain after initial incident. Outcomes improved despite an increase in census and were maintained for 5 years following the study period, suggesting the program was both feasible and sustainable.
Cost containment was not an outcome of interest mandated by the Hospice Quality Reporting Program but would nonetheless be a valuable endpoint. Because pharmaceutical costs continue to make up a large share of the United States’ healthcare expenditures, more research is needed to assess how clinicians can aid the containment of this spending at the patient level (2). In 2012, over $200 billion of healthcare costs were driven by the improper and unnecessary prescription of medicines–amounting to 8% of that year’s national healthcare spending (3). Meaningful research assessing the impact of initiatives aimed specifically at changing the prescribing patterns of clinicians is therefore essential for aiding the provision high-quality care in an increasingly cost-constrained environment.
One potential strategy to address quality improvement and cost containment concerns the implementation of auditing and feedback (A&F), a behavior change method which entails providing clinicians with details of their performance over time. Despite its widespread use, however, economic and performance outcomes of A&F are varied. Several studies concluded that A&F had a statistically significant but marginally important effect in altering clinical practice patterns (4). Alternately, other research suggests A&F initiatives can lead to real changes in physician prescribing behaviors (5), including a reduction in inappropriate prescribing and lower drug expenditures. However, little is known about the implementation of A&F in community hospice settings, where responsible but economic pain prescribing is highly desirable.
There is also scant literature about the use of Pharmacy and Therapeutics Committees (P&T) in community hospice settings to reduce expenditures. Snapp and colleagues (6) report successfully implementing a P&T Committee, which included developing a Preferred Drug List and incorporating ongoing staff education programs, to decrease opioid drug acquisition costs while maintaining high patient satisfaction with pain control. Hospice clinicians and administrators could benefit from research that clarifies how P&T Committees, and particularly those incorporating A&F, could potentially be leveraged to reduce pharmacy spending, especially in the face of increasing patient volume.
The aim of this paper is to report outcomes from (1) A&F elements designed to alter clinician’s oral pharmaceutical prescribing patterns and (2) using pain scores to monitor effects of the A&F intervention. This paper helps extend the literature about the use of A&F in community hospice settings by describing the retrospective evaluation of leveraging, through a P&T Committee, A&F strategies to provide cost-effective yet high-quality care. This could potentially provide a model for other hospice organizations seeking to use formulary management as a way to reduce pharmacy spending.
Measures
The aim of the A&F mechanism was to measure and track prescribing of opioids, antipsychotics, and antidepressants. The cost-containment portion of the A&F program emphasized the following strategies: utilizing the relationships and contracting power of the Pharmacy Benefits Manager; performing a quality review of prescribed medications; prescribing medication quantities appropriate for hospice patients; setting preauthorization thresholds to curb unnecessary high-cost prescribing; and, finally, providing an A&F mechanism for clinicians regarding their use of generics and adherence to the evidence-based Preferred Drug List that was jointly developed by the P&T Committee and the Pharmacy Benefits Manager. Cost-related outcomes were measured by calculation of oral pharmaceutical prescription costs per-patient-day (PPD).
Pain was measured as a metric of quality care and is regularly collected and documented in the electronic medical record as a required element of every nurse and physician encounter. To assess our progress in achieving the pain quality aims, pain relief data was recorded in the electronic medical record based on each patient’s reported discomfort at the start of care and again within 48 hours of initiating care using a 0–10 pain scale. Pain data was aggregated by a QI Committee, enabling us to pull data while blinded to PHI. Individual and aggregate pain data were collated to measure improvement in reporting and care over time.
Intervention
P&T Committee/A&F Intervention
In 2007, our hospice and palliative care organization established a P&T Committee and sought to develop a set of symptom management algorithms to help monitor and refine pharmaceutical care delivery. As noted above, a Preferred Drug List was established, and clinician adherence was tracked. Prescriber education was targeted to those clinicians who were consistently outside the desired prescribing pattern as defined by national benchmarks provided by the Pharmacy Benefits Manager as well as by an internal analysis of our own clinicians practicing in similar settings. Prescriber education was provided at medical staff meetings by the chief of medical staff and staff pharmacist and consisted of an evidence-based review of prescribing recommendations. Informational handouts regarding critical medication choices (e.g., choice of opioid) also were provided.
These initial small efforts brought some success, but costs continued to increase dramatically despite adherence to the Preferred Drug List. In mid-2008, our hospice and palliative care organization transitioned to a new Pharmacy Benefits Manager and made medication cost containment (while preserving quality of care) a priority effort. We developed a strong relationship with the new Pharmacy Benefits Manager through weekly meetings with the consultant pharmacist. Committee members regularly reviewed invoices and prescribing data to identify factors contributing to unnecessary spending. It became evident that, at that time, three categories of medications were primarily driving up costs: opioid analgesics, antidepressants, and antipsychotics.
Staff-wide and individually targeted education programming was implemented by incorporating into the P&T Committee an A&F element. This was included in monthly Capital Caring medical staff meetings with the ultimate goals of transitioning to more cost-effective but equally efficacious oral drugs and decreasing oral pharmaceutical prescription costs. We hypothesized that, through A&F, clinicians’ recognition of the financial impact of clinical decisions would lead to more economical prescribing without a negative effect on clinical outcomes.
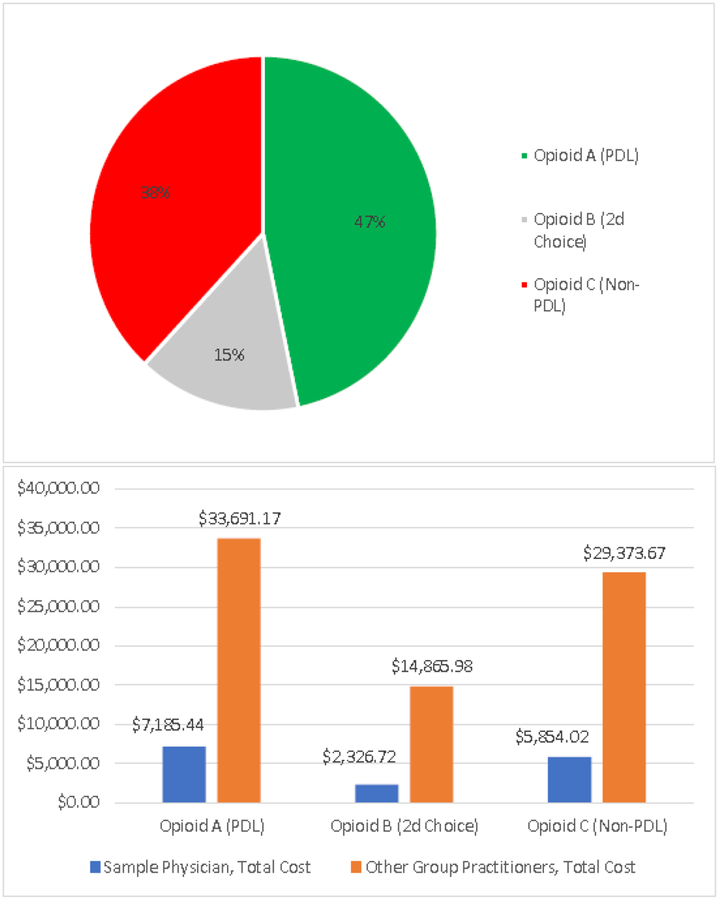
In meetings where pharmaceutical prescribing patterns and costs were discussed, physicians and nurse practitioners were provided with personal files containing A&F information. On average, these files were provided on a quarterly basis. The personal profiles illustrated, for each clinician, his or her prescribing pattern of 8 commonly prescribed medications in 3 classes (i.e., opioids, antidepressants, and antipsychotics) that would have the most significant effect on financial performance without affecting efficacy, as our consultant pharmacists had identified appropriate alternatives. In addition, these profiles included comparisons to the performance of his/her peers. For example, the individual profile contained a pie chart of opioid usage based on adherence to the Preferred Drug List (Figure 1, top image). During the feedback process, clinicians were also shown data on group performance, allowing them to compare their individual opioid prescribing patterns to those of their peers. This was reinforced by also providing clinicians an accompanying bar graph showing their individual opioid prescribing costs compared to the overall dollars spent on opioids by all hospice prescribers (Figure 1, bottom image). These pie charts and bar graphs were presented for all 3 classes and all 8 medications of interest. In addition, the packet contained a graph showing each clinician’s total spending on generic versus branded drugs, as well as a summary graph depicting the number of prescriptions written for these 8 medications for a rolling 12-month period. For those clinicians who were not adhering to recommended practice, a handwritten note was made on their personal file by the chief of staff, and a conversation would usually ensue.
Figure 1. Sample Clinician Prescribing Profile Including Individual Prescribing Habits (PDL vs Non-PDL Prescriptions) and Comparisons to Other Group Practitioners.
Pie chart shows an individual prescriber’s adherence to PDL prescribing of opioids.
Bar graph shows that individual prescriber’s opioid costs compared to the combined total of the rest of the medical group
Outcomes
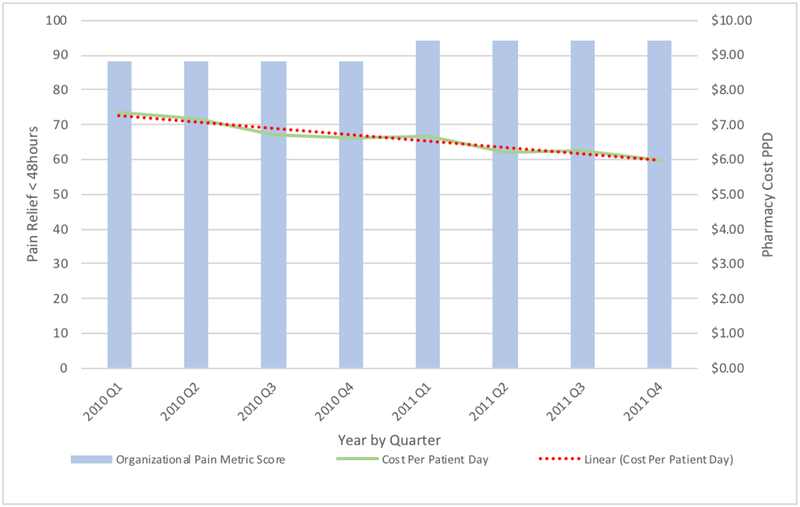
Our data analysis revealed that, overall, PPD prescription costs decreased by approximately 19% (from $7.33 to $5.98) from Q1 of 2010 to Q4 of 2011. Over the same period, an increase in average daily patient census was observed, and pain, which is 1 of the metrics of care quality we routinely monitor, increased or stayed stable (Figure 2). Specifically, the percent of patients with problematic pain (i.e., pain score 4 or greater) who were provided pain relief within 48 hours (i.e., pain score decreased to <4) increased from 88% in Q1 of 2010 to 94% by Q4 of 2011.
Figure 2.
Pain Metric Score and Cost Per-Patient-Day by Quarter (2010–11)
Lessons Learned
Preliminary data evaluation suggests that Capital Caring’s P&T Committee/A&F intervention was effective in improving and maintaining quality care (as indicated by pain score) while lowering the cost of oral pharmaceutical prescriptions PPD by encouraging clinicians to use of more cost-effective drugs. That decreases in spending were accompanied by similar or improved patient-reported pain scores and increases in patient census suggests that cost containment did not occur at the expense of quality patient care. This is consistent with a previously published report of a P&T Committee to reduce pharmaceutical expenditures while preserving patients’ satisfaction with pain care in an outpatient hospice setting (6).
Our findings are consistent with previous research suggesting that A&F can have a small but meaningful effect on clinical and nonclinical practice-related outcomes, particularly when compared to no intervention or when compared to audit alone or feedback alone (3). Physician feedback that utilizes peer comparator benchmarks is an understudied but potentially useful strategy that could incentivize desirable, high-value practice behaviors and targeted clinical outcomes (7). These include reducing inappropriate prescribing and minimizing unnecessary variations in care (7). Peer comparison feedback reports may be especially effective when tailored to specific performance goals or behaviors and when practice patterns are clearly depicted using a variety of graphics, images, and formatting (8). Moreover, some reports have shown that, depending on the design of the intervention, the implementation of A&F programs can nullify the savings it produces (9). When comparing our implementation of A&F to that reported in the literature, reasons for this specific intervention’s success may be attributed to several key characteristics. First, feedback was provided, both verbally and in writing, by the chief of the medical staff. Second, it was provided frequently, on a monthly basis. Third, it was individualized for each clinician and compared to peer performance.
Evaluating the effectiveness of P&T Committee strategies in general for improving cost-effective prescribing habits in home hospice is of timely import given the recent Medicare hospice payment reform. While Medicare continues to reimburse for hospice services at a fixed daily rate for each day that a patient is enrolled in the Hospice benefit. These ‘per diem’ payments are made regardless of the actual costs associated with providing hospice care and, since 2016, these payment now decrease based on length of stay. Historically, reimbursements were limited to only those interventions and medications related to hospice diagnoses. However, in the FY 2014 Hospice Wage Index and Payment rate update, CMS requires that hospices cover all costs associated with providing care for terminally ill patients and, unless there is strong evidence that an illness is not associated to the terminal prognosis, all services are to be considered related. The per diem must cover all care provided by members of the hospice interdisciplinary team; as well as all medical equipment, supplies, therapies, and medications; and all overhead. It is therefore increasingly essential that hospices carefully manage all of their costs while preserving quality and financial outcomes. This is especially true in light of an increasingly ageing population and a greater national use of hospice care.
Conclusion
To our knowledge, there is virtually no published research on cost-effectiveness outcomes derived from P&T Committee/A&F strategies implemented in outpatient hospice settings. This report helps address this gap by describing an approach to utilizing P&T Committees—and A&F in particular—that potentially could be modeled by other community hospice and palliative care systems. Despite the fact that our costs were reduced by more than $1 PPD, our patients received the same medications and the same number of prescriptions per patient as before implementation of the A&F program. This suggests that the P&T Committee (heavily featuring those A&F strategies) was able to successfully contain expenditures without sacrificing quality of care or impinging on patient outcomes, at least in relation to pain outcomes. We did not correlate depression and anxiety metrics with A&F processes in the same manner as we did our pain metric, which should be investigated in future studies.
There is a clear need for more scientifically rigorous research in this field. Whereas evaluating the effect of quality improvement initiatives is important to confirm that desired changes in practice have ensued, it is difficult to attribute causation to such studies. Further rigorous research in the form of randomized control trials would produce more generalizable results where causation could be evaluated. Despite the real potential of P&T Committees and A&F strategies to increase quality and reduce costs (5, 7, 8), the scarcity of systematic and coordinated research in this area has led to significant knowledge gaps in how to design effective programs across settings, patient populations and, provider groups (10).
Acknowledgements:
The authors gratefully acknowledge the contribution of the members of the Pharmacy Benefits Manager team for their tireless working in making the P&T Committee initiatives successful.
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Disclosures: None of the authors have any disclosures to report
References
- 1.Muir JC, Davis MS, Connor S, Kuhl EA, Fine PG. A systematic assessment and monitoring intervention to improve pain management and quality reporting among home hospice patients. J Pain Symp Manage 2018; 56(6):957–961. [DOI] [PubMed] [Google Scholar]
- 2.Hoffman JM, Li E, Doloresco F, Matusiak L, Hunkler RJ, Shah ND, Vermeulen LC, Schumock GT. Projecting future drug expenditures – 2012. A J Health Sys Pharmacists 2012; 69: e5–e21 [DOI] [PubMed] [Google Scholar]
- 3.IMS 2013. Avoidable Costs in U.S. Healthcare: The $200 Billion Opportunity from Using Medicines More Responsibly. Report by the IMS Institute for Healthcare Informatics. Available at: http://www.imshealth.com/deployedfiles/imshealth/Global/Content/Corporate/IMS%20Institute/RUOM-2013/IHII_Responsible_Use_Medicines_2013.pdf
- 4.Balas EA, Boren SA, Brown GD, Ewigman BG, Mitcell JA, Perkoff GT, 1996. Effect of physician profiling on utilization. Meta-analysis of randomized clinical trials. Journal of General Internal Medicine, 11:584–90 [DOI] [PubMed] [Google Scholar]
- 5.Ivers N, Jamtvedt G, Flottorp S, Young JM, Odgaard-Jensen J, French SD, O’Brien MA, Johansen M, Grimshaw J, Oxman AD, 2012. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database System Review, 13:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Snapp J, Kelley D, Gutgsell TL. Creating a hospice pharmacy and therapeutics committee. Am J Hosp Palliat Care 2002;19(20):129134. [DOI] [PubMed] [Google Scholar]
- 7.Navathe AS, Emanuel EJ. Physician Peer Comparisons as a Nonfinancial Strategy to Improve the Value of Care. JAMA. 2016. November 1;316(17):1759–1760. [DOI] [PubMed] [Google Scholar]
- 8.McNamara P, & McNellis RJ. Making Physician Feedback Reports More Effective. NEJM Catalyst; January 3, 2018. Retrieved July 10, 2018, from https://catalyst.nejm.org/physician-feedback-reports-effective/ [Google Scholar]
- 9.Schroeder SA, Kenders K, Cooper JK, et al. , 1973. Use of laboratory tests and pharmaceuticals: variation among physicians and effect of cost audit on subsequent use. JAMA, 225:969. [PubMed] [Google Scholar]
- 10.Ivers NM, Sales A, Colquhoun H, Michie S, Foy R, Francis JJ, Grimshaw JM, 2014. No more ‘business as usual’ with audit and feedback interventions: towards an agenda for a reinvigorated intervention. Implementation Science, 9:14. [DOI] [PMC free article] [PubMed] [Google Scholar]