Mast cell disorders (mastocytosis) are a hematologic neoplasm defined by abnormal expansion and dense accumulation of clonally altered mast cells in various organ systems.1–5 The disease exhibits a complex pathology and an equally complex pattern of clinical presentations.1–5 The classification of the World Health Organization (WHO) splits mast cell disorders into cutaneous entities, systemic variants, and localized mast cell tumors.2–5 In more than 80% of all cases with systemic mastocytosis (SM), a somatic point mutation in KIT at codon 816 is detected.3–6 Whereas patients with indolent forms of the disease have a normal or close-to-normal life expectancy, patients with advanced mast cell neoplasms, including aggressive SM (ASM) and mast cell leukemia (MCL), have an unfavorable prognosis with clearly reduced survival times.2–5 In a majority of these patients, multiple somatic mutations and/or an associated hematologic neoplasm, such as a myeloid leukemia, can be detected. Regardless of the category of mastocytosis and the serum tryptase level, patients with mast cell disorders may suffer from (more or less severe) mediator-related symptoms and/or osteopathy.1–5 Depending on co-morbidities, the symptoms in such patients require anti-mediator-type therapy and may be mild, more severe, or even life-threatening.5
A number of different mediators and cytokines are produced by mast cells and are involved in the clinical symptoms and pathological features that can be recorded in patients with mastocytosis.7–12 Histamine is considered one of the most relevant mediators released from activated mast cells in patients with mastocytosis.1–5,9 In fact, many of the symptoms reported by patients with SM can be kept under control by applying histamine receptor (HR)1 and HR2-targeting drugs.5 However, mast cells also produce other clinically relevant mediators, such as prostaglandin D2, leukotrienes, heparin and tryptases.1,9,13,14 In addition, activated mast cells can produce and release a number of functional cytokines, such as tumor necrosis factor (TNF), oncostatin M (OSM), or interleukin-6 (IL-6).7–14 So far little is known about the mechanisms underlying the production and release of these cytokines in neoplastic mast cells in patients with SM. In many instances, activation of KIT and/or the IgE receptor may play a role in cytokine secretion.7,9 Correspondingly, most of these cytokines are measurable in the sera of patients with SM and, in several instances, cytokine levels correlate with the variant of SM and with prognosis.7–12 For example, a clear correlation between the variant of SM and IL-6 levels has been described.11,12 In addition, in SM, elevated IL-6 levels are regarded as an indicator of a poor prognosis.11,12
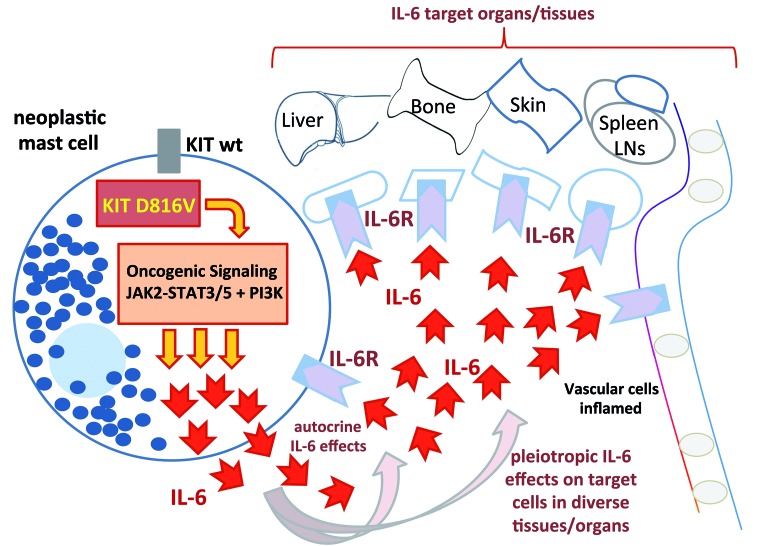
In this issue of the Journal, Tobío et al. report that the D816V-mutated KIT receptor triggers expression and release of IL-6 in neoplastic mast cells.15 In particular, they were able to show that bone marrow mast cells in patients with KIT D816V+ SM express and release IL-6, and that the levels of IL-6 in cultured mononuclear cells in these patients correlate with the D816V KIT allele burden and with the percentage of mast cells in these samples.15 In addition, they found that human mast cell lines expressing KIT D816V produce and secrete IL-6. Finally, they deciphered the KIT D816V-dependent signaling machinery that triggers IL-6 production in neoplastic mast cells. It is worth noting that these signaling molecules, like PI3K, AKT, TOR or JAK2-STAT5, represent druggable therapeutic targets.15 An overview of the concept proposed by Tobío et al. is shown in Figure 1.
Figure 1.
An overview of the concept proposed by Tobío et al.15 of the KIT D816V-dependent signaling machinery that involves PI3K, AKT, TOR, and JAK2-STAT5 and triggers IL-6 production in neoplastic mast cells. In most patients with systemic mastocytosis, the transforming KIT mutation D816V is expressed in neoplastic mast cells. The KIT mutant form induces oncogenic signaling pathways which in turn leads to an abnormal production of various effector molecules, including cytokines. One such cytokine is interleukin-6 (IL-6). In contrast to normal mast cells, KIT D816V-transformed mast cells express and release substantial amounts of this cytokine (red arrows). Once released, IL-6 acts as an autocrine growth stimulator as well as a trigger of cell activation and inflammation. The effects of IL-6 on various target cells are exerted via specific IL-6 receptors (IL-6R).
IL-6 is a multi-functional cytokine that plays a role in various biological and pathological processes. In particular, IL-6 has been implicated as a regulator of inflammatory reactions, infectious diseases and host defense, stromal reactions, and bone metabolism. In various neoplastic states, elevated levels of IL-6 have been reported, and in most disease models, higher IL-6 levels are associated with a poor prognosis.11,12,16–18 Based on these observations, IL-6 has also been discussed as a new potential therapeutic target in chronic inflammatory and neoplastic disorders.19
In mastocytosis, IL-6 has been implicated as a potential mediator of mast cell development and activation, accumulation and function of lymphocytes, bone marrow remodeling, and bone pathology (ostesclerosis, osteopenia/osteoporosis). In addition, high IL-6 levels have been implicated as a prognostic parameter in SM.11,12 In this regard, it is noteworthy that IL-6 may also act as an autocrine growth factor for neoplastic mast cells (Figure 1).
The observation by Tobío et al. confirms the impact of IL-6 in SM and suggests that IL-6 production in neoplastic mast cells is triggered by the oncogenic signaling machinery activated by KIT D816V (Figure 1).15 This observation may have clinical implications and may lead to the development of new treatment concepts. For example, high IL-6 levels may already be detected in indolent SM (ISM) before the disease progresses to ASM or MCL.11,12 In these cases, high IL-6 levels may serve as a biomarker of “high risk ISM” where a closer follow up or early interventional therapy may be considered.
There may be several ways to interfere with KIT D816V-dependent signaling in neoplastic mast cells in SM. One is to apply strong inhibitors of KIT D816V, such as midostaurin or avapritinib.20–23 It will be of great interest to learn whether IL-6 levels decrease during therapy with these KIT-targeting drugs. Another possibility may be to block KIT-downstream signaling molecules involved in IL-6 production, such as JAK2 or PI3K. Indeed, the data of Tobío et al. suggest that signaling through these target molecules leads to IL-6 production in neoplastic mast cells (Figure 1).15 Finally, IL-6 effects can directly be blocked by applying antibodies against IL-6 or the IL-6 receptor.24 However, it remains unclear whether these drugs can block the symptoms and pathologies in patients with SM.
Acknowledgments and Funding
Research by PV and his team is supported by the Austrian Science Fund, grants F4701-B20 and F4704-B20.
References
- 1.Metcalfe DD. Mast cells and mastocytosis. Blood. 2008;112(4):946–956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Valent P, Horny HP, Escribano L, et al. Diagnostic criteria and classification of mastocytosis: a consensus proposal. Leuk Res. 2001;25(7):603–625. [DOI] [PubMed] [Google Scholar]
- 3.Akin C, Valent P. Diagnostic criteria and classification of mastocytosis in 2014. Immunol Allergy Clin North Am. 2014;34(2):207–218. [DOI] [PubMed] [Google Scholar]
- 4.Valent P, Akin C, Metcalfe DD. Mastocytosis: 2016 updated WHO classification and novel emerging treatment concepts. Blood. 2017;129(11):1420–1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Valent P, Akin C, Gleixner KV, et al. Multidisciplinary Challenges in Mastocytosis and How to Address with Personalized Medicine Approaches. Int J Mol Sci. 2019;20(12). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arock M, Sotlar K, Akin C, et al. KIT mutation analysis in mast cell neoplasms: recommendations of the European Competence Network on Mastocytosis. Leukemia. 2015;29(6):1223–1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hoermann G, Cerny-Reiterer S, Perné A, et al. Identification of oncostatin M as a STAT5-dependent mediator of bone marrow remodeling in KIT D816V-positive systemic mastocytosis. Am J Pathol. 2011;178(5):2344–2356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rabenhorst A, Christopeit B, Leja S, et al. Serum levels of bone cytokines are increased in indolent systemic mastocytosis associated with osteopenia or osteoporosis. J Allergy Clin Immunol. 2013;132(5):1234–1237.e7. [DOI] [PubMed] [Google Scholar]
- 9.Theoharides TC, Valent P, Akin C. Mast Cells, Mastocytosis, and Related Disorders. N Engl J Med. 2015;373(2):163–172. [DOI] [PubMed] [Google Scholar]
- 10.Hoermann G, Greiner G, Valent P. Cytokine Regulation of Microenvironmental Cells in Myeloproliferative Neoplasms. Mediators Inflamm. 2015;2015:869242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brockow K, Akin C, Huber M, Metcalfe DD. IL-6 levels predict disease variant and extent of organ involvement in patients with mastocytosis. Clin Immunol. 2005;115(2):216–223. [DOI] [PubMed] [Google Scholar]
- 12.Mayado A, Teodosio C, Garcia-Montero AC, et al. Increased IL6 plasma levels in indolent systemic mastocytosis patients are associated with high risk of disease progression. Leukemia. 2016;30(1):124–130. [DOI] [PubMed] [Google Scholar]
- 13.Galli SJ, Tsai M. Mast cells: versatile regulators of inflammation, tissue remodeling, host defense and homeostasis. J Dermatol Sci. 2008;49(1):7–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mukai K, Tsai M, Saito H, Galli SJ. Mast cells as sources of cytokines, chemokines, and growth factors. Immunol Rev. 2018;282(1):121–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tobío A, Bandara G, Morris DA, et al. Oncogenic D816V-KIT signaling in mast cells causes persistent IL-6 production. Haematologica. 2019;105(1):124–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Burger R. Impact of Interleukin-6 in Hematological Malignancies. Transfus Med Hemoth. 2013;40(5):336–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Taniguchi K, Karin M. IL-6 and related cytokines as the critical lynch-pins between inflammation and cancer. Semin Immunol. 2014;26(1):54–74. [DOI] [PubMed] [Google Scholar]
- 18.Hong DS, Angelo LS, Kurzrock R. Interleukin-6 and its receptor in cancer: implications for translational therapeutics. Cancer. 2007;110(9):1911–1928. [DOI] [PubMed] [Google Scholar]
- 19.Rossi JF, Lu ZY, Jourdan M, Klein B. Interleukin-6 as a therapeutic target. Clin Cancer Res. 2015;21(6):1248–1257. [DOI] [PubMed] [Google Scholar]
- 20.Gotlib J, Kluin-Nelemans HC, George TI, et al. Efficacy and Safety of Midostaurin in Advanced Systemic Mastocytosis. N Engl J Med. 2016;374(26):2530–2541. [DOI] [PubMed] [Google Scholar]
- 21.Valent P, Akin C, Hartmann K, et al. Midostaurin: a magic bullet that blocks mast cell expansion and activation. Ann Oncol. 2017;28(10):2367–2376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Arock M, Wedeh G, Hoermann G, et al. Preclinical human models and emerging therapeutics for advanced systemic mastocytosis. Haematologica. 2018;103(11):1760–1771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lübke J, Naumann N, Kluger S, et al. Inhibitory effects of midostaurin and avapritinib on myeloid progenitors derived from patients with KIT D816V positive advanced systemic mastocytosis. Leukemia. 2019;33(5):1195–1205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kang S, Tanaka T, Kishimoto T. Therapeutic uses of anti-interleukin-6 receptor antibody. Int Immunol. 2015;27(1):21–29. [DOI] [PubMed] [Google Scholar]