Madam,
Obesity with high variability of epidural space, its depth and anatomical references increase the challenges of an anesthesiologist leading to procedural complications. Ultrasound being used in various fields of anesthesiology is also becoming popular in central neuraxial procedures. Following case demonstrates the use of ultrasound in neuraxial procedures as a guide to epidural space in obese patients.
Fifty five-year old male with weight 170 kg, height 185 cm and Body Mass Index of 49.6 kg/m2 was posted for infected femur implant removal and debridement. Patient was accepted for surgery under combined spinal epidural anesthesia (CSEA).
The patient had indistinct spine anatomical landmarks along with obesity, therefore we opted to perform a lumbar ultrasound scan using a low-frequency (2–5 MHz) curvilinear probe. After an informed written consent, preprocedural ultrasound scan was done in sitting arched back posture. The level of intervertebral space (L3–L4, L4–L5) and midline was identified in median longitudinal view of ultrasound using counting up method and marked with the skin marker. Then, the probe was moved 90°, that is, in transverse position and inclined slightly, to obtain image of the epidural space in interlaminar transverse view. After freezing the image, the depth of the epidural and dural space were measured with electronic caliper from the skin point to the mid surface and anterior surface of the posterior complex seen, respectively. Epidural and dural depth measured by ultrasound were 8.43 cm and 8.66 cm, respectively [Figure 1]. Needle insertion site was marked for both the spaces using interlaminar transverse view.
Figure 1.
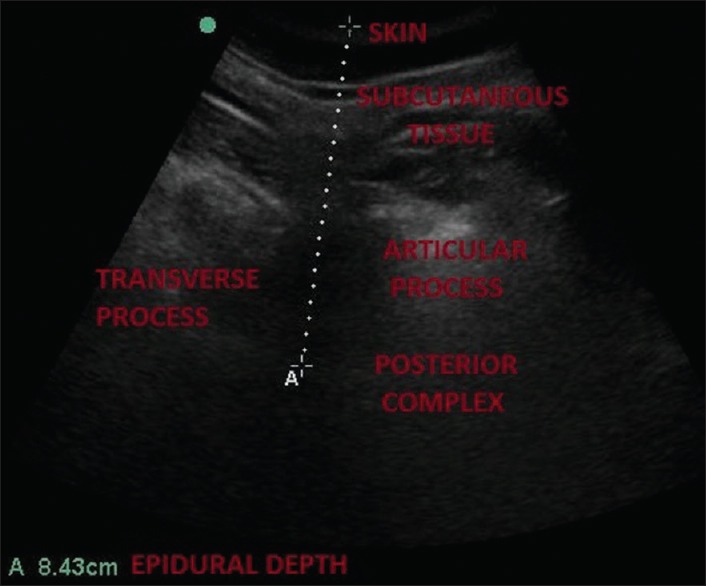
Epidural depth of the patient is 8.43 cm as measured by ultrasound in transverse interlaminar view using a curvilinear probe
Epidural and spinal components of CSEA were administered separately using Tuohy's needle (Vygon 16G, L90 mm, 1.35 × 1.65 mm ref184.16) and Quincke's needle (BD, 25G, L90 mm), respectively, at marked needle insertion site with predetermined epidural and dural depth in first attempt. Predetermined epidural depth was confirmed with loss of resistance technique. The surgery lasted for 3.5 hours and was uneventful.
In 1980, use of ultrasound was first demonstrated in epidural anesthesia and since then, potential uses of preprocedural use of ultrasound in obstetric population have been demonstrated.[1,2] In 2008, NICE guidelines were issued regarding use of ultrasound for epidural catheterisation.[3]
KJ chin et al. and Srinivasan et al. have described the sonoanatomy of neuraxial structures.[1,4]
The interspinous spaces were chosen based on visualisation and clarity of posterior complex and anterior complex assuming that their presence suggests a sufficiently large acoustic window through which a needle can pass. As posterior complex was only visualised, technical difficulty of the procedure could be anticipated that correlated with clinical findings therefore, needle insertion site was marked to decrease the technical difficulty as concluded by Perlas et al.[5]
Preprocedural use of ultrasound accurately measured epidural depth and was useful in selecting the appropriate length of the needle and preventing accidental dural puncture. Lumbar ultrasound scan helped us to choose 9 cm Tuohy's needle in first attempt instead of usual 8 cm Tuohy's needle, preventing multiple attempts of puncture. Given the predetermined epidural depth and needle insertion site, ultrasound scan would also facilitate learning curve and decrease the complications.
Ultrasound lumbar scan can also help in decision-making both for an anesthesiologist and the patient. Patients can have either soft or hard copy of their scan predicting technical difficulty and epidural depth, helping them to choose appropriate anesthesia plan considering their benefits and risks. This strategy will ascertain anesthesiologist to identify patients at risk of multiple attempts and complications like accidental dural puncture and to select the appropriate length of the needle. This will prompt the anesthesiologist to use an adjunct like preprocedural ultrasound scan to mark the best interspace or point of needle insertion before the procedure, to get a lumbar spine X-ray done preoperatively, have a low threshold to abort the procedure or even change the anesthesia plan. Ultrasound lumbar scan is a non-invasive, easily accessible and safe tool with steep learning curve involving around 35–40 pilot cases.[1]
To conclude, lumbar ultrasound scan is a useful guide to epidural space. Anesthesiologist should be encouraged to increasingly adopt preprocedural lumbar ultrasound scan especially in obese patients in modern anesthesiology practice for raising health care standards and safety.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Chin KJ, Karmakar MK, Peng P. Ultrasonography of the adult thoracic and lumbar spine for central neuraxial blockade. Anesthesiology. 2011;114:1459–85. doi: 10.1097/ALN.0b013e318210f9f8. [DOI] [PubMed] [Google Scholar]
- 2.Lie J, Patel S. Ultrasound for obstetric neuraxial anesthetic procedures: Practical and useful.? J Obstet Anaesth Crit Care. 2015;5:49–53. [Google Scholar]
- 3.National Institute for Health and Care Excellence. Ultrasound-guided catheterisation of the epidural space. London: NICE; 2008. [Last cited on 2018 Jun 01]. Available from: http://www.nice.org.uk/nicemedia/pdf/ipg249guidance.pdf . [Google Scholar]
- 4.Srinivasan KK, Lee PJ, Lohom G. Ultrasound for neuraxial blockade. Med Ultrason. 2014;16:356–63. [PubMed] [Google Scholar]
- 5.Perlas A, Chaparro LE, Chin KJ. Lumbar Neuraxial ultrasound for spinal and epidural anesthesia: A systemic review and meta-analysis. Reg Anesth Pain Med. 2016;41:251–60. doi: 10.1097/AAP.0000000000000184. [DOI] [PubMed] [Google Scholar]


