Abstract
The purpose of this systematic review is to (1) synthesize evidence facilitators and barriers affecting adolescent willingness to communicate symptoms to health care providers (HCPs) and (2) create practice recommendations. The PICOT (Population, Intervention, Comparison, Outcome, Time) question guiding the review was, among adolescents with cancer, what factors affect their willingness to communicate symptoms to HCPs? Three databases, PubMed, CINAHL, and PsychINFO, were searched using keywords from the PICOT question. Inclusion criteria included original research studies with samples of at least 51% adolescents aged 10–18 years who were receiving or had received cancer treatment. Studies were included that evaluated outcomes related to willingness to communicate in general as well as communication of specific treatment symptoms. Exclusion criteria included systematic reviews and publications emphasizing cancer screening, cancer prevention, survivorship, or decision making. A total of 11 studies were included in the systematic review. Two of the studies focused on symptom communication; the remaining nine studies focused on general communication or the overlap between general and symptom communication. Barriers to symptom and/or general communication included negative expectations, health-related uncertainty, ambiguousness with assessments, unfamiliarity, restriction of information, perceived negative provider characteristics/behaviors, adolescent circumstance, worry about others' perceptions, and provider approach. Facilitators to symptom and/or general communication included open communication, perceived favorable provider characteristics/behaviors, seasoned adolescent, and patient–provider rapport. Five practice recommendations were developed from the evidence that supports general and symptom communication between adolescents who are receiving or have completed cancer treatment and their HCPs.
Keywords: symptom communication, barriers, facilitators, adolescents, cancer
Introduction
The common developmental and psychosocial milestones of gaining independence and acquiring self-identity that arise during adolescence can be hindered when an adolescent is diagnosed with cancer.1 Changes in body image, separation from peers and school, and presence of new stressors related to cancer and its treatment, combined with increased reliance on adult caregivers, can significantly impede an adolescent's achievement of self-identity and independence.2 In a typical adolescent, development evolves in the cognitive, emotional, and social domains, as evidenced by physical changes seen on brain imaging.3 There is individual variability in adolescent brain maturation that may be correlated with ongoing development of the prefrontal cortex, which is vulnerable to internal and external factors.4 Communication progresses from language fluency, first developed during childhood, to more complex oral and written communication during adolescence that coincides with and improves due to abstract thinking.5
Importantly, specialized communication and relationship-building skills are essential for health care providers (HCPs) who care for adolescents with cancer.6 The American Academy of Pediatrics (AAP) Committee on Bioethics recommends that HCPs include adolescent patients in the discussion of their medical care to the greatest extent possible, and communicate information in a way that is truthful and developmentally appropriate.7 However, evidence is lacking that guides promotion of adolescent communication with their HCPs, particularly in regard to symptoms reporting during cancer treatment.8
Although definitions regarding the specific age range vary, adolescence is generally recognized as beginning when a sense of competency is achieved, and ending with the development of an adult identity,9 which typically corresponds with the ages of 10–18 years.10,11 Because of their need to meet ongoing developmental milestones, adolescents with cancer present distinct challenges and require special attention during lengthy cancer treatement.2
All patients with cancer experience numerous symptoms related to their disease and treatment during and after cancer care, but adolescents may experience more symptoms and more symptom-related distress than younger children.12 A recent study found that patients 12 years and older reported more psychological and psychosomatic symptoms compared with children younger than 12 years of age.13 Despite their more frequent symptoms, adolescents with cancer may not communicate their symptoms to HCPs.12 Many adolescents believe that symptoms are an expected part of cancer treatment that must be endured to treat the disease.14 Poor communication between adolescents and their HCPs can lead to unrelieved symptoms and suffering.12,14 In fact, a qualitative study of adolescents with cancer revealed that symptom-related distress and suffering was the most significant challenge of the cancer experience.15 HCPs need to encourage adolescents to discuss their symptom experiences so that they can receive care that is comprehensive and individualized.16 Therefore, the purpose of this systematic review is (1) to synthesize available evidence regarding factors that promote or deter adolescent willingness to communicate symptoms to HCPs and (2) to provide practice recommendations.
Methods
This systematic review team was formed in 2016 to align with the Children's Oncology Group (COG) Nursing Discipline commitment to promote best nursing practices for children and adolescents receiving protocol-based care.17 The multidisciplinary evidence-based practice (EBP) team consisted of two pediatric nurse practitioners, two family nurse practitioners, and one psychologist. In addition, two doctorally prepared pediatric nurse practitioners with experience in pediatric oncology and EBP served as mentors for the review. All members of the team are employed at COG member institutions.
Question development
The EBP question was developed using the PICOT (Population, Intervention, Comparison, Outcome, Time) format.18 The PICOT question was, “Among adolescents with cancer, what factors affect their willingness to communicate symptoms to healthcare providers?” For this systematic review, adolescents were defined as individuals between the ages of 10 and 18 years. This age range aligns closely with the World Health Organization11 and the National Cancer Institute10 definitions of adolescence. The PICOT question guided the literature search, and the summary and synthesis of the evidence.
Literature search
A comprehensive search of the literature was conducted in February 2017 by the first author with the assistance of a medical librarian. The databases included PubMed (MEDLINE), CINAHL (Cumulative Index to Nursing and Allied Health Literature), and PsycINFO. The MeSH (Medical Subject Headings), CINAHL, and PsycINFO subheadings included pediatrics, adolescents, teenagers, juvenile, neoplasm, carcinoma, tumor, leukemia, communication, professional–patient relationship, patient preference, attitudes, patient engagement, interview, questionnaires, surveys, semistructure, mixed, systematic review, meta-analysis, and qualitative. Searches were conducted with a combination of these subheadings. Limits to the database search included the English language. No date limits were placed on the search to retrieve all evidence related to the topic.
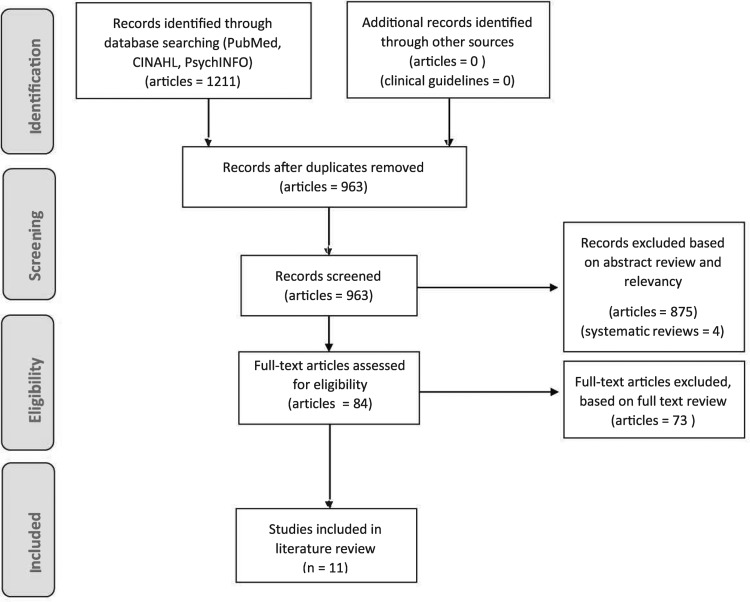
Search results were reviewed for the following inclusion criteria: the sample comprised original research studies with at least 51% of adolescents aged 10–18 years; adolescents were receiving or had received any type of cancer treatment; and outcomes were focused on adolescents' willingness to communicate symptoms. Owing to the limited availability of evidence on communication with symptoms, the inclusion criteria was broadened to include study outcomes focused on adolescent willingness to communicate in general. Exclusion criteria included publications with an emphasis on cancer screening, cancer prevention, survivorship, or decision making. Systematic reviews were excluded due to our aim for original research. The literature search initially yielded 1211 articles. Duplicates were removed for a total of 963 publications. Eight hundred seventy-five records were excluded based on title and abstract review because they were not relevant to the PICOT question, leaving 88 possible articles. Four additional studies were excluded because they were systematic reviews, leaving 84 full text articles to be reviewed. Seventy-three articles were excluded because they did not meet our inclusion criteria, leaving a total of 11 studies included in the review. Most excluded articles did not meet the age requirements for inclusion or were geared toward survivorship. Reference lists of included studies were reviewed for additional evidence; however, no additional evidence met the inclusion criteria. See Figure 1 for the PRISMA diagram.
FIG. 1.
PRISMA diagram.
In addition to the database searches, a search for clinical guidelines related to the PICOT question was conducted within the Agency for Healthcare Research and Quality (AHRQ), National Comprehensive Cancer Network (NCCN), Oncology Nursing Society (ONS), American Society of Clinical Oncology (ASCO), and COG. The search did not yield any relevant clinical guidelines.
Evidence review method
Each member of the team acted as a primary reviewer for one study each month and presented the information during a monthly conference call. One mentor served as the secondary reviewer and presented any additional discussion points about the study during the conference call. In addition to the verbal discussion, each study was summarized using a matrix evidence table.19 The tables included the following information: purpose, design, variables, setting/subjects, measurements and instruments, results/implications, and evidence quality.
Evidence quality was assessed for the following criteria: methodological flaws, inconsistency, indirectness, imprecision, and publication bias according to the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) system.20 The level of evidence using the GRADE system is categorized as very low-, low-, moderate-, or high-quality evidence. Concerns about the evidence quality for each study were presented during the monthly conference calls. Discussion about the evidence quality issues continued until group consensus was reached for each of the GRADE criteria.
Review of the Evidence
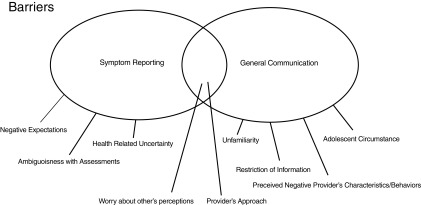
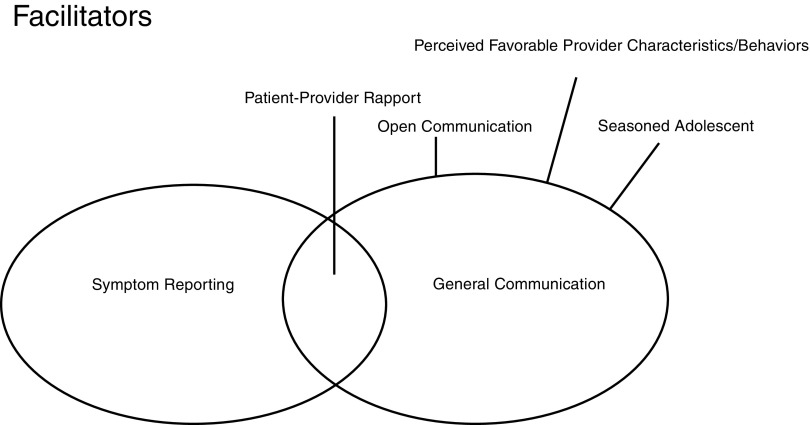
Eleven studies were included in the review of evidence regarding adolescents' willingness to communicate. A summary of each study is listed in Table 1. Symptoms communication was defined as any portion of a study that discussed the communication of specific cancer-related symptoms (e.g., pain). General communication was defined as any portion of a study that discussed communication in general between adolescents and HCPs without any focus on specific cancer-related symptoms (e.g., need for trust). The overlap of general and symptoms communication was defined as any portion of a study that addressed both symptoms and general communication. Two of the studies focused specifically on symptom communication, whereas the remaining nine studies focused on general communication or the overlap between general and symptom communication. Evidence was categorized and reported according to barriers and facilitators of communication about symptoms and general communication and is illustrated in Figures 2 and 3.
Table 1.
Evidence Summary
| First author, year | Sample | Study design, setting | Findings |
|---|---|---|---|
| Ameringer, 2006 | Adolescents (n = 5, ages 13–19 years) | Qualitative, United States, outpatient | • Adolescents worry about the provider perceiving them as a complainer when reporting pain, and parental and provider reactions to reports of pain • Adolescents uncomfortable with using analgesics • Believe pain is inevitable and cannot be relieved |
| Anderzén Carlsson, 2008 | Children and adolescents with cancer (n = 10, ages 3–18 years) and their caregivers, physicians (n = 6), and nurses (n = 4) | Observational, Sweden, outpatient | • Barriers are providers that appear focused on other issues, show a distant attitude, or show a lack of respect |
| Bahrami, 2017 | Adolescents with cancer (n = 12, ages 15–20 years) and their family members (n = 6), physicians or psychosocial providers (n = 6), and nurses (n = 6) | Qualitative, Iran, outpatient | • Adolescents feel disenfranchised when they have limited information about their disease and seldom present information in conversations with HCP and parents. They have unanswered questions and seek information from unreliable sources. • Adolescents may not ask questions due to shyness, embarrassment, lack of time, and perceived hastiness or negligence of the medical team • Parents may act as gatekeepers of medical information, which limits information sharing • Important for HCPs to assess adolescent's desire to receive information and provide information in a way that corresponds to adolescent's level of understanding |
| Coyne, 2016 | Children and adolescents with cancer (n = 20, ages 7–16 years), their parents (n = 22), and health care professionals (n = 40) | Qualitative, Ireland, inpatient or outpatient | • Adolescents prefer an open and honest approach to sharing information and want to be present for important discussions • Adolescents prefer parents to filter what they hear when fearful of hearing bad news or feeling unwell |
| Dunsmore, 1996 | Adolescents and young adults with current or historical diagnosis of cancer (n = 51, ages 15–24 years) | Cross-sectional, exploratory, and descriptive; Australian Teenage Cancer Patients Society; Camp | • Qualities of HCPs that facilitate communication: interactional communication, professional friendship, knowledge and professional expertise, honesty, and a straightforward approach • Qualities of HCPs that hinder communication: impersonal, detached, or professional manner; use of jargon; authoritarian behavior; lack of time or haste; and a generation gap |
| Gibson, 2010 | Children and adolescents with current or historical diagnosis of cancer (n = 38, ages 4–19 years) | Qualitative, United Kingdom, inpatient or outpatient | • Adolescents want to receive information directly from HCPs; information should be clear, specific, unambiguous, and directed at the adolescent • Medical information can be overwhelming; it is helpful when HCPs are open to cues that indicate when it is a good time to talk • Adolescents may not tell HCPs about their worries because they want to avoid being judged • Adolescents appreciate when HCPs try to get to know them • HCPs that listen and are sensitive are easier to approach with worries and preferences for care |
| Ruhe, 2016 | Children and adolescents with cancer (n = 17, ages 9–17 years) | Qualitative, Switzerland, outpatient | • Medical information is confusing and overwhelming and not always provided in a way that helps to anticipate future care • Want to talk directly to HCP • Adolescents' desire to be involved varies |
| Wangmo, 2016 | Children and adolescents with cancer (n = 17, ages 9–17 years) and their parents (n = 19) | Qualitative, Switzerland, inpatient or outpatient | • Communication facilitators: honest and comforting communication and a caring attitude • Communication barriers: communication that does not meet their needs and is too long |
| Weaver, 2016 | Adolescents with cancer (n = 40, ages 12–19 years) | Qualitative, United States, inpatient or outpatient | • Reporting symptoms to HCP is eased with a trusting relationship and a listening provider • Sharing concerns outside of a pre-existing patient/provider relationship is uncomfortable • Ways for HCPs to help adolescents: offer affirmation, use communication as a compass, prioritize a positive approach, see the adolescent as unique, set an example, and attend to the adolescent's space |
| Woodgate, 2008 | Children and adolescents with a current or historical diagnosis of cancer (n = 13, ages 9–17 years) | Qualitative, Canada, outpatient | • Suffering is inevitable • Side effects from treatment and lingering symptoms are “normal” and not reported • Symptoms such as those experienced at diagnosis are scary and not reported • Hard to assign symptoms using a 1–10 scale • Hope providers can tell how they feel based on how they look |
| Zwaanswijk, 2007 | Children and adolescents with a current or historical diagnosis of cancer (n = 25, ages 8–17 years) and parents (n = 11) | Qualitative, The Netherlands, inpatient | • Communication preferences: open and honest; provide reassurance, support and empathy; allow time to talk; appreciate conversation about life, not just about cancer; information presented in an age-appropriate way and directed to the adolescent • Continuity of care valued |
HCP, health care provider.
FIG. 2.
Barriers of adolescents' willingness to communicate.
FIG. 3.
Facilitators of adolescents' willingness to communicate.
Symptom communication barriers
Two studies focused on barriers specific to adolescent symptom communication.16,21 Overarching themes included negative expectations, health-related uncertainty, and ambiguousness with assessments.
Negative expectations
Adolescents expressed a belief that symptoms related to disease, specifically pain, were inevitable with cancer and could not be relieved.16,21 Furthermore, adolescents did not talk about their treatment-related symptoms if side effects of treatment were expected or were persistent during treatment.16
Health-related uncertainty
Adolescents were reluctant to report symptoms if they were concerned that something was seriously wrong, especially if symptoms were similar to those experienced at diagnosis.16 In addition, adolescents were hesitant to report pain, because they were concerned that the subsequent analgesic might cause side effects or addiction.21
Ambiguousness with assessments
Some adolescents did not report symptoms because it was difficult to quantify their symptoms, especially when providers asked them to rate their symptoms on a Likert-type scale.16
General communication barriers
Six studies described barriers associated with general communication between adolescents and providers.22–27 Overarching themes included unfamiliarity, restriction of information, perceived negative provider characteristics/behaviors, and adolescent circumstance.
Unfamiliarity
Adolescents described difficulty understanding medical concepts or terminology22,27 and difficulty asking questions,24 which deterred their willingness to converse with providers. Inexperience with the health care environment also hindered adolescents' willingness to communicate. Adolescents felt less comfortable and more prohibited to talk when there was not a pre-established relationship with the provider.26
Restriction of information
Secrecy or exclusion by a parent and/or HCP impeded the adolescent's willingness to communicate.22 Furthermore, communication was inhibited when adolescents received little or limited information.22
Perceived negative provider characteristics/behaviors
Adolescents reported difficulty communicating when there was a generation gap with the provider, described as the provider being “too clinical, too text-bookie, ancient, or stuffy.”23 Provider behaviors that hampered adolescent communication consisted of using medical jargon,23 providing limited or no anticipatory guidance,25,27 delivering lengthy discussions,25 failing to read patient cues,24 lack of time, hastiness, or unwillingness to do more than the minimum,22,23 and displaying insensitive behaviors such as dishonesty or making false accusations.22 Finally, communication was reduced when adolescents did not have a reliable person to whom they could ask questions.22
Adolescent circumstance
Being shy or embarrassed22 hampered an adolescent's ability to communicate. Feelings of despair or loneliness at the time of diagnosis23 and a sense of being overwhelmed by medical information24,27 also hindered an adolescent's willingness to communicate.
General and symptoms communication barriers
Four studies described factors that deterred both general communication and symptom-related communication.21,23,24,28 These themes included worry about others' perceptions and provider approach.
Worry about others' perceptions
Adolescents worried about sharing concerns for fear of being judged by their provider24; more specifically, they worried about reporting pain for fear that their provider would see them as a complainer.21 Adolescents were also concerned about their parents' reactions to their reports of pain.21
Provider approach
Providers who did not show any response to the adolescent's fear, and/or focused on other issues that were not related to their fears, affected the adolescent's willingness to communicate.28 Other provider factors that hindered both general and symptom communication included a distant attitude,28 lack of respect for the adolescent,28 and an uncaring, impersonal, detached, or intimidating approach.23
Symptom communication facilitators
There were no studies that identified facilitators to promote adolescent symptom reporting.
General communication facilitators
Seven studies described facilitators that improved adolescent and provider general communication.22–25,27,29,30 Overarching themes included open communication, perceived favorable provider characteristics/behaviors, and seasoned adolescent.
Open communication
Adolescents preferred talking directly with their provider,24,27,29,30 having sufficient time for feedback,23 and asking questions.23,25,30 Information was best received when it was specific, clear, and unambiguous.23,24,27 In addition, adolescents wanted providers to read their cues or assess their desire to receive more information.22,24,30
Perceived favorable provider characteristics/behaviors
Adolescents valued honest communication,23,25,29,30 which was integral to establishing trust.29 Providers who exhibited professional expertise facilitated communication.23 The use of humor,23 reassurance,25,30 supportiveness,30 and empathy30 were all seen as preferred provider characteristics.30
Seasoned adolescent
Adolescents who were well acquainted with the hospital environment and treatment routine were more willing to communicate with their provider.30 Having the same HCP at repeated visits was favorable.30
General and symptoms communication facilitators
Four studies identified patient–provider rapport as a theme that supported general and symptoms communication between the adolescent and provider.23,24,26,30
Patient–provider rapport
The establishment of a partnership or bond with the provider was seen by the adolescent as essential for reporting symptoms and sharing general concerns.23,26 Trust was identified as a fundamental principle for developing that partnership.26 Other provider factors identified to help build patient–provider rapport included listening23,24,26,30 and the provider showing a genuine concern for the adolescent as an individual.23,24,30
Quality of Evidence
The 11 articles included in the systematic review consisted primarily of descriptive or qualitative designs, which is associated with a low quality level according to the GRADE appraisal.20 Methodological flaws included two studies that used outcome measurement tools that were not validated. There were no overall issues with inconsistency, indirectness, imprecision, or publication bias. The overall rating of the quality of the body of evidence is low quality.
Practice Recommendations
The following recommendations were based on the evidence, clinical expertise, and recognized patients' preferences and values.18 Although the quality of evidence was defined as low per the GRADE criteria, the practice recommendations developed were categorized as strong recommendations because the benefits of applying these recommendations into practice outweigh the risks or harms, there are minimal undesirable consequences expected, and these recommendations are believed to apply to the majority of adolescents undergoing cancer therapy.31
There is a strong recommendation that providers display honesty, humor, professional expertise, respect, trustworthiness, reassurance, support, and empathy as a means to facilitate communication with the adolescent with cancer.
There is a strong recommendation that providers promote open communication with the adolescent with cancer by allowing time for discussion and repeated questions, talking directly to the adolescent, using specific, clear, unambiguous language, and assessing the adolescent's desire to receive information.
There is a strong recommendation for providers to explore symptom expectations and provide symptom education for the adolescent with cancer.
There is a strong recommendation that providers establish rapport with the adolescent with cancer by listening, demonstrating genuine concern, and being trustworthy, to facilitate symptom and general communication.
There is a strong recommendation that providers foster a nonjudgmental environment that allows the adolescent with cancer to communicate symptoms and health-related concerns.
Discussion
To our knowledge, this is the first systematic review of the literature aimed at exploring factors that contribute to adolescents' willingness to communicate with their HCPs regarding cancer treatment and related symptoms. Overall, there is limited published evidence that directly relates to adolescents' willingness to communicate symptoms, and future research should be conducted to address this gap. The practice recommendations are based on evidence from 11 qualitative studies that gathered findings from semistructured interviews, 1 questionnaire, and 1 online focus group. The themes were categorized by critical analysis of the existing evidence. The practice recommendations were then developed through consensus process that considered the evidence and clinical expertise while incorporating patient and family preferences when possible.
As soon as possible after the cancer diagnosis, providers should communicate with adolescents about what symptoms they can expect to experience, and the importance of open communication and early symptom reporting. Using these initial meetings to communicate in a direct and open manner can establish trust and set expectations for ongoing dialogue that decreases the likelihood that the adolescent will be reluctant to communicate when the need to report symptoms arises.
Developing an understanding of the adolescent's goals and interests will guide the focus of symptom assessment and management.32 For example, if an adolescent's goal is to go to school, then addressing fatigue might be most important; and if another adolescent's goal is to participate in horseback riding, then addressing lower extremity weakness might be most important. When symptoms are not reported, the provider is unable to provide optimal management. With detailed symptom education and management throughout treatment, adolescents can learn the importance of communicating symptoms as they recognize the benefits of optimal supportive care.
Adolescents are often unable to describe how they feel by referring to just one symptom; how they feel usually involves a combination of symptoms.33 Likert-type symptom scales, such as a 1–10 scale to report pain, do not offer the opportunity to fully express symptom experiences.16 Rather, providers should encourage narrative symptom questions, such as “what does it feel like to have…” instead of “what level is your pain?”16 This allows the adolescent to discuss symptom experiences as a combination of symptoms rather than focusing on individual symptoms. In addition, providers should use ordinary words and lay expressions to describe symptoms.34 The adolescent's understanding of symptoms can be used as a point of communication, and providers should gain detailed insight into their level of understanding through thorough questioning.34 Exploring nonlanguage-based alternatives to communication, such as art or drawing, may be helpful for some adolescents.35
Parents often take the lead in communicating with HCPs, but many adolescents appreciate active involvement in medical communication.27 Provider communication practices, such as involving the adolescent in the discussion, contribute to the adolescent's willingness to communicate.22–25,27,29,30 It is imperative that providers read patient cues and assess whether the adolescent is feeling overwhelmed by medical information, versus desiring more information but not having the ability to formulate a specific question.22,24 Excluding adolescents from discussions that include medical information negatively impacts their overall willingness to communicate with providers and may foster resentment.36 When excluded from information-sharing sessions, left with unanswered questions, or unable to identify a reliable person with whom to communicate, adolescents may resort to alternative sources of information that are less reliable, such as friends or the internet.22 A limitation of this systematic review is the low-quality research (i.e., descriptive studies with small sample sizes) available in this area. Higher quality evidence from randomized controlled trials was not available. Further research around adolescent cancer patient communication, specifically factors that impact the communication of disease- and treatment-related symptoms, is needed to discover barriers and facilitators that remain unknown at this time. The findings identified in this systematic review may be generalized to broader definitions of adolescence and young adulthood (i.e., 15–39 years old) and other chronic disease groups.
Effective communication between adolescents and their HCPs is essential to building and maintaining a relationship that impacts an adolescents' willingness to communicate. Recommendations from this systematic review are based on the evidence from the literature that identified potential barriers as well as facilitators to support communication and ultimately improve symptom-related communication. Knowledge of factors that affect communication of symptoms may assist the provider in preventing symptom-related distress, achieving satisfactory care, and maintaining optimal quality of life in adolescents with cancer.16,34
Acknowledgments
The authors thank medical librarians Jamie Conklin, MLIS, and Virginia Carden, MS, AHIP, for their literature search and EndNote assistance of this article. The authors also thank Marilyn Hockenberry, PhD, and Wendy Landier, PhD, for their guidance with the final edits of the article. This project was supported by the National Cancer Institute/National Clinical Trials Network Group Operations Center Grant (U10CA180886; PI-Adamson).
Author Disclosure Statement
No competing financial interests exist.
References
- 1. D'Agostino NM, Penney A, Zebrack B. Providing developmentally appropriate psychosocial care to adolescent and young adult cancer survivors. Cancer. 2011;117(10 Suppl):2329–34 [DOI] [PubMed] [Google Scholar]
- 2. Belpame N, Kars MC, Beechman D, et al. “The AYA director”: a synthesizing concept to understand psychosocial experiences of adolescents and young adults with cancer. Cancer Nurs. 2016;39(4):292–302 [DOI] [PubMed] [Google Scholar]
- 3. Sowell ER, Peterson BS, Thompson PM, et al. Mapping cortical change across the human life span. Nat Neurosci. 2003;6(3):309–15 [DOI] [PubMed] [Google Scholar]
- 4. Ciccia AH, Meulenbroek P, Turkstra LS. Adolescent brain and cognitive developments. Top Lang Disord. 2009;29(3):249–65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bauer M. Language development in teens. 2015. Accessed June26, 2018 from: https://www.livestrong.com/article/226031-language-development-in-teenagers
- 6. Brand SR, Fasciano K, Mack JW. Communication preferences of pediatric cancer patients: talking about prognosis and their future life. Support Care Cancer. 2017;25(3):769–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Levetown M. Communicating with children and families: from everyday interactions to skill in conveying distressing information. Pediatrics. 2008;121(5):e1441–60 [DOI] [PubMed] [Google Scholar]
- 8. Feraco AM, Brand SR, Mack JW, et al. Communication skills training in pediatric oncology: moving beyond role modeling. Pediatr Blood Cancer. 2016;63(6):966–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Erikson EH. Childhood and society. New York: Norton; 1950 [Google Scholar]
- 10. National Cancer Institute. Cancer in children and adolescents. 2018. Accessed March30, 2018 from: https://www.cancer.gov/types/childhood-cancers/child-adolescent-cancers-fact-sheet
- 11. World Health Organization. Adolescent health. 2018. Accessed March30, 2018 from: www.who.int/topics/adolescent_health/en
- 12. Ruland CM, Hamilton GA, Schjødt-Osmo B. The complexity of symptoms and problems experienced in children with cancer: a review of the literature. J Pain Symptom Manage. 2009;37(3):403–18 [DOI] [PubMed] [Google Scholar]
- 13. Maeda K, Hasegawa D, Urayama KY, et al. Risk factors for psychological and psychosomatic symptoms among children with malignancies. J Paediatr Child Health. 2018;54(4):411–5 [DOI] [PubMed] [Google Scholar]
- 14. Woodgate RL, Degner LF. Expectations and beliefs about children's cancer symptoms: perspectives of children with cancer and their families. Oncol Nurs Forum. 2003;30(3):479–91 [DOI] [PubMed] [Google Scholar]
- 15. Woodgate RL. A different way of being: adolescents' experiences with cancer. Cancer Nurs. 2005;28(1):8–15 [DOI] [PubMed] [Google Scholar]
- 16. Woodgate RL. Feeling states: a new approach to understanding how children and adolescents with cancer experience symptoms. Cancer Nurs. 2008;31(3):229–38 [DOI] [PubMed] [Google Scholar]
- 17. Children's Oncology Group. Nursing Discipline. Evidence based practice. 2018. Accessed March30, 2018 from: www.childrensoncologygroup.org
- 18. Melnyk MB, Fineout-Overhold E. (Eds). Evidence-based practice in nursing & healthcare. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2015 [Google Scholar]
- 19. Garrard J. Health sciences literature review made easy: the matrix method. Boston: Jones & Bartlett; 2014 [Google Scholar]
- 20. Guyatt G, Oxman AD, Akl EA, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383–94 [DOI] [PubMed] [Google Scholar]
- 21. Ameringer S, Serlin RC, Hughes SH, et al. Concerns about pain management among adolescents with cancer: developing the adolescent barriers questionnaire. J Pediatr Oncol Nurs. 2006;23(4):220–32 [DOI] [PubMed] [Google Scholar]
- 22. Bahrami M, Namnabati M, Mokarian F, et al. Information-sharing challenges between adolescents with cancer, their parents and health care providers: a qualitative study. Support Care Cancer. 2017;25(5):1587–96 [DOI] [PubMed] [Google Scholar]
- 23. Dunsmore J, Quine S. Information, support, and decision-making needs and preferences of adolescents with cancer: implications for health professionals. J Psychosoc Oncol. 1996;13(4):39–56 [Google Scholar]
- 24. Gibson F, Aldiss S, Horstman M, et al. Children and young people's experiences of cancer care: a qualitative research study using participatory methods. Int J Nurs Stud. 2010;47(11):1397–407 [DOI] [PubMed] [Google Scholar]
- 25. Wangmo T, Ruhe KM, Badarau DO, et al. Parents' and patients' experiences with paediatric oncology care in Switzerland—satisfaction and some hurdles. Swiss Med Wkly. 2016;146:w14309. [DOI] [PubMed] [Google Scholar]
- 26. Weaver MS, Baker JN, Gattuso JS, et al. “Being a good patient” during times of illness as defined by adolescent patients with cancer. Cancer. 2016;122(14):2224–33 [DOI] [PubMed] [Google Scholar]
- 27. Ruhe KM, Badarau DO, Brazzola P, et al. Participation in pediatric oncology: views of child and adolescent patients. Psychooncology. 2016;25(9):1036–42 [DOI] [PubMed] [Google Scholar]
- 28. Anderzén Carlsson A, Sørlie V, Gustafsson K, et al. Fear in children with cancer: observations at an outpatient visit. J Child Health Care. 2008;12(3):191–208 [DOI] [PubMed] [Google Scholar]
- 29. Coyne I, Amory A, Gibson F, Kiernan G. Information-sharing between healthcare professionals, parents and children with cancer: more than a matter of information exchange. Eur J Cancer Care (Engl). 2016;25(1):141–56 [DOI] [PubMed] [Google Scholar]
- 30. Zwaanswijk M, Tates K, van Dulmen S, et al. Young patients', parents', and survivors' communication preferences in paediatric oncology: results of online focus groups. BMC Pediat. 2007;7:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Neumann I, Santesso N, Akl EA, et al. A guide for health professionals to interpret and use recommendations in guidelines developed with the GRADE approach. J Clin Epidemiol. 2016;72:45–55 [DOI] [PubMed] [Google Scholar]
- 32. Hedström M, Skolin I, von Essen L. Distressing and positive experiences and important aspects of care for adolescents treated for cancer. Adolescent and nurse perceptions. Eur J Oncol Nurs. 2004;8(1):6–17 [DOI] [PubMed] [Google Scholar]
- 33. Erickson JM, Macpherson CF, Ameringer S, et al. Symptoms and symptom clusters in adolescents receiving cancer treatment: a review of the literature. Int J Nurs Stud. 2013;50(6):847–69 [DOI] [PubMed] [Google Scholar]
- 34. Vatne TM, Slaughter L, Ruland CM. How children with cancer communicate and think about symptoms. J Pediatr Oncol Nurs. 2010;27(1):24–32 [DOI] [PubMed] [Google Scholar]
- 35. Rollins JA. Tell me about it: drawing as a communication tool for children with cancer. J Pediatr Oncol Nurs. 2005;22(4):203–21 [DOI] [PubMed] [Google Scholar]
- 36. Phillips-Salimi C. Young adult cancer survivors' experiences of connectedness with their healthcare providers [dissertation]. Indianapolis: Indiana University; 2009; 281 p [Google Scholar]