Abstract
Objective
The aim of this study was to investigate the relationship between the inflammatory parameters including neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) and the prognosis of idiopathic granulomatous mastitis (IGM).
Materials and methods
In this retrospective study, a total of 41 patients with IGM who had no malignant disease or inflammatory pathologies were included between January 2010 and December 2017. The patients were divided into two groups according to presence or absence of recurrence. Subsequently, the relationship between patient characteristics, pre- and postoperative NLR and PLR levels and disease recurrence were evaluated.
Results
With a mean follow-up period of 28.4 months, 19.5% of patients were found to have recurrent IGM. Age, body mass index, patient characteristics such as oral contraceptive use, smoking status, and family history, surgical treatment and postoperative NLR, preoperative PLR, and postoperative PLR were not statistically significant between groups. However, only preoperative NLR was significantly associated with a recurrent IGM (p=0.024). Preoperative NLR predicted recurrence with a sensitivity of 62.5% and specificity of 84.8%.
Conclusion
These results demonstrated that a high level of NLR was predictive of poor outcome in patients with IGM.
Keywords: Granulomatous mastitis, neutrophils, platelets, ratios
Introduction
Idiopathic granulomatous mastitis (IGM) is a rare chronic inflammatory disease of breast. It is a difficult entity for both clinicians and patients due to its diagnosis, prognosis, and related complications (1, 2). Although IGM is a histopathologically benign disease, its complications such as fistulas and recurrences make the disease behave like a malignant entity (3, 4). Its etiology remains unknown; however, some associate it with tuberculosis, sarcoidosis, mycotic or parasitic infections, local irritants, and autoimmune process (2, 4). There are case series in the literature from all over the world, mostly being reported in the Eastern countries, although there is no epidemiological evidence (3, 5, 6). Additionally, there is a still controversy in the diagnosis due to its clinical and radiological similarity to the malignant breast tumors (1, 2, 4, 6).
Idiopathic granulomatous mastitis can be diagnosed through biopsy, including fine-needle aspiration, core or excisional biopsy; and excisional biopsy is commonly reported superior to identify the presence or absence of malignancy (1, 3). Although there is no established marker for the recurrence of IGM, the most common factor and the main etiology is the failure in excision margins. The main treatment modality is surgery, and drug therapies have been still investigated including anti-inflammatory agents, corticosteroids, and antibiotics to treat the primary disease and prevent recurrences (1–3, 5). Recurrence may be observed at the rate of 5% to 50% despite wide surgical excision of IGM (7). Although IGM is a chronic and recurrent disease, there is an obvious lack of knowledge regarding its recurrence.
In the present study, we aimed to investigate the relationship between the inflammatory parameters including neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) and the prognosis of IGM.
Materials and Methods
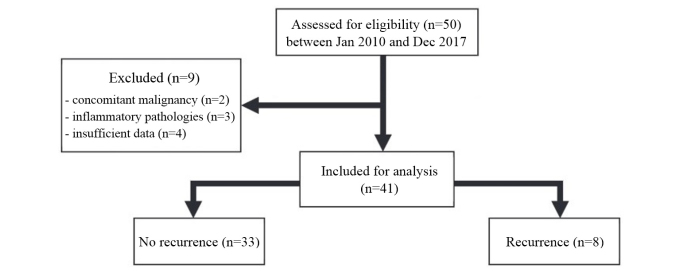
In this retrospective study, a total of 50 patients’ medical records were collected from two centers in Ankara, Turkey between January 2010 and December 2017. Nine patients were excluded from the study due to concomitant malignancy, inflammatory pathologies such as infections, fat necrosis, and foreign body reactions, or insufficient data (Figure 1). The study was carried out in accordance with the 1964 Helsinki Declaration and its later amendments. Informed consent was not required because of the retrospective nature of the study.
Figure 1.
Flow diagram of recruitment and procedure
All of the patients underwent a clinical breast examination and an ultrasound examination of the affected breast; mammographic examination was performed as needed. Definitive diagnosis was obtained by fine-needle aspiration biopsy, core needle biopsy, or surgical excision. The pathological criteria for the diagnosis of IGM were presence of non-caseous granulomatous inflammation on breast lobule. All patients underwent a surgical excision of the lesion, based on the physical examination and ultrasound findings.
The main outcome of this study was recurrence of IGM. All patients were divided into two groups according to presence or absence of disease. Data on demographic features, patient characteristics, pertinent family history of IGM, diagnosis strategies, pre- and postoperative NLR and PLR levels, and clinical outcomes was garnered from the hospital database. Information about height and weight based on the patients’ own statement in the preoperative period were also obtained from the database. The return of inflammatory signs, skin changes, and symptoms after a remission was accepted as recurrence. While preoperative parameters were measured before the surgical procedure, postoperative parameters were measured just before discharge.
Blood sample analysis
Platelet, lymphocyte, and neutrophil counts were measured as part of the automated complete blood cell count using a Coulter LH 750 hematology analyzer (Beckman Coulter, Fullerton, CA, USA). The measurements were performed using the similar technique in both centers. In addition, there was no change in the measurement process and the devices used during the study period. NLR was calculated by dividing the absolute neutrophil count by the absolute lymphocyte count and PLR was calculated by dividing the absolute platelets by the absolute lymphocytes.
Statistical Analysis
Data were expressed as mean ± standard deviation for continuous variables and frequency for categorical variables. The Shapiro-Wilk test was used to ensure the normality of the data. Numerical data were analyzed using Student’s t-test for normally disturbed variables or Mann-Whitney U test for non-normally distributed continuous variables. Two-tailed chi-square or Fisher’s exact tests were used where appropriate to compare categorical variables. Receiver-operating characteristic (ROC) curve analysis was used to determine the optimal cut-off value of the preoperative NLR to predict recurrent disease. p value of <0.05 was considered statistically significant. All statistical analyses were performed using Statistical Package for the Social Sciences version 16.0 for Windows (SPSS Inc.; Chicago, IL, USA).
Results
The study included 41 female patients. The age ranged from 20 to 55 years (mean, 35.0±7.3 years). The mean follow-up was 28.4±10.1 months. 12.2% of patients were unmarried; the others were (87.8%) married. The vast majority of the patients (85.4%) gave a history of breastfeeding for 6 months or more. All patients, except two, were premenopausal. The mean BMI was 30.9±5.4 kg/m2. Of the 41 patients, 7 (17.1%) had a history of oral contraceptive use, 12 (29.3%) had a history of cigarette smoking. Only 4.9% of the cases were bilateral. The demographics and clinical characteristics of enrolled patients are detailed in Table 1.
Table 1.
The demographic and clinical characteristics of the study population (n=41)
| Variables | |
|---|---|
| Age (years) | 35.0±7.3 |
| Follow-up (month) | 28.4±10.1 |
| BMI (kg/m2) | 30.9±5.4 |
| Marital status, n (%) | |
| Unmarried | 4 (12.2%) |
| Married | 37 (87.8%) |
| Breastfeeding status, n (%) | |
| No | 6 (14.6%) |
| Yes | 35 (85.4%) |
| Menopausal status, n (%) | |
| Premenopausal | 39 (95.1%) |
| Postmenopausal | 2 (4.9%) |
| Oral contraceptive use, n (%) | 7 (17.1%) |
| Cigarette smoking habits, n (%) | 12 (29.3%) |
| Family history of IGM, n (%) | 4 (9.8%) |
| Localization of the disease, n (%) | |
| Unilateral | 39 (95.1%) |
| Bilateral | 2 (4.9%) |
| Pathological diagnosis, n (%) | |
| Fine-needle aspiration biopsy | 5 (12.2%) |
| Core needle biopsy | 25 (61.0%) |
| Surgical excision | 11 (26.8%) |
| Recurrence, n (%) | 8 (19.5%) |
IGM: idiopathic granulomatous mastitis; BMI: body mass index
The recurrence rate of IGM was 19.5% at one-year follow-up. Age (p=0.594), follow-up (p=0.306), BMI (p=0.672), and patient characteristics such as marital status (p=0.596), breastfeeding (p=0.331), oral contraceptive use (p=0.416), smoking habits (p=0.158), family history (p = 0.596), or localization of the disease (p=0.356) were not statistically significant between patients with recurrence and those with no recurrence. Regarding inflammatory parameters, postoperative NLR, preoperative PLR, and postoperative PLR were not also found to be statistically significant between groups. However, patients with recurrence of IGM had significantly higher preoperative NLR (7.1±4.5 vs. 3.3±1.4) compared to others (p=0.024) (Table 2).
Table 2.
Comparison of the findings in patients with non-recurrent and recurrent IGM
| Parameters | No recurrence (n=33) | Recurrence (n=8) | p |
|---|---|---|---|
| Age (years) | 34.6±7.4 | 36.7±7.6 | 0.594 |
| Follow-up (month) | 27.8±10.3 | 30.8±9.5 | 0.306 |
| BMI (kg/m2) | 30.7±5.5 | 31.7±5.7 | 0.672 |
| Patient characteristics | |||
| Married | 30 (90.9%) | 7 (87.5%) | 0.596 |
| Breastfeeding | 29 (87.9%) | 6 (75.0%) | 0.331 |
| Oral contraceptive use | 5 (15.2%) | 2 (25%) | 0.416 |
| Smoking | 8 (24.2%) | 4 (50.0%) | 0.158 |
| Positive family history | 3 (9.1%) | 1 (12.5%) | 0.596 |
| Bilateral IGM | 1 (3.0%) | 1 (12.5%) | 0.356 |
| Preoperative NLR | 3.3±1.4 | 7.1±4.5 | 0.024 |
| Postoperative NLR | 3.3±3.7 | 2.8±0.8 | 0.778 |
| Preoperative PLR | 160.0±58.7 | 174.2±41.1 | 0.642 |
| Postoperative PLR | 156.1±46.4 | 149.7±30.3 | 0.628 |
BMI: body mass index; IGM: idiopathic granulomatous mastitis; NLR: neutrophil-to-lymphocyte ratio; PLR: platelet-to-lymphocyte ratio
The ROC curves of preoperative NLR were found to be associated with IGM recurrence. The area under curve (AUC) for the preoperative NLR was 0.76 (95% CI 0.55–0.97; p=0.024). Using a cut-off value of 5.02, the preoperative NLR predicted recurrence with a sensitivity of 62.5% and specificity of 84.8%. When the study population was divided into 2 groups using a cut-off value of 5.02, the odds ratio (OR) of patients with an NLR greater than 5.02 was calculated as 9.3 (95% CI 1.67–52.06; p=0.013) (Figure 2).
Figure 2.
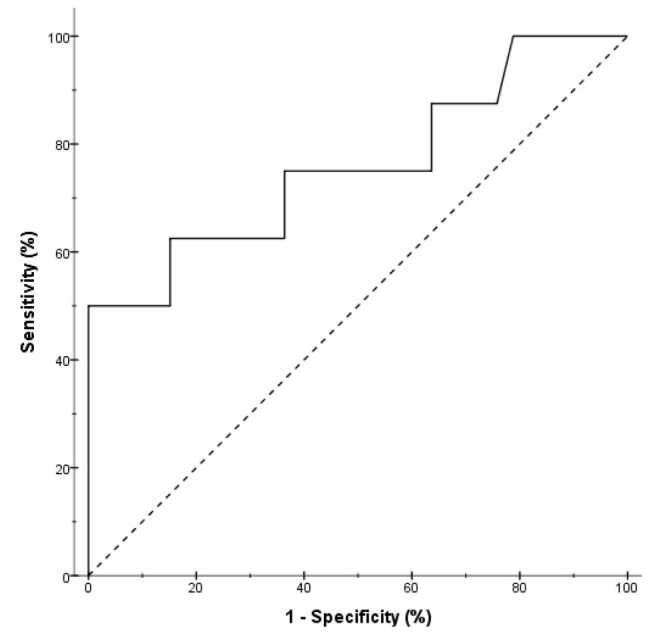
The receiver-operating characteristic (ROC) curve analysis of preoperative neutrophil to lymphocyte ratio for recurrence prediction
Discussion and Conclusion
Idiopathic granulomatous mastitis is a histopathologically benign disease, although it is associated with recurrences and complications such as fistulation, ulceration, and delayed wound healing (1–3). It is a clinically chronic inflammatory disease of the breast of unclear etiology (2–7). Granulomatous mastitis is referred as ‘idiopathic’ when no etiologic explanation can be found after an appropriate and complete diagnostic evaluation. Therefore, other possible causes of granulomatous lesions, such as infections, systemic disorders, foreign body reaction, and fat necrosis must be excluded (1, 5). To-date, there is no consensus or guideline on the ideal treatment approach for patients with IGM. Several different treatment modalities are used for IGM, including antibiotic therapy, systemic or topical steroids, anti-inflammatory agents, surgical excision, and mastectomy (2, 4–8). Recurrence rates vary according to the treatment strategy, patient specific factors, and duration of follow-up. It is reported up to 50% despite wide surgical excision and even complete resolution (5–8).
In present study, 41 patients with IGM were evaluated with a mean follow-up time of 28.4 months. The follow-up periods were almost same in both groups. The mean age of the patients was 35 years, and only two patients were postmenopausal, which is consistent with the previous findings (4–7). Our recurrence rate of 19.5% is also comparable to the reported rates (5–7). We think that this low recurrence rate is probably due to the fact that all patients were treated with the surgical removal of the lesions. A systemic review and meta-analysis by Lei et al. (8) revealed that complete remission rate of oral steroids (71.8%) was much lower than that of surgical managements (90.6%) and oral steroids plus surgical managements (94.5%). It was also reported that the recovery period of steroids was much longer when compared to surgical excision (8).
Idiopathic granulomatous mastitis is an inflammatory disease with high rates of recurrence which usually makes it difficult to follow and evaluate the results of surgical treatment. Various clinical, patients-related, and treatment-related factors may influence the prognosis of IGM. In a recent study by Yılmaz et al. (9), the mean number of births, duration of lactation, BMI, presence of fistulas, presence of abscess formation, and luminal inflammation were found to be significantly different between patients with recurrence and those with no recurrence. In addition, they developed a scoring system to predict IGM recurrence risk using clinical, radiological, and pathological factors. However, to date, there is no established marker for IGM to predict recurrence. This study compared the pre- and postoperative NLR and PLR levels of patients with and without recurrence. Moreover, several patient characteristics were compared between the groups. Age, BMI, breastfeeding, oral contraceptive use, smoking habits, family history, or localization of the disease were not found to be statistically significant between patients with recurrence and those with no recurrence; unlike other studies, which found an association between BMI (9), breastfeeding (6), or smoking (4, 6) and IGM recurrence. Regarding inflammatory parameters, the mean preoperative serum NLR level was significantly higher in patients with recurrence than in those without recurrence.
Neutrophil-to-lymphocyte ratio and PLR are found to be associated with inflammatory response and disease activity in a variety of autoimmune diseases and have been considered as the indicators of representing the severity of inflammation (10). Today, these parameters are being increasingly used as a prognostic marker for predicting prognosis of several diseases, and cancers (10–12). In a study, Pan et al. (10) demonstrated that NLR and PLR had positive correlation with disease activity in patients with Takayasu’s arteritis. In a systematic review and meta-analysis, Zheng al. (13) concluded that an increased pretreatment NLR or PLR significantly associated with poor outcomes for patients with hepatocellular carcinoma. Another systematic review and meta-analysis by Ethier et al. (14) revealed that high NLR was associated with an adverse overall survival and disease-free survival in patients with breast cancer. In the present study, increased preoperative NLR (cut-off value of 5.02) predicted IGM recurrence. Therefore, this simple marker can be used for the follow-up of the patients and be evaluated as a recurrence predictor. However, a similar association was not found for pre- or postoperative PLR levels.
A number of important limitations need to be considered. First, this study has a relatively low number of cases in both groups. In addition, there is no standard definition of recurrence or remission of IGM (8); thus, different definitions may lead to strikingly different conclusion. Considering that some authors suggest that IGM is an autoimmune process (2, 7), the relatively short follow-up period may be another limitation. Also, it was not evaluated whether the IGM lesions were unifocal or multifocal and the size of the lesions. Lastly, there are inherent selection biases that confound any retrospective cohort. Despite these limitations, it is the first study that focused on the prognostic values of NLR and PLR levels measured pre- and postoperatively in patients IGM treated with the surgical removal of the lesions.
Clinicians commonly use complete blood count in their daily practice particularly in inflammatory conditions and following the treatment responses. The use of NLR seems simple, cost-effective, and promising indicator of the prognosis and recurrence of IGM, which is a challenging disease for both clinicians and patients. However, PLR is not associated with the outcomes for patients with IGM.
Footnotes
Ethics Committee Approval: Authors declared that the research was conducted according to the principles of the World Medical Association Declaration of Helsinki “Ethical Principles for Medical Research Involving Human Subjects” (amended in October 2013).
Informed Consent: Informed consent was not received due to the retrospective nature of the study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - S.G.T., A.E.; Design - Ö.A.Ç., S.U.Ç., S.G.T.; Supervision - Ö.A.Ç., S.U.Ç.; Resources - Ö.A.Ç., S.U.Ç., S.G.T.; Materials - Ö.A.Ç., S.U.Ç., S.G.T.; Data Collection and/or Processing - Ö.A.Ç., S.U.Ç.; Analysis and/or Interpretation - S.U.Ç., S.G.T., A.E.; Literature Search - Ö.A.Ç., S.U.Ç.; Writing Manuscript - Ö.A.Ç., S.U.Ç., S.G.T.; Critical Review - S.G.T., A.E.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Kayahan M, Kadioglu H, Muslumanoglu M. Management of patients with granulomatous mastitis: analysis of 31 cases. Breast Care. 2012;7:226–230. doi: 10.1159/000337758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ozel L, Unal A, Unal E, Kara M, Erdoğdu E, Krand O, Güneş P, Karagül H, Demiral S, Titiz MI. Granulomatous mastitis: is it an autoimmune disease? Diagnostic and therapeutic dilemmas. Surg Today. 2012;42:729–733. doi: 10.1007/s00595-011-0046-z. [DOI] [PubMed] [Google Scholar]
- 3.Asoglu O, Ozmen V, Karanlik H, Tunaci M, Cabioglu N, Igci A, Selcuk UE, Kecer M. Feasibility of surgical management in patients with granulomatous mastitis. Breast J. 2005;11:108–114. doi: 10.1111/j.1075-122X.2005.21576.x. [DOI] [PubMed] [Google Scholar]
- 4.Co M, Cheng VCC, Wei J, Wong SCY, Chan SMS, Shek T, Kwong A. Idiopathic granulomatous mastitis: a 10-year study from a multicentre clinical database. Pathology. 2018;50:742–747. doi: 10.1016/j.pathol.2018.08.010. [DOI] [PubMed] [Google Scholar]
- 5.Kok KY, Telisinghe PU. Granulomatous mastitis: presentation, treatment and outcome in 43 patients. Surgeon. 2010;8:197–201. doi: 10.1016/j.surge.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 6.Uysal E, Soran A, Sezgin E. Factors related to recurrence of idiopathic granulomatous mastitis: what do we learn from a multicentre study? ANZ J Surg. 2018;88:635–639. doi: 10.1111/ans.14115. [DOI] [PubMed] [Google Scholar]
- 7.Aghajanzadeh M, Hassanzadeh R, Alizadeh Sefat S, Alavi A, Hemmati H, Esmaeili Delshad MS, Emir Alavi C, Rimaz S, Geranmayeh S, Najafi Ashtiani M, Habibzadeh SM, Rasam K, Massahniya S. Granulomatous mastitis: presentations, diagnosis, treatment and outcome in 206 patients from the north of Iran. Breast. 2015;24:456–460. doi: 10.1016/j.breast.2015.04.003. [DOI] [PubMed] [Google Scholar]
- 8.Lei X, Chen K, Zhu L, Song E, Su F, Li S. Treatments for idiopathic granulomatous mastitis: systematic review and meta-analysis. Breastfeed Med. 2017;12:415–421. doi: 10.1089/bfm.2017.0030. [DOI] [PubMed] [Google Scholar]
- 9.Yılmaz TU, Gürel B, Güler SA, Baran MA, Erşan B, Duman S, Utkan Z. Scoring idiopathic granulomatous mastitis: an effective system for predicting recurrence? Eur J Breast Health. 2018;14:112–116. doi: 10.5152/ejbh.2018.3709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pan L, Du J, Li T, Liao H. Platelet-to-lymphocyte ratio and neutrophil-to-lymphocyte ratio associated with disease activity in patients with Takayasu’s arteritis: a case-control study. BMJ Open. 2017;7:e014451. doi: 10.1136/bmjopen-2016-014451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ma Y, Mao Y, He X, Sun Y, Huang S, Qiu J. The values of neutrophil to lymphocyte ratio and platelet to lymphocyte ratio in predicting 30 day mortality in patients with acute pulmonary embolism. BMC Cardiovasc Disord. 2016;16:123. doi: 10.1186/s12872-016-0304-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee JS, Kim NY, Na SH, Youn YH, Shin CS. Reference values of neutrophil-lymphocyte ratio, lymphocyte-monocyte ratio, platelet-lymphocyte ratio, and mean platelet volume in healthy adults in South Korea. Medicine. 2018;97:e11138. doi: 10.1097/MD.0000000000011138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zheng J, Cai J, Li H, Zeng K, He L, Fu H, Zhang J, Chen L, Yao J, Zhang Y, Yang Y. Neutrophil to lymphocyte ratio and platelet to lymphocyte ratio as prognostic predictors for hepatocellular carcinoma patients with various treatments: a meta-analysis and systematic review. Cell Physiol Biochem. 2017;44:967–981. doi: 10.1159/000485396. [DOI] [PubMed] [Google Scholar]
- 14.Ethier JL, Desautels D, Templeton A, Shah PS, Amir E. Prognostic role of neutrophil-to-lymphocyte ratio in breast cancer: a systematic review and meta-analysis. Breast Cancer Res. 2017;19:2. doi: 10.1186/s13058-016-0794-1. [DOI] [PMC free article] [PubMed] [Google Scholar]