Abstract
Background
Pervasive misperceptions about nicotine may influence uptake of quit smoking aids and the impact of policies addressing nicotine as a tobacco product constituent.
Methods
Latent class analyses were conducted using four items on nicotine beliefs asked of 4037 adults aged 18–40 in wave 9 (February–March 2016) of the Truth Initiative Young Adult Cohort Study. Confirmatory factor analyses identified three factors from 12 items: nicotine susceptibility (NSUS), nicotine severity (NSEV), and tobacco severity (TSEV). Analyses assessed correlations between latent classes, sociodemographics, and nicotine/tobacco factor scores.
Results
A four-class model of nicotine beliefs was the best fit, with the largest class believing that nicotine plays a major part in smoking risks (class 1, n = 2070; 52%). Class 2 shared that belief but also responded “Don’t know” to addiction questions (class 2, n = 382; 11%). Fewer belonged in class 3, who reported that nicotine plays a small part in health risks (n = 1277; 30%), and class 4, who perceived nicotine as not cancer causing (n = 308; 7%). Latent class membership was correlated with sociodemographics, peer smoking, and past 30-day tobacco use. Classes 1 and 2 had similar NSUS scores and classes 3 and 4 had similar NSEV and TSEV scores.
Discussion
Differences in the perceptions of nicotine and tobacco-related harms can be partially explained by clustering of underlying nicotine beliefs. These classes of beliefs are correlated with sociodemographic predictors of smoking. These findings may help to identify specific beliefs or groups to be targeted by public education efforts on nicotine.
Implications
The current study supports that underlying nicotine beliefs are associated with perceived harms of specific nicotine and tobacco products (relative to cigarettes), with greater false beliefs about nicotine correlated with greater perceived susceptibility to nicotine addiction. Two important inferences emerge from this study: first, that education to address nicotine beliefs may also reframe perceptions of the harms of nicotine and tobacco products; and second, that this type of education may differentially impact perceptions of the harms of nicotine products (e.g., nicotine replacement therapy and e-cigarettes) and tobacco products (e.g., cigars, smokeless, and hookah).
Introduction
In March 2018, the US Food and Drug Administration (FDA) issued an Advance Notice of Proposed Rulemaking (ANPRM) to “obtain information for consideration in developing a tobacco product standard to set the maximum nicotine level for cigarettes.” In this ANPRM, FDA highlights that tobacco-related harms ultimately result from addiction to the nicotine in tobacco products. However, it is primarily exposure to the toxicants in tobacco smoke, not nicotine itself, that causes premature morbidity and mortality from tobacco use.1–5
To date, many studies report on the perceived harms of tobacco products, but few recent population studies address the perceived harms of nicotine itself. A 2013–2014-study of US adults highlighted discrepancies between current scientific evidence and public perceptions of relative risks of using e-cigarettes and smokeless tobacco and smoking hookah compared to smoking cigarettes.6 Recent research also shows that the proportion of US adults who perceive that e-cigarettes are less harmful than cigarettes has declined since 2010.7,8 Misperceptions among young people have also been documented,9,10 including a latent class analysis using three items on harm perceptions of cigarette smoking in the 2012 National Youth Tobacco Survey.11 This study revealed three classes of US youth: (1) those with consistently high perceptions of cigarette harms; (2) those with consistently low perceptions of cigarette harms; and (3) those who perceive cigarette harm as dose dependent.11 Current cigarette users were most prevalent in the “consistently low” class.
A few population-level studies to date also suggest that the general public overestimates the harms of nicotine12,13 or conflates the harms of nicotine with the harms of cigarette smoking.14 One of these studies presented data from 19 items on nicotine and nicotine product perceptions, including addictiveness and health harms, in a national sample of US young adults aged 18–40 participating in the Truth Initiative Young Adult Cohort Study.13 Results revealed young adults’ widespread misperceptions equating the risks of nicotine, nicotine replacement therapy (NRT) products, and e-cigarettes with cigarettes and greater misperceptions of the health risks of nicotine in females, Blacks, Hispanics, and those with less than some college education.13 The goal of the current study is to extend analyses in this sample, characterizing young adult subgroups based on their nicotine beliefs using latent class analysis. The use of latent class analysis can be an important tool in risk perception research to identify patterns and subgroups of people with similar beliefs that can be used to inform the need for and development of targeted messages or other interventions.11,15 In line with the earlier study in adolescents,11 we hypothesized that three meaningful latent classes would emerge: perceptions of high harms from nicotine (class 1); mixed perceptions of nicotine (class 2); and perceptions of low harms from nicotine (class 3). We expected that tobacco users would be more prevalent in the latter class. Additionally, we examined whether latent classes developed from nicotine beliefs were correlated with specific perceptions of the addictiveness and health harms of nicotine and tobacco products relative to cigarettes.
Methods
The current study leverages data from 4100 respondents aged 18–40 in wave 9 of the Truth Initiative Young Adult Cohort Study (YA Cohort; February–March 2016). The detailed methods of this study have been described elsewhere.16 The cohort was comprised of a nationally representative sample of young adults ages 18–34 at study entry drawn from GfK’s KnowledgePanel, which is recruited via address-based sampling to provide a statistically valid representation of the US population, including cell phone-only households. The survey was administered online in English and Spanish. The cohort was refreshed at each wave to retain the initial sample size. The panel recruitment rate was 13.2% for wave 9.17 In 63.9% of the identified households, one member completed a core profile survey in which key demographic information was collected (profile rate). At each wave, only one panel member per household was selected at random to be part of the study sample, and no members outside the panel were recruited. The completion rate was 60.7% and the cumulative response rate (a product of these three rates) was 5.1%.18 This study was approved by the Chesapeake Institutional Review Board, Inc (Protocol #20036020; now Advarra). Online consent was collected from participants before survey self-administration.
Latent Class Model of Nicotine Beliefs
Four items addressing nicotine beliefs were included in latent class models informed by available study measures and discussion among the study authors. Three items assessed nicotine’s role in causing disease (ie, “Nicotine is a cause of cancer”; “According to you, how large a part of the health risks of cigarette smoking comes from the nicotine itself?”; and “According to you, how large a part of the cancer caused by cigarette smoking comes from the nicotine itself?”), while the fourth evaluated the relationship between nicotine and addiction (“The claim that a cigarette brand is low in nicotine means that it is less addictive”).
Latent class analyses were conducted in 2018 using Mplus 8.1 (www.statmodel.com) to identify subgroups of young adults based on beliefs about the health effects of nicotine. Full information maximum likelihood estimation (FIML) was used based on the assumption that the probability of missingness may depend on data that are observed.19 The optimal number of classes was determined by running models with a successive number of classes from two to five and comparing model fit indices, the odds of correct classification (OCC),20 entropy, and interpretability. Model fit indices included the log likelihood (−2 LL), the Akaike Information Criterion, the Bayesian Information Criterion (BIC),21 and the sample-size-adjusted BIC, as well as Pearson and likelihood ratio chi-square statistics, and the Lo–Mendell–Rubin and Vuong–Lo–Mendell–Rubin likelihood ratio tests.22
Perceived Harms of Nicotine and Tobacco Products
Additionally we sought to explore whether latent classes developed from nicotine beliefs were correlated with specific perceptions of the addictiveness and health harms of nicotine and tobacco products relative to cigarettes. Rosenstock’s Health Belief Model23 provided the underlying conceptual framework of the way individual perceptions influence health behavior, supported empirically in evidence reviews and meta-analyses.24–26 We posited that perceived harms of nicotine and tobacco products would be differentiated as perceived susceptibility to nicotine-related harms (NSUS), perceived susceptibility to tobacco-related harms (TSUS), perceived severity of nicotine-related harms (NSEV), and perceived severity of tobacco-related harms (TSEV). A priori, we classified 12 items related to nicotine and tobacco harm perceptions in the survey based on three of these four constructs (NSUS, NSEV, and TSEV; Table 3); there were no items on TSUS in the wave 9 survey. All items asked about the perceived relative harm of nicotine products (ie, nicotine gum, nicotine patch, and e-cigarettes) or tobacco products (ie, cigars, pipe, little cigars/cigarillos, smokeless tobacco, and hookah) compared to “regular cigarettes” on a Likert scale. The five-point Likert scales were collapsed into three-point scales to make the responses scales more comparable; these were defined as ordinal data in the program, with the lowest scores indicating the lowest perceived harm and the highest scores, the highest perceived harm. NSUS items related to the likelihood of a product causing addiction, while NSEV and TSEV items related to the likelihood of a product causing health harm. Exploratory factor analysis supported the a priori categorization of items into the three factors (NSUS, NSEV, and TSEV), so confirmatory factor analysis (CFA) was conducted, with comparative fit index (CFI) and Tucker–Lewis index (TLI) used to determine model fit. Items involving the same product (eg, the three items asking about e-cigarettes) had their error terms correlated. In the optimal CFA model, both are greater than 0.95.27 Respondents who skipped more than 50% of the susceptibility and severity questions were dropped from the analyses (n = 109, 2.7%) and as in the latent class analysis, FIML was used to address missing responses for the remaining data.
Table 3.
Perceived harm of nicotine and tobacco by latent class
| Class 1 “Large role in health risks” (n = 2070; 52%) | Class 2 “Don’t Know; large role in health risks” (n = 382; 11%) | Class 3 “Small role in health risks” (n = 1277; 30%) | Class 4 “None/small part of cancer caused by nicotine” (n = 308; 7%) | p | |
|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||
| Factor 1—nicotine susceptibility | |||||
| Are nicotine patches more likely, about the same, or less likely to cause someone to become addicted as regular cigarettes? | 1.7 (0.6)a | 1.8 (0.5)a | 1.5 (0.6)b | 1.5 (0.6)b | <.0001 |
| Is nicotine gum more likely, about the same, or less likely to cause someone to become addicted as regular cigarettes? | 1.7 (0.6)a | 1.8 (0.5)a | 1.5 (0.6)b | 1.5 (0.6)b | <.0001 |
| Are electronic cigarettes (e-cigarettes) more likely, about the same, or less likely to cause someone to become addicted as regular cigarettes? | 1.9 (0.6) | 1.8 (0.5)a | 1.8 (0.6)a | 1.7 (0.6) | <.0001 |
| Are nicotine patches more likely, about the same, or less likely to cause someone to have a heart attack as cigarettes? | 1.8 (0.6)a | 1.8 (0.5)a | 1.5 (0.6) | 1.5 (0.6) | <.0001 |
| Are electronic cigarettes (e-cigarettes) more likely, about the same, or less likely to cause someone to have a heart attack as cigarettes? | 1.9 (0.6)a | 1.8 (0.5)a | 1.6 (0.6) | 1.6 (0.6) | <.0001 |
| Mean of factor items | 1.8 (0.5) a | 1.8 (0.5) a | 1.6 (0.4) | 1.5 (0.5) | <.0001 |
| Factor score | 0.139 a | 0.167 a | −0.171 | −0.267 | <.0001 |
| Factor 2—nicotine severity | |||||
| Relative harm to health: e-cigarettes vs. cigarettes | 1.9 (0.7) | 2.1 (0.7) | 1.5 (0.6)a | 1.5 (0.7)a | <.0001 |
| Relative harm to health: nicotine products vs. cigarettes | 1.8 (0.7) | 2.1 (0.7) | 1.4 (0.6)a | 1.4 (0.7)a | <.0001 |
| Mean of factor items | 1.8 (0.7) | 2.1 (0.6) | 1.5 (0.5) a | 1.5 (0.6) a | <.0001 |
| Factor score | 0.203 | 0.398 | −0.270 a | −0.298 a | <.0001 |
| Factor 3—tobacco severity | |||||
| Relative harm to health: cigars vs. cigarettes | 2.2 (0.6)a | 2.3 (0.6)a | 2.1 (0.7)b | 2.1 (0.7)b | <.0001 |
| Relative harm to health: pipe vs. cigarettes | 2.2 (0.6)a | 2.2 (0.6)a | 2.0 (0.7)b | 2.1 (0.7)b | <.0001 |
| Relative harm to health: little cigars/cigarillos vs. cigarettes | 2.2 (0.6)a | 2.3 (0.6)a | 2.1 (0.6)b | 2.1 (0.6)b | <.0001 |
| Relative harm to health: smokeless tobacco vs. cigarettes | 2.3 (0.6)a | 2.3 (0.6)a | 2.1 (0.6)b | 2.1 (0.7)b | <.0001 |
| Relative harm to health: hookah vs. cigarettes | 2.0 (0.7) | 2.2 (0.6) | 1.8 (0.7)a | 1.8 (0.7)a | <.0001 |
| Mean of factor items | 2.2 (0.5) | 2.3 (0.5) | 2.0 (0.4) a | 2.0 (0.5) a | <.0001 |
| Factor score | 0.131 | 0.261 | −0.201 a | −0.178 a | <.0001 |
Item-level missing data: 0.1–0.9%. Items that share a subscript (a or b) across rows do not differ from each other; there are significant pairwise differences in all other comparisons by class.
Correlates of Nicotine Beliefs
Age, gender, race/ethnicity, education, and household income were collected at each wave of the YA Cohort. We also included a validated measure of subjective financial status,28 given that young adults may not have finished their education or achieved a stable income. Based on primary socialization theory,29,30 we hypothesized that social influences, specifically peer and parent smoking, would be correlated with young adults’ perceptions of nicotine. Peer smoking was assessed by asking how many of one’s four closest friends smoke cigarettes and coded as 0 friends who smoke or 1+ friends who smoke. Parental smoking was assessed by asking at study entry whether one or both parents or guardians smoked cigarettes during the respondent’s childhood. Self-identified smoking status was also included, given that it is associated with smoking progression in adolescents31 and young adults32,33; the item asked “Which of the following best describes how you think of yourself?” with response choices of “smoker,” “social smoker,” “occasional smoker,” “ex-smoker,” “someone who tried smoking,” and “nonsmoker.” Categories were collapsed to “smoker,” “social/occasional smoker,” “ex-smoker/tried smoking” and “nonsmoker.” Participants were asked about past 30-day use (yes/no) of seven tobacco products including cigarettes, cigars (traditional cigars, little cigars/ cigarillos), electronic cigarettes (e-cigarettes), smokeless tobacco (chew, dip/snuff), and hookah.
Statistical Analyses
Bivariate analyses were used to describe the latent classes of nicotine beliefs based on responses to the four items in the model and to summarize the sociodemographic characteristics, social influences, and tobacco use behaviors by latent class, accounting for survey weighting using svy commands in Stata MP, Version 15 (www.stata.com). Variables identified as being correlated with latent class at p < .1 in the bivariate analyses were included in a multivariable multinomial logistic regression model to compare correlates of class membership. Age was retained in the multivariable model despite lack of significant correlation with nicotine beliefs and income was excluded from the model in favor of subjective financial status, given previous work by our group.28,34 Analyses comparing nicotine beliefs (latent class) and nicotine and tobacco harm perceptions (factor analysis) were unweighted. Mean response to each of the 12 items in the nicotine and tobacco harm perceptions factor analyses, as well as the mean of the factor items, and the factor scores were assessed by latent class to determine whether patterns of responses to the three factors were consistent with underlying nicotine beliefs. Separate analysis of variance models were run for each factor and Fisher’s least significant difference (LSD) test was used for all pairwise comparisons by latent class.
Results
The four-class solution was chosen as the best fitting latent class model, as it yielded entropy of 0.9, minimized BIC, and was interpretable. Table 1 presents the response patterns to the nicotine beliefs items by latent class. Of the four latent classes of nicotine beliefs, the largest class believed that nicotine causes cancer and plays a large part in smoking risks (class 1, n = 2070; 52%). Members of class 2 shared the belief about nicotine’s large part in causing smoking health harms with members of class 1 but expressed more uncertainty by responding “Don’t know” to the addiction question and the question about nicotine causing cancer (class 2, n = 382; 11%). Members of class 3 (n = 1277; 29%) and class 4 (n = 308; 7%) more accurately believed that nicotine plays no role or a small part in health risks but diverged on perceived cancer risk, with members of class 4 believing that none or a very small part of cancer was caused by nicotine and members of class 3 believing that a relatively small part of the cancer caused by smoking comes from the nicotine itself.
Table 1.
Response to nicotine belief items by latent class in adults aged 18–40 (n = 4037)
| Class 1 “Large role in health risks” (n = 2070; 52%) | Class 2 “Don’t Know; large role in health risks” (n = 382; 11%) | Class 3 “Small role in health risks” (n = 1277; 30%) | Class 4 “None/small part of cancer caused by nicotine” (n = 308; 7%) | Total (n = 4037) | p | |
|---|---|---|---|---|---|---|
| Weighted % | Weighted % | Weighted % | Weighted % | Weighted % | ||
| Nicotine is a cause of cancer. | <.001 | |||||
| True | 84.5 | 0.0 | 23.5 | 17.4 | 51.8 | |
| False | 6.5 | 0.0 | 43.5 | 54.6 | 20.2 | |
| Don’t know | 8.9 | 100.0 | 33.1 | 27.9 | 28.0 | |
| The claim that a cigarette brand is low in nicotine means that it is less addictive. | <.001 | |||||
| True | 15.2 | 0.0 | 23.2 | 21.6 | 16.3 | |
| False | 70.4 | 0.0 | 56.4 | 48.4 | 56.5 | |
| Don’t know | 14.4 | 100.0 | 20.4 | 30.0 | 27.3 | |
| According to you, how large a part of the health risks of cigarette smoking come from the nicotine itself? | <.001 | |||||
| None or a very small part | 0.8 | 1.3 | 2.7 | 54.7 | 5.5 | |
| A relatively small part | 3.2 | 5.0 | 80.1 | 36.8 | 28.7 | |
| A relatively large/very large part/all | 96.0 | 93.7 | 17.2 | 8.5 | 65.8 | |
| According to you, how large a part of the cancer caused by cigarette smoking comes from the nicotine itself? | <.001 | |||||
| None or a very small part | 0.0 | 0.8 | 0.0 | 100.0 | 7.7 | |
| A relatively small part | 3.6 | 8.1 | 96.0 | 0.0 | 31.1 | |
| A relatively large/very large part/all | 96.4 | 91.2 | 4.0 | 0.0 | 61.2 |
Latent class membership was correlated with sociodemographics, peer smoking, and past 30-day tobacco use (Table 2). Specifically, non-Hispanic Black (relative risk ratio [RRR] = 1.75), non-Hispanic “other” (RRR = 1.47), or Hispanic (RRR = 1.97) were more likely than Whites to be in class 1 than class 3. Females (vs. male; RRR = 1.37) and those with less than a college education (less than high school, RRR = 1.76; high school, RRR = 1.52) were also more likely to belong to class 1 than class 3. Compared to those “meeting needs with a little left,” those “living comfortably” (RRR = 0.74) were less likely to report being in class 1 than class 3. Similarly, participants who were non-Hispanic Black, non-Hispanic “other,” or Hispanic (vs. White) and those with less than a college education were more likely to be in class 2 compared to class 3. However, those with peers who smoke (RRR = 0.71) and who self-identify as an ex-smoker/someone who tried smoking versus nonsmoker (RRR = 0.55) were less likely to belong in class 2 than class 3. The only significant difference in characteristics of those in class 3 versus class 4 was that class 4 participants were less likely to be female (RRR = 0.72).
Table 2.
Correlates of nicotine beliefs latent classes, weighted percentages, and multinomial logistic regression model
| Class 1 “Large role in health risks” (n = 2070; 52%) | Class 2 “Don’t Know; large role in health risks” (n = 382; 11%) | Class 3 “Small role in health risks” (n = 1277; 30%) | Class 4 “None/small part of cancer caused by nicotine” (n = 308; 7%) | Total (n = 4037) | |||||
|---|---|---|---|---|---|---|---|---|---|
| Weighted % | Class 1 vs. Class 3 | Weighted % | Class 2 vs. Class 3 | Ref. | Weighted % | Class 4 vs. Class 3 | Weighted % | p | |
| RRR (95% CI)a | RRR (95% CI)a | Weighted % | RRR (95% CI)a | ||||||
| Age group | .521 | ||||||||
| 18–24 | 25.4 | 0.84 (0.65–1.07) | 22.4 | 0.72 (0.46–1.12) | 24.4 | 27.5 | 1.18 (0.74–1.86) | 24.9 | |
| 25–34 | 55.3 | 0.87 (0.70–1.08) | 60.4 | 0.99 (0.67–1.47) | 58.2 | 56.4 | 1.03 (0.68–1.55) | 56.8 | |
| 35–40 | 19.3 | Ref. | 17.2 | Ref. | 17.5 | 16.2 | Ref. | 18.3 | |
| Race/ethnicity | <.001 | ||||||||
| White, non-Hispanic | 53.5 | Ref. | 44.5 | Ref. | 69.0 | 61.6 | Ref. | 57.6 | |
| Black, non-Hispanic | 13.2 | 1.75 (1.26–2.42) | 19.9 | 2.99 (1.93–4.63) | 9.0 | 14.8 | 1.63 (0.90–2.95) | 12.9 | |
| Other, non-Hispanic | 8.9 | 1.47 (1.06–2.04) | 10.2 | 1.98 (1.20–3.28) | 7.9 | 6.5 | 0.91 (0.48–1.73) | 8.6 | |
| Hispanic | 24.5 | 1.97 (1.55–2.50) | 25.3 | 2.12 (1.45–3.09) | 14.0 | 17.1 | 1.30 (0.86–1.98) | 21.0 | |
| Sex | <.001 | ||||||||
| Male | 44.9 | Ref. | 46.0 | Ref. | 53.6 | 61.6 | Ref. | 48.8 | |
| Female | 55.1 | 1.37 (1.16–1.63) | 54.0 | 1.26 (0.95–1.67) | 46.4 | 38.4 | 0.72 (0.53–0.97) | 51.2 | |
| Education completed | <.001 | ||||||||
| Less than high school | 11.2 | 1.76 (1.16–2.70) | 15.4 | 3.20 (1.83–5.61) | 6.5 | 7.9 | 1.20 (0.54–2.71) | 10.1 | |
| High school | 26.3 | 1.52 (1.21–1.91) | 32.0 | 2.38 (1.70–3.34) | 19.7 | 26.8 | 1.39 (0.94–2.05) | 25.0 | |
| Some college or greater | 62.5 | Ref. | 52.6 | Ref. | 73.8 | 65.3 | Ref. | 64.9 | |
| Annual household income | <.001 | ||||||||
| Less than $10 000 | 12.7 | 19.1 | 7.1 | 15.4 | 12.0 | ||||
| $10 000–$24 999 | 16.3 | 19.0 | 15.4 | 13.2 | 16.1 | ||||
| $25 000–$49 999 | 27.3 | 28.0 | 23.6 | 26.9 | 26.3 | ||||
| $50 000–$99 999 | 29.7 | 24.2 | 36.0 | 30.3 | 31.0 | ||||
| More than $100 000 | 14.0 | 9.7 | 17.9 | 14.2 | 14.6 | ||||
| Subjective financial situation | <.001 | ||||||||
| Don’t meet basic expenses | 6.5 | 1.19 (0.78–1.83) | 10.6 | 1.73 (0.95–3.14) | 5.0 | 10.1 | 1.56 (0.81–2.99) | 6.8 | |
| Just meet basic expenses | 30.9 | 1.19 (0.96–1.48) | 28.8 | 1.09 (0.76–1.55) | 24.0 | 23.9 | 0.91 (0.60–1.36) | 28.1 | |
| Meet needs with a little left | 39.9 | Ref. | 38.1 | Ref. | 39.8 | 39.9 | Ref. | 39.7 | |
| Live comfortably | 22.7 | 0.74 (0.60–0.90) | 22.4 | 0.72 (0.51–1.03) | 31.1 | 26.1 | 0.84 (0.59–1.20) | 25.4 | |
| Peer cigarette smoking, 1+ vs. 0 | .033 | ||||||||
| 0 | 57.5 | Ref. | 62.4 | Ref. | 54.6 | 50.7 | Ref. | 56.7 | |
| 1+ | 42.5 | 0.90 (0.75–1.09) | 37.6 | 0.71 (0.51–0.98) | 45.4 | 49.3 | 1.04 (0.72–1.48) | 43.3 | |
| Parent cigarette smoking, 1+ vs. 0 | .626 | ||||||||
| 0 | 61.0 | 56.3 | 55.7 | 57.0 | |||||
| 1+ | 43.3 | 39.0 | 43.7 | 44.3 | 43.0 | ||||
| Self-identified smoking description | <.001 | ||||||||
| Smoker | 8.6 | 0.79 (0.50–1.25) | 6.1 | 0.58 (0.25–1.35) | 11.0 | 13.0 | 0.72 (0.35–1.46) | 9.3 | |
| Social or occasional smoker | 7.2 | 0.66 (0.43–1.01) | 8.0 | 0.81 (0.41–1.61) | 10.4 | 10.3 | 0.70 (0.34–1.44) | 8.5 | |
| Ex-smoker/tried smoking | 15.9 | 0.83 (0.66–1.05) | 10.1 | 0.55 (0.35–0.85) | 17.5 | 16.1 | 0.86 (0.59–1.28) | 15.7 | |
| Nonsmoker | 68.3 | Ref. | 75.7 | Ref. | 61.1 | 60.6 | Ref. | 66.5 | |
| Past 30-day tobacco use | <.001 | ||||||||
| No | 81.6 | Ref. | 85.7 | Ref. | 74.7 | 69.2 | Ref. | 79.1 | |
| Yes | 18.4 | 0.77 (0.55–1.09) | 14.3 | 0.60 (0.33–1.12) | 25.3 | 30.8 | 1.41 (0.83–2.41) | 20.9 | |
| Past 30-day cigarette use | .027 | ||||||||
| No | 86.0 | 87.8 | 83.1 | 79.6 | 84.9 | ||||
| Yes | 14.0 | 12.2 | 16.9 | 20.4 | 15.1 | ||||
| Past 30-day cigar use | <.001 | ||||||||
| No | 99.1 | 98.6 | 96.5 | 95.8 | 98.0 | ||||
| Yes | 0.9 | 1.4 | 3.5 | 4.2 | 2.0 | ||||
| Past 30-day little cigar/cigarillo use | .234 | ||||||||
| No | 96.5 | 97.3 | 94.9 | 95.9 | 96.1 | ||||
| Yes | 3.5 | 2.7 | 5.1 | 4.1 | 3.9 | ||||
| Past 30-day e-cigarette use | <.001 | ||||||||
| No | 97.6 | 97.3 | 93.5 | 86.4 | 95.5 | ||||
| Yes | 2.4 | 2.7 | 6.5 | 13.6 | 4.5 | ||||
| Past 30-day smokeless use | <.001 | ||||||||
| No | 98.4 | 99.9 | 96.5 | 95.3 | 97.8 | ||||
| Yes | 1.6 | 0.1 | 3.5 | 4.7 | 2.2 | ||||
| Past 30-day hookah use | .154 | ||||||||
| No | 98.3 | 98.2 | 96.8 | 96.7 | 97.7 | ||||
| Yes | 1.7 | 1.8 | 3.2 | 3.3 | 2.3 |
Missing: Subjective financial situation (n = 11; 0.3%); peer smoking (n = 51; 1%); parent smoking (n = 1132; 28%); self-identified smoking status (n = 7; 0.2%); past 30-day cigarette use (n = 12; 0.3%); past 30-day cigar use (n = 8; 0.2%); past 30-day little cigar/cigarillo use (n = 8; 0.2%); past 30-day e-cigarette use (n = 87; 2%); past 30-day smokeless tobacco use (n = 8; 0.2%); past 30-day hookah use (n = 10; 0.3%).
aMultinomial logistic regression model accounting for survey weighting and controlling for age, race/ethnicity, sex, education, subjective financial situation, peer smoking (1+ vs. 0), self-identified smoking status, and past 30-day use of any tobacco product. The adjusted relative risk ratio (RRR) estimates the likelihood of the outcome (eg, membership in class 1 vs. class 3) for a variable, holding all other variables in the model constant.
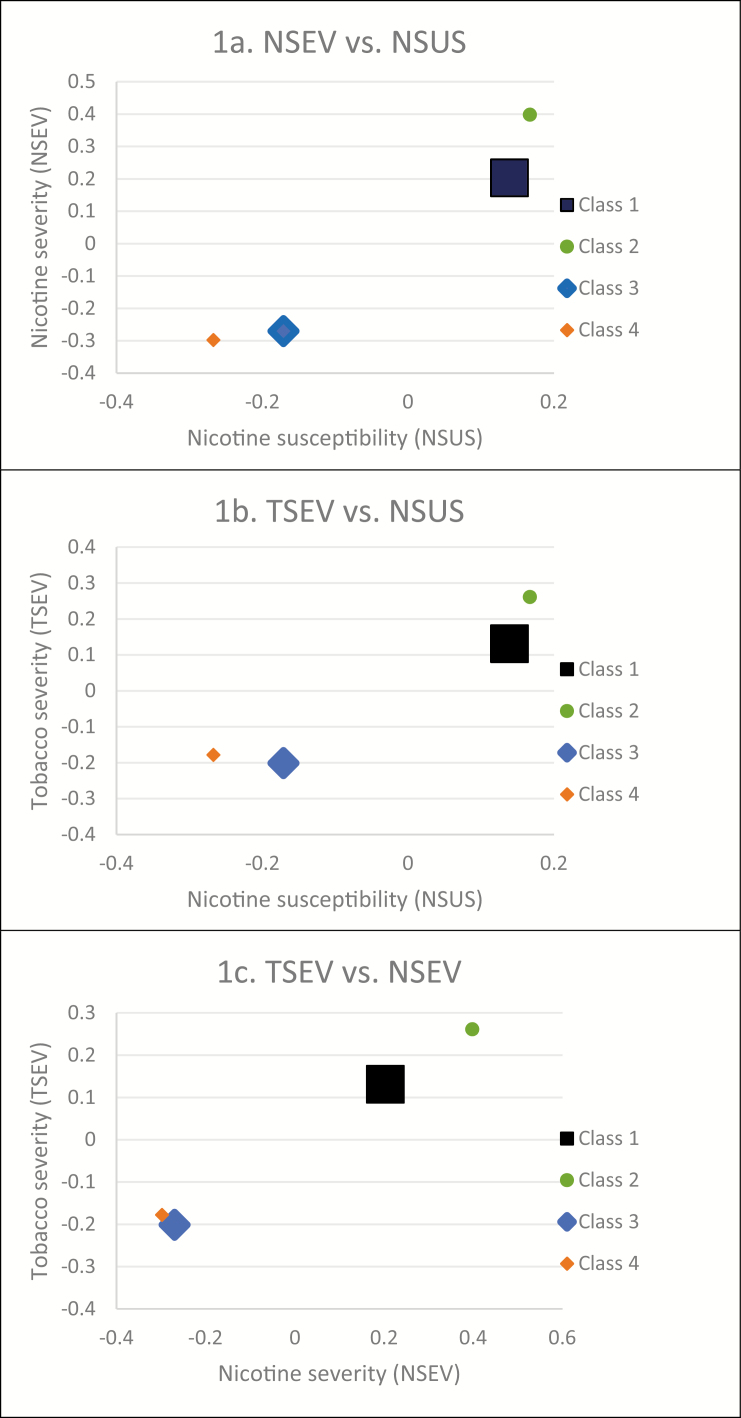
Confirmatory factor analyses using our a priori categorization of items had fit indices that were below recommended values (CFI = .929, TLI = .885). The model improved by combining two items initially grouped with the NSEV factor (ie, “Are nicotine patches more likely, about the same, or less likely to cause someone to have a heart attack as cigarettes?” and “Are electronic cigarettes (e-cigarettes) more likely, about the same, or less likely to cause someone to have a heart attack as cigarettes?”) with the three available NSUS items (CFI = .97, TLI = .952). There were many significant differences between perceptions of NSUS, NSEV, and TSEV by latent class (Table 3; all ps < .001). Members of classes 1 and 2 perceived a similar susceptibility to nicotine’s harms; those in both classes had significantly higher mean response and factor score than classes 3 and 4 for the NSUS construct. Those in classes 3 and 4 perceived similarly lower NSEV and TSEV compared to those in classes 1 and 2. Otherwise, pairwise comparisons indicated that latent classes differed significantly from each other on these constructs. Figure 1 depicts a consistent ordering of latent class across the three factors, with those in class 2 reporting the highest perceived severity to nicotine and tobacco harms, followed by those in class 1. Members of class 4 reported the lowest perceived susceptibility to nicotine’s harms. These results were also the same when using the mean response of all items included in the factor.
Figure 1.
Correlations between factor scores for perceived harms of nicotine and tobacco products by latent class. Note: Markers are proportional to group size.
Discussion
Findings from this study provide novel evidence that underlying nicotine beliefs impact and differentiate perceptions of susceptibility and severity of the harms from nicotine and tobacco products relative to cigarettes. Four distinct classes of young adults emerged based on their nicotine beliefs, largely consistent with our hypotheses: one defined by perceptions of high harms from nicotine and tobacco products (class 1; largest class); one defined by uncertainty about nicotine and tobacco product harms (class 2); and two defined by perceptions of low harms from nicotine and tobacco products (classes 3 and 4). There was a greater proportion of any past 30-day tobacco use in the two “low harm” classes (classes 3 and 4) in bivariate analyses, but this did not remain significant in multivariable analyses. These latent classes revealed variation in beliefs about nicotine, with the largest class (52% of the sample) reporting the greatest number of false beliefs about nicotine. This is consistent with recent studies in population samples, which have reported on one or more of the items included in the latent class analysis but not the combination of these four items.12–14 Those in classes 1 and 2 were also less likely to be non-Hispanic White or to have a college education. These findings may help to identify specific beliefs or groups to be targeted by public education efforts on nicotine. Also, consistent with our a priori constructs from the Health Belief Model,23 items related to nicotine and tobacco product harm perceptions (relative to cigarettes) “hung together” in exploratory and confirmatory factor analysis as NSUS, NSEV, and TSEV. One interesting note was that two items originally characterized as NSEV (ie, likelihood of heart attack from nicotine patch and e-cigarettes compared to cigarettes) fit better on the NSUS factor than the NSEV factor. Nicotine and TSEV factors were differentiated as the general health harms of specific products compared to regular cigarettes. Importantly, nicotine and tobacco perception factor scores varied significantly by latent class of nicotine beliefs and classes with common beliefs about health harms (high or low) were similar to each other on some of these factors. Generally, class 2 members reported the highest perceived nicotine and tobacco harms, followed by class 1, class 3, and class 4 members. Those in classes 1 and 2 had a higher perceived susceptibility to nicotine’s harms, which differed significantly from classes 3 and 4. Classes 3 and 4 similarly perceived a lower severity of nicotine and tobacco harms compared to classes 1 and 2. There were, however, many pairwise differences between latent classes when looking at the factor scores, suggesting that underlying nicotine beliefs distinguish patterns of response to items on nicotine and tobacco harm perceptions.
Strengths of the study include a large, national sample of young adults and a novel approach to comparing latent classes to responses on a large number of nicotine and tobacco perceptions items using factor analysis. There are, however, several limitations to this study. First, the generalizability of the sample is limited by a low cumulative response rate. While this is similar to other health studies that have relied on KnowledgePanel35–38 and the prevalence of response to the “nicotine is a cause of cancer” item in this sample is consistent with another national sample,12 we acknowledge that this may limit the external validity of our findings. Second, we were unable to fully test the consistency of constructs in the Health Belief Model, since the wave 9 survey did not include items on susceptibility to tobacco harms (TSUS). Further exploration of the relationships between latent classes of nicotine beliefs and the addictiveness of tobacco products will be essential to understanding how these underlying beliefs inform harm perceptions across all four a priori constructs in our conceptual framework: NSUS, NSEV, TSUS, and TSEV. Third, this study was conducted prior to the rise of e-cigarette marketing in the form of sponsored posts and influencers on social media39–41 and before national public education campaigns were launched to address e-cigarettes,42,43 which may affect more contemporary responses to the items on NSUS and severity related to those products. Finally, all of our harm perceptions items use “regular cigarettes” as a common comparator; it is unknown whether or how these relationships between nicotine beliefs and nicotine and tobacco harm perceptions would change if these items were asked in terms of absolute harm or if asked using a different comparator (eg, no use). Absolute harm measures may have been a cleaner fit with the Health Belief Model constructs, though the relative harm measures still loaded well onto the construct factors.
Communicating about the risks of smoking separate from the risks of nicotine will be essential to maximizing the public health benefit of FDA’s warning labels on nicotine and the proposed policy on nicotine reduction in combustible cigarettes. The current study supports that underlying nicotine beliefs are associated with perceived harms of specific nicotine and tobacco products (relative to cigarettes), with greater false beliefs about nicotine correlated with greater perceived susceptibility to nicotine addiction. Mixed beliefs about nicotine, specifically, responding “don’t know” to “Nicotine is a cause of cancer” and “The claim that a cigarette brand is low in nicotine means that it is less addictive” and that nicotine is responsible for a large part of the health risks of smoking, were correlated with the highest perceived harms of nicotine and tobacco products. As seen in other national studies,12,14 including in this sample of young adults,13 misperceptions of nicotine are widespread. Two important inferences emerge from this study: first, that education to address nicotine beliefs may also reframe perceptions of the harms of nicotine and tobacco products and second, that this type of education may differentially impact perceptions of the harms of nicotine products (eg, nicotine replacement therapy and e-cigarettes) and tobacco products (eg, cigars, smokeless, hookah). Pilot evidence suggests that brief nicotine corrective messages consistent with the type of messages used in health communication mass media campaigns can reduce false beliefs about nicotine.44 Together, these studies support that public education may move consumers closer to an understanding that there is a continuum of risk across tobacco products,45 as acknowledged by the FDA, and the fact that nicotine is “most harmful when delivered through smoke particles in combustible cigarettes.” 46 Future research is needed to test the efficacy of corrective messaging about nicotine as a product constituent in population samples, to examine whether and how latent classes of nicotine beliefs are affected by such educational efforts and to explore whether there is a consistent relationship between latent classes of nicotine beliefs and response to items on nicotine product perceptions.
Funding
Research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health under award number R03CA212694. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Declaration of Interests
RSN receives funding from the FDA Center for Tobacco Products via contractual mechanisms with Westat and the National Institutes of Health. Within the past 3 years, he has served as a paid consultant to the Government of Canada and has received an honorarium for a virtual meeting from Pfizer. The authors have no other conflicts to disclose. No financial disclosures were reported by the authors of this paper.
References
- 1. US Department of Health and Human Services. How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease: A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2010. [Google Scholar]
- 2. US Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress. A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; January 2014. [Google Scholar]
- 3. IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Tobacco Smoking. 2012; Vol. 100-E http://publications.iarc.fr/122. Accessed September 5, 2019. [Google Scholar]
- 4. IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Smokeless Tobacco. 2012; Vol. 100-E http://publications.iarc.fr/122. Accessed September 5, 2019. [Google Scholar]
- 5. IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Smokeless Tobacco and Some Tobacco-specific N-Nitrosamines. 2007; Vol. 89 http://publications.iarc.fr/107. Accessed September 5, 2019. [PMC free article] [PubMed] [Google Scholar]
- 6. Fong GT, Elton-Marshall T, Driezen P, et al. . U.S. adult perceptions of the harmfulness of tobacco products: descriptive findings from the 2013–14 baseline wave 1 of the path study. Addict Behav. 2019;91:180–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Tan AS, Bigman CA. E-cigarette awareness and perceived harmfulness: prevalence and associations with smoking-cessation outcomes. Am J Prev Med. 2014;47(2):141–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Huang J, Feng B, Weaver SR, Pechacek TF, Slovic P, Eriksen MP. Changing perceptions of harm of e-cigarette vs cigarette use among adults in 2 US national surveys from 2012 to 2017. JAMA Netw Open. 2019;2(3):e191047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Berg CJ, Stratton E, Schauer GL, et al. . Perceived harm, addictiveness, and social acceptability of tobacco products and marijuana among young adults: marijuana, hookah, and electronic cigarettes win. Subst Use Misuse. 2015;50(1):79–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wackowski OA, Delnevo CD. Young adults’ risk perceptions of various tobacco products relative to cigarettes: results from the national young adult health survey. Health Educ Behav. 2016;43(3):328–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ambrose BK, Rostron BL, Johnson SE, et al. . Perceptions of the relative harm of cigarettes and e-cigarettes among U.S. youth. Am J Prev Med. 2014;47(2 suppl 1):S53–S60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. O’Brien EK, Nguyen AB, Persoskie A, Hoffman AC. U.S. adults’ addiction and harm beliefs about nicotine and low nicotine cigarettes. Prev Med. 2017;96:94–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Villanti AC, Naud S, West JC, et al. . Prevalence and correlates of nicotine and nicotine product perceptions in U.S. young adults, 2016. Addict Behav. 2019;98:106020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Byron MJ, Jeong M, Abrams DB, Brewer NT. Public misperception that very low nicotine cigarettes are less carcinogenic. Tob Control. 2018;27(6):712–714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wackowski OA, Ray AE, Stapleton JL. Smokers’ perceptions of risks and harm from snus relative to cigarettes: a latent profile analysis study. Addict Behav. 2019;91:171–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rath JM, Villanti AC, Abrams DB, Vallone DM. Patterns of tobacco use and dual use in US young adults: the missing link between youth prevention and adult cessation. J Environ Public Health. 2012;2012:679134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. The American Association for Public Opinion Research. Standard Definitions: Final Dispositions of Case Codes and Outcome Rates for Surveys. 8th ed 2015. Oakbrook Terrace, IL: AAPOR. [Google Scholar]
- 18. Callegaro M, DiSogra C. Computing response metrics for online panels. Public Opin Q. 2008;72(5):1008–1032. [Google Scholar]
- 19. Enders CK, Bandalos DL. The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Struct Equ Modeling. 2001;8(3):430–457. [Google Scholar]
- 20. Nagin D. Group-Based Modeling of Development. Cambridge, MA: Harvard University Press; 2005. [Google Scholar]
- 21. Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Struct Equ Modeling. 2007;14(4):535–569. [Google Scholar]
- 22. Collins LM, Lanza ST.. Latent Class and Latent Transition Analysis with Applications in the Social, Behavioral, and Health Sciences. Hoboken, NJ: John Wiley & Sons, Inc; 2010. [Google Scholar]
- 23. Rosenstock IM. The health belief model and preventive health behavior. Health Educ Monogr. 1974;2(4):355–385. [DOI] [PubMed] [Google Scholar]
- 24. Brewer NT, Chapman GB, Gibbons FX, Gerrard M, McCaul KD, Weinstein ND. Meta-analysis of the relationship between risk perception and health behavior: the example of vaccination. Health Psychol. 2007;26(2):136–145. [DOI] [PubMed] [Google Scholar]
- 25. Ferrer R, Klein WM. Risk perceptions and health behavior. Curr Opin Psychol. 2015;5:85–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Brewer NT, Weinstein ND, Cuite CL, Herrington JE. Risk perceptions and their relation to risk behavior. Ann Behav Med. 2004;27(2):125–130. [DOI] [PubMed] [Google Scholar]
- 27. Hu Lt, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6(1):1–55. [Google Scholar]
- 28. Williams VF, Smith AA, Villanti AC, et al. . Validity of a subjective financial situation measure to assess socioeconomic status in US young adults. J Public Health Manag Pract. 2017;23(5):487–495. [DOI] [PubMed] [Google Scholar]
- 29. Oetting ER. Primary socialization theory. Developmental stages, spirituality, government institutions, sensation seeking, and theoretical implications. V. Subst Use Misuse. 1999;34(7):947–982. [DOI] [PubMed] [Google Scholar]
- 30. Oetting ER, Donnermeyer JF. Primary socialization theory: the etiology of drug use and deviance. I. Subst Use Misuse. 1998;33(4):995–1026. [DOI] [PubMed] [Google Scholar]
- 31. Hertel AW, Mermelstein RJ. Smoker identity and smoking escalation among adolescents. Health Psychol. 2012;31(4):467–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Villanti AC, Johnson AL, Rath JM, et al. . Identifying “social smoking” U.S. young adults using an empirically-driven approach. Addict Behav. 2017;70:83–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Johnson AL, Villanti AC, Williams V, et al. . Smoking trajectory classes and impact of social smoking identity in two cohorts of U.S. young adults. Emerg Adulthood. 2018;7(4):258–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Villanti AC, Johnson AL, Rath JM. Beyond education and income: identifying novel socioeconomic correlates of cigarette use in U.S. young adults. Prev Med. 2017;104:63–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Rhodes DJ, Radecki Breitkopf C, Ziegenfuss JY, Jenkins SM, Vachon CM. Awareness of breast density and its impact on breast cancer detection and risk. J Clin Oncol. 2015;33(10):1143–1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Grande D, Mitra N, Shah A, Wan F, Asch DA. Public preferences about secondary uses of electronic health information. JAMA Intern Med. 2013;173(19):1798–1806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kumar S, Quinn SC, Kim KH, Daniel LH, Freimuth VS. The impact of workplace policies and other social factors on self-reported influenza-like illness incidence during the 2009 H1N1 pandemic. Am J Public Health. 2012;102(1):134–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Fowler FJ Jr, Gerstein BS, Barry MJ. How patient centered are medical decisions?: results of a national survey. JAMA Intern Med. 2013;173(13):1215–1221. [DOI] [PubMed] [Google Scholar]
- 39. Chu KH, Colditz JB, Primack BA, et al. . JUUL: spreading online and offline. J Adolesc Health. 2018;63(5):582–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Allem JP, Dharmapuri L, Unger JB, Cruz TB. Characterizing JUUL-related posts on Twitter. Drug Alcohol Depend. 2018;190:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Huang J, Duan Z, Kwok J, et al. . Vaping versus JUULing: how the extraordinary growth and marketing of JUUL transformed the US retail e-cigarette market. Tob Control. 2019;28(2):146–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. U.S. Department of Health and Human Services. The real cost: Don’t get hacked by vaping https://therealcost.betobaccofree.hhs.gov/gm/hacked-ends.html. Accessed April 6, 2019.
- 43. Truth Initiative. Am I a puppet?https://www.thetruth.com/articles/videos/vaping-inner-monologue. Accessed April 6, 2019.
- 44. Villanti AC, West JC, Mays D, Donny EC, Cappella JN, Strasser AA. Impact of brief nicotine messaging on nicotine related beliefs in a U.S. online sample. Am J Prev Med. 2019; in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Abrams DB, Glasser AM, Pearson JL, Villanti AC, Collins LK, Niaura RS. Harm minimization and tobacco control: reframing societal views of nicotine use to rapidly save lives. Annu Rev Public Health. 2018;39:193–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. U.S. Food and Drug Administration. FDA’s Plan for Tobacco and Nicotine Regulation 2017; https://www.fda.gov/TobaccoProducts/NewsEvents/ucm568425.htm. Accessed February 7, 2018.