Abstract
Background
Guidelines recommend conservative management for a spontaneous coronary artery dissection (SCAD) in the absence of ongoing ischaemia, haemodynamic instability, or left main dissection. Conventional percutaneous coronary intervention methods for SCAD are associated with an unfavourable prognosis due to difficulties wiring the lesion, dissection propagation, and potential ‘milking’ of the intramural haematoma along the vessel or into other vessels. These factors promote implantation of multiple stents which are often undersized, increasing the risk of in-stent restenosis significantly. There have been several case reports demonstrating the novel use of small diameter cutting balloons in the left anterior descending artery system. Here, we describe the successful use of a larger 4 mm cutting balloon to treat a spontaneous right coronary artery (RCA) dissection.
Case summary
A 53-year-old woman with troponin negative chest pain and was diagnosed with unstable angina due to ischaemic electrocardiographic features. Coronary angiography revealed a tight discrete lesion in the RCA. Intravascular imaging confirmed SCAD and a 4 mm cutting balloon was used to dissect the tunica intima to allow complete resorption of the intramural haematoma and resolution of symptoms.
Discussion
This case demonstrates the safe use of a larger 4 mm cutting balloon to treat an RCA SCAD, resulting in complete resolution of the haematoma.
Keywords: Case report, Spontaneous coronary artery dissection, Cutting balloon, Percutaneous coronary intervention
Learning points
Cutting balloons provide an effective treatment of spontaneous coronary artery dissections (SCADs) and can prevent the necessity of stent implantation.
Controlled dissection of the tunica intima allows the intramural haematoma to resorb into the true lumen without significant damage to the coronary vessel.
A 4-mm diameter cutting balloon can be safely used with slow and gentle inflation.
Intravascular imaging is highly recommended in cases of SCAD to aid diagnosis, balloon sizing, and assess response to treatment.
Introduction
Spontaneous coronary artery dissection (SCAD) is a non-traumatic, non-atherosclerotic epicardial coronary dissection, often resulting in a subintimal haematoma that can compromise coronary flow. It is an important and often under-recognized cause of acute coronary syndromes (ACS), particularly in females. While the true prevalence is unknown, SCAD may account for up to 2–4% of all ACS cases.1,2 Conservative management remains the mainstay of treatment in the absence of ongoing ischaemia, haemodynamic instability, or left main stem involvement. When percutaneous coronary intervention (PCI) is indicated, it is often associated with an unfavourable prognosis due to difficulties wiring the lesion, dissection propagation, and potential ‘milking’ of the intramural haematoma along the vessel or into other vessels. The use of a cutting balloon to fenestrate the tunica intima and drain the intramural haematoma has emerged as a novel treatment technique. Their use has thus far been limited to small diameter cutting balloons in the left coronary system.
Timeline
| Date | |
|---|---|
| 23 May 2019 |
|
| 24 May 2019 | Transthoracic echocardiogram: normal |
| 28 May 2019 | Coronary angiography demonstrating Type 3 spontaneous coronary artery dissection on optical coherence tomography—successfully treated with a 4-mm diameter cutting balloon intervention with resolution of symptoms |
| 30 May 2019 | Discharged from hospital. Remained asymptomatic. |
| 2 August 2019 | Followed-up in outpatient clinic. No recurrence of symptoms. |
Case presentation
A 53-year-old woman presented to the Cardiology clinic with a 1-month history of retrosternal chest tightness since the bereavement of a friend. Examination was unremarkable. The past medical history included hypertension and there was a family history of premature coronary artery disease. The pain radiated to shoulders, arms, jawline and was present at rest. The patient was, therefore, admitted to hospital for urgent cardiac investigations and inpatient coronary angiography. Post-admission, despite medical therapy, she continued to experience ongoing chest pain in the days preceding and during angiography.
Investigations
Blood tests: Full blood count, renal function tests, and high-sensitivity troponin I levels were normal.
Echocardiogram: Biventricular size and systolic function normal with no regional wall abnormalities and no significant valvular disease.
Twelve-lead electrocardiogram (ECG): Sinus rhythm with T-wave inversion in the inferolateral leads.
Treatment
The patient underwent coronary angiography via the right radial artery using a 6-Fr sheath. The left coronary artery was engaged using a Voda left 3.5 guide catheter and initial injections in the posteroanterior caudal view revealed TIMI 0 flow in the first obtuse marginal (OM1) branch (Figure 1A). The left anterior descending artery was free of disease and by the second contrast injection, OM1 flow had normalized (Figure 1B). Assessment of this vessel using optical coherence tomography (OCT) revealed no abnormalities (Figure 2), suggesting that the temporary occlusion was due to vasospasm.
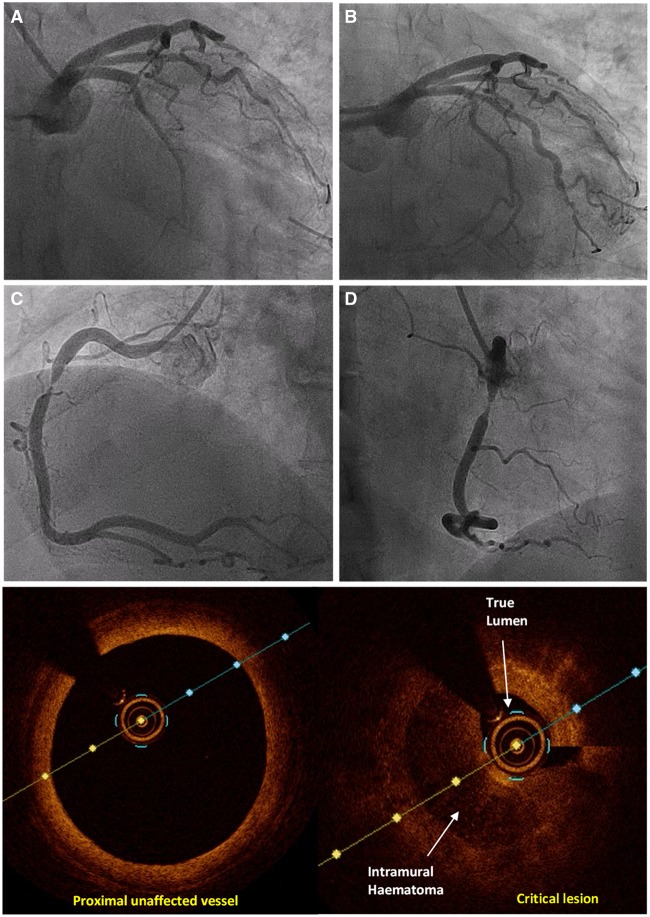
Figure 1.
(A) Left coronary angiography (posteroanterior caudal) revealing a vasospastic occlusion of first obtuse marginal. (B) Left coronary angiography (posteroanterior cranial) normal subsequent flow in first obtuse marginal. (C and D) Right coronary angiography demonstrating a critical lesion in the mid-vessel. (E) Right coronary optical coherence tomography demonstrating normal appearances of the proximal vessel. (F) Right coronary optical coherence tomography demonstrating spontaneous coronary artery dissection within the critical lesion.
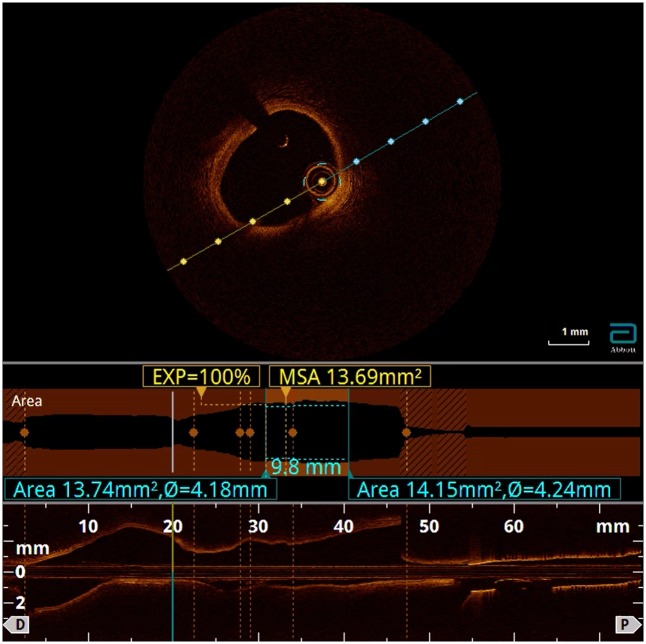
Figure 2.
Optical coherence tomography interrogation of first obtuse marginal demonstrating no significant acute lesions or adverse features.
The right coronary artery (RCA) was engaged using a Judkins Right 4 catheter and selective angiography revealed a critical lesion in the mid-vessel (Figure 1C and D). In view of the history of stress-induced chest pain, the lesion was interrogated with OCT. This revealed a significant intramural haematoma within the mid-vessel causing a critical stenosis with a minimal luminal area of just 1 mm2 (Figure 1F).
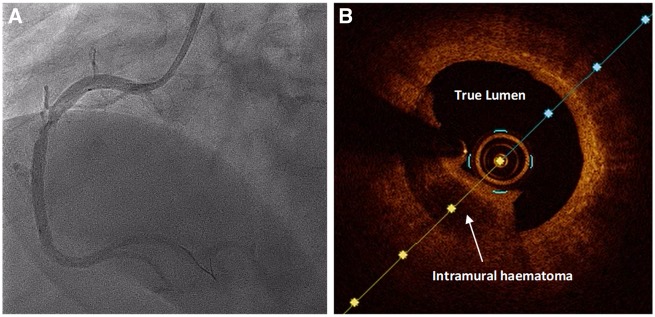
These findings were consistent with Type 3 SCAD. In view of the patient’s ongoing ischaemia and ECG changes, the decision was made to treat this lesion. A 2.5-mm semi-compliant balloon was inflated to six atmospheres to gently pre-dilate the vessel. Repeat angiography and OCT imaging revealed improved appearances of the lesion (Figure 3).
Figure 3.
(A) Right coronary angiography (left anterior oblique) revealing improvement of lesion following balloon dilatation. (B) Right coronary angiography optical coherence tomography showing improvement of lesion following balloon dilatation.
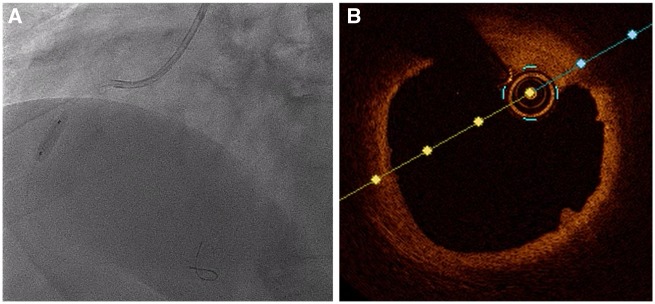
A 4 × 10 mm Flextome cutting balloon (Boston Scientific, MA, USA) was then gently inflated for 8 s to nominal pressure on three occasions (Figure 4A). This led to complete resolution of the intramural haematoma with only very minimal residual intimal dissection on OCT (Figure 4B). The maximal luminal area of the vessel by the end of the procedure increased to over 10 mm2.
Figure 4.
(A) Inflation of the 4 × 10 mm flextome cutting balloon in the right coronary artery. (B) Right coronary optical coherence tomography showing resolution of the lesion.
Final angiographic appearances showed excellent resolution of the lesion and TIMI III flow (Figure 5C and D). The patient’s symptoms resolved and she was subsequently discharged 2 days later on a regimen of aspirin and clopidogrel for 3 months and aspirin alone thereafter. This dual antiplatelet regimen was prescribed due to disruption of the intimal layer by balloon angioplasty. The patient was followed-up in clinic and found to be asymptomatic with no further recurrences of angina. She will be investigated for associated conditions such as fibromuscular dysplasia.
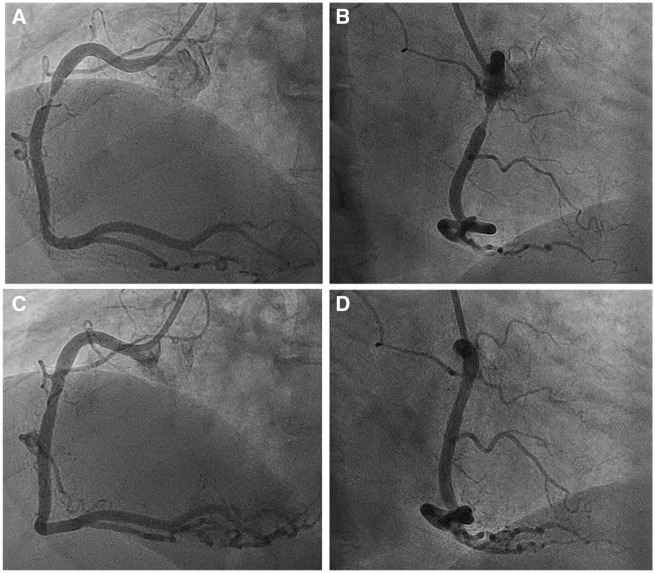
Figure 5.
Right coronary angiography images in the left anterior oblique and right anterior oblique projection demonstrating the difference in vessel calibre at the beginning (A and B) and end (C and D) of the procedure.
Discussion
Conservative management is the favoured approach for patients with SCAD in the absence of ongoing ischaemia, haemodynamic instability, or left main dissection. In the case described, the patient experienced ongoing chest pain, providing a mandate for coronary intervention.
Conventional PCI methods are associated with an unfavourable prognosis in SCAD compared with atherosclerotic disease. This is due to recognized complications such as difficulty wiring the lesion, dissection propagation, and ‘milking’ of the intramural haematoma along the vessel or into other vessels. These factors often lead to the use of multiple stents which are often undersized due to difficulty in assessing the true luminal diameter. This combination of multiple malapposed stents increases the risk of in-stent restenosis significantly.
The use of a cutting balloon to treat SCAD is a novel technique with only a small number of reported cases worldwide to date.3–9 The intention is to create a fenestration in the tunica intima to drain the subintimal haematoma into the true lumen, which is thus decompressed. The use of larger cutting balloons has been avoided due to the risk of creating large dissection flaps or even coronary perforation. Case reports have so far described the use of small cutting balloons (usually <2.5 mm diameter) in the left coronary artery system.
This case uniquely demonstrates the safe and effective use of a larger (4 mm diameter) cutting balloon in an RCA SCAD. The rationale behind the use of larger cutting balloons is to ensure that the microblades of the cutting balloon reach the tunica intima. This is particularly important in larger diameter vessels. Using OCT in the case described above, the patient was found to have a SCAD in an otherwise large 4-mm diameter RCA. This thereby necessitated a larger cutting balloon, the use of which was not associated with any adverse events. The risk of coronary perforation was minimized by gentle inflation of the cutting balloon to low (nominal) pressure.
Intravascular imaging with intravascular ultrasound or OCT is critical in suspected cases of SCAD. Unfortunately, the appearances of Type 3 SCAD mimic atherosclerotic lesions closely. The clinical history and risk profile of the patient are important factors that help a clinician to determine when intravascular imaging should be used to differentiate atherosclerotic lesions from potential SCAD. Aside from the diagnostic benefits, intravascular imaging is also useful for sizing the vessel and assessing resolution of the intramural haematoma. In the above case, OCT was also used to assess the temporary occlusion of OM1 which was likely caused by coronary vasospasm. It is worth noting that the likelihood of coronary and radial vasospasm is increased in patients with SCAD and a femoral approach may be more favourable if the clinical history is suggestive of SCAD.
Conclusion
We anticipate that cutting balloons will be increasingly used in the treatment of SCAD, provided the clinical scenario warrants percutaneous intervention. The avoidance of unnecessary stent implantation provides a clear advantage over conventional PCI methods, however, long-term data on the recurrence of SCAD following the use of cutting balloons are lacking.
Lead author biography

Dr Harish Sharma graduated from the University of Oxford and is a Cardiology Registrar at the Queen Elizabeth Hospital Birmingham where he has been awarded a research fellowship. His interests include Interventional Cardiology and Cardiac Imaging.
Supplementary material
Supplementary material is available at European Heart Journal - Case Reports online.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The author/s confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: none declared.
Supplementary Material
References
- 1. Mortensen KH, Thuesen L, Kristensen IB, Christiansen EH.. Spontaneous coronary artery dissection: a Western Denmark Heart Registry study. Catheter Cardiovasc Interv 2009;74:710–717. [DOI] [PubMed] [Google Scholar]
- 2. Nishiguchi T, Tanaka A, Ozaki Y, Taruya A, Fukuda S, Taguchi H, Iwaguro T, Ueno S, Okumoto Y, Akasaka T.. Prevalence of spontaneous coronary artery dissection in patients with acute coronary syndrome. Eur Heart J Acute Cardiovasc Care 2016;5:263–270. [DOI] [PubMed] [Google Scholar]
- 3. Main A, Lombardi W, Saw J.. Cutting balloon angioplasty for treatment of spontaneous coronary artery dissection: case report, literature review, and recommended technical approaches. Cardiovasc Diagn Ther 2019;9:50–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Yumoto K, Sasaki H, Aoki H, Kato K.. Successful treatment of spontaneous coronary artery dissection with cutting balloon angioplasty as evaluated with optical coherence tomography. JACC Cardiovasc Interv 2014;7:817–819. [DOI] [PubMed] [Google Scholar]
- 5. Ito T, Shintani Y, Ichihashi T, Fujita H, Ohte N.. Non-atherosclerotic spontaneous coronary artery dissection revascularized by intravascular ultrasonography-guided fenestration with cutting balloon angioplasty. Cardiovasc Interv Ther 2017;32:241–243. [DOI] [PubMed] [Google Scholar]
- 6. Alkhouli M, Cole M, Ling FS.. Coronary artery fenestration prior to stenting in spontaneous coronary artery dissection. Catheter Cardiovasc Interv 2016;88:E23–E27. [DOI] [PubMed] [Google Scholar]
- 7. Lee R, Ben-Dor I.. Revascularization methods in spontaneous coronary artery dissection: a focused review. Cardiovasc Revasc Med 2017;18:544–548. [DOI] [PubMed] [Google Scholar]
- 8. Noguchi M, Obunai K, Fukui Y, Okumura H, Watanabe H.. Usefulness of cutting balloon angioplasty prior to stenting with intravascular ultrasound imaging guidance for spontaneous multi-vessel coronary artery dissection including the left main coronary artery. Intern Med 2018;57:1867–1871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. McGrath BM, Vo MN.. Novel use of cutting balloon to manage compressive subintimal hematoma during left main stenting in a patient with spontaneous coronary artery dissection. Clin Case Rep 2018;6:1291–1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.