Abstract
The Society of Radiologists in Ultrasound convened a panel of specialists from gynecology, radiology, and pathology to arrive at a consensus regarding the management of ovarian and other adnexal cysts imaged sonographically in asymptomatic women. The panel met in Chicago, Ill, on October 27–28, 2009, and drafted this consensus statement. The recommendations in this statement are based on analysis of current literature and common practice strategies, and are thought to represent a reasonable approach to asymptomatic ovarian and other adnexal cysts imaged at ultrasonography.
© RSNA, 2010
Introduction
The Society of Radiologists in Ultrasound (SRU) convened a panel of specialists from gynecology, radiology, and pathology to arrive at a consensus regarding the management of ovarian and other adnexal cysts imaged at ultrasonography (US) in asymptomatic women. The panel (along with observers with expertise in US and gynecology) met in Chicago, Ill, on October 27–28, 2009, and drafted this consensus statement. The expertise of the panelists included radiology, with subspecialty interests in gynecologic US; gynecology, with subspecialty interests in gynecologic US, general gynecology, reproductive endocrinology and infertility, menopause, and gynecologic oncology; pathology, with subspecialty interest in gynecologic pathology; and epidemiology.
Pelvic US remains the primary, and in most cases the preferred, imaging modality to evaluate adnexal cysts (1). The majority of adnexal masses can be correctly categorized based on grayscale and color or power Doppler US features (2). Surgical removal is the generally accepted management for cystic adnexal masses with sonographic features suggestive of malignancy (which is the minority of adnexal masses). The vast majority of cystic adnexal masses are benign (2), and either have typical sonographic features that allow a confident determination of benignity or have indeterminate sonographic features that do not allow a confident diagnosis to be made. There is a lack of consensus on how to manage patients in these two groups, and current approaches vary. Our goal was to reach a consensus on which masses require no follow-up; which masses need imaging follow-up, as well as when this evaluation should occur; and which masses warrant surgical evaluation.
This conference dealt with masses in asymptomatic nonpregnant women. It should be recognized that these recommendations may be helpful in symptomatic women, but the clinical setting will often determine management in a manner beyond the scope of this consensus panel.
Methods and Conference Preparations
The comoderators of the conference (D.L. and D.L.B.) planned the topics and enlisted speakers to discuss thorough coverage of these topics. We limited the discussion to asymptomatic, nonpregnant, adult women with ovarian or other adnexal cysts. The specific topics were the appropriate follow-up of cysts with respect to patient age and/or menopausal status, cyst size, cyst morphology, and Doppler US findings. Management of adnexal cysts in symptomatic women will be considerably influenced by patient symptoms in addition to the previously mentioned parameters. We did not address solid adnexal masses, since such lesions, although most commonly benign, will generally be referred for surgical evaluation (3) unless they can be shown to be pedunculated fibroids. Our goal was to improve patient care, and where possible, decrease unnecessary additional imaging and patient anxiety associated with the diagnosis of an adnexal cyst. As much as possible, recommendations were based on published evidence, though in many situations reliable evidence was lacking and recommendations were based on a consensus opinion of the panelists.
Speakers were asked to provide a brief summary of their talks and a short list of relevant references (4–41), which were made available to the panelists before the meeting. The panel consisted of the two comoderators and 14 additional panelists. An audience of invited representatives from various medical societies and industry was also present. The first day of the conference consisted of presentations and discussion regarding normal ovarian sonographic findings, sonographic findings that may occur with different types of adnexal cysts, pathologic and clinical data regarding ovarian cysts, timing and related features of menopause, and management options. During the evening of the first day, a subset of panelists drafted a preliminary statement. The following morning, the preliminary statement was discussed and revised by the panel until a consensus was reached. After the conference, the consensus document was prepared by the comoderators and sent to all the panelists and participating SRU Executive Board members for review.
Consensus Discussion
US Technical Aspects
The sonographic features discussed in this document, and the subsequent recommendations, require that a technically adequate pelvic US study has been obtained. Generally this includes transvaginal US, with transabdominal US as needed, and requires that the entire cyst be adequately imaged. We recognize that, for various reasons, there will be occasional instances where an adequate US study cannot be obtained. In this instance, reliable characterization of the type of cyst may not be possible with US. Color or power Doppler US is needed for evaluation of most complex cysts to ensure that no solid elements are present (that might appear hypoechoic on gray-scale images and not be recognized as solid), and to evaluate for the presence or absence of flow within any seemingly solid areas or septations. Color or power Doppler US requires proper technique to prevent erroneous interpretation. Multiple parameters, including gain and pulse repetition frequency, need to be optimized to detect slow flow. In some cases, such as when color or power Doppler imaging demonstrates small foci of color rather than distinct vessels, spectral Doppler imaging should be performed to distinguish flow from noise or artifact. Much has been written about use of pulsatility index and resistive index in distinguishing between benign and malignant adnexal masses. However, the sensitivity and specificity of threshold spectral Doppler values are not sufficiently better than those of morphologic assessment for recommendation of use of these parameters. It was the consensus opinion in the conference that presence of flow in a solid element was the most important Doppler feature. We also recognize that measurements of cysts in three dimensions can be modified by pressure with the vaginal probe and that there is variability in accuracy of measurements. Mean or maximum diameters have been used variably in published studies. The panelists chose to use maximum diameter of the cyst in our recommendations.
US Reporting
We recognize that different reporting styles exist, and that the extent of the description of normal and clinically inconsequential findings in imaging reports can be variable. In general, normal and clinically inconsequential findings (described below) do not require any follow-up, and no follow-up studies should be recommended.
When making recommendations on management options, cyst aspiration was not considered as an option, as the panel felt that cyst aspiration was not generally a reasonable approach in the asymptomatic patient. The sensitivity of cyst fluid cytology for malignancy is low, and many cysts will recur after aspiration (3,6).
Clinical Information Pertinent to Pelvic Sonography
Important information that should be known at the time of each pelvic sonogram includes patient age, last menstrual period, and relevant signs or symptoms of a pelvic abnormality (ie, indication for examination). The majority of the panel also felt that a patient’s hormonal status (oral contraceptives, hormone replacement therapy, or fertility drugs) should be known. Other information that may be helpful includes a personal or family history of cancer, history of prior pelvic surgery, and results of prior imaging studies.
Definition of Menopause
A strict determination of menopause (especially early postmenopause) and perimenopause is difficult because it represents a continuum. Variations of physiology may occur in perimenopausal women, and the ovaries may appear somewhere in the spectrum between pre-and postmenopausal ovaries. The average age of menopause is 51–53 years in Western countries (42), with a wide variation from 40–60 years of age (43). Postmenopause is defined as 1 year or more of amenorrhea from final menstrual period. Physiologically, the postmenopausal period can be divided into two stages: early postmenopause (years 1–5 since final menstrual period) and late postmenopause (greater than 5 years since final menstrual period) (44). Ovulatory cycles occur infrequently after the final menstrual period (31).
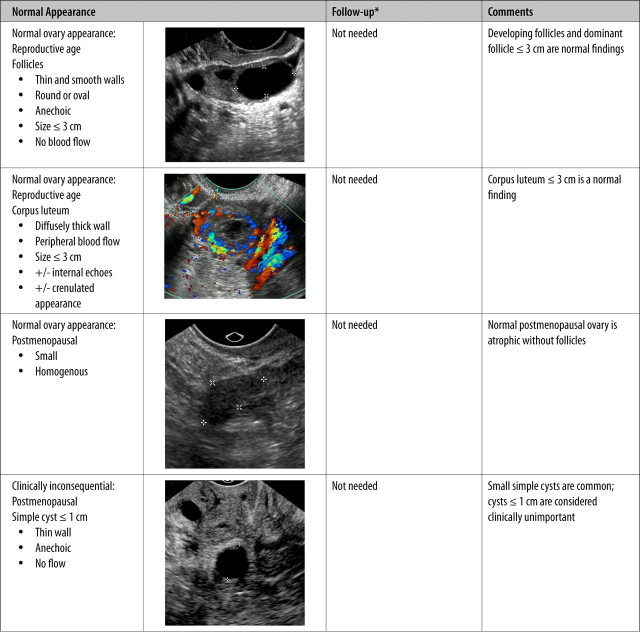
Sonographic Appearance of the Normal Ovary
The normal ovary in a woman of reproductive age has a varying appearance throughout the menstrual cycle, which may include multiple developing follicles, one or more dominant follicles, and a corpus luteum. At US the follicles appear as multiple, thin and smooth walled, round or oval, anechoic spaces with no flow by means of color Doppler US (ie, appearing as simple cysts). The size of the dominant follicle at ovulation averages 2–2.4 cm, with a range of 1.7–2.8 cm (45,46). For simplicity, the panel felt that follicles or simple cysts up to 3 cm in maximal diameter should be considered normal physiologic findings. After ovulation takes place, the dominant follicle turns into a corpus luteum. The corpus luteum is typically a cyst with diffusely thick walls and crenulated inner margins, measuring less than 3 cm in maximal diameter (47–49). It usually has internal echoes and a ring of vascularity at the periphery at color Doppler US (47–49).
Folliculogenesis ceases and the ovaries decrease in size after menopause. At US the normal postmenopausal ovary typically appears small and homogeneous in echotexture. Small simple cysts become less frequently observed as a patient progresses through the menopause transition (50). Some of these cysts appreciated in early menopause may reflect an ovulatory event, and others may be paraovarian or tubal in origin. Even in late menopause where ovulation is unlikely to occur, small simple cysts up to 1 cm may be seen in up to 21% of women (51). The panel agreed that simple cysts up to 1 cm in greatest diameter in the ovary of a postmenopausal woman should be considered a finding of no clinical importance. Therefore, these small simple cysts do not require follow-up.
Malignant Potential of Ovarian Cysts
Simple ovarian cysts that are removed surgically tend to be larger cysts and/or those in postmenopausal women, and up to 84% are serous cystadenomas (52). Hence, a central question is whether cystadenomas, particularly serous cystadenomas, have malignant potential.
Although ovarian cystadenoma and cystadenofibroma may be precursor lesions for borderline (low malignant potential) tumors and low-grade carcinoma, the rate of transformation is exceedingly slow, and these lesions can be considered benign (53). A small subset of apparently “simple cysts” is found to have borderline histologic findings at excision (54). However, short-term follow-up is unlikely to demonstrate clinically important progressive disease since the risk and rate of malignant transformation of a borderline tumor is low. Mucinous borderline tumors generally stay confined to the ovary even when they contain intraepithelial carcinoma. Serous borderline tumors may progress to low-grade carcinoma, but the recurrence rate is only 0.27% per year for stage I tumors and 2.4% for high-stage tumors (55). Lesions at risk for recurrence and transformation typically show peritoneal implants at initial presentation (32,41). Serous borderline tumors and high-grade serous carcinomas are genetically distinct lesions, and it is rare to see a transformation from borderline to high-grade malignancy (11).
Cysts with Benign Characteristics: Sonographic Features and Recommendations
Simple adnexal cysts.—A simple cyst is a round or oval anechoic space with smooth thin walls, posterior acoustic enhancement, no solid component or septation, and no internal flow at color Doppler US. Simple adnexal cysts up to 10 cm in a patient of any age are highly likely to be benign, with malignancy rates of less than 1% (6,52,56,57). The rare simple cyst that is found to have ovarian cancer is usually a large cyst where the wall has presumably been incompletely imaged. Small mural nodules may be missed at US in seemingly simple cysts larger than 7.5 cm (56). Other than these size thresholds, the panel recognized that there is little evidence to guide management. These simple cysts are either nonneoplastic cysts (including physiologic cysts, paraovarian or paratubal cysts, and small hydrosalpinges) or benign neoplastic cysts (including serous and mucinous cystadenomas).
The panelists recognized that, while simple cysts of any size are almost certainly benign, there is little evidence in the literature to guide which asymptomatic simple cysts may be ignored versus which need to be followed. The decision regarding the lower size threshold above which simple cysts need to be followed in postmenopausal women was the most difficult issue on which to reach a consensus, and we debated thresholds up to 3 cm. The majority of the panelists chose 1 cm as the threshold but recognized that practices may choose to increase that threshold up to 3 cm, at the risk of allowing a small benign neoplasm to grow until it becomes recognized later clinically or on a future imaging study. The panelists also recognized that there is little evidence to guide when follow-up can occur with decreased frequency or cease. Our recommendations entail yearly follow-up US initially. Practitioners may chose to decrease the frequency of follow-up once they are reasonably assured of stability or decrease in size, however, the panel did not feel they could make specific recommendations on this issue. It is hoped that forthcoming investigations will provide data to better guide these decisions. It may be that in the future, we can completely ignore these cysts or only follow them for a few years if they are stable in size and appearance. The panel reached the following consensus recommendations for simple cysts.
In women of reproductive age:
1. Cysts ≤3 cm: Normal physiologic findings; at the discretion of the interpreting physician whether or not to describe them in the imaging report; do not need follow-up.
2. Cysts >3 and ≤5 cm: Should be described in the imaging report with a statement that they are almost certainly benign; do not need follow-up.
3. Cysts >5 and ≤7 cm: Should be described in the imaging report with a statement that they are almost certainly benign; yearly follow-up with US recommended.
4. Cysts >7 cm: Since these may be difficult to assess completely with US, further imaging with magnetic resonance (MR) or surgical evaluation should be considered.
In postmenopausal women:
1. Cysts ≤1 cm: Are clinically inconsequential; at the discretion of the interpreting physician whether or not to describe them in the imaging report; do not need follow-up.
2. Cysts >1 and ≤7 cm: Should be described in the imaging report with statement that they are almost certainly benign; yearly follow-up, at least initially, with US recommended. Some practices may opt to increase the lower size threshold for follow-up from 1 cm to as high as 3 cm. One may opt to continue follow-up annually or to decrease the frequency of follow-up once stability or decrease in size has been confirmed. Cysts in the larger end of this range should still generally be followed on a regular basis.
3. Cysts >7 cm: Since these may be difficult to assess completely with US, further imaging with MR or surgical evaluation should be considered.
Paraovarian and paratubal cysts were considered together with ovarian cysts. Unlike the ovary, where folliculogenesis usually explains follicles up to 3 cm, we recognize that there is no similar rationale for ignoring small simple paraovarian cysts. However, paraovarian cysts are common and usually appear sonographically as simple cysts (30,33). Simple paraovarian cysts are very unlikely to be malignant (30,33). Studies showing the benign nature of simple cysts have often evaluated adnexal cysts, not distinguishing ovarian from paraovarian cysts (52,56,58). While they are not likely to resolve, simple paraovarian cysts generally are inconsequential in asymptomatic women. The panel felt that using the same size thresholds as for ovarian cysts was reasonable.
Hemorrhagic ovarian cyst.—Hemorrhagic ovarian cysts are generally due to expanding hemorrhage within a corpus luteum or other functional cyst. Sonographic features that are considered classic for a hemorrhagic ovarian cyst and that allow a confident diagnosis are: a complex cystic mass with a reticular pattern of internal echoes (also known as fishnet, cobweb, spiderweb, or lacy appearance, generally due to fibrin strands) and/or a solid-appearing area with concave margins, no internal flow at color Doppler US, and usually circumferential flow in the wall of the cyst (28,38). Wall thickness is variable in hemorrhagic cysts.
While hemorrhagic cysts typically resolve within 8 weeks (59), the panel recognized that there is little evidence in the literature to guide which ovarian cysts with classic features of a hemorrhagic cyst as described above need follow-up. The panel reached the following consensus recommendations for such cysts.
In women of reproductive age:
1. Cysts ≤3 cm: At the discretion of the interpreting physician whether or not to describe them in the imaging report; do not need follow-up.
2. Cysts >3 and ≤5 cm: Should be described in the imaging report; do not need follow-up.
3. Cysts >5 cm: Should be described in the imaging report; short-interval follow-up (6–12 weeks) with US recommended to ensure resolution. While imaging in the follicular phase, on days 3–10 of the menstrual cycle, is optimal, the panel recognized that this is sometimes difficult to coordinate in clinical practice.
Since women in early postmenopause occasionally ovulate and, therefore, develop complex cysts with the appearance of a classic hemorrhagic cyst, any such cyst should be described in the imaging report; short-interval follow-up (6–12 weeks) with US recommended to ensure resolution.
Since late postmenopausal women should never have a hemorrhagic cyst, any cyst with such an appearance should be considered neoplastic and surgical evaluation should be considered.
Endometrioma.—Sonographically, many endometriomas demonstrate internal homogeneous ground-glass or low-level echoes, without internal color Doppler flow, wall nodules, or other neoplastic features; in such masses, the additional features of multilocularity and/or tiny echogenic wall foci can help distinguish them from an acute hemorrhagic cyst (27,33,38). When these additional features are not present, an initial short-interval follow-up with US (6–12 weeks) in a woman of menstrual age is helpful to ensure that an acute hemorrhagic cyst has not been mistaken for an endometrioma. Cystic masses with classic features of an endometrioma should be followed with US if they are not removed surgically. The frequency of follow-up is variable, and should be based on factors such as the patient’s age and clinical symptoms, such as pain. In general follow-up should be at least yearly, to ensure that the cyst is not progressively enlarging and not changing in internal architecture (for example, new development of a solid element).
About 1% of endometriomas are believed to undergo malignant transformation, usually endometrioid or clear cell carcinoma (60). Malignancy is uncommon in endometriomas smaller than 6 cm, and most malignancies occur in endometriomas larger than 9 cm (60,61). The majority of women with carcinoma in an endometrioma are older than 45 years (61). The mean latency period for development of carcinoma is 4.5 years (range, 1–16 years), with shorter latency periods in older women (60). Rapid cyst growth or development of a significant solid component with flow at Doppler US should raise concern for malignancy. The panel recognized that a minority of benign endometriomas will have small solid-appearing areas (27,62), sometimes even with flow at Doppler US (63), and these are in the indeterminate category, which is discussed below.
Dermoid.—We considered the term “dermoid” to be synonymous with mature cystic teratoma of the ovary. Sonographic features that are considered classic for a dermoid, and that allow a confident diagnosis are: focal or diffuse hyperechoic components, hyperechoic lines and dots, and area of acoustic shadowing, with no internal flow at color Doppler US (33,38,64–66). Additionally, floating spherical structures, though uncommon, allow a confident diagnosis (67). Masses with features classic for a dermoid usually do not need other imaging modalities to establish the diagnosis but should generally be followed with US at an initial interval of between 6 months and 1 year, regardless of age, if they are not removed. The purpose of follow-up is to ensure that the lesion is not changing in size or internal architecture.
Malignant transformation, reported in 0.17%–2% of dermoids, is almost exclusively due to squamous cell carcinoma and tends to occur in women older than 50 years and in tumors larger than 10 cm, although malignant transformation has been reported in tumors as small as 3 cm (68–71). Most dermoids are detected 15–20 years before they undergo malignant transformation (68,70). Reliable sonographic features to predict malignant transformation have not been established, but malignancy should be considered if there are isoechoic (echogenicity similar to the wall of the cyst) branching structures (72), solid areas with flow at Doppler US (69,73), or invasion into adjacent organs. Benign teratomas may have flow detected peripherally at color Doppler US, but malignancy should be considered if flow is seen centrally since it is unusual to see central flow in a benign teratoma (74,75).
Hydrosalpinx.—Sonographic features that are considered classic for a hydrosalpinx, and that allow a confident diagnosis, are a tubular shaped cystic mass with either short round projections (ie, small nodules generally < 3 mm, also known as “beads on a string” appearance representing the endosalpingeal folds) or a waist sign (ie, indentations on opposite sides) (26,33,38). The hydrosalpinx should be seen separate from the ipsilateral ovary. Incomplete septations may allow the imager to appreciate the tubular nature of the cyst. Cine clips or three-dimensional imaging (including inversion mode imaging) may be helpful in establishing the diagnosis in some cases with uncertain features on two-dimensional US images. Masses with features classic for a hydrosalpinx do not need further imaging or follow-up to establish the diagnosis. The frequency of follow-up is variable and should be based on factors such as patient’s age and clinical symptoms.
Peritoneal inclusion cyst.—Peritoneal inclusion cysts, sometimes termed peritoneal pseudocysts, are typically seen in patients with prior pelvic surgery, endometriosis, or pelvic inflammatory disease. Sonographic features that are considered classic for a peritoneal inclusion cyst, and that allow a confident diagnosis, are a cystic mass in which the ovary is either at the edge of the mass or suspended within the mass (17,33). Such masses usually have septations and often follow the contour of adjacent pelvic organs or peritoneal cavity, although they can occasionally be spherical or ovoid (38). The septations can have flow detected at Doppler US. Masses with features classic for a peritoneal inclusion cyst do not need further imaging or follow-up to establish the diagnosis. If the appearance is not classic for a peritoneal inclusion cyst, then alternative imaging may be required. The need for, and frequency of, follow-up is variable and should be based on factors such as patient’s age and clinical symptoms.
Cysts with Indeterminate, but Probably Benign, Characteristics: Sonographic Features and Recommendations
A number of sonographic features can be seen in both benign and malignant masses. The presence of these sonographic features raises concern for malignancy, but they are not predictive enough to allow a confident determination of either a benign or malignant process. Some of these indeterminate features are less worrisome for malignancy than others.
A cyst that is otherwise simple but has a single thin septation (<3 mm) or a small calcification in the wall is almost always benign. Such cysts should be followed in a similar fashion as a simple cyst, as indicated by patient age and cyst size.
Another type of indeterminate cyst is one with features that are suggestive, but not sufficiently classic to allow a confident diagnosis, of hemorrhagic cyst, endometrioma, or dermoid. The panel reached the following consensus recommendations for such cysts:
1. In women of reproductive age or women in early postmenopause: Follow-up US should be performed in 6–12 weeks. Resolution of the lesion confirms a hemorrhagic cyst. If the lesion is unchanged, then hemorrhagic cyst is unlikely, and continued follow-up with either US or MR imaging should then be considered. If these studies do not confirm an endometrioma or dermoid, then surgical evaluation should be considered.
2. In postmenopausal women: Consider surgical evaluation.
Features that we would specifically consider as indeterminate are multiple thin septations or a solid nodule without detectable flow at Doppler US. These findings are suggestive of neoplasms, most often benign. Irregularity or tiny areas of focal thickening of the cyst wall may be difficult to distinguish from a small solid component and thus are indeterminate for malignancy. Cysts with either of these indeterminate features merit more attention than the previously described cysts with typical benign sonographic findings. In a woman of reproductive age, this entails a short-interval follow-up (6–12 weeks) with US or occasionally further characterization with MR imaging (1). MR imaging may be particularly helpful to confirm absence of MR contrast enhancement in sonographically solid-appearing areas that do not have demonstrable flow at Doppler US. We believe a short-interval follow-up of 6–12 weeks with US should allow for sufficient time for a physiologic cyst to resolve, but should be at a different phase of the menstrual cycle, ideally during days 3 to 10 of the menstrual cycle, so that the development of a new cyst does not complicate the interpretation. The larger the cyst the more time it may take to resolve. If the lesion persists, and continues to have indeterminate findings at US or MR imaging, surgical evaluation should be considered. Although size cannot be used to distinguish between benign and malignant cysts, once cyst size increases above 10 cm, the lesion has a 13% chance of being malignant (15).
Cysts with Characteristics Worrisome for Malignancy: Sonographic Features and Recommendations
Thick septations (≥3 mm), solid elements with flow at Doppler US, and focal areas of wall thickening (≥3 mm) are very worrisome for a malignant neoplasm, particularly when seen in association with omental or peritoneal masses or a moderate or large amount of ascitic fluid in the pelvis (7,76). A cyst with a nodule that has internal blood flow has the highest likelihood of being malignant (7). Therefore, these lesions do not need follow-up imaging but rather should be considered for surgical evaluation.
Consensus Statement
The consensus recommendations are summarized in the Figure. These recommendations were developed to assist health care providers in deciding which asymptomatic ovarian and other adnexal cystic masses can be ignored and which should be followed with US (or MR imaging) or surgically evaluated. The recommendations were based on the state of knowledge and available data at the time of the consensus conference (October 2009), and it is understood that as research continues, the recommendations regarding management of adnexal cysts may change.
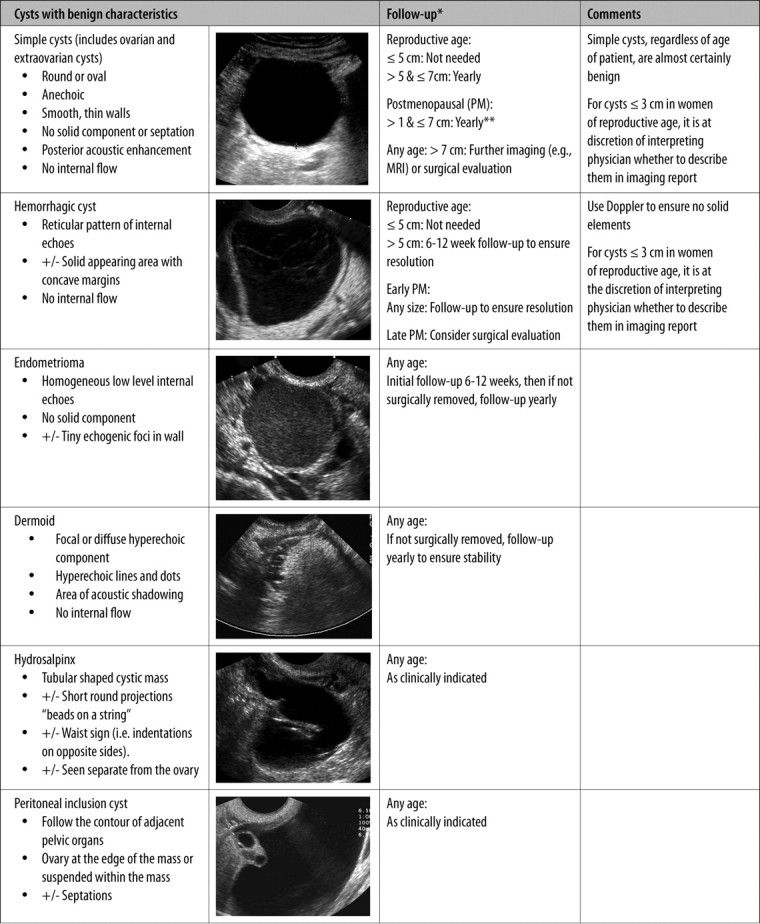
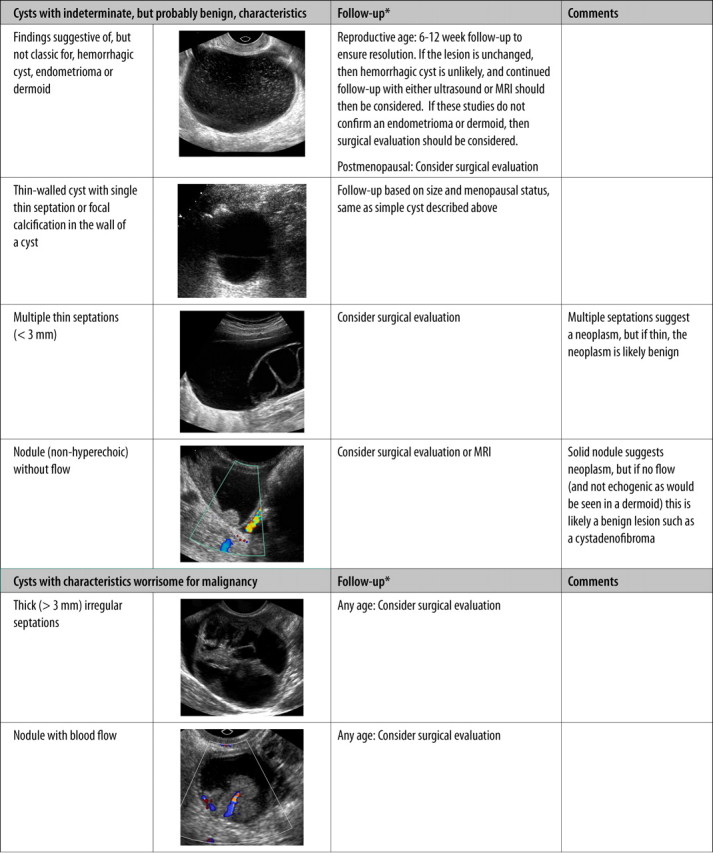
Summary of recommendations for management of asymptomatic ovarian and other adnexal cysts. * = Follow-up recommendations are for US, unless otherwise indicated. ** = Some practices may choose a threshold size slightly higher than 1 cm before recommending yearly follow-up. Practices may choose to decrease the frequency of follow-up once stability or decrease in size has been confirmed.
The goal of sonographic assessment of an adnexal mass is to determine if it is likely benign or if it is indeterminate or malignant. Those masses in the physiologic range in size and appearance in a woman of menstrual age, or a simple adnexal cyst smaller than or equal to 1 cm in a postmenopausal woman, are likely benign. These findings are almost always of no clinical importance in asymptomatic women and can be safely ignored.
Simple cysts larger than 3 cm in women of reproductive age or larger than 1 cm in postmenopausal women should be described in US reports. Although simple cysts of any size are unlikely to be malignant lesions, the consensus was that since sonographic follow-up is a low-risk procedure, it is reasonable to perform yearly sonographic follow-up on cysts larger than 5 cm in premenopausal women and 1 cm in postmenopausal women. The 5-cm limit was also used for the recommendation of follow-up in classic-appearing hemorrhagic cysts in premenopausal women.
Dermoids and endometriomas, given their typical slow growth and small potential for associated malignancy should be followed with US yearly, at least initially. It is possible that the follow-up interval could be lengthened once consistent stability has been demonstrated, but the panel recognized that we do not know when this is appropriate. Hydrosalpinx and peritoneal inclusion cysts need not be followed, unless the patient develops symptoms that warrant follow-up.
Cysts that have thick septations, nodules with blood flow, or focal areas of wall thickening have a substantial likelihood of malignancy. Surgical evaluation should be strongly considered for these cysts.
Recommendations for Future Research
There are many areas for future research that will further our ability to appropriately diagnose and follow adnexal cysts. The panel recommended the following areas for particular attention:
1. Long-term follow-up to elucidate the natural history of adnexal masses that, by the guidelines described in this document, will be followed with imaging rather than surgically removed. This includes simple cysts, cysts with thin septations, and cysts with focal wall calcification. This may allow us to know how often clinicians follow recommendations for follow-up as well as when a mass may no longer need follow-up.
2. Investigation of suspected endometriomas that have a solid-appearing component, to determine features that allow a confident diagnosis of endometrioma, and thus allow the lesion to be followed if there are no clinical indications for surgical removal.
3. Refinement of the clinical importance of three-dimensional and Doppler US findings.
4. Investigation into structured reporting of adnexal cysts to allow for improved communication of results and recommendations for follow-up.
5. Investigations into the role of contrast-enhanced US and other new techniques for tissue characterization in assessment of adnexal cysts.
6. Assessment of noninvasive methods for identification of early ovarian cancer.
Acknowledgments
We thank Phil Ralls, MD, President of the Society of Radiologists in Ultrasound at the time of the Consensus Conference, for his efforts in the development of the conference. We also thank Susan Roberts, Executive Director of the SRU, and Justine Wood, Senior Meeting Manager of the American College of Radiology, for their invaluable assistance in planning and facilitating the Consensus Conference.
Received Jan 27, 2010; revision requested Mar 8; revision received Mar 30; accepted Mar 31; final version accepted Apr 5.
Authors stated no financial relationship to disclose.
Abbreviation:
- SRU
- Society of Radiologists in Ultrasound
References
- 1.American College of Radiology ACR Appropriateness Criteria: clinically suspected adnexal masses. http://www.acr.org/SecondaryMainMenuCategories/quality_safety/app_criteria/pdf/ExpertPanelonWomensImaging/SuspectedAdnexalMassesDoc11.aspx Accessed September 2009.
- 2.Valentin L, Ameye L, Jurkovic D, et al. Which extrauterine pelvic masses are difficult to correctly classify as benign or malignant on the basis of ultrasound findings and is there a way of making a correct diagnosis? Ultrasound Obstet Gynecol 2006;27(4):438–444. [DOI] [PubMed] [Google Scholar]
- 3.Barney SP, Muller CY, Bradshaw KD. Pelvic masses. Med Clin North Am 2008;92(5):1143–1161,xi. [DOI] [PubMed] [Google Scholar]
- 4.Allison KH, Swisher EM, Kerkering KM, Garcia RL. Defining an appropriate threshold for the diagnosis of serous borderline tumor of the ovary: when is a full staging procedure unnecessary? Int J Gynecol Pathol 2008;27(1):10–17. [DOI] [PubMed] [Google Scholar]
- 5.American College of Obstetricians anf Gynecologists ACOG Committee Opinion: number 280, December 2002. The role of the generalist obstetrician-gynecologist in the early detection of ovarian cancer. Obstet Gynecol 2002;100(6):1413–1416. [DOI] [PubMed] [Google Scholar]
- 6.American College of Obstetricians and Gynecologists ACOG Practice Bulletin. Management of adnexal masses. Obstet Gynecol 2007;110(1):201–214. [DOI] [PubMed] [Google Scholar]
- 7.Brown DL, Doubilet PM, Miller FH, et al. Benign and malignant ovarian masses: selection of the most discriminating gray-scale and Doppler sonographic features. Radiology 1998;208(1):103–110. [DOI] [PubMed] [Google Scholar]
- 8.Burger HG, Hale GE, Dennerstein L, Robertson DM. Cycle and hormone changes during perimenopause: the key role of ovarian function. Menopause 2008;15(4):603–612. [DOI] [PubMed] [Google Scholar]
- 9.Canis M, Botchorishvili R, Manhes H, et al. Management of adnexal masses: role and risk of laparoscopy. Semin Surg Oncol 2000;19(1):28–35. [DOI] [PubMed] [Google Scholar]
- 10.Dearking AC, Aletti GD, McGree ME, Weaver AL, Sommerfield MK, Cliby WA. How relevant are ACOG and SGO guidelines for referral of adnexal mass? Obstet Gynecol 2007;110(4):841–848. [DOI] [PubMed] [Google Scholar]
- 11.Dehari R, Kurman RJ, Logani S, Shih IeM. The development of high-grade serous carcinoma from atypical proliferative (borderline) serous tumors and low-grade micropapillary serous carcinoma: a morphologic and molecular genetic analysis. Am J Surg Pathol 2007;31(7):1007–1012. [DOI] [PubMed] [Google Scholar]
- 12.Exacoustos C, Zupi E, Amadio A, et al. Laparoscopic removal of endometriomas: sonographic evaluation of residual functioning ovarian tissue. Am J Obstet Gynecol 2004;191(1):68–72. [DOI] [PubMed] [Google Scholar]
- 13.Firouzabadi RD, Sekhavat L, Javedani M. The effect of ovarian cyst aspiration on IVF treatment with GnRH. Arch Gynecol Obstet 2010;281(3):545–549. [DOI] [PubMed] [Google Scholar]
- 14.Geomini P, Kruitwagen R, Bremer GL, Cnossen J, Mol BW. The accuracy of risk scores in predicting ovarian malignancy: a systematic review. Obstet Gynecol 2009;113(2 Pt 1):384–394. [DOI] [PubMed] [Google Scholar]
- 15.Ghezzi F, Cromi A, Bergamini V, et al. Should adnexal mass size influence surgical approach? A series of 186 laparoscopically managed large adnexal masses. BJOG 2008;115(8):1020–1027. [DOI] [PubMed] [Google Scholar]
- 16.Goldstein SR, Subramanyam B, Snyder JR, Beller U, Raghavendra BN, Beckman EM. The postmenopausal cystic adnexal mass: the potential role of ultrasound in conservative management. Obstet Gynecol 1989;73(1):8–10. [PubMed] [Google Scholar]
- 17.Guerriero S, Ajossa S, Mais V, Angiolucci M, Paoletti AM, Melis GB. Role of transvaginal sonography in the diagnosis of peritoneal inclusion cysts. J Ultrasound Med 2004;23(9):1193–1200. [DOI] [PubMed] [Google Scholar]
- 18.Guerriero S, Alcazar JL, Pascual MA, et al. Diagnosis of the most frequent benign ovarian cysts: is ultrasonography accurate and reproducible? J Womens Health (Larchmt) 2009;18(4):519–527. [DOI] [PubMed] [Google Scholar]
- 19.Hart WR. Mucinous tumors of the ovary: a review. Int J Gynecol Pathol 2005;24(1):4–25. [PubMed] [Google Scholar]
- 20.Hertzberg BS, Kliewer MA. Sonography of benign cystic teratoma of the ovary: pitfalls in diagnosis. AJR Am J Roentgenol 1996;167(5):1127–1133. [DOI] [PubMed] [Google Scholar]
- 21.Im SS, Gordon AN, Buttin BM, et al. Validation of referral guidelines for women with pelvic masses. Obstet Gynecol 2005;105(1):35–41. [DOI] [PubMed] [Google Scholar]
- 22.Kinkel K, Hricak H, Lu Y, Tsuda K, Filly RA. US characterization of ovarian masses: a meta-analysis. Radiology 2000;217(3):803–811. [DOI] [PubMed] [Google Scholar]
- 23.Levanon K, Crum C, Drapkin R. New insights into the pathogenesis of serous ovarian cancer and its clinical impact. J Clin Oncol 2008;26(32):5284–5293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Levine D, Gosink BB, Wolf SI, Feldesman MR, Pretorius DH. Simple adnexal cysts: the natural history in postmenopausal women. Radiology 1992;184(3):653–659. [DOI] [PubMed] [Google Scholar]
- 25.Liu J, Xu Y, Wang J. Ultrasonography, computed tomography and magnetic resonance imaging for diagnosis of ovarian carcinoma. Eur J Radiol 2007;62(3):328–334. [DOI] [PubMed] [Google Scholar]
- 26.Patel MD, Acord DL, Young SW. Likelihood ratio of sonographic findings in discriminating hydrosalpinx from other adnexal masses. AJR Am J Roentgenol 2006;186(4):1033–1038. [DOI] [PubMed] [Google Scholar]
- 27.Patel MD, Feldstein VA, Chen DC, Lipson SD, Filly RA. Endometriomas: diagnostic performance of US. Radiology 1999;210(3):739–745. [DOI] [PubMed] [Google Scholar]
- 28.Patel MD, Feldstein VA, Filly RA. The likelihood ratio of sonographic findings for the diagnosis of hemorrhagic ovarian cysts. J Ultrasound Med 2005;24(5):607–614; quiz 615. [DOI] [PubMed] [Google Scholar]
- 29.Patlas M, Rosen B, Chapman W, Wilson SR. Sonographic diagnosis of primary malignant tumors of the fallopian tube. Ultrasound Q 2004;20(2):59–64. [DOI] [PubMed] [Google Scholar]
- 30.Savelli L, Ghi T, De Iaco P, Ceccaroni M, Venturoli S, Cacciatore B. Paraovarian/paratubal cysts: comparison of transvaginal sonographic and pathological findings to establish diagnostic criteria. Ultrasound Obstet Gynecol 2006;28(3):330–334. [DOI] [PubMed] [Google Scholar]
- 31.Seungdamrong A, Weiss G.. Ovulation in a postmenopausal woman. Fertil Steril 2007;88:1438.e–1438.e2. doi:10.1016/j.fertnstert.2006.11.152. Published February 12, 2007. [DOI] [PubMed] [Google Scholar]
- 32.Shih IeM, Kurman RJ. Ovarian tumorigenesis: a proposed model based on morphological and molecular genetic analysis. Am J Pathol 2004;164(5):1511–1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sokalska A, Timmerman D, Testa AC, et al. Diagnostic accuracy of transvaginal ultrasound examination for assigning a specific diagnosis to adnexal masses. Ultrasound Obstet Gynecol 2009;34(4):462–470. [DOI] [PubMed] [Google Scholar]
- 34.Strandell A. The influence of hydrosalpinx on IVF and embryo transfer: a review. Hum Reprod Update 2000;6(4):387–395. [DOI] [PubMed] [Google Scholar]
- 35.Stroud JS, Mutch D, Rader J, Powell M, Thaker PH, Grigsby PW. Effects of cancer treatment on ovarian function. Fertil Steril 2009;92(2):417–427. [DOI] [PubMed] [Google Scholar]
- 36.Timmerman D, Valentin L, Bourne TH, Collins WP, Verrelst H, Vergote I International Ovarian Tumor Analysis (IOTA) Group . Terms, definitions and measurements to describe the sonographic features of adnexal tumors: a consensus opinion from the International Ovarian Tumor Analysis (IOTA) Group. Ultrasound Obstet Gynecol 2000;16(5):500–505. [DOI] [PubMed] [Google Scholar]
- 37.Timor-Tritsch IE, Goldstein SR. The complexity of a “complex mass” and the simplicity of a “simple cyst”. J Ultrasound Med 2005;24(3):255–258. [DOI] [PubMed] [Google Scholar]
- 38.Valentin L. Use of morphology to characterize and manage common adnexal masses. Best Pract Res Clin Obstet Gynaecol 2004;18(1):71–89. [DOI] [PubMed] [Google Scholar]
- 39.Vallerie AM, Lerner JP, Wright JD, Baxi LV. Peritoneal inclusion cysts: a review. Obstet Gynecol Surv 2009;64(5):321–334. [DOI] [PubMed] [Google Scholar]
- 40.Wolf SI, Gosink BB, Feldesman MR, et al. Prevalence of simple adnexal cysts in postmenopausal women. Radiology 1991;180(1):65–71. [DOI] [PubMed] [Google Scholar]
- 41.Zanetta G, Rota S, Chiari S, Bonazzi C, Bratina G, Mangioni C. Behavior of borderline tumors with particular interest to persistence, recurrence, and progression to invasive carcinoma: a prospective study. J Clin Oncol 2001;19(10):2658–2664. [DOI] [PubMed] [Google Scholar]
- 42.Lobo RA. Menopause: endocrinology, consequences of estrogen deficiency, effects of hormone replacement therapy, treatment regimens. In: , Katz VL, Lentz GM, Lobo RA, Gershenson DM, eds. Comprehensive Gyncology. 5th ed Philadelphia, PA: Mosby Elsevier, 2007; 1039–1071. [Google Scholar]
- 43.te Velde ER, Pearson PL. The variability of female reproductive ageing. Hum Reprod Update 2002;8(2):141–154. [DOI] [PubMed] [Google Scholar]
- 44.Soules MR, Sherman S, Parrott E, et al. Executive summary: Stages of Reproductive Aging Workshop (STRAW). Fertil Steril 2001;76(5):874–878. [DOI] [PubMed] [Google Scholar]
- 45.Bakos O, Lundkvist O, Wide L, Bergh T. Ultrasonographical and hormonal description of the normal ovulatory menstrual cycle. Acta Obstet Gynecol Scand 1994;73(10):790–796. [DOI] [PubMed] [Google Scholar]
- 46.Ritchie WGM. Sonographic evaluation of normal and induced ovulation. Radiology 1986;161(1):1–10. [DOI] [PubMed] [Google Scholar]
- 47.Baerwald AR, Adams GP, Pierson RA. Form and function of the corpus luteum during the human menstrual cycle. Ultrasound Obstet Gynecol 2005;25(5):498–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bourne TH, Hagström H, Hahlin M, et al. Ultrasound studies of vascular and morphological changes in the human corpus luteum during the menstrual cycle. Fertil Steril 1996;65(4):753–758. [PubMed] [Google Scholar]
- 49.Durfee SM, Frates MC. Sonographic spectrum of the corpus luteum in early pregnancy: gray-scale, color, and pulsed Doppler appearance. J Clin Ultrasound 1999;27(2):55–59. [DOI] [PubMed] [Google Scholar]
- 50.Sokalska A, Valentin L. Changes in ultrasound morphology of the uterus and ovaries during the menopausal transition and early postmenopause: a 4-year longitudinal study. Ultrasound Obstet Gynecol 2008;31(2):210–217. [DOI] [PubMed] [Google Scholar]
- 51.Healy DL, Bell R, Robertson DM, et al. Ovarian status in healthy postmenopausal women. Menopause 2008;15(6):1109–1114. [DOI] [PubMed] [Google Scholar]
- 52.Castillo G, Alcázar JL, Jurado M. Natural history of sonographically detected simple unilocular adnexal cysts in asymptomatic postmenopausal women. Gynecol Oncol 2004;92(3):965–969. [DOI] [PubMed] [Google Scholar]
- 53.World Health Organization Classification of Tumours Working Group on Gynecologic Tumours Tumors of the ovary and peritoneum. In: Tavassoli FA, Devilee P, eds. Pathology and genetics: tumours of the breast and female genital organs. Lyon, France: IARC Press, 2003; 124–127. [Google Scholar]
- 54.Gramellini D, Fieni S, Sanapo L, Casilla G, Verrotti C, Nardelli GB. Diagnostic accuracy of IOTA ultrasound morphology in the hands of less experienced sonographers. Aust N Z J Obstet Gynaecol 2008;48(2):195–201. [DOI] [PubMed] [Google Scholar]
- 55.Seidman JD, Kurman RJ. Ovarian serous borderline tumors: a critical review of the literature with emphasis on prognostic indicators. Hum Pathol 2000;31(5):539–557. [DOI] [PubMed] [Google Scholar]
- 56.Ekerhovd E, Wienerroith H, Staudach A, Granberg S. Preoperative assessment of unilocular adnexal cysts by transvaginal ultrasonography: a comparison between ultrasonographic morphologic imaging and histopathologic diagnosis. Am J Obstet Gynecol 2001;184(2):48–54. [DOI] [PubMed] [Google Scholar]
- 57.Modesitt SC, Pavlik EJ, Ueland FR, DePriest PD, Kryscio RJ, van Nagell JR. Risk of malignancy in unilocular ovarian cystic tumors less than 10 centimeters in diameter. Obstet Gynecol 2003;102(3):594–599. [DOI] [PubMed] [Google Scholar]
- 58.Alcázar JL, Castillo G, Jurado M, García GL. Is expectant management of sonographically benign adnexal cysts an option in selected asymptomatic premenopausal women? Hum Reprod 2005;20(11):3231–3234. [DOI] [PubMed] [Google Scholar]
- 59.Okai T, Kobayashi K, Ryo E, Kagawa H, Kozuma S, Taketani Y. Transvaginal sonographic appearance of hemorrhagic functional ovarian cysts and their spontaneous regression. Int J Gynaecol Obstet 1994;44(1):47–52. [DOI] [PubMed] [Google Scholar]
- 60.Kawaguchi R, Tsuji Y, Haruta S, et al. Clinicopathologic features of ovarian cancer in patients with ovarian endometrioma. J Obstet Gynaecol Res 2008;34(5):872–877. [DOI] [PubMed] [Google Scholar]
- 61.Kobayashi H, Sumimoto K, Kitanaka T, et al. Ovarian endometrioma—risks factors of ovarian cancer development. Eur J Obstet Gynecol Reprod Biol 2008;138(2):187–193. [DOI] [PubMed] [Google Scholar]
- 62.Alcázar JL, Laparte C, Jurado M, López-García G. The role of transvaginal ultrasonography combined with color velocity imaging and pulsed Doppler in the diagnosis of endometrioma. Fertil Steril 1997;67(3):487–491. [DOI] [PubMed] [Google Scholar]
- 63.Guerriero S, Ajossa S, Mais V, Risalvato A, Lai MP, Melis GB. The diagnosis of endometriomas using colour Doppler energy imaging. Hum Reprod 1998;13(6):1691–1695. [DOI] [PubMed] [Google Scholar]
- 64.Caspi B, Appelman Z, Rabinerson D, Elchalal U, Zalel Y, Katz Z. Pathognomonic echo patterns of benign cystic teratomas of the ovary: classification, incidence and accuracy rate of sonographic diagnosis. Ultrasound Obstet Gynecol 1996;7(4):275–279. [DOI] [PubMed] [Google Scholar]
- 65.Mais V, Guerriero S, Ajossa S, Angiolucci M, Paoletti AM, Melis GB. Transvaginal ultrasonography in the diagnosis of cystic teratoma. Obstet Gynecol 1995;85(1):48–52. [DOI] [PubMed] [Google Scholar]
- 66.Patel MD, Feldstein VA, Lipson SD, Chen DC, Filly RA. Cystic teratomas of the ovary: diagnostic value of sonography. AJR Am J Roentgenol 1998;171(4):1061–1065. [DOI] [PubMed] [Google Scholar]
- 67.Umesaki N, Nagamatsu A, Yada C, Tanaka T. MR and ultrasound imaging of floating globules in mature ovarian cystic teratoma. Gynecol Obstet Invest 2004;58(3):130–132. [DOI] [PubMed] [Google Scholar]
- 68.Hackethal A, Brueggmann D, Bohlmann MK, Franke FE, Tinneberg HR, Münstedt K. Squamous-cell carcinoma in mature cystic teratoma of the ovary: systematic review and analysis of published data. Lancet Oncol 2008;9(12):1173–1180. [DOI] [PubMed] [Google Scholar]
- 69.Park JY, Kim DY, Kim JH, Kim YM, Kim YT, Nam JH. Malignant transformation of mature cystic teratoma of the ovary: experience at a single institution. Eur J Obstet Gynecol Reprod Biol 2008;141(2):173–178. [DOI] [PubMed] [Google Scholar]
- 70.Rim SY, Kim SM, Choi HS. Malignant transformation of ovarian mature cystic teratoma. Int J Gynecol Cancer 2006;16(1):140–144. [DOI] [PubMed] [Google Scholar]
- 71.Yamanaka Y, Tateiwa Y, Miyamoto H, et al. Preoperative diagnosis of malignant transformation in mature cystic teratoma of the ovary. Eur J Gynaecol Oncol 2005;26(4):391–392. [PubMed] [Google Scholar]
- 72.Mlikotic A, McPhaul L, Hansen GC, Sinow RM. Significance of the solid component in predicting malignancy in ovarian cystic teratomas: diagnostic considerations. J Ultrasound Med 2001;20(8):859–866; quiz 867. [DOI] [PubMed] [Google Scholar]
- 73.Emoto M, Obama H, Horiuchi S, Miyakawa T, Kawarabayashi T. Transvaginal color Doppler ultrasonic characterization of benign and malignant ovarian cystic teratomas and comparison with serum squamous cell carcinoma antigen. Cancer 2000;88(10):2298–2304. [DOI] [PubMed] [Google Scholar]
- 74.Zalel Y, Caspi B, Tepper R. Doppler flow characteristics of dermoid cysts: unique appearance of struma ovarii. J Ultrasound Med 1997;16(5):355–358. [PubMed] [Google Scholar]
- 75.Zalel Y, Seidman DS, Oren M, et al. Sonographic and clinical characteristics of struma ovarii. J Ultrasound Med 2000;19(12):857–861. [DOI] [PubMed] [Google Scholar]
- 76.Sassone AM, Timor-Tritsch IE, Artner A, Westhoff C, Warren WB. Transvaginal sonographic characterization of ovarian disease: evaluation of a new scoring system to predict ovarian malignancy. Obstet Gynecol 1991;78(1):70–76. [PubMed] [Google Scholar]