Abstract
BACKGROUND
Art therapies are advocated by national bodies, such as the United Kingdom’s National Institute for Health and Care Excellence, to alleviate the negative symptoms associated with schizophrenia. The last decade has however, seen several new larger well-controlled trials published suggesting an update is timely.
AIM
To asses randomised controlled trials (RCT) of art therapies for reducing the symptoms of schizophrenia – particularly negative symptoms.
METHODS
Searches of PubMed and Scopus were conducted until May 2019 for RCTs examining the impact of art therapies on psychosis (positive, negative and total) symptoms in people diagnosed with schizophrenia. Study quality was assessed using the Cochrane risk of bias tool. Random effects meta-analyses were used to derive overall effect sizes. Moderator analyses were conducted using both meta-regression and categorical comparisons.
RESULTS
We identified 133 articles, of which 9 RCTs involving 948 participants (475 assigned to art therapies and 473 controls) met our inclusion criteria. Using random effects models, we calculated pooled effect sizes (Hedges g) for end-of-trial symptomatic outcomes. Effect sizes both for total symptoms [g = -0.27, 95% confidence interval (CI) -0.60 to 0.05, k = 6] and for positive symptoms (g = -0.10, 95%CI -0.35 to 0.15, k = 6) were non-significant; however, we did find significant reduction of negative symptoms (g = -0.42, 95%CI -0.70 to -0.14, k = 9). Meta-regression revealed that negative symptom reduction was larger in trials with a greater proportion of women and in trials with younger patients. Crucially, the negative symptom reduction following art therapies was limited to lower quality trials and did not emerge in trials that used blind assessment of outcomes.
CONCLUSION
This review presents a comprehensive meta-analysis of art therapies in schizophrenia in terms of both studies included and participant numbers. We found that art therapies did not significantly reduce total or positive symptoms. A "small" therapeutic effect was found for negative symptoms, but we show that the effect is not present in blind trials and may be subject to publication bias.
Keywords: Schizophrenia, Symptoms, Art therapy, Meta-analysis, Bias
Core tip: This meta-analysis examines data from randomised controlled trials looking at whether art therapies reduce the symptoms of schizophrenia-particularly negative symptoms. Our study indicates that art therapies do not significantly reduce total symptoms or positive symptoms. While we found a "small" therapeutic effect on negative symptoms, the effect appears to reflect two forms of bias-first, no effect emerges when trials use blind outcome assessment; second, the trials also point to the possibility of publication bias.
INTRODUCTION
Over the past 60 years art therapies have been promoted as a medium in which individuals may engage with psychotherapy in a non-judgemental, creative space and has been applied to numerous conditions and situations. Encompassing a variety of non-verbal, creative interventions, arts therapies typically combine the use of art materials and psychotherapeutic techniques with the aim of achieving psychological change, e.g., promoting insight and general well-being. Such interventions include not only traditional art therapy, but also dance therapy, music therapy and body-oriented psychotherapy (a form of therapy that involves an explicit theory of body–mind functioning designed to improve emotional, cognitive, physical and social integration)[1-5].
Adding adjunctive psychological interventions to pharmacotherapy has become more common in efforts to help improve the mental state and functioning of those living with schizophrenia. While much research and debate has centred on the efficacy of Cognitive Behavioural Therapy (CBTp) for psychosis[6-8], much less attention has been paid to the role of art therapies as an adjunctive to medication.
Art therapies may have some potential advantages over more traditional talk-based psychological interventions for those diagnosed with schizophrenia. For example, individuals experiencing the negative symptoms of schizophrenia (e.g., impoverished speech) may find it difficult to verbally communicate their thoughts and emotions to a conventional therapist. Art therapies therefore are unique in their potential to circumvent this obstacle, with a nuanced relationship between the service-user, the therapist and the artwork itself[6].
The first systematic review undertaken by the Cohrane Collaboration[9] was limited to two small underpowered traditional art therapy trials and they concluded that “There is no evidence to support the use of art therapy as part of policy” (p. 12). The Cochrane review was updated two years later[10] although it failed to locate any further studies. Later meta-analyses by the National Institute of Clinical Excellence (NICE, 2009)[11] refer more broadly to art therapies (including art therapy or art psychotherapy, dance movement therapy, body psychotherapy, drama therapy and music therapy) and featured 5 randomised controlled trials (RCTs). While NICE reported that art therapies did not significantly reduce total symptoms [-0.49 (-0.98 to 0.01), k = 4] or positive symptoms [0.06 (-0.67 to 0.79), k = 2] at end-of-trial, they reported a significant benefit in reducing negative symptoms [-0.59 (-0.83 to -0.36), k = 5]. Nonetheless, the findings were somewhat limited– based on five trials involving only 148 receiving art therapies and 146 controls in total. Despite this, the NICE recommendation 1.4.4.3 asserts that “…clinicians should offer art therapies to all people with schizophrenia, particularly for the alleviation of negative symptoms”. As currently practised in the United Kingdom, arts therapies comprise: Art therapy or art psychotherapy, dance movement therapy, body psychotherapy, drama therapy and music therapy.
By contrast, however, the latest treatment guideline published by the Scottish Intercollegiate Guidelines network (2013)[12], came to a quite different conclusion that “There is insufficient high-quality evidence on which to base any recommendation for arts therapies in general” (p. 25). In a similar vein, and more recently, the Royal Australian and New Zealand College of Psychiatry[13] concluded that the evidence from RCTs “is inconclusive” and that more research and assessment is required before art therapy could be recommended. In the most recent systematic review covering studies published from 2007 onwards, Attard and Larkin (2016)[14] concluded that while “High quality quantitative articles provided inconclusive evidence for the effectiveness of art therapy in adults with psychosis…high-quality qualitative articles indicated that therapists and clients considered art therapy to be a beneficial, meaningful and acceptable intervention, although this conclusion was based on a small number of studies” (our italics).
A central suggestion for future research proposed by NICE in their 2009 CG178 guideline was that "an adequately powered RCT should be conducted to investigate the clinical and cost-effectiveness of arts therapies as compared to an active control in people with schizophrenia" (p. 200). Since this recommendation, the two largest-ever clinical trials have been conducted. Both trials unequivocally reported no significant alleviation of negative symptoms for those receiving art therapies vs their respective control group. Crawford et al[15] note that while “many service users greatly value using art materials and taking part in other creative activities, the widespread referral of people with established schizophrenia to group art therapy as delivered in this study did not lead to measurable improvements in patient outcomes or provide a cost effective use of resources” (p. 41). Slightly more positively perhaps, Priebe et al[16] concluded that their study “…does not support group body psychotherapy as a treatment for negative symptoms of schizophrenia. Reviewing the effectiveness of different arts therapy modalities separately may be informative to determine whether existing guidelines should be more cautious in recommending art and body psychotherapy specifically, or whether this extends to arts therapies as a whole” (p. 7).
Conflicting conclusions concerning the efficacy of art therapies for individuals diagnosed with schizophrenia may reflect several factors including that: Meta-analytic data are now a decade-old, the initial body of clinical research was modest and earlier RCTs may not have been as well-controlled as more recent trials. With several larger, appropriately powered and better-controlled trials published since the NICE guidance in 2009, it seems timely to re-assess whether art therapies aid in alleviating the symptoms of schizophrenia, particularly negative symptoms. This review will also conduct separate analyses assessing any impact on both positive and total symptoms. Finally, we examine whether blinding of the outcome assessment has a mediating effect on results (something that has not been examined in previous meta-analyses, including NICE guidance).
MATERIALS AND METHODS
A literature review was conducted in accordance with Preferred Reporting for Systematic Reviews and Meta-analysis guidelines[17] (for checklist, see appendices). The search strategy involved identifying peer-reviewed articles published in English since the NICE review[9] and so included the period of 2008 to May 2019 (earlier trials were retrieved from the NICE review).
We searched the electronic databases PubMed and Scopus according to the PICO strategy (Patients: Diagnosed with schizophrenia; Intervention: Arts therapies; Comparator: Any control group; and Outcome: Symptom measures). The search terms were comparable to those originally used by NICE and included: (1) “schizophrenia” OR “psychosis” OR “schizo*” paired with the descriptors; (2) “art therapy” OR “arts psychotherapy” OR “creative arts therapy” using all possible combinations. The comparator was a control group of any description and the outcome was negative (positive or total) symptom measures (see below). The electronic search was supplemented by "hand-searching" of obtained article reference lists for any trials not identified by the online searches.
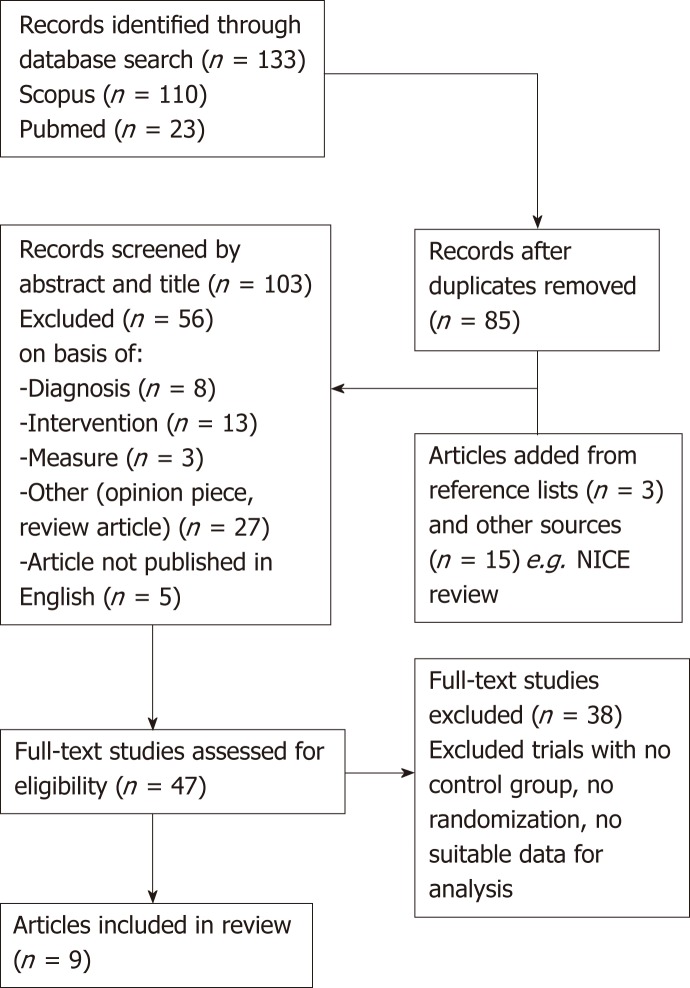
Our inclusion criteria closely mirrored those used by NICE, with studies included (Figure 1) if after the initial screening of title, abstract and keywords, they featured: (1) A formal diagnosis of schizophrenia, in accordance with standardised diagnostic criteria e.g., DSM-V; (2) A randomised control trial with ≥ 10 participants per arm; (3) A parallel control group of any type as a comparator, i.e., an active control, waitlist or treatment as usual; (4) An intervention of art therapy, both individual or group, which could also include variations, i.e., dance therapy, music therapy; (5) Reporting means, standard deviation and sample size for a measure of negative symptoms; and (6) The full-text was available in English.
Figure 1.
PRISMA flow diagram.
Data extraction and procedure
Effect sizes were derived from the post-intervention symptom rating scores using Hedges g (i.e., the standardized mean difference using group means divided by the pooled standard deviation, corrected for the tendency towards overestimation in small studies). The scales used included: the positive and negative symptom subscales of the PANSS, the Schedule for the Assessment of Positive Symptoms, the Schedule for the Assessment of Negative Symptoms; and the Brief Psychiatric Rating Scale. All analyses used random effects models were conducted using Comprehensive Meta-Analysis (Version 2). We examined studies for possible follow-up assessments (ranging from 12 weeks to 2-years after initial post-data measurements); however, the limited number of studies with relevant data meant that no analyses were feasible for follow-up. If data were unavailable in a paper, authors were contacted. Effect sizes are described using Cohen’s convention: an effect size of 0.20 was considered small, 0.50 moderate, and 0.80 large.
Heterogeneity was examined by calculating I². Following Higgins et al[18] (2011), we interpreted I² values of 0-40% as suggesting that heterogeneity may not be important, 30%-60% representing moderate heterogeneity, 50%-90% substantial heterogeneity, and 75%-100% as potentially representing considerable heterogeneity. Potential publication bias was examined using Duval et al[19]’s (2000) trim and fill method.
Data pertaining to participants age (mean age range 35.4 to 41, k = 9), gender (proportion of males: 0.43 to 0.73, k = 9), duration of illness (years: 8.9 to 12.8, k = 5), and the number of therapy sessions (8 to 72, k = 9) were also extracted, for potential moderator analyses using meta-regression. Despite no definitive minimum number of studies being required to complete a meta-regression, a general recommendation proposed by Cochrane is at least 6 to 10 studies for a continuous variable[14]. On this criterion, moderator variables which failed to meet this minimum requirement were not selected for further analysis and as such, meta-regressions were only conducted on gender (percentage of participants that were male) and the total number of therapy sessions in each study; the latter of which was proposed as a topic of future research by NICE[9]. Data relating to blinding the assessment of outcome was extracted to examine any effects on the primary outcome variable i.e., negative symptoms.
Risk of bias was using the Cochrane risk of bias tool (RoB2)[20] covering the following areas of potential bias: Sequence generation, allocation concealment, blinding of participants, blinding of outcome assessors, incomplete outcome data, selective reporting, researcher allegiance.
RESULTS
Following our search a total of 9 articles were included for the final review[15,16,21-27] (Table 1 and Figure 1), providing a sample of 948 participants: 475 randomly assigned to art therapies including conventional art therapy (k = 3), music therapy (k = 3), body-oriented psychotherapy (k = 2) and dance therapy (k = 1); and 473 were assigned to control conditions.
Table 1.
Trials included in the meta-analyses
| Art (n) | Control (n) | Blind assess | Sessions | Control | Art therapy type | |
| Yang et al[21], 1998 | 40 | 30 | No | 6 per week × 3 mo | TAU | Music |
| Röhricht et al[22], 2006 | 24 | 121 | Yes | 20 over 20 wk | Supp couns | Body-oriented psychotherapy |
| Ulrich et al[23], 2007 | 21 | 16 | Yes | Mean = 7.5 | TAU | Music |
| Richardson et al[24], 2007 | 43 | 47 | No | 12 | TAU | Art |
| Talwar et al[25], 2008 | 33 | 48 | Yes | Median = 8 | TAU | Music |
| Crawford et al[15], 2010 | 140 | 137 | Yes | Weekly for 12 mo | Activity | Group art therapy |
| Montag et al[26], 2014 | 16 | 19 | Yes | 12 over 6 wk | TAU | Psychodynamic art therapy |
| Lee et al[27], 2015 | 18 | 20 | No | 1 per week × 12 wk | TAU | Dance/movement |
| Priebe et al[16], 2016 | 140 | 135 | Yes | 20 | Pilates | Body psychotherapy |
Risk of bias
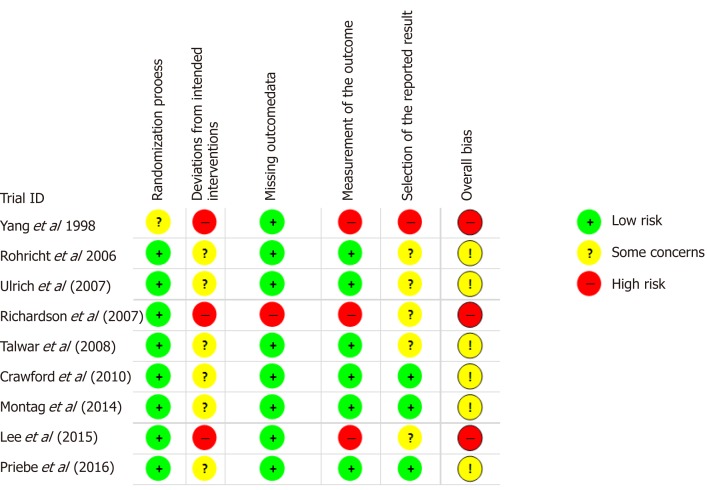
Risk of bias was assessed using the RoB2[16]. The RoB tool assess five areas of potential bias in trials: (1) Bias arising from the randomisation process (randomisation and allocation concealment); (2) Bias due to deviations from intended interventions (blinding of participants and personnel); (3) Bias due to missing data (incomplete outcome data); (4) Bias in measurement of the outcome (blinding of outcome assessment); and (5) bias in selection of the reported result (selective reporting).
Using these criteria, 3 trials were overall at high risk of bias[17,20,23]; the remaining 6 showed "some concern" (Figure 2), largely reflecting the inability of participants to be blind to whether they received the psychological intervention or control.
Figure 2.
Risk of bias in each trial according to the Cochrane RoB2 tool.
Effect sizes
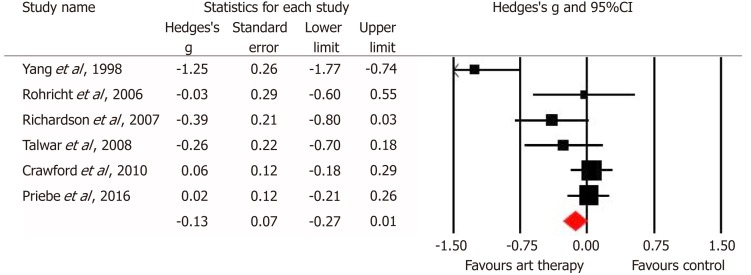
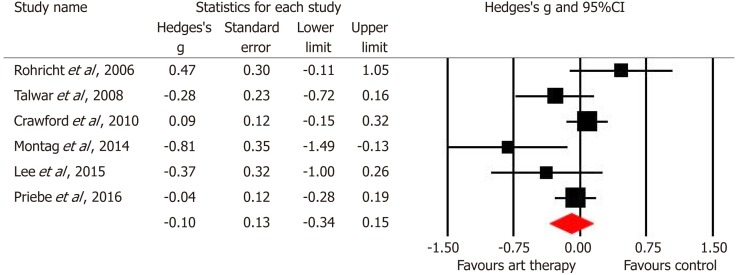
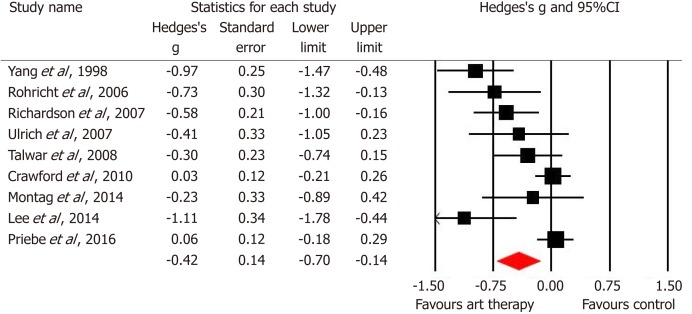
The pooled effects size for the 6 studies of total symptoms was nonsignificant [g = -0.27, 95% confidence interval (CI) -0.60 to 0.05, P = 0.10]. These studies were also heterogeneous (Q = 24.5, P < 0.001) with an I² value of 79.6. For forest plot see Figure 3 (negative sign favours art therapies). The pooled effect size for the 6 studies of positive symptoms was non-significant (g = -0.10, 95%CI -0.34 to 0.15, P = 0.44). The studies were again heterogeneous (Q = 11.2, P = 0.05) with an I² value of 55.4 (Figure 4). The pooled effect size was for negative symptoms in 9 trials was significant (g = -0.42, 95%CI -0.70 to -0.14, P = 0.004). The studies were heterogeneous (Q = 31.3, P < 0.001), with an I² value of 74.4 (Figure 5).
Figure 3.
Forest plot of the studies in the meta-analysis for total symptoms.
Figure 4.
Forest plot of the studies in the meta-analysis for positive symptoms.
Figure 5.
Forest plot of the studies in the meta-analysis for negative symptoms.
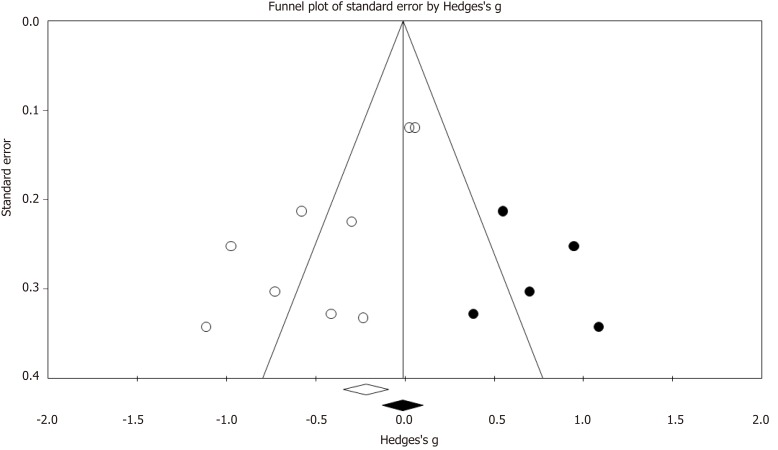
Examination of publication bias was assessed using Duval and Tweedie’s trim and fill[19], indicated 5 potentially missing studies–adjusting for these studies reduced the effect size to -0.01 (95%CI -0.13 to 0.10), which became nonsignificant (Figure 6). We also analysed possible bias using Egger’s[28] regression intercept and this confirmed significant funnel plot asymmetry (P < 0.01; 2 tailed).
Figure 6.
Funnell plot outlining trim and fill estimates for imputed missing trials (dark circles) for negative symptoms.
Moderator analyses
Meta-regressions were run on samples with a minimum of 6 trials[18], which included the influence of gender (the proportion of male participants) and the number of therapy sessions. Table 2 provides a summary of the meta-regressions completed in this review (see below).
Table 2.
Meta-regressions findings for moderator variables
| Moderator variable | k | Q-statistic |
| Age | 9 | Q = 4.66, df = 1, P = 0.02 |
| Percentage of female participants (%) | 9 | Q = 5.10, df = 1, P = 0.02 |
| Number of therapy sessions | 9 | Q = 0.07, df = 1, P = 0.78 |
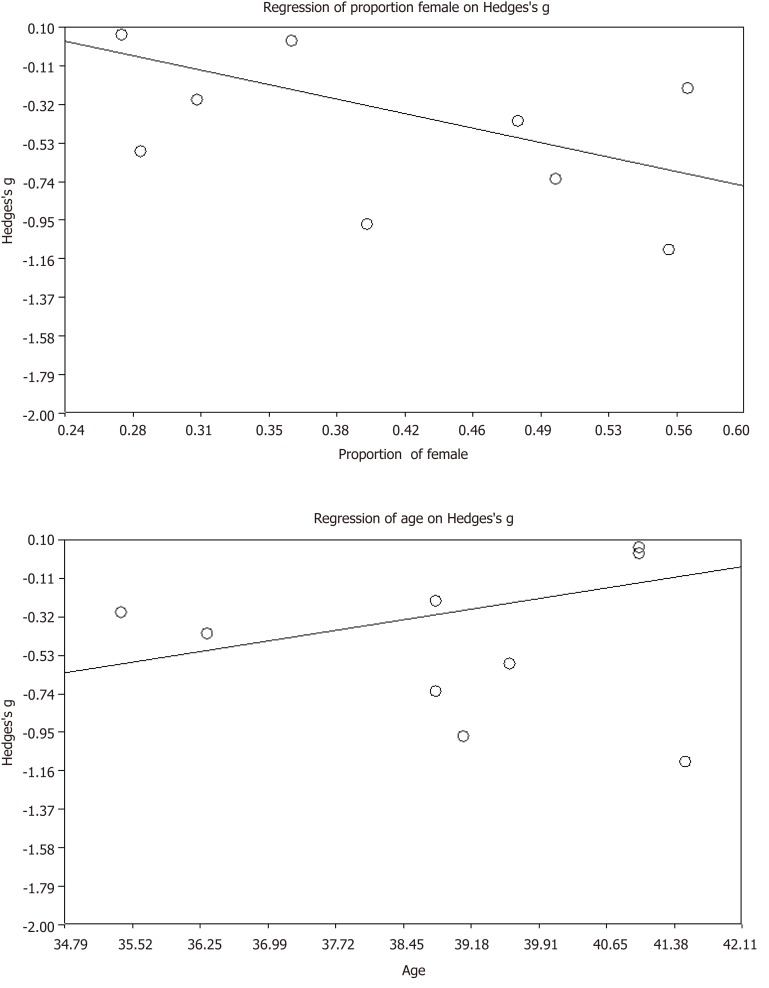
Trials with a greater proportion of female participants and with younger participants reported significantly larger effect sizes for the alleviation of negative symptoms (Figure 7). The number of therapy sessions offered to participants throughout each trial, ranging from 8 forty-five-minute sessions to 72 two-hour sessions, was not a significant predictor of the effect size for negative symptoms.
Figure 7.
Regression plots showing effect size for negative symptoms against proportion of female patients per trial (top) and mean age (bottom).
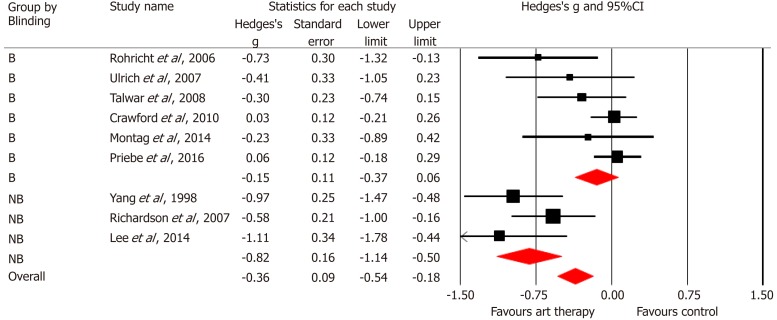
Turning to categorical variables, trials with high risk of bias had significantly larger effect sizes than those at lower risk of bias [(g = -0.82, -1.14 to -0.50, k = 3) vs (g = -0.15, -0.37 to 0.10, k = 6), Q = 11.59, df = 1, P < 0.001]. We assessed the specific impact blinding of outcome assessment as a categorical moderator for negative symptoms. The pooled effect size for 6 blind studies was nonsignificant (g = -0.15, 95%CI -0.37 to 0.06, P = 0.17), whereas that in 3 non-blind studies was highly significant (g = -0.82, 95%CI -1.14 to -0.50, P < 0.001). The effect size for blind trials was significantly smaller than that for nonblind trials (Q = 11.55, df=1, P < 0.001, Figure 8). Heterogeneity was non-significant for both blind and nonblind trials (Q = 8.78, df = 5, P = 0.12, I2 = 43.16; Q = 2.39 df = 2, P = 0.30, I2 = 16.26, respectively).
Figure 8.
Forest plot comparing blind vs non-blinded outcome assessment. B: Blind; NB: Non-blinded.
DISCUSSION
A key aim of the current paper was to analyse evidence from RCTs regarding the efficacy of art therapies to reduce the symptoms of schizophrenia, especially negative symptoms. Like previous meta-analyses[9-11], we found no significant benefit of art therapies in reducing total symptoms or positive symptoms. On the key claim regarding negative symptoms, we did find a significant reduction, thus replicating the earlier finding reported by NICE[9]. Crucially, however, this interpretation must be qualified – as any symptom reduction was subject to potential biases.
Although overall bias - as assessed by the RoB2[20] - was not high in most trials, trials at high-risk did produce significantly larger effect sizes for negative symptoms. An issue of central concern is that effect sizes were exaggerated considerably by non-blind assessment of outcomes. The pooled effect size for 3 non-blind trials was more than five-times larger than that for 6 blind trials (-0.82 vs -0.15). This accords with observations at the level of individual RCTs, where each of the 3 non-blind trials produced moderate-large significant effect sizes, while 5 out of 6 blinded trials produced nonsignificant outcomes. The failure to use blind assessment clearly inflates the apparent efficacy of art therapies and crucially, this source of bias was not assessed in previous meta-analyses. Such effect size inflation in unblinded trials is well-documented in medicine[29-32], but the impact is exacerbated in trials that use more subjective measures such as clinician rating scales to assess symptomatic outcomes[26]. The same bias has been reported in trials of CBT for schizophrenia, where effect sizes are inflated between 4 and 7 times by non-blind compared to blind outcome assessment for various symptom ratings[6]. This inflation is in the same range as that documented here for art therapies where unblinded assessment of negative symptoms produced an effect size more than 5 times that for blind assessment. To put the latter into perspective, the difference between blind and nonblind effect sizes is larger than the mean effect size reported by NICE to underpin their recommendation of art therapies for negative symptoms.
Evidence of possible publication bias also emerged for negative symptoms from the trim and fill analysis (and Egger’s test) - with 5 imputed missing trials reducing the effect size for negative symptoms effectively to zero (regardless of blinding). Of course, such tests do not provide direct evidence of publication bias and are estimates based upon various assumptions. The influence of unblinded assessment and the evidence of publication bias both undermine findings regarding the efficacy of art therapies to reduce negative symptoms.
One advantage of the current study is that it almost doubles the number of trials and more than triples the number of participants that were assessed by NICE (475 art therapies and 473 control participants vs 148 art therapies and 146 controls analysed by NICE). In their critique of NICE guidance (CG178), Taylor et al[33] (2015, p. 358) allude to the issue of statistical power questioning the fact that NICE “…concludes that there is sufficient evidence only for art therapies to be offered to service users with psychosis and schizophrenia (recommendation 9.3.8.1) based on a limited review of six RCTs. These RCTs had small sample sizes (n = 24-90)”. The current analysis includes newer larger trials and in contrast to previous meta-analyses, was sufficiently powered (0.8) with 9 trials to detect the mean effect size (-0.42) we report[34]. By contrast, the NICE analysis of art therapies was severely underpowered – having a mean power of just 0.37 to detect the overall effect size for negative symptoms reported here.
The recent additions of the MATISSE[15] and Priebe et al[16] trials provide – to date - the largest RCTs assessing art therapies. These two studies are the only published trials that are sufficiently powered (at 0.83 and 0.82 respectively) to detect the modest effect size reported in this meta-analysis; and both reported zero effect sizes - 0.03 and 0.06 respectively. Indeed, each of these two trials alone contained almost as many participants as all 5 trials combined in the NICE[11] meta-analysis for negative symptoms. Crucially both trials were also pre-registered and did not deviate from what was proposed in terms of approach, recruitment and analyses. Nonetheless, meta-analyses are only as reliable as the individual studies that are assessed. While the MATISSE trial is the largest assessment of art therapy and exceptionally well-controlled, it is not without its critics[35,36]. Holttum et al[35] raised a series of methodological and procedural issues relating to the trial, which they believe may have influenced the null findings. For example, although actual trial drop-out was reasonable, attendance at sessions was often quite low. On another point, Wood[36] has argued that the MATISSE trial failed to actually test art therapy as currently practised in the UK. The MATISSE authors have responded to many of these points[37]. The other large well conducted trial by Priebe et al[16] has also received some critical commentary. Crawford et al[38] raise important questions concerning why so many phase III trials, especially of complex psychological interventions such as the body-oriented psychotherapy trial by Priebe et al[16] fail to build on earlier promising exploratory studies. Psychological interventions are clearly complex and Crawford et al[38] note that they “are often relational in nature and rely even more on a clinician’s ability to navigate interpersonal relationships and actively engage people in treatment” – this therefore makes them less predictable than, for example, a drug trial. While art therapies may not lend themselves as readily to randomised control designs, current treatment guideline such as those of NICE rely heavily upon RCTs as their gold standard evidence.
A further recommendation that NICE[11] proposed for future research was to assess the optimal number of sessions that should be offered to people with schizophrenia. The number of trial sessions included in the current meta-analysis varied considerably - the least offered was 8[25], while the most was 72[15]. Our meta-regression analysis revealed that number of intended sessions was not a predictor of the efficacy of art therapies on negative symptomatology.
While we found no evidence for symptom reduction, it may be that art therapies produce other benefits or are beneficial for some individuals and not others. Maujean et al[4] in their systematic review concluded that “It is possible that limited exposure to art therapy is insufficient to bring about change in such a significant illness as schizophrenia and …may not be expected to reduce global symptoms or enhance overall quality of life, but could be reasonably expected to improve emotional states” (p. 42). Related concerns have arisen regarding the "quasi-neuroleptic" focus on symptom reduction in art therapies as well as other psychological interventions e.g., CBT for psychosis[39]. Psychological interventions in general and art therapies in particular might be better placed to focus on non-symptomatic outcomes such as reducing distress (associated with symptoms), depression or anxiety or improving functioning and quality of life; and for future trials of art therapies to consider moving away from a symptom reduction focus[8].
As already noted, art therapy is an umbrella term that encompasses a diverse range of approaches (including dance therapy, music therapy and body-oriented psychotherapy) and this might account for some effect size heterogeneity. While we included the same broad forms of art therapies indicated by NICE, the number of trials limit assessing whether any specific approach might be more successful pursued than others. Nonetheless, Crawford et al[15] used a more conventional art therapy, while Preibe et al[16] used group body psychotherapy and neither found a significant effect.
Turning to the question of "individuality", some may benefit more from art therapies than others. In this context, our moderator analyses revealed a significantly greater negative symptom reduction in trials with more female patients and those who are younger. The role of patient gender requires further investigation – especially since better outcomes for women in art therapy have been reported in other patient groups[40]. Moreover, since art therapists are also more likely to be women - the American Art Therapy Association suggest a ratio of 10 to 1 female: Male[41], the relationship role itself might further be examined. Turning to age, the range was limited and any future trials might investigate whether the benefits are greater for those who are younger and/or have a shorter duration of illness.
Certain limitations of the current meta-analysis should be considered. The number of randomised control trials published to date is low. Although the current analysis did have sufficient power, the small number of trials allied to missing data did mean that some planned moderator analyses were not feasible e.g. length of illness. Similarly, it was not possible to examine any impact of art therapies at follow-up because it was so rarely assessed.
In summary, the current meta-analysis found no evidence that art therapies alleviate positive or total symptoms in schizophrenia. Like previous meta-analyses, we found some evidence that they may alleviate the negative symptoms of schizophrenia, but this finding did not emerge in trials using blind outcome assessment and may also be prone to publication bias. In this context, national guidelines, such as that by NICE[11] suggesting that art therapy reduces negative symptoms require reconsideration.
ARTICLE HIGHLIGHTS
Research background
Art therapies are advocated by national bodies, such as the United Kingdom’s National Institute for Health and Care Excellence, particularly to alleviate the negative symptoms associated with schizophrenia. The last meta-analysis is now a decade old and several new larger well-controlled trials have been recently published. A meta-analytic update is timely.
Research motivation
The present study aimed to assess randomised controlled trials (RCT) of art therapies for reducing the symptoms of schizophrenia – particularly negative symptoms.
Research objectives
A key objective is to evaluate and update evidence for future guidelines concerning treatment suggestions.
Research methods
A search of PubMed and Scopus was conducted until May 2019 for RCTs assessing symptomatic outcomes following art therapy. Study quality was assessed using the Cochrane risk of bias tool. Random effects meta-analyses were conducted using Comprehensive Meta-Analysis (version 2). Moderator analyses were conducted using both meta-regression and categorical comparisons.
Research results
We identified 133 articles, of which 9 RCTs involving 948 participants (475 assigned to art therapy and 473 controls) met our inclusion criteria. Using random effects models, we calculated pooled effect sizes (Hedges g) for end-of-trial symptomatic outcomes. Effect sizes were non-significant for total symptoms [g = -0.27, 95% confidence interval (CI) -0.60 to 0.05, k = 6] and positive symptoms (g = -0.10, 95%CI -0.35 to 0.15, k = 6); however, we did find significant negative symptom reduction (g = -0.42, 95%CI -0.70 to -0.14, k = 9). Meta-regression revealed that negative symptom reduction was larger in trials with a greater proportion of women and in trials with younger patients. Crucially, the negative symptom reduction following art therapies did not, however, emerge in trials that used blind assessment of outcomes.
Research conclusions
This review presents a comprehensive meta-analysis of art therapies in schizophrenia in terms of both studies included and participant numbers. We found that art therapies did not significantly reduce total or positive symptoms. A "small" therapeutic effect was found for negative symptoms, but we show that the effect is not present in blind trials and may be subject to publication bias. The findings have implications for clinical practice and future treatment guidelines (e.g., National Institute of Clinical Excellence) that have previously recommended using art therapies to alleviate negative symptoms in people with schizophrenia.
Research perspectives
The current meta-analysis suggests that RCTs of art therapies do not provide evidence of any reduction in total, positive or indeed, negative symptoms. The latter is important as this has been viewed as a key aspect of art therapies in schizophrenia – being recommended in influential national guidelines such as that by National Institute of Clinical Excellence. Future trials might investigate whether one particular form of art therapy offers more benefit than others. They might also look at whether younger individuals and women do benefit more than men.
Footnotes
Conflict-of-interest statement: The authors have no conflicts of interest to declare.
PRISMA 2009 Checklist statement: The authors have read the PRISMA 2009 Checklist, and the manuscript was prepared and revised according to the PRISMA 2009 Checklist.
Manuscript source: Invited manuscript
Peer-review started: June 4, 2019
First decision: August 2, 2019
Article in press: October 14, 2019
Specialty type: Psychiatry
Country of origin: United Kingdom
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B, B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chakrabarti S, Seeman MV, Shiina A, Wang YP S-Editor: Yan JP L-Editor: A E-Editor: Xing YX
Contributor Information
Keith R Laws, School of Life and Medical Sciences, University of Hertfordshire, Hatfield AL10 9AB, United Kingdom. k.laws@herts.ac.uk.
William Conway, School of Life and Medical Sciences, University of Hertfordshire, Hatfield AL10 9AB, United Kingdom.
References
- 1.Uttley L, Stevenson M, Scope A, Rawdin A, Sutton A. The clinical and cost effectiveness of group art therapy for people with non-psychotic mental health disorders: a systematic review and cost-effectiveness analysis. BMC Psychiatry. 2015;15:151. doi: 10.1186/s12888-015-0528-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Röhricht F. Body oriented psychotherapy. The state of the art in empirical research and evidence-based practice: A clinical perspective. Body Movement Dance Psychother. 2009;4:135–156. [Google Scholar]
- 3.Regev D, Cohen-Yatziv L. Effectiveness of Art Therapy With Adult Clients in 2018-What Progress Has Been Made? Front Psychol. 2018;9:1531. doi: 10.3389/fpsyg.2018.01531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maujean A, Pepping CA, Kendall E. A systematic review of randomized controlled studies of art therapy. Art Ther. 2014:31: 37–44. [Google Scholar]
- 5.Hogan S. The art therapy continuum: A useful tool for envisaging the diversity of practice in British art therapy. Int J Art Ther. 2019;14:29–37. [Google Scholar]
- 6.Jauhar S, McKenna PJ, Radua J, Fung E, Salvador R, Laws KR. Cognitive-behavioural therapy for the symptoms of schizophrenia: systematic review and meta-analysis with examination of potential bias. Br J Psychiatry. 2014;204:20–29. doi: 10.1192/bjp.bp.112.116285. [DOI] [PubMed] [Google Scholar]
- 7.Jauhar S, Laws KR, McKenna PJ. CBT for schizophrenia: a critical viewpoint. Psychol Med. 2019;49:1233–1236. doi: 10.1017/S0033291718004166. [DOI] [PubMed] [Google Scholar]
- 8.Laws KR, Darlington N, Kondel TK, McKenna PJ, Jauhar S. Cognitive Behavioural Therapy for schizophrenia - outcomes for functioning, distress and quality of life: a meta-analysis. BMC Psychol. 2018;6:32. doi: 10.1186/s40359-018-0243-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ruddy R, Milnes D. Art therapy for schizophrenia or schizophrenia-like illnesses. Cochrane Database Syst Rev. 2003;(2):CD003728. doi: 10.1002/14651858.CD003728. [DOI] [PubMed] [Google Scholar]
- 10.Ruddy R, Milnes D. Art therapy for schizophrenia or schizophrenia-like illnesses. Cochrane Database Syst Rev. 2005;(4):CD003728. doi: 10.1002/14651858.CD003728.pub2. [DOI] [PubMed] [Google Scholar]
- 11.National Collaborating Centre for Mental Health. Psychosis and Schizophrenia in Adults: Treatment and Management. NICE Clinical Guideline 178. NICE, 2014. Available from: URL: http://www.nice.org.uk/guidance/cg178/ evidence/cg178-psychosis-and-schizophrenia-in-adults-full-guideline3. [Google Scholar]
- 12.Scottish Intercollegiate Guidelines Network. Management of Schizophrenia: A National Clinical Guideline. SIGN 131. SIGN, 2013. Available from: URL: http://www.sign.ac.uk/ pdf/sign131.pdf. [Google Scholar]
- 13.Galletly C, Castle D, Dark F, Humberstone V, Jablensky A, Killackey E, Kulkarni J, McGorry P, Nielssen O, Tran N. Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for the management of schizophrenia and related disorders. Aust N Z J Psychiatry. 2016;50:410–472. doi: 10.1177/0004867416641195. [DOI] [PubMed] [Google Scholar]
- 14.Attard A, Larkin M. Art therapy for people with psychosis: a narrative review of the literature. Lancet Psychiatry. 2016;3:1067–1078. doi: 10.1016/S2215-0366(16)30146-8. [DOI] [PubMed] [Google Scholar]
- 15.Crawford MJ, Killaspy H, Barnes TR, Barrett B, Byford S, Clayton K, Dinsmore J, Floyd S, Hoadley A, Johnson T, Kalaitzaki E, King M, Leurent B, Maratos A, O'Neill FA, Osborn D, Patterson S, Soteriou T, Tyrer P, Waller D MATISSE project team. Group art therapy as an adjunctive treatment for people with schizophrenia: a randomised controlled trial (MATISSE) Health Technol Assess. 2012;16:iii–iiv, 1-76. doi: 10.3310/hta16080. [DOI] [PubMed] [Google Scholar]
- 16.Priebe S, Savill M, Wykes T, Bentall RP, Reininghaus U, Lauber C, Bremner S, Eldridge S, Röhricht F. Effectiveness of group body psychotherapy for negative symptoms of schizophrenia: multicentre randomised controlled trial. Br J Psychiatry. 2016;209:54–61. doi: 10.1192/bjp.bp.115.171397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions Version 5.1.0 2014. [updated March 2011] Available from: http://handbook-5-1.cochrane.org/
- 19.Duval S, Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56:455–463. doi: 10.1111/j.0006-341x.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- 20.Higgins J, Savovic J, Sterne JAC, Page M, Hróbjartsson A, Boutron A. A revised tool to assess risk of bias in randomized trials (RoB 2.0). Available from: Available from: URL: https://sites.google.com/site/riskofbiastool/welcome/rob-2-0-tool. [Google Scholar]
- 21.Yang WY, Li Z, Weng YZ, Zhang HY, Ma B. Psychosocial rehabilitation effects of music therapy in chronic schizophrenia. Hong Kong J Psychiatry. 1998;8:38–40. [Google Scholar]
- 22.Röhricht F, Priebe S. Effect of body-oriented psychological therapy on negative symptoms in schizophrenia: a randomized controlled trial. Psychol Med. 2006;36:669–678. doi: 10.1017/S0033291706007161. [DOI] [PubMed] [Google Scholar]
- 23.Ulrich G, Houtmans T, Gold C. The additional therapeutic effect of group music therapy for schizophrenic patients: a randomized study. Acta Psychiatr Scand. 2007;116:362–370. doi: 10.1111/j.1600-0447.2007.01073.x. [DOI] [PubMed] [Google Scholar]
- 24.Richardson P, Jones K, Evans C, Stevens P, Rowe A. Exploratory RCT of art therapy as an adjunctive treatment in schizophrenia. J Mental Health. 2007;16:483–491. [Google Scholar]
- 25.Talwar N, Crawford MJ, Maratos A, Nur U, McDermott O, Procter S. Music therapy for in-patients with schizophrenia: exploratory randomised controlled trial. Br J Psychiatry. 2006;189:405–409. doi: 10.1192/bjp.bp.105.015073. [DOI] [PubMed] [Google Scholar]
- 26.Montag C, Haase L, Seidel D, Bayerl M, Gallinat J, Herrmann U, Dannecker K. A pilot RCT of psychodynamic group art therapy for patients in acute psychotic episodes: feasibility, impact on symptoms and mentalising capacity. PLoS One. 2014;9:e112348. doi: 10.1371/journal.pone.0112348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee HJ, Jang SH, Lee SY, Hwang KS. Effectiveness of dance/movement therapy on affect and psychotic symptoms in patients with schizophrenia. Arts Psychother. 2015;45:64–68. [Google Scholar]
- 28.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hróbjartsson A, Thomsen AS, Emanuelsson F, Tendal B, Hilden J, Boutron I, Ravaud P, Brorson S. Observer bias in randomised clinical trials with binary outcomes: systematic review of trials with both blinded and non-blinded outcome assessors. BMJ. 2012;344:e1119. doi: 10.1136/bmj.e1119. [DOI] [PubMed] [Google Scholar]
- 30.Hróbjartsson A, Thomsen AS, Emanuelsson F, Tendal B, Hilden J, Boutron I, Ravaud P, Brorson S. Observer bias in randomized clinical trials with measurement scale outcomes: a systematic review of trials with both blinded and nonblinded assessors. CMAJ. 2013;185:E201–E211. doi: 10.1503/cmaj.120744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias. Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA. 1995;273:408–412. doi: 10.1001/jama.273.5.408. [DOI] [PubMed] [Google Scholar]
- 32.Wood L, Egger M, Gluud LL, Schulz KF, Jüni P, Altman DG, Gluud C, Martin RM, Wood AJ, Sterne JA. Empirical evidence of bias in treatment effect estimates in controlled trials with different interventions and outcomes: meta-epidemiological study. BMJ. 2008;336:601–605. doi: 10.1136/bmj.39465.451748.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Taylor M, Perera U. NICE CG178 Psychosis and Schizophrenia in Adults: Treatment and Management - an evidence-based guideline? Br J Psychiatry. 2015;206:357–359. doi: 10.1192/bjp.bp.114.155945. [DOI] [PubMed] [Google Scholar]
- 34.Cuijpers P. Amsterdam, the Netherlands: Pim Cuijpers Uitgeverij;; 2016. Meta-analyses in mental health research: A practical guide. [Google Scholar]
- 35.Holttum S, Huet V. The MATISSE trial–a critique: does art therapy really have nothing to offer people with a diagnosis of schizophrenia? Sage Open. 2014;4:1–11. [Google Scholar]
- 36.Wood C. In the wake of the Matisse RCT: What about art therapy and psychosis? Int J Art Ther. 2013;18:88–97. [Google Scholar]
- 37.Patterson S, Waller D, Killaspy H, Crawford MJ. Riding the wake: detailing the art therapy delivered in the MATISSE study. Int J Art Ther. 2015;20:28–38. [Google Scholar]
- 38.Crawford MJ, Barnicot K, Patterson S, Gold C. Negative results in phase III trials of complex interventions: cause for concern or just good science? Br J Psychiatry. 2016;209:6–8. doi: 10.1192/bjp.bp.115.179747. [DOI] [PubMed] [Google Scholar]
- 39.Birchwood M, Shiers D, Smith J. CBT for psychosis: not a 'quasi-neuroleptic'. Br J Psychiatry. 2014;204:488–489. doi: 10.1192/bjp.204.6.488a. [DOI] [PubMed] [Google Scholar]
- 40.Gussak D. Comparing the effectiveness of art therapy on depression and locus of control of male and female inmates. Arts Psychother. 2009;36:202–207. [Google Scholar]
- 41.Gussak D. An interactionist perspective on understanding gender identity in art therapy. Art Ther. 2008;25:64–69. [Google Scholar]