Abstract
Purpose: Social and economic factors have been shown to affect health outcomes. In particular, social determinants of health (SDH) are linked to poor health outcomes in children. Research and some professional academies support routine social needs screening during primary care visits. Translating this recommendation into practice remains challenging due to the resources required and dearth of evidence-based research to guide health center level implementation. We describe our experience implementing a novel social needs screening program at an academic pediatric clinic. Methods: The Community Linkage to Care (CLC) pilot program integrates social needs screening and referral support using community health workers (CHWs) as part of routine primary care visits. Our multidisciplinary team performed process mapping, developed workflows, and led ongoing performance improvement activities. We established key elements of the CLC program through an iterative process We conducted social needs screens at 65% of eligible well-child visits from May 2017 to April 2018; 19.7% of screens had one or more positive responses. Childcare (48.8%), housing quality and/or availability (39.9%), and food insecurity (22.8%) were the most frequently reported needs. On average, 76% of providers had their patients screened on more than half of eligible well-child visits. Discussion: Our experience suggests that screening for social needs at well-child visits is feasible as part of routine primary care. We attribute progress to leveraging resources, obtaining provider buy-in, and defining program components to sustain activities.
Keywords: social determinants of health, community health workers, quality, improvement, pediatrics, implementation
Background and Significance
In the United States, 1 in 5 children live in poverty, with 47% of children in the South Bronx living below the federal poverty level.1 There is a growing body of research supporting the impact of social and economic factors on health outcomes. Social determinants of health (SDH) are defined by the World Health Organization as “the conditions, in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life.”2 Unmet social needs are linked to increased prevalence of asthma, obesity, infant mortality, and poorer developmental outcomes in children specifically.3,4 Though population health studies continue to support the impact of social factors on community health, it is less clear how health systems can address these social influences in practical ways at the clinic center level beyond advocating for national and state health policies that support social programs.5-8 Several recent studies suggest that screening for social needs in ambulatory settings is associated with increased uptake of social services,9-11 and furthermore, an increased uptake of social services may be associated with improved health outcomes.12,13 In 2016, the American Academy of Pediatrics issued a policy statement on poverty and child health, which recommended that providers “screen for risk factors within social determinants of health during patient encounters.”14 However, translating this policy recommendation into practice is difficult due to the dearth of evidence-based research to guide health center level implementation.15,16
Academic centers and their community-based partners may have a unique role to play in addressing these knowledge gaps.3,15,17,18 Starting in 2016, our health system partnership, consisting of a partnership between the Bronx Community Health System, Montefiore Office of Community and Population Health, and the Montefiore Medical Group ambulatory network, launched a new initiative aimed to systematize screening and outreach initiatives for social needs at ambulatory sites. In collaboration with these partners, we co-developed the Community Linkage to Care (CLC) program, which aimed to leverage the resources provided by this initiative, translate policy recommendations into practice, and identify core program elements for an integrated social needs screening and outreach model using provider, staff, and patient feedback as guidance. In this article, we describe our experiences developing and implementing this novel program to illustrate that social needs screening in an ambulatory pediatric clinic is both feasible and practical.
Setting
The site of the CLC pilot is a federally qualified health center. It was founded in 1967 as one of the first community health centers in the Bronx and provides primary care services, including pediatrics, adult medicine, obstetrics and gynecology, dental, mental health, social services, dermatology, and podiatry and is the ambulatory training site for residents in a Social Medicine residency program. In 2017, 11 pediatric providers conducted approximately 17 000 visits.
The clinic is located in New York’s 15th congressional district in the South Bronx. This is the poorest urban district in the United States, with a median household income roughly half of the national and state average.19 In addition to high rates of child poverty, food insecurity, and homelessness, the Bronx has the highest rates of preterm births, infant mortality, childhood obesity, asthma, and teen births in New York City.20 Bronx County consistently ranks last in health outcomes for New York State.21
Methods
Piloting and Developing Community Linkage to Care Program
Many departments, community-based partners, and divisions within our health system collaborated to introduce a system-wide SDH screening initiative to identify patients with unmet social needs throughout its ambulatory network. Some of the authors on this article were involved in a working group to develop the screening instrument that would be integrated into our electronic medical record (EMR). The screen was adapted from the Health Leads screening toolkit22 and included 7 yes/no validated questions on domains such as housing insecurity and quality, food insecurity, health care costs, utilities, transportation, childcare, and violence. As part of the New York State Delivery System Reform Incentive Program (DSRIP), this site received funding to support a variety of additional staffing, including community health workers (CHWs) and a social worker. CHWs are members of the Bronx community who are trained by a community-based organization partner to provide additional support services to patients and families, and who serve as a link between the health system and community resources.
Over the pilot period of 12 months, our team delineated core program elements based on guidelines for integrating CHWs into health centers23 and staff feedback. This process resulted in a focus on standardized workflows for both screening and referral, developing CHW scope of work, creating new data systems, and developing performance improvement opportunities. Based on staff experience with the screen, screening data, and several revisions, our multidisciplinary patient-centered medical home (PCMH) transformation team including nurses, physicians, administrative staff, and transformation coach developed new clinical workflows for both screening and referrals processes. All the pilot activities were integrated as a new focused project within ongoing PCMH activities including assigning a project team, obtaining leadership buy-in and support, and planning performance metrics, such as number of screens completed and percentage of providers using the screen. Multiple discussions were planned with our site medical director, who provided leadership and direction, as well as the health center administration director. Within this team, we had bimonthly discussions on developing and adjusting a clinic workflow for both screening and referring positive screens, using an iterative approach and revising based on implementer feedback that was provided during PCMH meetings and performance metrics. Finalizing the CLC workflow involved discussions determining screening frequency, roles of different team members, and referral protocols. This team was also responsible for educating and training staff on how to conduct screening and referrals. Daily morning huddles were used to reinforce program elements and discuss issues. Of note, this project was a part of expected PCMH functions and did not involve specific research funding, support, or staff.
Measures
Data collection and performance improvement measures were adapted using an implementation science framework, RE-AIM (Reach, Effectiveness, Adoption, Implementation, and Maintenance),24 to guide assessment and define and organize metrics (Table 1). Screening results and pediatric visit encounters were extracted on a monthly basis from our EMR, Epic. We tabulated metrics using Microsoft Excel tables and constructed run charts for Reach & Adoption measures. These run charts were annotated with key events to facilitate program adoption and performance improvement activities.
Table 1.
Overview of Community Linkage to Care Program Evaluation Metrics, Adapted From RE-AIM Framework, Including Pilot Phase, RE-AIM Domain, Metric Name, and Definition.
| RE-AIM Domain | Metric | Definition |
|---|---|---|
| Reach | Social needs screening ratio | Number of screens conducted/“Potential” or eligible screen encounters |
| Reach | CHW referral ratio | Number of positive screens referred to CHW/Total number of positive screens |
| Adoption | Provider adoption ratio | Proportion of providers “active” in screening and referral (“active” = screening >50% of eligible encounters) |
Abbreviations: RE-AIM, Reach, Effectiveness, Adoption, Implementation, and Maintenance; CHW, community health worker.
Ethics
This study was reviewed and approved by the Institutional Review Board at Albert Einstein School of Medicine (IRB# 2017-8434).
Results
Components of Community Linkage to Care Program
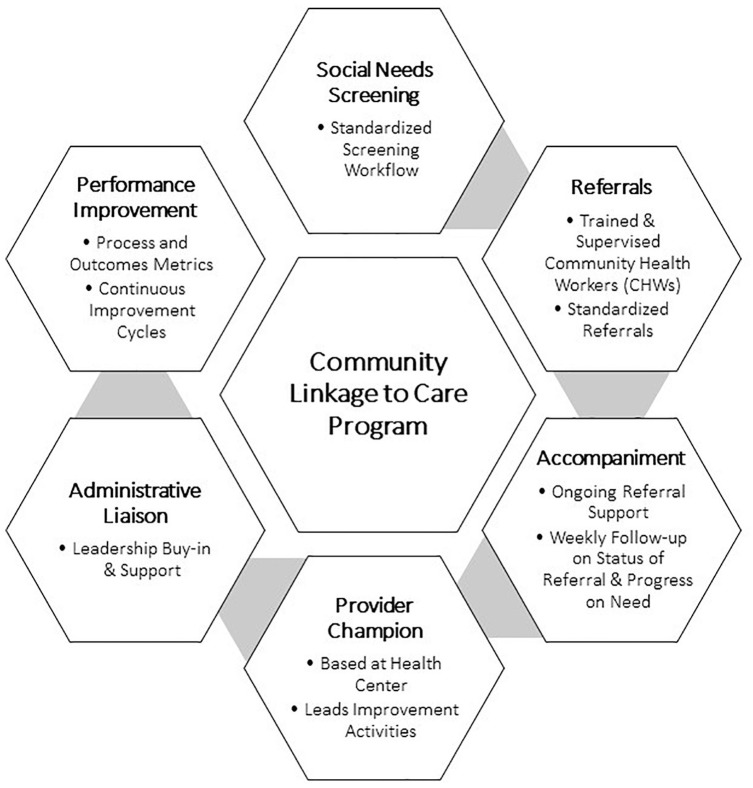
Starting in May 2017, we conducted an iterative and experiential process through PCMH meetings to establish key elements of the CLC program that resulted in the following (Figure 1): (1) social needs screening workflow included a standardized process for screening at well-child visits at a set frequency, which was iterated and tested to identify who would be screened, at what frequency, where in the visit process, and by whom; (2) referral workflow defined a systematic process for making referrals for positive screens to trained and supervised clinic based CHWs, or to social workers for more urgent issues like intimate partner violence; (3) accompaniment, systematic patient follow-up included routinized, active follow-up by CHWs with families on a regular basis to assess whether outreach service was obtained and progress on social need(s) had been made; (4) provider champion was a designated clinician based at the health center who led ongoing program quality improvement, CHW coaching efforts, and program adaptions; (5) administrative liaisons were key clinical site leaders who were engaged with the program and provided leadership, direction, and supervision (included the medical director and administrator directed at this site); and (6) performance improvement activities involved organizing, key process and outcomes metrics that were then disseminated to staff and used to foster provider feedback and continuous improvement.
Figure 1.
Schematic of Community Linkage to Care program elements.
Developing Clinic-Based Workflow
Our PCMH team was tasked with the development of a clinic-specific workflow for this initiative. Modifications to the workflow were driven by discussions among PCMH team members until a final consensus was agreed upon (Figure 2). For our patient population, we focused on annual well-child exams, adapting a recommendation by the AAP 2016 statement and Bright Futures Guidelines.14,25 Reasons for this choice were based on perceived feasibility for both staff and families. At annual visits, our staff is accustomed to handing out screens, and caregivers expect to complete forms. Caregivers are given SDH screens in the exam room prior to the medical visit, allowing nurses to enter screen results into the EMR. We intentionally opted for voluntary “self-administration” of the screening instrument to reduce possible stigma associated with asking for assistance with social needs. If a screen is positive, the provider is expected to discuss the positive item with the patient, as they would discuss social concerns that were brought up by a patient independent of a screening process. Part of this discussion includes an assessment of whether the family identifies it as an issue for which they would like assistance. Providers can note in the EMR if a patient with a positive screen declines assistance or referral. If a screen is positive for an urgent issue (domestic violence, impending eviction, etc), the patient is referred to an available onsite social worker who can meet with the family during or immediately after the visit. This is to ensure that patients receive counseling from an appropriately trained professional, if needed, and receive real-time assistance for emergency situations. For non-urgent issues, an effort is made to conduct a warm handoff with the CHW, at which time the CHW may provide the patient with resources and schedule a follow-up. If the CHW is not available in a timely manner due to a busy patient panel, providers can send a referral through the EMR. CHWs are based within the health center and coordinate referrals with patients either by phone or in-person.
Figure 2.
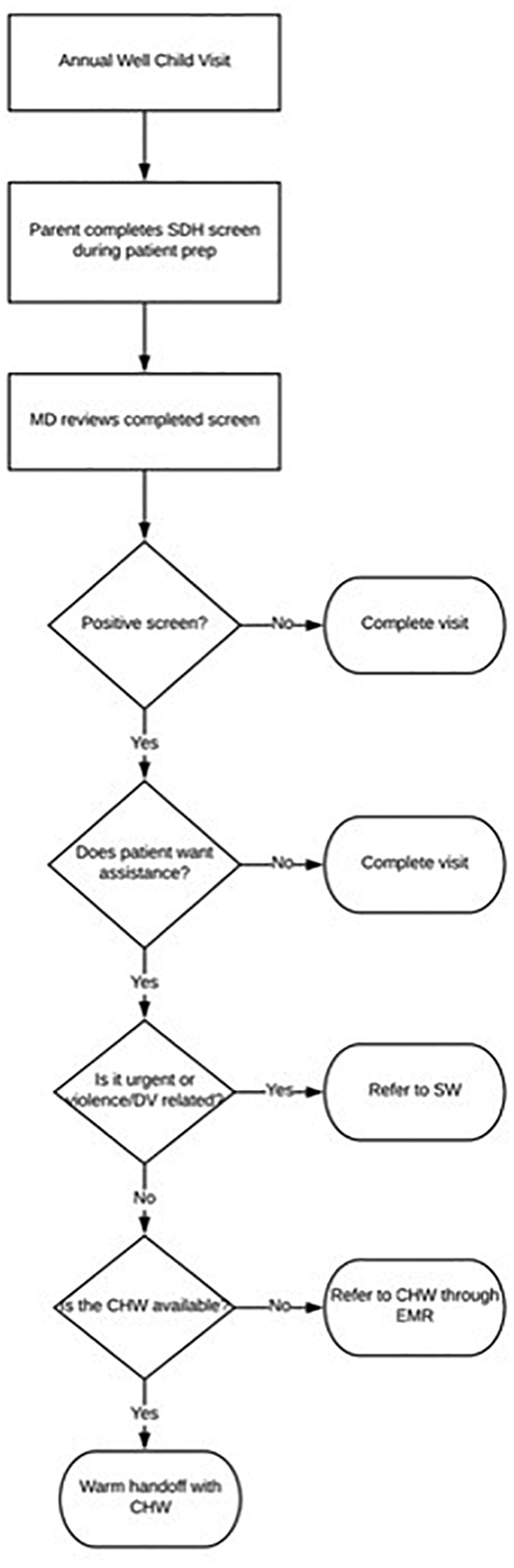
Community Linkage to Care health center workflow for social needs screening and community health worker referrals.
Reach Metrics
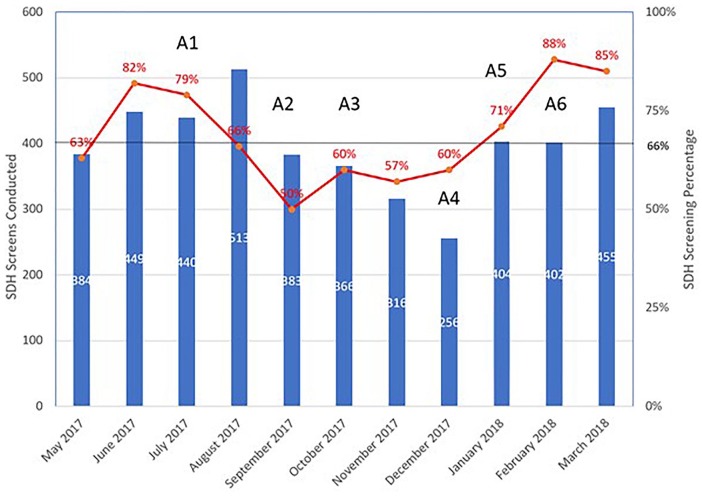
There were 7266 active CHCC pediatric patients during the study period from May 1, 2017 through April 1, 2018 as summarized in Table 2. A total of 4162 SDH screens were conducted at 6410 eligible well-child visits for an overall screening rate of 65%. The median monthly primary Reach metric (screens performed/eligible well-child visits) over the 11-month period was 66% (interquartile range of 60% to 82%). A total of 19.7% (820/4162) of the SDH screens performed had one or more positive responses. Overall, 37.8% (310/820) of positive SDH screens had more than 1 positive item. Of the positive screens, the social need categories that were most frequently cited included needs for: childcare 48.8% (400/820), housing quality and/or availability 39.9% (327/820), and food 22.8% (187/820). Figure 3 summarizes screening measures including numbers of screens conducted and SDH screening percentage by month.
Table 2.
Summary of social needs screen results at Community Linkage to Care Pilot from May 1, 2017 to April 1, 2018.
| Active pediatric patients, n | 7266 |
| Age, months, median (IQR) | 88 (37-144) |
| Sex, male/female, n (%) | 2068/2094 (49.7/50.3) |
| Number of screens conducted | 4162 |
| Patients presenting for physical screens (unique patients screened during time period/well-child visits), n (%) | 4162/6410 (65) |
| Monthly screening rate, median (IQR) | 66 (60-82) |
| Number of positive SDH screens | 820 |
| Proportion SDH positive/total screen, % | 19.7 |
| Social need category, n (%)a | |
| Childcare | 400 (48.8) |
| Housing | 327 (39.9) |
| Food | 187 (22.8) |
| Utilities | 178 (21.7) |
| Health care cost | 116 (14.1) |
| Threats/Violence | 40 (4.9) |
Abbreviations: IQR, interquartile range; SDH, social determinants of health.
Percent total >100% because 37.8% (n = 310) of positive SDH screens had more than 1 positive item.
Figure 3.
Summary of monthly social determinant of health screens (bar) and social needs screening percentages (line) with key time events from May 1, 2017 to April 1, 2018.
Key time events from project log (with Community Linkage to Care [CLC] program component in boldface):
A1: Four residents and a chief resident depart and 4 interns begin (Social Needs Screening and Referrals).
A2: Two attending physicians depart, including a project leader, and 2 new clinicians begin (Provider Champion, Social Needs Screening and Referrals).
A3: Nursing provider champion departs (Provider Champion).
A4: Nursing staff shortage due to multiple vacancies (Social Needs Screening).
A5: One of 2 community health workers (CHWs) takes extended leave (Referrals and Accompaniment).
A6: New administrative liaison, reinvigorated patient-centered medical home (PCMH) meetings, use of huddles by provider champion to discuss workflow (Administrative Liaison, Provider Champion and Social Needs Screening.
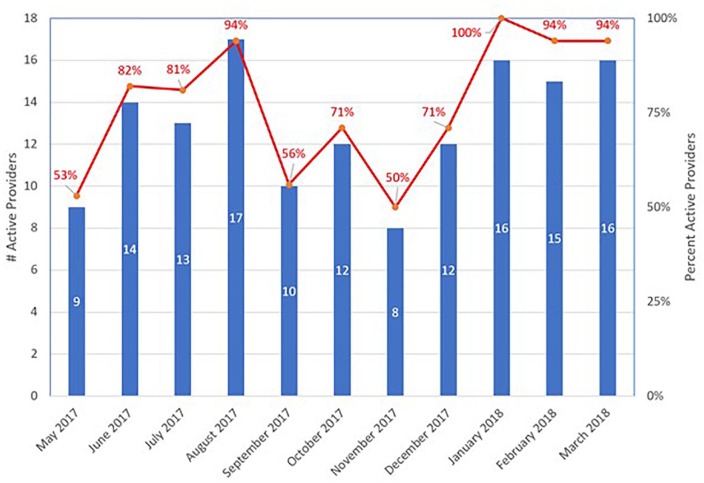
Adoption Metrics
Providers were considered “active” in SDH screening if screens were performed on more than half of their well-child encounters for that month (Figure 4). The percent of “active” providers ranged from 50% to 100%, depending on the month, with an average of 76% of providers actively participating in screening over the study period. The total number of providers present in clinic varied month to month due to medical leaves, vacation, and transitioning of providers.
Figure 4.
Summary of monthly number of “active” providersa (bar) and percentage of “active” providers (line) from May 1, 2017 to April 1, 2018.
a “Active” provider defined as provider using social needs screen at >50% of eligible well-child visits for that month.
Performance Improvement Activities and Staff Engagement
As part of monthly PCMH meetings, we discussed progress and issues with the program and made changes as applicable. Provider champions reviewed metrics and kept a log of changes in clinic environment. We associated each “event” in the log with one of the CLC program key components. Figure 3 is annotated with the following key events that may have contributed and informed observed changes in Reach and Adoption metrics (applicable CLC key program component in boldface). We made deliberate attempts to elicit input and created opportunities for regular verbal feedback in monthly staff meetings and daily huddles regarding both barriers and enabling factors. This verbal feedback was included in our monthly staff meeting minutes and on daily huddle sheets, reviewed by the provider champion, and then presented at our bimonthly PCMH meetings where changes were subsequently made to the program. For example, based on both nursing and provider feedback, the frequency of social needs screening was changed to balance patient flow and optimize screening fidelity.
Discussion
Our initial experience translating policy recommendations into practice resulted in a novel and feasible program that incorporated clinical provider feedback, and this case example contributes to addressing the gap in knowledge regarding optimizing and applying guidelines to screen for social needs in a real-world setting.15,16 We attribute observed progress of the CLC program pilot to be a result of identifying and being explicit about key program components, as we found that these components helped sustain the screening process through multiple clinic environmental changes (ie, staff turnover). These elements included utilizing an established social needs screen, having clear referral protocols, defining the role and scope of work, designating provider champions, engaging administrative liaison(s), and making program changes based on provider feedback. To ensure a screening process that would be successful in our individual clinic center, we went through an iterative process using an established forum, our PCMH meetings, to develop and improve workflows. The workflow design included all members of our clinic team (front desk staff, nursing staff, providers, CHWs) and avoided automatically referring patients to our social worker or CHW. Rather, the design emphasized the importance of family-centered screening and shared decision making.5 Over an 11-month period, we screened more than 4000 patients and encountered almost 800 positive screens, about 20% of the screened population. Most of our providers were actively engaged in the screening process during any given month of the study period.
There were several limitations regarding the generalizability of our experience. With regard to context, we were operating at a clinic site that had previous experience with social medicine principles, with a majority of physicians acknowledging the impact of social needs and being open to addressing these needs in a well-child visit. Therefore, there was likely a high level of provider buy-in prior to program implementation initially and may limit generalizability. Next, our workflow included grant-funded CHWs, which may not be financially feasible at other health centers. As mentioned in multiple monthly meetings, it is likely that the integration of CHWs to assist families motivated clinic team members to screen patients. Although CHWs, who are themselves members of the community, may be more effective in communicating and coordinating referrals, we did not assess this in our study. Furthermore, there may be alternative team members who could play this role, as other programs have successfully screened for social needs utilizing other positions with different titles but similar roles such as patient navigators, resource handouts, or in-depth physician training with success.9,12 In regard to our metrics, data was solely extracted from an EMR system, which is not ideal as there may have been missing screening data and/or mistakes in data entry. Finally, we used ICD-10 (International Classification of Diseases–10th Revision) codes to determine the “number of eligible visits” for both Reach and Adoption metrics, which can be inaccurate.
There clearly remain additional opportunities for improvement with multiple quality improvement projects underway. We are working in collaboration with multiple actors and health system leadership regarding the sustainability of the model, including funding for CHWs, implementing neighborhood- or place-based interventions targeting SDH, optimizing outreach for social needs categories such as food insecurity, and studying the impact of the CLC program on healthcare utilization, outcomes, and costs. Our experience suggests that screening for social needs at well-child visits is both feasible and practical even in a busy ambulatory pediatric clinic. This case description and these findings will inform scale strategies planned for other ambulatory sites within our health system. We attribute our initial progress to leveraging health center resources, including provider buy-in, and having structural components in place to sustain screening, including a practical workflow, resource availability, provider champions, and meaningful metrics.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The authors received funding support from the Doris Duke Charitable Foundation (grant #2018169) to support the publication of this article.
ORCID iD: Kevin Fiori  https://orcid.org/0000-0003-1370-7366
https://orcid.org/0000-0003-1370-7366
References
- 1. Denavas-Walt C, Proctor BD. Income and poverty in the United States: 2014. Current population reports; https://www.census.gov/content/dam/Census/library/publications/2015/demo/p60-252.pdf. Published September 2015. Accessed August 10, 2018. [Google Scholar]
- 2. World Health Organization. A conceptual framework for action on the social determinants of health. Social Determinants of Health Discussion Paper 2; http://www.who.int/sdhconference/resources/ConceptualframeworkforactiononSDH_eng.pdf. Published 2010. Accessed June 29, 2018. [Google Scholar]
- 3. Turney K, Lee H, Mehta N. The social determinants of child health. Soc Sci Med. 2013;95:1-5. doi: 10.1016/j.socscimed.2013.07.015 [DOI] [PubMed] [Google Scholar]
- 4. Braveman P, Gottlieb L. The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep. 2014;129(suppl 2):19-31. doi: 10.1177/00333549141291S206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Garg A, Boynton-Jarrett R, Dworkin PH. Avoiding the unintended consequences of screening for social determinants of health. JAMA. 2016;316:813-814. doi: 10.1001/jama.2016.9282 [DOI] [PubMed] [Google Scholar]
- 6. Fazalullasha F, Taras J, Morinis J, et al. From office tools to community supports: the need for infrastructure to address the social determinants of health in paediatric practice. Paediatr Child Health. 2014;19:195-199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sills MR, Hall M, Colvin JD, et al. Association of social determinants with children’s hospitals’ preventable readmissions performance. JAMA Pediatr. 2016;170:350-358. doi: 10.1001/jamapediatrics.2015.4440 [DOI] [PubMed] [Google Scholar]
- 8. Gottlieb LM, Wing H, Adler NE. A systematic review of interventions on patients’ social and economic needs. Am J Prev Med. 2017;53:719-729. doi: 10.1016/j.amepre.2017.05.011 [DOI] [PubMed] [Google Scholar]
- 9. Chung EK, Siegel BS, Garg A, et al. Screening for social determinants of health among children and families living in poverty: a guide for clinicians. Curr Probl Pediatr Adolesc Health Care. 2016;46:135-153. doi: 10.1016/j.cppeds.2016.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Garg A, Sarkar S, Marino M, Onie R, Solomon BS. Linking urban families to community resources in the context of pediatric primary care. Patient Educ Couns. 2010;79:251-254. doi: 10.1016/j.pec.2009.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Berkowitz SA, Hulberg AC, Hong C, et al. Addressing basic resource needs to improve primary care quality: a community collaboration programme. BMJ Qual Saf. 2016;25:164-172. doi: 10.1136/bmjqs-2015-004521 [DOI] [PubMed] [Google Scholar]
- 12. Gottlieb LM, Hessler D, Long D, et al. Effects of social needs screening and in-person service navigation on child health: a randomized clinical trial. JAMA Pediatr. 2016;170:e162521. doi: 10.1001/JAMAPEDIATRICS.2016.2521 [DOI] [PubMed] [Google Scholar]
- 13. Berkowitz SA, Hulberg AC, Standish S, Reznor G, Atlas SJ. Addressing unmet basic resource needs as part of chronic cardiometabolic disease management. JAMA Intern Med. 2017;177:244-252. doi: 10.1001/JAMAINTERNMED.2016.7691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Council on Community Pediatrics. Poverty and child health in the United States. Pediatrics. 2016;137:e20160339. doi: 10.1542/peds.2016-0339 [DOI] [PubMed] [Google Scholar]
- 15. Gottlieb L, Sandel M, Adler NE. Collecting and applying data on social determinants of health in health care settings. JAMA Intern Med. 2013;173:1017-1020. doi: 10.1001/jamainternmed.2013.560 [DOI] [PubMed] [Google Scholar]
- 16. Beck AF, Cohen AJ, Colvin JD, et al. Perspectives from the Society for Pediatric Research: interventions targeting social needs in pediatric clinical care. Pediatr Res. 2018;84:10-21. doi: 10.1038/s41390-018-0012-1 [DOI] [PubMed] [Google Scholar]
- 17. DeVoe JE, Bazemore AW, Cottrell EK, et al. Perspectives in primary care: a conceptual framework and path for integrating social determinants of health into primary care practice. Ann Fam Med. 2016;14:104-108. doi: 10.1370/afm.1903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Alberti PM. Achieving health equity: how academic medicine is addressing the social determinants of health. https://www.aamc.org/91514/reproductions.html. Accessed May 23, 2016.
- 19. US Census Bureau. American Community Survey. https://censusreporter.org/profiles/50000US3615-new-york-congressional-district-15/. Accessed July 2, 2018.
- 20. Citizens Committee for Children of New York. Keeping track online: The status of New York City children. https://data.cccnewyork.org/. Published 2018. Accessed September 14, 2018.
- 21. Robert Wood Johnson Foundation. County Health Rankings & Roadmaps.Bronx County, NY: http://www.countyhealthrankings.org/app/new-york/2018/rankings/bronx/county/outcomes/overall/snapshot. Published 2018. Accessed September 13, 2018. [Google Scholar]
- 22. Health Leads. Social Needs Screening Toolkit. https://nopren.org/wp-content/uploads/2016/12/Health-Leads-Screening-Toolkit-July-2016.pdf. Published July 2016. Accessed December 21, 2019.
- 23. Ballard M, Bonds M, Burey J, et al. Community Health Worker Assessment and Imorvement Matrix (CHW AIM): updated program functionality matrix for optimizing community health programs. https://chwimpact.org/. Published 2018. Accessed December 21, 2019.
- 24. Glasgow RE, Klesges LM, Dzewaltowski DA, Estabrooks PA, Vogt TM. Evaluating the impact of health promotion programs: using the RE-AIM framework to form summary measures for decision making involving complex issues. Health Educ Res. 2006;21:688-694. doi: 10.1093/her/cyl081 [DOI] [PubMed] [Google Scholar]
- 25. Hagan JF, Jr, Shaw JS, Duncan PM. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents. 4th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2017. [Google Scholar]