Abstract
Background:
Proximal hamstring avulsions are severe tendon injuries and are commonly sports-related. Open and endoscopic techniques as well as different anchor configurations have already been described for proximal hamstring repair. Novel all-suture anchors have been developed to provide decreased bone loss during placement and reduced occupied bone volume when compared with titanium suture anchors.
Hypothesis:
Complete proximal hamstring avulsions repaired with all-suture anchors will demonstrate equal load to failure and comparable displacement under cyclic loading when compared with titanium suture anchors.
Study Design:
Controlled laboratory study.
Methods:
Complete proximal hamstring avulsions were created in 18 paired cadaveric specimens (mean ± SD age, 63.0 ± 10.4 years). Either all-suture anchors or titanium suture anchors were used for repair. Cyclic loading from 10 to 125 N at 1 Hz was performed for 1500 cycles with a material testing machine. Displacement was assessed along anterior and posterior aspects of the tendon repair with optical tracking. Specimens were loaded to failure at a rate of 120 mm/min. Displacement, load to failure, and repair construct stiffness were compared between matched pairs with the Wilcoxon signed-rank test. Correlations were determined by Spearman rho analysis.
Results:
The all-suture anchors showed significantly higher load-to-failure values when compared with the titanium anchor repairs (799.64 ± 257.1 vs 573.27 ± 89.9 N; P = .008). There was no significant difference in displacement between all-suture anchors and titanium suture anchors at the anterior aspect (6.60 ± 2.2 vs 5.49 ± 1.1 mm; P = .26) or posterior aspect (5.87 ± 2.08 vs 5.23 ± 1.37 mm; P = .678) of the repaired hamstring tendons.
Conclusion:
All-suture anchors demonstrated similar displacement and superior load to failure when compared with titanium suture anchors.
Clinical Relevance:
The results of this study suggest that all-suture anchors are an equivalent alternative to titanium suture anchors for proximal hamstring avulsion repair.
Keywords: proximal hamstring avulsion, hip, all-suture anchor, titanium suture anchor, biomechanics, proximal hamstring repair
Hamstring injuries are one of the most common injuries in sports and can reach a prevalence up to 25%, depending on the sport.8,9,20,26,28 Both athletes and middle-aged individuals are affected by proximal hamstring avulsions, which account for up to 11% of all hamstring injuries and result in significant functional impairment.3,6,9,16,20,37 Surgical treatment of proximal hamstring avulsions is preferred over nonoperative treatment due to superior subjective clinical outcomes, strength, and endurance as well as faster return to sports.18,30,36 Early surgical intervention within 4 to 6 weeks after trauma is associated with a quicker return to preinjury level of play, decreased muscle retraction, and less risk of operative complications.2,18,36
Multiple techniques for proximal hamstring repair have been described; these include transosseous sutures or suture anchors in variable numbers, sizes, and configurations.5,11,17,27 Recently developed all-suture anchors show decreased bone loss with reduced bone volume occupied as compared with traditional anchors.10,12,23 A lower drill diameter allows easier surgical revision and makes all-suture anchors a reasonable alternative to metal implants in revision cases.12 Furthermore, the lack of metal components in all-suture anchors enables detailed postoperative follow-up with magnetic resonance imaging (MRI). Schröder et al34 reported that the use of titanium suture anchors produced metal artifacts on MRI that prevented the accurate diagnosis of rotator cuff retears in one-third of their patients.
There are currently no data available showing that all-suture anchors are a comparable biomechanical alternative for proximal hamstring repair. The aim of this study was to compare the biomechanical properties of metal suture anchors with all-suture anchors for proximal hamstring repairs. We hypothesized that the 2 types of suture anchors would demonstrate equal load to failure and comparable displacement under cyclic loading.
Methods
We obtained 18 hemipelvis pairs from 9 donors (mean ± SD age, 63.0 ± 10.4 years; 5 females, 4 males) through Science Care. This study was presented to the institutional review board of the University of Connecticut via a Human Research Determination Form, and it was determined that approval was not required, as deidentified specimens are not regarded as human subject research.
Specimens were placed prone, and an open posterior approach was used to reflect the gluteus maximus medially and superiorly to expose the proximal insertion of the semimembranosus, semitendinosus, and the long head of the biceps femoris at the ischial tuberosity. The hamstring muscles were separated from the femur before the femur was disarticulated from the acetabulum. All other soft tissue was carefully removed from the pelvis to preserve the isolated hamstring insertion. Dissected specimens were stored in a freezer at –20° C. Specimens were thawed 24 hours in advance of biomechanical testing.
Bone mineral density at the ischial tuberosity was evaluated by using DexaScan (XL Image Densitometer; GE/Lunar Expert) before biomechanical testing. Matched hemipelvises from each donor were randomized to be fixed with either titanium suture anchors or all-suture anchors. The repair technique was based on prior publications from Harvey et al19 and Sandmann et al31 and represented the standard surgical application of anchors for open proximal hamstring repair.
Prior to repair, the hamstring tendons were completely removed from the ischial tuberosity to re-create a complete avulsion.
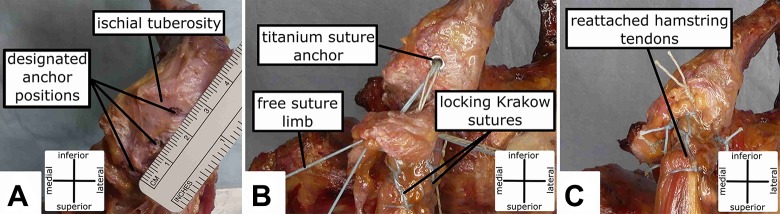
Titanium Suture Anchor Technique
Three unicortical bone sockets19 separated by 12 mm were prepared in line, proximal to distal, with a 3.2-mm drill at the anatomic proximal hamstring insertion along the ischial tuberosity (Figure 1A). Three 5.5 × 16.3–mm titanium Corkscrew (Arthrex) anchors preloaded with No. 2 FiberWire (Arthrex) suture were placed into the aforementioned sockets (Figure 1B). One suture limb from each anchor was used to augment the tendon with a locking Krakow suture pattern along a 2-cm length from the insertion. The tendon was then repositioned into its anatomic footprint by pulling on the free suture limb before being tied securely to the stitching limb with 8 surgical knots (Figure 1C). The use of 8 surgical knots to preclude knot failure has been implemented by our laboratory in previous biomechanical pilot studies.
Figure 1.
(A) Position marking for the 3 unicortical bone sockets, each separated 12 mm from the other. (B) Embedded titanium suture anchors with locking Krakow suture. (C) Proximal hamstring tendons reattached to the anatomic footprint.
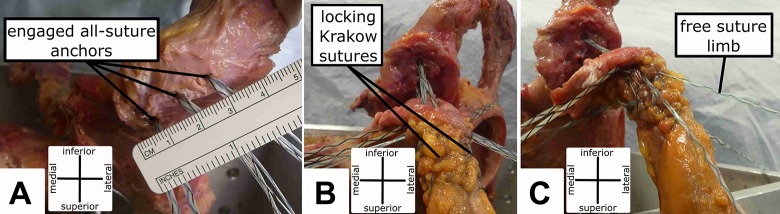
All-Suture Anchor Technique
Three unicortical bone sockets19 separated by 12 mm were prepared in line with a 2.6-mm drill (Arthrex) at the anatomic proximal hamstring insertion along the ischial tuberosity. Each FiberTak (Arthrex) anchor was passed into the drill guide and securely deployed into its socket (Figure 2A). The locking Krakow pattern, tendon repositioning, and knotting were accomplished according to the previous description with the 1.3-mm SutureTape (Arthrex) loaded into each all-suture anchor (Figure 2, B and C).
Figure 2.
(A) Three unicortical bone sockets with engaged all-suture anchors. (B) Proximal hamstring tendon with interlocking Krakow suture. (C) Repositioning of the proximal hamstring tendon by pulling the free suture limb.
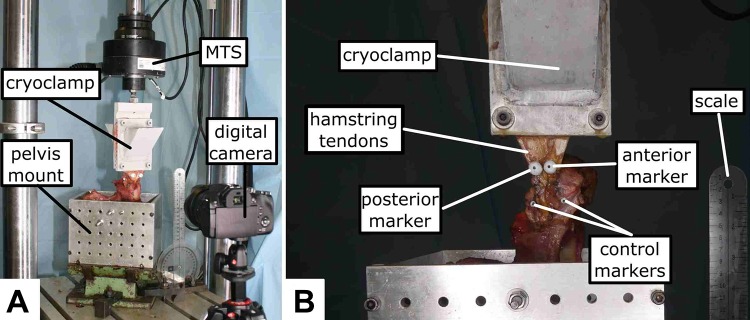
Biomechanical Testing
The current biomechanical setup was based on a prior publication by Harvey et al.19 The hemipelvis specimens were secured at 0° of hip flexion (Figure 3A).19 Three rigid metal rods were drilled through the pelvis and securely fixed to the customized fixture box. The flexion angle was achieved by vertically aligning the anterior iliac spine with the pubic tubercle.19 The proximal hamstring was secured at the myotendinous junction 3 cm from the end of the suture with a cryoclamp attached to a vertical loading actuator such that the force vector was constantly applied at 0° of hip flexion (Figure 3B). A material testing system machine (MTS 858 Mini-Bionix) was used to assess the biomechanical properties of both repairs under cyclic loading and load to failure. Specimens were preloaded at 5 N, held for 5 seconds, and then cyclically loaded from 10 to 125 N at 1 Hz for 1500 cycles. These force loads were based on the findings of Schache et al33 as well as the biomechanical setup of Harvey et al19 to simulate cyclic stretching and shortening of the hamstring muscles during sprinting. Load to failure was performed after the last cycle at a constant rate of 120 mm/min. Mode of failure was recorded for each specimen.
Figure 3.
(A) Specimen secured by metal rods in the custom fixture box. (B) Optical tracking was performed with 4 markers at 0° of hip flexion. MTS, material testing system.
Motion Analysis
Displacement of the repair was measured by optical tracking with 4 markers.19 One pair was placed on the reattached tendon 20 mm from the tendon footprint at the end level of the sutures, and another pair was placed on the medial and lateral margin of the ischial tuberosity to serve as control (Figure 3B). Digital motion analysis was performed with Kinovea (v 0.8.27) to track displacement from the cyclic loading recordings. Puig-Diví et al29 have confirmed the validity and reliability for Kinovea as an accurate measurement tool. A standard error of measurement between 0.00 and 0.07 and a minimum detectable change between 0.00 and 0.19 were reported while Kinovea was used for optical tracking.29 Normalized displacements were determined for the anterior and posterior marker pairs by subtracting the displacement of the control markers from their corresponding tendon markers. To completely capture the tendon displacement and given the broad insertion of the hamstring tendons, tendon markers as well as control markers were positioned at the anterior and posterior aspects.
Statistical Analysis
Power analysis was performed with outcome parameters published by Harvey et al.19 For load to failure, a standard deviation of 100 N was assumed. A sample size of 9 specimens per group was determined to provide 80% power to detect a 135-N difference in load to failure at an α of .05. Biomechanical outcomes data were statistically assessed for normal distribution. Given continuous variables and skewed distributions, the nonparametric Wilcoxon signed-rank test was used to determine if there was a statistically significant difference in outcomes between matched pairs. Correlation between continuous variables was assessed with Spearman rho. All statistical analyses were performed with SPSS v 25 (IBM).
Results
There was no significant difference for bone mineral density at the ischial tuberosity between specimens in the all-suture anchor group (0.59 ± 0.22 g/cm2) and the titanium suture anchor group (0.67 ± 0.26 g/cm2; P = .173).
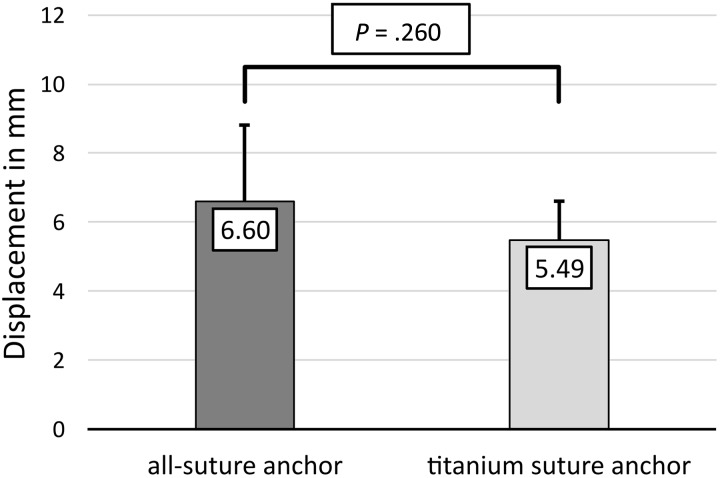
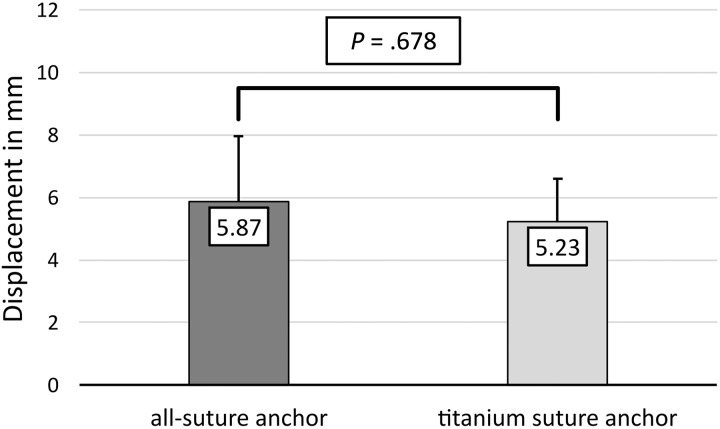
After 1500 cycles, the mean displacement at the anterior aspect of the repaired tendon did not significantly differ between all-suture anchors and titanium suture anchors (6.60 ± 2.2 vs 5.49 ± 1.1 mm; P = .260) (Figure 4). The displacement of the posterior aspect of the repaired hamstring tendons was not significantly different between all-suture anchors and titanium anchors (5.87 ± 2.08 vs 5.23 ± 1.37 mm; P = .678) (Figure 5).
Figure 4.
Comparison of displacement (in millimeters) at the anterior aspect of the repaired hamstring tendon between all-suture anchors and titanium suture anchors after 1500 cycles. Data reported as means with SD (error bars).
Figure 5.
Comparison of displacement (in millimeters) at the posterior aspect of the repaired hamstring tendons between all-suture anchors and titanium suture anchors after 1500 cycles. Data reported as means with SD (error bars).
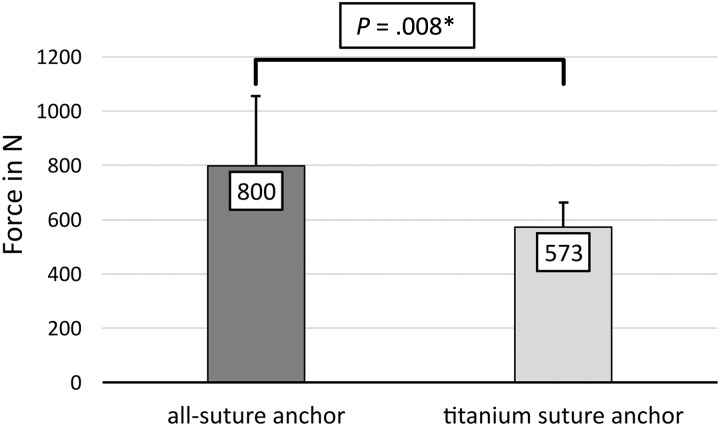
Significantly higher mean peak load to failure was observed for all-suture anchor repairs in comparison with titanium suture anchor repairs (799.64 ± 257.1 vs 573.27 ± 89.9 N; P = .008) (Figure 6). Mean repair construct stiffness was 33.67 ± 8.99 N/mm in the all-suture group and 37.09 ± 8.11 N/mm in the titanium suture anchor group (P = .374). Suture rupture was the most common mode of failure for both repairs. In all cases of suture failure in the titanium suture anchor group, the suture ruptured at the suture-anchor interface. For all-suture anchors, suture rupture occurred at the midsuture section. Additionally, there were 3 failures by soft tissue tearing in the all-suture anchor group and 2 failures by anchor pullout in the titanium suture anchor group.
Figure 6.
Comparison of peak load (in newtons) to failure between all-suture anchor repairs and titanium suture anchor repairs. Data reported as means with SD (error bars). *Statistically significant difference.
Spearman rank correlation showed that bone mineral density and stiffness were not significantly correlated with displacement or load-to-failure values. Anterior and posterior displacement values were significantly correlated with each other for the titanium suture anchor repair (ρ = 0.867; P = .002) and all-suture anchor repair (ρ = 0.883; P = .002). Load to failure was significantly correlated with posterior displacement for the titanium suture anchor repair only (ρ = –0.667; P = .05).
Discussion
The most important finding of this study was that proximal hamstring avulsions repaired with all-suture anchors demonstrated a significantly higher load to failure with equal displacement under cyclic loading as compared with avulsions repaired with titanium anchors. Our findings showed that all-suture anchors are a comparable biomechanical alternative to titanium suture anchors for proximal hamstring repair. Surgeons can expect higher primary stability if all-suture anchors are used for proximal hamstring repair. Furthermore, the surgeon can take advantage of a lower drill diameter, which facilitates revision surgery and the possibility of a detailed postoperative follow-up with MRI.
Displacement after cyclic loading was not significantly different between the 2 repair groups in the current study. Previously published studies demonstrated a mean displacement between 2.39 and 7.36 mm for hamstring repairs with solid anchors.17,19 The observed displacement values in our study are within this range and thus are representative of the current literature. At present, there is no known displacement value that indicates clinical failure of the hamstring tendons. Previous studies extrapolated thresholds from rotator cuff repairs, using displacement values between 5 and 10 mm as the parametric range for mechanical failure of the repaired hamstring tendons.4,19,40 In comparison, the current threshold for clinical failure of a distal biceps repair is 10 mm of displacement in the bone-tendon unit.25,35 Proximal hamstring repairs in our study showed mean displacement values below the threshold for failure of rotator cuff and distal biceps repairs.
The hamstring muscle complex varies from the biceps brachii muscle anatomically and biomechanically.13,24,38 The insertion footprint of the distal biceps brachii is much smaller than that of the hamstring complex,24 measuring only 2.8 cm2. In comparison, the common footprint13 of the semitendinosus and long head of the biceps femoris measures 5.5 cm2, while the semimembranosus footprint measures 5.4 cm2. Additionally, the fibers of the proximal hamstring tendon are aligned vertically to their attachment site at the ischial tuberosity, whereas the biceps brachii tendon rotates 90° as it crosses the elbow joint and inserts obliquely onto the radial tuberosity.32,39 It is thus very likely that the threshold for clinical failure due to displacement in hamstring repairs is higher than in biceps repair.
Recent biomechanical studies have reported loads to failure for proximal hamstring repairs using various constructs.14,17,19 Harvey et al19 found that specimens fixed with three 2.9-mm single-loaded biocomposite anchors withstood a mean maximum load of 326 N. In a study by Hamming et al,17 specimens were tested after hamstring repair with two 2.9-mm anchors (2-S), two 5.5-mm anchors (2-L), or five 2.9-mm anchors (5-S). Mean maximum load to failure was 474 N for the 2-S repair, 543 N for the 2-L repair, and 1164 N for the 5-S repair.17 Gerhardt et al14 evaluated a knotless anchor configuration with suture tapes and observed a mean peak load to failure of 767 N. Our data for mean peak load to failure of all-suture anchors as well as titanium anchors are within the range reported in current literature.
For the native proximal hamstring tendons, a mean peak load to failure between 750 and 1405 N has been reported.14,17 The mean peak load to failure of all-suture anchors is within the observed range of native hamstring tendons. The load to failure of 1405 N for native proximal hamstring tendons17 shows the magnitude of hamstring forces on their insertion and may warrant the use of early postoperative treatment with a hip and knee orthosis to prevent reruptures.3,7 Additionally, no failure occurred during cyclic loading in the current study. Here, loads comparable with the forces experienced during sprinting were applied to simulate the cyclic stretching and shortening of the hamstring muscles.19,33 Consequently, both repair techniques should be able to prevent failure during walking and exercising in the early phase of rehabilitation.
There are limitations to this biomechanical study. Because cadaveric hemipelvis specimens were used, the biological influence of healing and the physiological effects of loading on the repair site are unknown. The present study used a validated biomechanical setup, introduced by Harvey et al19 except for the motion analysis software. However, the motion analysis software was evaluated by Grigg et al15 in a marker-less motion capture study that showed high intratester reliability and low absolute error in kinematic measurements. Another recent study demonstrated the validity and reliability of Kinovea as an accurate tool for optical tracking.29 To minimize the possible influence of specimen slippage on the collected data, a cryoclamp, standardized tendon markers, a validated video analysis tool, and corrected displacement values were used. To evaluate each specimen with a comparable repair, a standardized linear anchor configuration, which was validated in a prior biomechanical study, was applied.19 As shown by Hamming et al17 and Gerhardt et al,14 the amount and configuration of anchors influence the load to failure. Under consideration of these findings, our results are limited to a linear anchor configuration. The anchors evaluated in this study might show higher failure loads in other configurations.
Bisson and Manohar1 demonstrated no difference between No. 2 FiberWire suture (Arthrex) and 2-mm FiberWire tape (Arthrex) in elongation or stiffness but showed a significantly higher ultimate tensile load for FiberWire tape. Liu et al22 reported significantly higher failure loads for double-row repairs with 2-mm FiberWire tape in comparison with No. 2 FiberWire in an ovine rotator cuff repair model. Leishman and Chudik21 compared SutureTape and No. 2 FiberWire in a biomechanical study and observed significant higher knot security, tensile stiffness, and failure loads for SutureTape. These recent findings show that the suture material in the all-suture anchors and titanium suture anchors in this study possessed different biomechanical properties, and this must be considered by the surgeon choosing between both anchor types for proximal hamstring repair. The observed differences in the current study might not only be the result of different anchor types but might also be due to different suture material. Although the titanium suture anchors and all-suture anchors in this study were distinguished by suture material, the titanium suture anchors represent a standard implant and are an appropriate reference when evaluating a new anchor type. Furthermore, our data for mean peak load to failure and displacement for both anchors were within a representative range reported in the current literature.14,17,19
To our knowledge, a biomechanical evaluation of all-suture anchors for proximal hamstring repairs had not been previously performed. Overall, there was a comparable displacement between the 2 types of suture anchors and a significantly higher load to failure in the all-suture anchor repairs. Future clinical use of these anchors is needed to further validate these promising results and show the relevance and advantages of all-suture anchors in terms of return to preinjury level and outcomes. Further analysis of different anchors currently used for proximal hamstring repair would be interesting for a future study assessing the economic efficiency between the current implant types.
Conclusion
All-suture anchors with suture tape showed similar displacement and superior load to failure compared with titanium anchors with high-strength suture, demonstrating that they can be used as an equivalent alternative to titanium anchors in proximal hamstring avulsion repair.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: The University of Connecticut Health Center/UConn Musculoskeletal Institute has received direct funding and material support for this study from Arthrex. A.O. received material support from Arthrex during the conduct of this study. A.B.I. has received consulting fees from Arthrosurface, Arthrex, and Medi. K.B. has received consulting fees from Arthrex. A.D.M. has received grant support and consulting fees from Arthrex and honoraria from Arthrosurface. K.C. has received educational support from Arthrex and Pylant Medical, speaking fees from Arthrex, consulting fees from Johnson & Johnson, and hospitality payments from Biomet and Smith & Nephew. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was waived by the University of Connecticut Institutional Review Board.
References
- 1. Bisson LJ, Manohar LM. A biomechanical comparison of the pullout strength of No. 2 FiberWire suture and 2-mm FiberWire tape in bovine rotator cuff tendons. Arthroscopy. 2010;26(11):1463–1468. [DOI] [PubMed] [Google Scholar]
- 2. Bodendorfer BM, Curley AJ, Kotler JA, et al. Outcomes after operative and nonoperative treatment of proximal hamstring avulsions: a systematic review and meta-analysis. Am J Sports Med. 2018;46(11):2798–2808. [DOI] [PubMed] [Google Scholar]
- 3. Brucker PU, Imhoff AB. Functional assessment after acute and chronic complete ruptures of the proximal hamstring tendons. Knee Surg Sports Traumatol Arthrosc. 2005;13(5):411–418. [DOI] [PubMed] [Google Scholar]
- 4. Burkhart SS, Diaz Pagàn JL, Wirth MA, Athanasiou KA. Cyclic loading of anchor-based rotator cuff repairs: confirmation of the tension overload phenomenon and comparison of suture anchor fixation with transosseous fixation. Arthroscopy. 1997;13(6):720–724. [DOI] [PubMed] [Google Scholar]
- 5. Chakravarthy J, Ramisetty N, Pimpalnerkar A, Mohtadi N. Surgical repair of complete proximal hamstring tendon ruptures in water skiers and bull riders: a report of four cases and review of the literature. Br J Sports Med. 2005;39(8):569–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cohen S, Bradley J. Acute proximal hamstring rupture. J Am Acad Orthop Surg. 2007;15(6):350–355. [DOI] [PubMed] [Google Scholar]
- 7. Cohen SB, Rangavajjula A, Vyas D, Bradley JP. Functional results and outcomes after repair of proximal hamstring avulsions. Am J Sports Med. 2012;40(9):2092–2098. [DOI] [PubMed] [Google Scholar]
- 8. Croisier J-L. Factors associated with recurrent hamstring injuries. Sports Med. 2004;34(10):681–695. [DOI] [PubMed] [Google Scholar]
- 9. Dalton SL, Kerr ZY, Dompier TP. Epidemiology of hamstring strains in 25 NCAA sports in the 2009-2010 to 2013-2014 academic years. Am J Sports Med. 2015;43(11):2671–2679. [DOI] [PubMed] [Google Scholar]
- 10. Dhawan A, Ghodadra N, Karas V, Salata MJ, Cole BJ. Complications of bioabsorbable suture anchors in the shoulder. Am J Sports Med. 2012;40(6):1424–1430. [DOI] [PubMed] [Google Scholar]
- 11. Domb BG, Linder D, Sharp KG, Sadik A, Gerhardt MB. Endoscopic repair of proximal hamstring avulsion. Arthrosc Tech. 2013;2(1):e35–e39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Erickson J, Chiarappa F, Haskel J, et al. Biomechanical comparison of a first- and a second-generation all-soft suture glenoid anchor. Orthop J Sports Med. 2017;5(7):2325967117717010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Feucht MJ, Plath JE, Seppel G, Hinterwimmer S, Imhoff AB, Brucker PU. Gross anatomical and dimensional characteristics of the proximal hamstring origin. Knee Surg Sports Traumatol Arthrosc. 2015;23(9):2576–2582. [DOI] [PubMed] [Google Scholar]
- 14. Gerhardt MB, Assenmacher BS, Chahla J. Proximal hamstring repair: a biomechanical analysis of variable suture anchor constructs. Orthop J Sports Med. 2019;7(2):2325967118824149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Grigg J, Haakonssen E, Rathbone E, Orr R, Keogh JWL. The validity and intra-tester reliability of markerless motion capture to analyse kinematics of the BMX Supercross gate start. Sports Biomech. 2018;17(3):383–401. [DOI] [PubMed] [Google Scholar]
- 16. Guanche CA. Hamstring injuries. J Hip Preserv Surg. 2015;2(2):116–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hamming MG, Philippon MJ, Rasmussen MT, et al. Structural properties of the intact proximal hamstring origin and evaluation of varying avulsion repair techniques: an in vitro biomechanical analysis. Am J Sports Med. 2015;43(3):721–728. [DOI] [PubMed] [Google Scholar]
- 18. Harris JD, Griesser MJ, Best TM, Ellis TJ. Treatment of proximal hamstring ruptures—a systematic review. Int J Sports Med. 2011;32(7):490–495. [DOI] [PubMed] [Google Scholar]
- 19. Harvey MA, Singh H, Obopilwe E, Charette R, Miller S. Proximal hamstring repair strength: a biomechanical analysis at 3 hip flexion angles. Orthop J Sports Med. 2015;3(4):2325967115576910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Heiderscheit BC, Sherry MA, Silder A, Chumanov ES, Thelen DG. Hamstring strain injuries: recommendations for diagnosis, rehabilitation, and injury prevention. J Orthop Sports Phys Ther. 2010;40(2):67–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Leishman DJ, Chudik SC. Suture tape with broad full-width core versus traditional round suture with round core: a mechanical comparison. Arthroscopy. 2019;35(8):2461–2466. [DOI] [PubMed] [Google Scholar]
- 22. Liu RW, Lam PH, Shepherd HM, Murrell GAC. Tape versus suture in arthroscopic rotator cuff repair: biomechanical analysis and assessment of failure rates at 6 months. Orthop J Sports Med. 2017;5(4):2325967117701212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Mazzocca AD, Chowaniec D, Cote MP, et al. Biomechanical evaluation of classic solid and novel all-soft suture anchors for glenoid labral repair. Arthroscopy. 2012;28(5):642–648. [DOI] [PubMed] [Google Scholar]
- 24. Mazzocca AD, Cohen M, Berkson E, et al. The anatomy of the bicipital tuberosity and distal biceps tendon. J Shoulder Elbow Surg. 2007;16(1):122–127. [DOI] [PubMed] [Google Scholar]
- 25. Pereira DS, Kvitne RS, Liang M, Giacobetti FB, Ebramzadeh E. Surgical repair of distal biceps tendon ruptures: a biomechanical comparison of two techniques. Am J Sports Med. 2002;30(3):432–436. [DOI] [PubMed] [Google Scholar]
- 26. Petersen J, Hölmich P. Evidence based prevention of hamstring injuries in sport. Br J Sports Med. 2005;39(6):319–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Pombo M, Bradley JP. Proximal hamstring avulsion injuries: a technique note on surgical repairs. Sports Health. 2009;1(3):261–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Prior M, Guerin M, Grimmer K. An evidence-based approach to hamstring strain injury: a systematic review of the literature. Sports Health. 2009;1(2):154–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Puig-Diví A, Escalona-Marfil C, Padullés-Riu JM, Busquets A, Padullés-Chando X, Marcos-Ruiz D. Validity and reliability of the Kinovea program in obtaining angles and distances using coordinates in 4 perspectives. PLoS One. 2019;14(6):e0216448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Rust DA, Giveans MR, Stone RM, Samuelson KM, Larson CM. Functional outcomes and return to sports after acute repair, chronic repair, and allograft reconstruction for proximal hamstring ruptures. Am J Sports Med. 2014;42(6):1377–1383. [DOI] [PubMed] [Google Scholar]
- 31. Sandmann GH, Hahn D, Amereller M, et al. Mid-term functional outcome and return to sports after proximal hamstring tendon repair. Int J Sports Med. 2016;37(7):570–576. [DOI] [PubMed] [Google Scholar]
- 32. Sato K, Nimura A, Yamaguchi K, Akita K. Anatomical study of the proximal origin of hamstring muscles. J Orthop Sci. 2012;17(5):614–618. [DOI] [PubMed] [Google Scholar]
- 33. Schache AG, Dorn TW, Blanch PD, Brown NAT, Pandy MG. Mechanics of the human hamstring muscles during sprinting. Med Sci Sports Exerc. 2012;44(4):647–658. [DOI] [PubMed] [Google Scholar]
- 34. Schröder FF, Huis In’t Veld R, den Otter LA, van Raak SM, Ten Haken B, Vochteloo AJH. Metal artefacts severely hamper magnetic resonance imaging of the rotator cuff tendons after rotator cuff repair with titanium suture anchors. Shoulder Elbow. 2018;10(2):107–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Spang JT, Weinhold PS, Karas SG. A biomechanical comparison of EndoButton versus suture anchor repair of distal biceps tendon injuries. J Shoulder Elbow Surg. 2006;15(4):509–514. [DOI] [PubMed] [Google Scholar]
- 36. Subbu R, Benjamin-Laing H, Haddad F. Timing of surgery for complete proximal hamstring avulsion injuries: successful clinical outcomes at 6 weeks, 6 months, and after 6 months of injury. Am J Sports Med. 2015;43(2):385–391. [DOI] [PubMed] [Google Scholar]
- 37. van der Made AD, Reurink G, Gouttebarge V, Tol JL, Kerkhoffs GM. Outcome after surgical repair of proximal hamstring avulsions: a systematic review. Am J Sports Med. 2015;43(11):2841–2851. [DOI] [PubMed] [Google Scholar]
- 38. van der Made AD, Wieldraaijer T, Kerkhoffs GM, et al. The hamstring muscle complex. Knee Surg Sports Traumatol Arthrosc. 2015;23(7):2115–2122. [DOI] [PubMed] [Google Scholar]
- 39. Walton C, Li Z, Pennings A, Agur A, Elmaraghy A. A 3-dimensional anatomic study of the distal biceps tendon: implications for surgical repair and reconstruction. Orthop J Sports Med. 2015;3(6):2325967115585113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Waltrip RL, Zheng N, Dugas JR, Andrews JR. Rotator cuff repair: a biomechanical comparison of three techniques. Am J Sports Med. 2003;31(4):493–497. [DOI] [PubMed] [Google Scholar]