Abstract
Hemorrhage is one of the most obvious pathological phenomena in grass carp reovirus (GCRV) infection. The etiology of GCRV-induced hemorrhage is unclear. We found inducible nitric oxide synthase (iNOS) may relate to viral hemorrhage according to the previous studies, which is expressed at high levels after GCRV infection and is related to apoptosis. In this study, we aimed to investigate the mechanism of iNOS on apoptosis and hemorrhage at the cell level and individual level on subjects who were infected with GCRV and treated with S-methylisothiourea sulfate (SMT), an iNOS inhibitor. Cell structure, apoptosis rate, and hemorrhage were evaluated through fluorescence microscopy, Annexin V-FITC staining, and H&E staining, respectively. Cell samples and muscle tissues were collected for Western blotting, NO concentration measure, caspase activity assay, and qRT-PCR. iNOS-induced cell apoptosis and H&E staining showed that the vascular wall was broken after GCRV infection in vivo. When the function of iNOS was inhibited, NO content, apoptosis rate, caspase activity, and hemorrhage were reduced. Collectively, these results suggested iNOS plays a key role in apoptosis of vascular endothelial cells in GCRV-induced hemorrhage. This study is the first to elucidate the relationship between iNOS-induced cell apoptosis and GCRV-induced hemorrhage, which lays the foundation for further mechanistic research of virus-induced hemorrhage.
Keywords: inducible nitric oxide synthase, S-methylisothiourea sulfate, grass carp reovirus, hemorrhage, apoptosis
1. Introduction
Hemorrhage is a common pathological phenomenon. It could happen anywhere in the body where blood vessels are damaged. It can develop as a result of traumatic injury, fungal infection (such as Alternaria species, Cladosporium species, and Curvularia species) [1,2], bacterial infection (such as Pseudomonas fluorescens, and Aeromonas hydrophila) [3,4], viral infection (such as hantavirus, ebolavirus, and grass carp reovirus) [5,6,7], and some unknown causes. Hemorrhage is one of the most observable pathological phenomena in grass carp reovirus (GCRV) infection [8,9]. GCRV can cause hemorrhage disease in grass carp (Ctenopharyngodon idella) [10], black carp (Mylopharyngodon piceus) [11], rare minnow (Gobiocypris rarus) [12], etc. GCRV is a highly pathogenic viral agent that results in huge losses to the grass carp industry [13]. GCRV is icosahedron dsRNA virus without envelope, a member of the genus Aquareovirus and the family Reoviridae. GCRV is divided into three types (GCRV-I, GCRV-II and GCRV-III), and GCRV-II is the most prevalent strain in recent years in China [14]. In the present study, the GCRV097 strain (GCRV-II) is employed.
Previous research has shown that inducible nitric oxide synthase (iNOS) may be related to hemorrhage disease [15,16]. iNOS is one of four isoforms in the family of nitric oxide synthases (NOSs). Neuronal NOS (nNOS) exists in nervous tissue [17]. Endothelial NOS (eNOS) is in the endothelium [18]. Inducible NOS (iNOS) appears in the immune system and cardiovascular system [19]. Bacterial NOS (bNOS) can be found in various Gram-positive bacteria [20]. nNOS and eNOS exist in the neurocyte and endothelium, respectively, and their activities are switched by Ca2+ concentrations. In contrast, the expression of iNOS is determined by the de novo synthesis of iNOS mRNA and protein in various tissue and cell types [21,22]. iNOS significantly affects the responses of 874 genes to cytokines and bacteria. Previous studies showed iNOS regulated about 200 genes and led to at least a two-fold change in expression level [23]. iNOS is regulated by cytokines, viral products, oxygen tension, cell–cell contact, and various antibiotics, but it is not regulated by Ca2+ concentrations. Furthermore, it can produce more nitric oxide (NO) than eNOS and nNOS. NOSs catalyze the arginine to produce NO—an important signaling molecule [24]. NO regulates the normal physiological activity and can also be cytotoxic. The function of NO as regulatory or cytotoxic is determined by the magnitude as well as the duration [25]. NO diffuses into vascular smooth muscle cells and activates the cyclic guanosine monophosphate pathway to elicit vasorelaxation, which helps lower blood pressure. A lack of NO in the kidney has been proposed as a main cause of systemic hypertension [26]. NO has multiple functions in the immune system, such as antimicrobial activity, anti-tumor, tissue-damaging effect, anti-inflammatory-immunosuppressive effect, and more. NO also impedes the adhesion of platelets to endothelium, thus inhibiting healing of the injury of the vessel [23]. The massive quantity of NO produced by iNOS acts as a cytotoxic agent. NO transforms into peroxynitrite (ONOO-), which diffuses through the membranes and causes damage as it is a conjugate acid [27,28]. A smaller amount of ONOO- activates the process of cell apoptosis via inducing damage of the mitochondrion to release cytochrome C [29,30]. Apoptosis is a type of programmed cell death and can be activated through the extrinsic pathway, the intrinsic pathway, and the perforin pathway [31]. Viral infection also can induce cell apoptosis. For example, Dengue virus infects the human microvascular endothelial cells and the viral protease interacts with NF-κB inhibitor. Additionally, p50 and p65 translocate into the nucleus and activate downstream genes. Subsequently, caspase-8 and caspase-9 are activated and the cell apoptosis is developed [32]. Caspase-3 and caspase-9 are aspartate-specific cysteinyl protease and major proteins in the process of apoptosis [33]. Some aquatic viruses, such as Cyprinid herpesvirus 3 and Spring viremia of carp virus, can active caspases to induce apoptosis, and can also up-regulate the expression of iNOS [34].
The coagulation system and anticoagulation system are important components in the blood circulation system [35,36]. The coagulation system is immediately activated after the vascular endothelium is damaged [37]. Platelets bind directly to the underlying collagen, tissue factor pathway and contact activation pathway are also activated, and prothrombin and fibrinogen are subsequently activated. Stable fibrin clots then bind to the injury site to block bleeding [38]. The anticoagulation system balances the blood circulation system by counteracting the coagulation system [39]. Disorders of coagulation and anticoagulation can result in hemorrhage, thrombosis, or bruising [40,41]. Virus infection also affects coagulation and anticoagulation in the circulatory system. For example, disordered anticoagulation of patients caused by Epstein–Barr virus infection leads to intravascular coagulation [42]. Based on previous studies, we chose several factors in the present hemorrhage disease caused by a viral infection, including the coagulation factors: kininogen-1 (kng-1), f2, f3a, f3b and f10, as well as the anticoagulation factors: serine protease inhibitor (serpin) b1, c1, d1, f1, f2b, and g1 [43,44].
Accordingly, in this study, we aimed to investigate the relationship between iNOS, cell apoptosis, and GCRV-induced hemorrhage in order to explain the mechanism of hemorrhage after GCRV infection.
2. Results
2.1. iNOS Relates to Hemorrhage Symptom Caused by GCRV Infection
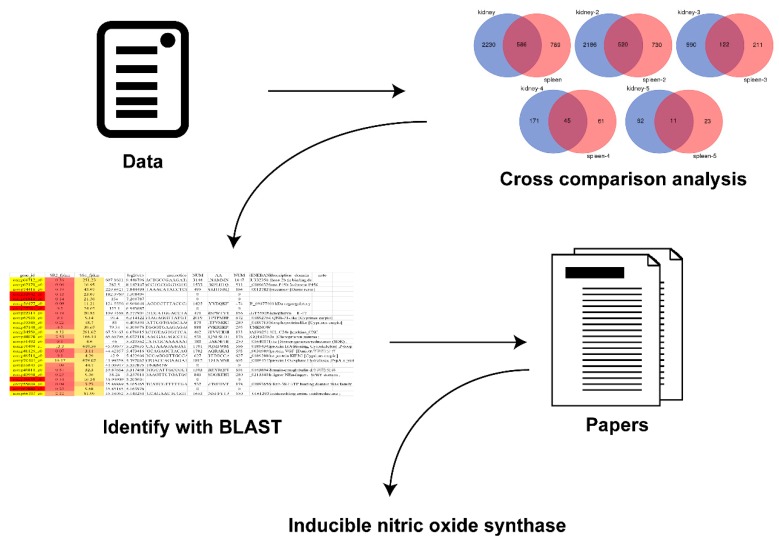
To search the gene that relates with GCRV-induced hemorrhage, the previous research data were employed to carry out a cross-comparison analysis and screen the co-changing genes in multiple organs [15,45]. These genes were identified with BLAST, and an advanced analysis technique was used to identify the gene that relates to hemorrhage (Figure 1). The result indicated that iNOS may play a role in GCRV-induced hemorrhage.
Figure 1.
The process of bioinformatic analysis to find the hemorrhage-related gene, inducible nitric oxide synthase. The previous research data were used to perform a cross-comparison analysis and screen the co-changing genes in multiple organs. Then, the gene was identified with BLAST. Finally, inducible nitric oxide synthase (iNOS) was found.
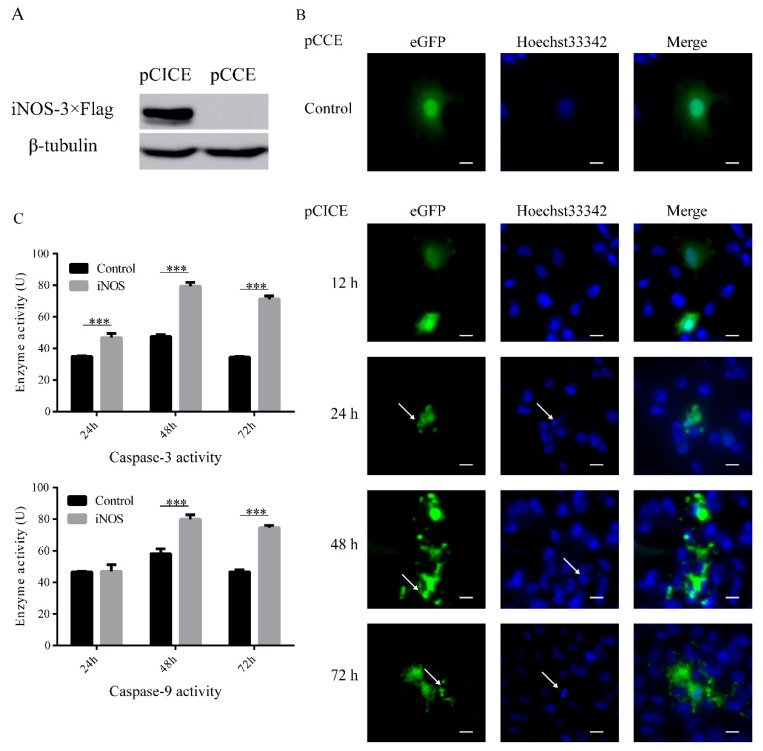
2.2. iNOS Induces Cell Apoptosis
Based on the previous finding, we questioned whether grass carp iNOS could induce cell apoptosis similarly to mammalian iNOS or not. The grass carp iNOS was cloned and FHM cells were transfected with overexpression vector, we found iNOS could over-express in FHM cells (Figure 2A). The plasmid we used could express the green fluorescent protein independently, allowing us to view the status of cells by fluorescence microscopy. The control group showed the complete structures of the cell nucleus and the cell membrane. The samples were collected at 12, 24, 48, and 72 h post transfection. There was no change at 12 h. But from 24 h to 72 h, the nuclei condensed and fragmented. The cells were broken and formed apoptosis bodies (Figure 2B). The activities of caspase-3 and caspase-9 were assayed by Caspase Activity Assay Kits. Caspase-3 and caspase-9 were activated by the overexpression of iNOS via the transfection of pCICE in FHM cells. Caspase-3 was activated at 24 h post transfection, but caspase-9 did not activate. At 48 h and 72 h, the activities of caspase-3 and caspase-9 were significantly up-regulated (Figure 2C).
Figure 2.
iNOS-induced cell apoptosis in FHM. (A) The protein overexpression of iNOS was detected by Western blot. FHM cells were transfected with 800 ng iNOS-3×Flag overexpression vector (pCMV-iNOS-3×Flag-CMV-eGFP, pCICE) in six-well plates. The control group was transfected with 800 ng empty vector (pCMV-CMV-eGFP, pCCE). Cell samples were collected after 24 h for Western blot. (B) iNOS overexpression induced cell apoptosis in FHM. FHM cells were transfected as (A) in glass-bottomed dishes. The samples were collected at 12 h, 24 h, 48 h, and 72 h and Incubated in 4% Paraformaldehyde and Hoechst 33342. The photos were imaged by fluorescence microscopy. There were no changes observed with the control group at 12 h. From 24 h to 72 h, the nuclei condensed and fragmented. The cells were broken and exploded into apoptosis bodies. As the white arrows show (scale 10 μm). (C) iNOS overexpression activated caspase-3 and caspase-9. FHM cells were transfected as (A) in the six-well plate. The samples were collected at 24 h, 48 h, and 72 h and the activity of caspase-3 and 9 were assayed by Caspase Activity Assay Kits. Data were analyzed as the mean ± SEM of the results from three independent experiments. *** p < 0.001.
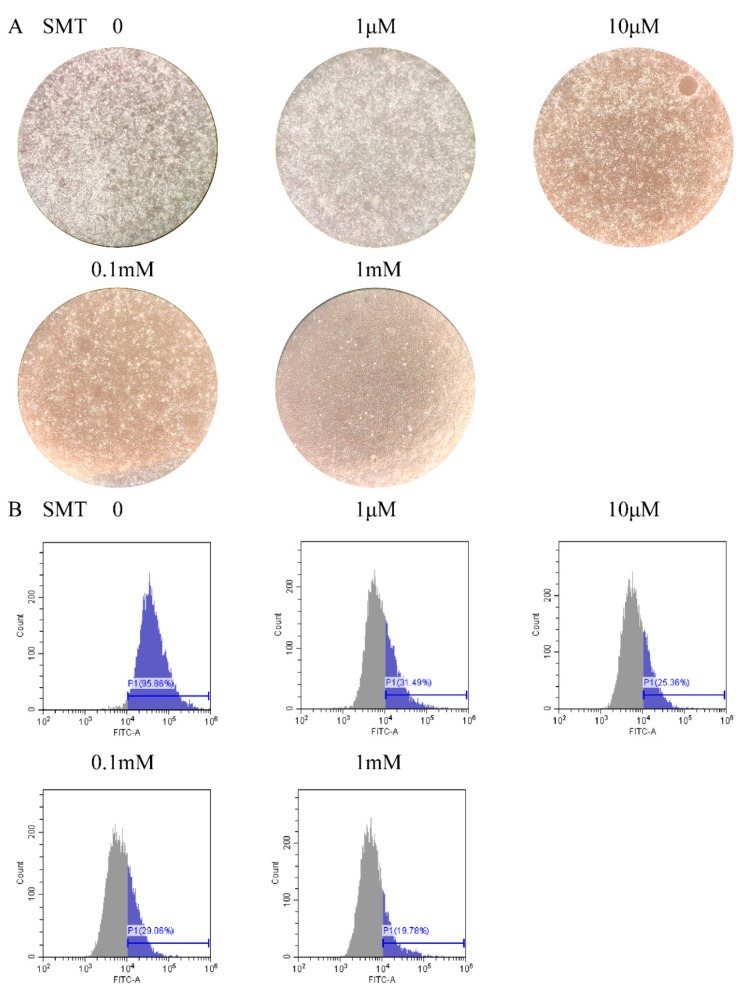
2.3. SMT Inhibits Cell Apoptosis Caused by GCRV Infection
To investigate whether SMT, a selective inhibitor of iNOS, inhibits cell apoptosis caused by GCRV infection via inhibiting iNOS. FHM cells were treated with different concentrations of SMT after GCRV infection. After a 48 h treatment with GCRV and SMT, FHM cells demonstrated evident changes in different SMT concentration treatments. From 0 to 1 mM, the cell lesions were attenuated as the SMT concentration increased and the dead cells and cell debris decreased (Figure 3A). Apoptotic cells were detected by flow cytometry following annexin V-FITC staining in different SMT concentrations. The fluorescent signal of FITC was slacked as the SMT concentration augmented. The percent of apoptotic cells was 95.86% in 0 μM SMT, 31.49% in 1 μM, 25.36% in 10 μM, 29.06% in 0.1 mM and 19.78% in 1 mM (Figure 3B).
Figure 3.
SMT inhibited cell apoptosis in GCRV infection. (A) The cytopathic effect decreased as the SMT concentration increased. FHM cells were infected with GCRV and treated with different SMT concentrations in the six-well plate, imaged by the light microscope (Zoom 100×). The white dots are dead cells and cell debris. (B) The apoptosis rate decreased with the SMT concentration increased. FHM cells in (A) were collected and apoptosis cells were detected by flow cytometry following annexin V-FITC staining. The blue part shows the percent of apoptosis in samples.
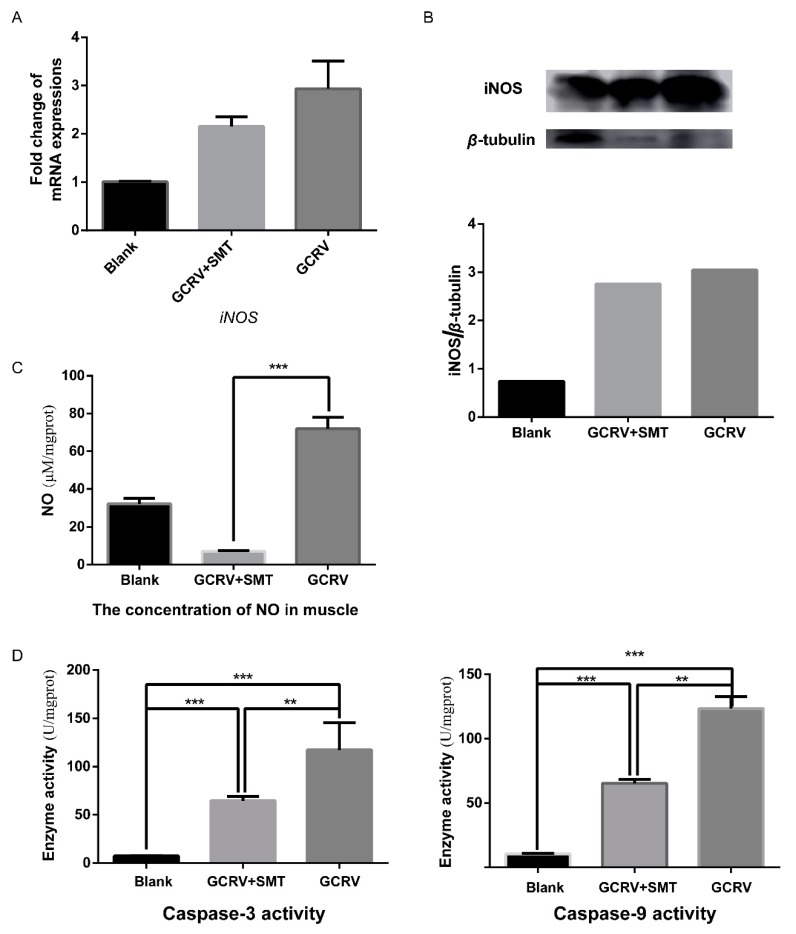
2.4. SMT Suppresses the Function of iNOS in Vivo
Given that SMT can inhibit cell apoptosis in vitro after GCRV infection, we conjectured that SMT can also inhibit cell apoptosis in vivo after GCRV infection. Rare minnow were treated with SMT after GCRV infection, we found SMT did not affect iNOS at the RNA level and the protein level. The RNA level and the protein level of iNOS did not change in the GCRV group compared to the GCRV+SMT group (Figure 4A,B). The concentration of NO in the SMT+GCRV group was significantly lower than that in the GCRV group (Figure 4C). This indicated that SMT significantly inhibits the activity of iNOS in vivo. The activities of caspase-3 and caspase-9 were significantly up-regulated in the SMT+GCRV group and the GCRV group than those in the Blank group, and the activities of caspase-3 and caspase-9 in the GCRV+SMT group were significantly lower than those in the GCRV group. The activities of caspase-3 and caspase-9 were significantly down-regulated upon reducing the concentration of NO (Figure 4D).
Figure 4.
SMT did not reduce iNOS expressions but inhibited NO production and caspase activities in vivo. (A) SMT had no effect on the mRNA transcription of iNOS by qRT-PCR (n = 3). (B) SMT had no effect on the protein expression of iNOS. The expression of iNOS was detected by Western blot, and quantitated by ImageJ. (C) The NO content in muscle was significantly decreased in GCRV+SMT group VS. GCRV group. Quantification of NO production was assayed by NO Content Assay Kit (n = 3). (D) The activities of caspases were significantly decreased in GCRV+SMT group VS. GCRV group. The activity of caspase-3 and 9 were assayed by Caspase Activity Assay Kits (n = 3). (** p < 0.01, *** p < 0.001).
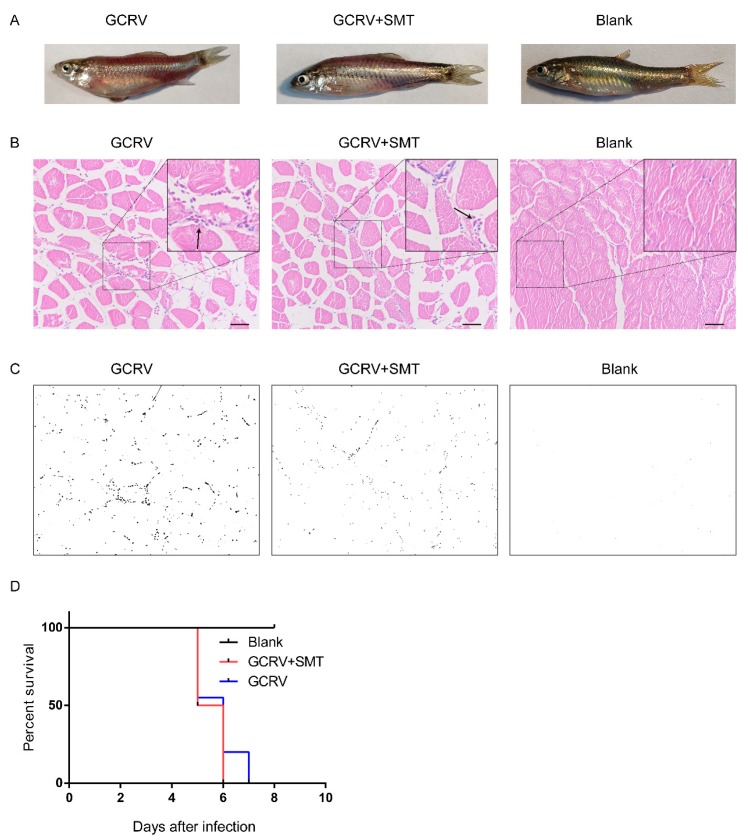
2.5. The Hemorrhage is Reduced When Inhibiting the Function of iNOS
To verify the relationship between hemorrhage—an obvious pathological phenomenon after GCRV infection—and the overexpression of iNOS after GCRV infection, rare minnow were treated with SMT after GCRV infection. Hemorrhagic symptoms appeared on day 5 post-GCRV injection in the GCRV group and GCRV+SMT group. In the GCRV group, the gloss on the body surface was fading and the muscle had acute hemorrhage. In the GCRV+SMT group, the gloss on the body surface was fading, but by a lesser degree than that of the GCRV group, and the muscle hemorrhage was also less than that in the GCRV group. In the blank group, the gloss on the body surface was normal and there was no subcutaneous hemorrhage (Figure 5A). Based on H&E stain analysis of muscle sections, the gap among the muscle cells became larger in the GCRV group and GCRV+SMT group compared to the blank group, likely edema, and the blood cells infiltrated in the gap (Figure 5B). The percent of the blood cell infiltration was calculated by ImageJ (1.51k, National Institutes of Health, Bethesda, MD, USA): GCRV group was 1.14930%, GCRV+SMT group was 0.40659%, and blank group was 0.00929%. The black dots showed the blood cells in muscle tissue (Figure 5C). Rare minnow died starting from the fifth day after GCRV infection and all died by the seventh day (Figure 5D).
Figure 5.
Hemorrhage status in individuals. (A) Hemorrhage was decreased when inhibiting the function of iNOS by SMT. Viewed from the surface of the rare minnow in different groups. The fading of the glossiness of the body surface and severe subcutaneous hemorrhage could be observed in the GCRV group. The slight fading of the glossiness of the body surface and minor subcutaneous hemorrhage in the GCRV+SMT group. The blank group has a normal body color and no subcutaneous hemorrhage. (B) H&E-stained sections show the infiltration of blood cells in muscle in different treatments. The black arrows show the blood cells (scale 50 μm). (C) The H&E-stained sections from (B) were analyzed with ImageJ image-analysis software to calculate the percent of blood cell infiltration. Black dots show the blood cells in muscle tissue. (D) Rare minnow died from the fifth day after GCRV infection and all died on the seventh day.
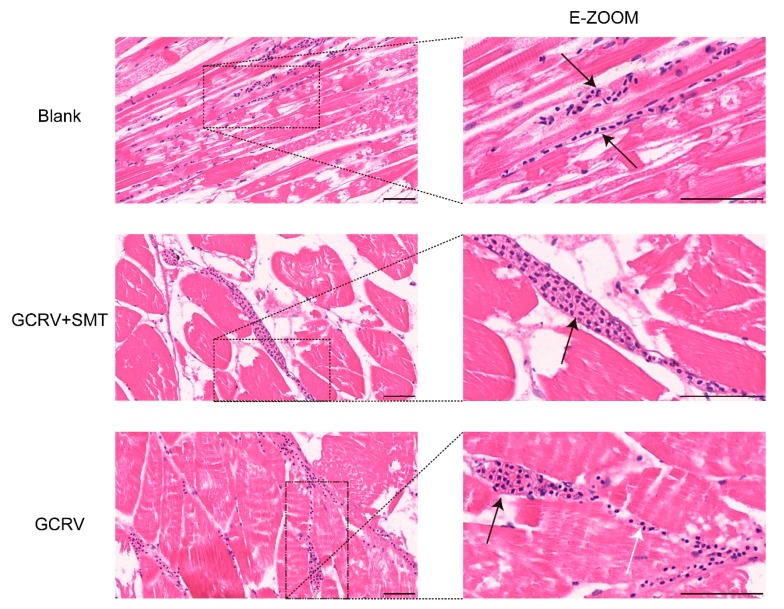
2.6. iNOS Breaks the Vascular Wall Via Activating Cell Apoptosis
To determine the status of vessels in different treatments, H&E stained sections were made. We found the capillary in the blank group is intact with a clear capillary wall and no damage. The red blood cells passed in a line through the capillary. In the GCRV+SMT group, most of the vascular wall was still complete with partial blood cell infiltration. In the GCRV group, the vascular wall was damaged and not clear. The blood cells that were located in the tissue gap were from the damaged vessel (Figure 6).
Figure 6.
The vascular injury was inhibited when inhibiting the function of iNOS by SMT. H&E-stained sections of the vessel in different treatments (scale 50 μm). The vascular wall was broken and the infiltration of blood cells could be observed in the GCRV group. The vascular wall was complete in GCRV+SMT and blank. The black arrow shows the vessel and the white shows hemorrhage.
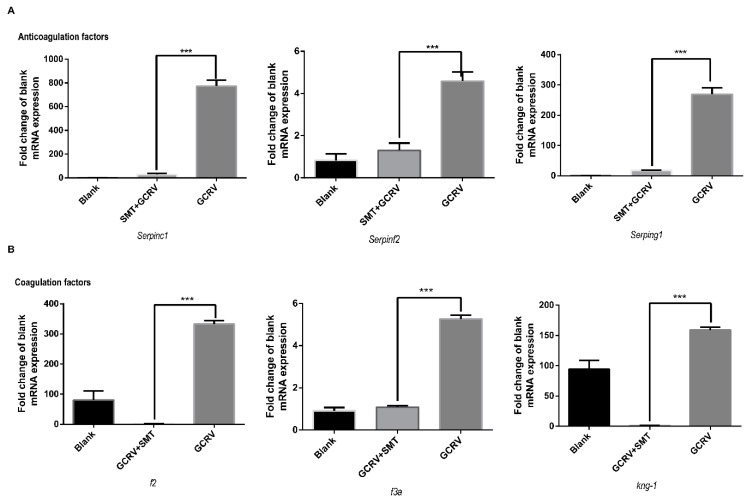
2.7. iNOS Activates Both the Coagulation and the Anticoagulation Systems
The changing expressions of coagulation factors and anticoagulation factors are important in hemorrhage. To investigate the effect of iNOS on these factors, the coagulation factors and anticoagulation factors were detected by qRT-PCR. The anticoagulation factors serpinc1, serpinf2, and serping1 were significantly up-regulated in the GCRV group (Figure 7A), while the anticoagulation factors serpinb1, serpind1, and serpinf1 had no significant change (Supplementary Figure S2A). The coagulation factors f2, f3a, and kng-1, were significantly up-regulated in the GCRV group (Figure 7B), while the coagulation factors f10 and f3b showed no significant change (Supplementary Figure S2B).
Figure 7.
Some coagulation factors and anticoagulation factors were inhibited when suppressing the function of iNOS in muscle. (A) Anticoagulation factors serpinc1, serpinf2, and serping1 are significantly up-regulated in the GCRV group VS. GCRV+SMT (n = 3). (B) Coagulation factors f2, f3a, and kng-1 are significantly up-regulated in the GCRV group VS. GCRV+SMT (n = 3). (*** p < 0.001).
3. Discussion
Viral hemorrhage is one of the severe pathological phenomena in GCRV infection [46]. The etiology of the GCRV-induced hemorrhage is still not clear. This study found that iNOS could lead to GCRV-induced hemorrhage. High quantities of NO generated by iNOS defend against viral infection [47]. A large quantity of NO activates caspase-3 and caspase-9 and induces cell apoptosis by releasing cytochrome C via mitochondrial apoptosis [48]. The aim of this study was to investigate the effect of iNOS on cell apoptosis and hemorrhage during GCRV infection.
Following the overexpression of iNOS in FHM cells, cell apoptosis occurred and the activities of caspase-3 and caspase-9 were significantly increased. These observations aligned with previous literature, which reported that the iNOS could generate high quantities of NO and induce cell apoptosis [30,49]. Therefore, grass carp iNOS was confirmed to have the same function as mammalian iNOS.
To investigate the inhibitor of iNOS, FHM cells were infected with GCRV, and a significant cytopathic effect and high rate of cell apoptosis were observed. When treated with SMT—a competitive inhibitor of iNOS, which has no direct effect on GCRV replication—coagulation factors and anticoagulation factors (Supplementary Figure S3) [50], the rate of cell apoptosis decreased and the cytopathic effect was attenuated. These observations demonstrated that SMT can reduce cell apoptosis by inhibiting iNOS.
Rare minnow were infected with GCRV, we observed obvious symptoms: vascular wall was broken and blood cells infiltrated into muscle tissue [51], the gloss on the body surface faded, the concentration of NO and activities of caspase-3 and caspase-9 significantly increased. Additionally, these effects were significantly attenuated by inhibition of iNOS via SMT treatment. These results indicated that iNOS reduces GCRV-induced hemorrhage. iNOS produced high quantities of NO to activate caspases and induce vascular endothelial cells apoptosis, and release blood cells out of the vessel. The vascular endothelial cells apoptosis resulted in hemorrhage development. This result is similar to the previous literature—dengue viral protease that interacts with NF-κB inhibitor α/β results in endothelial cell apoptosis and hemorrhage development [32].
Comprehensive comparative analyses of the expressions of key coagulation factors and key anticoagulation factors show that both the coagulation system and anticoagulation system are activated in GCRV infection, and the up-regulated expressions of anticoagulation factor genes were more prominent than those of coagulation factor genes. Therefore, anticoagulation may be more dominant in rare minnow during GCRV infection, which is the opposite in grass carp infected with GCRV [43]. NO also affects the coagulation disorder, it impedes the adhesion of platelets to the endothelium to block the repair of the vessel injury [23]. The high level of NO in the GCRV group also enhanced hemorrhage. The survival curve showed no significant difference between the GCRV group and GCRV+SMT group, which indicated that SMT could not be used as a protective agent to improve the survival rate of GCRV infection, and hemorrhage is not the major cause of death in GCRV infection.
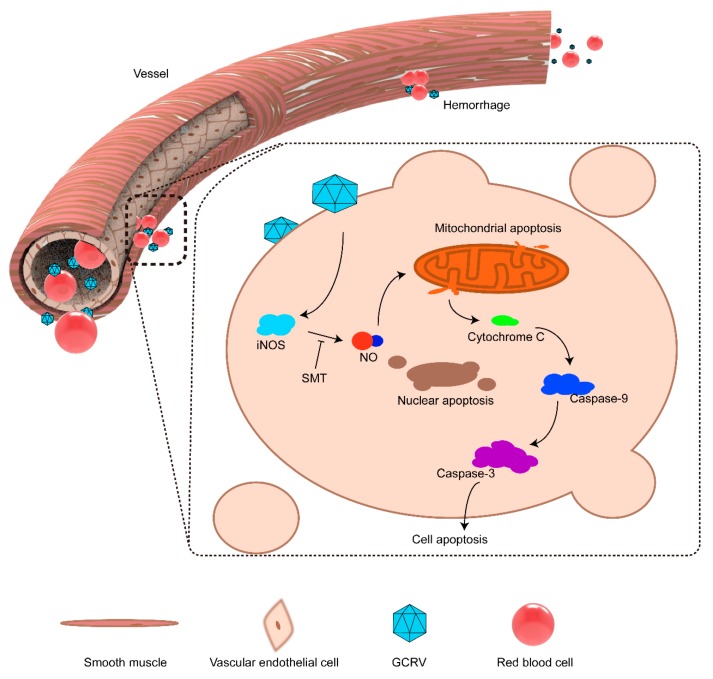
Based on previously published results and this study, we proposed a model to describe the molecular pathogenic process of GCRV-induced hemorrhage (Figure 8). GCRV infects the vascular endothelial cell and activates the expression of iNOS [15]. High quantities of NO are produced by iNOS, causing mitochondrial apoptosis and releasing cytochrome C [33]. Cytochrome C activates the caspase process and leads to vascular endothelial cell apoptosis [48]. Hemorrhage occurs following vascular endothelial cells apoptosis [32]. SMT inhibits the activity of iNOS to reduce NO [52].
Figure 8.
The proposed model for the mechanism of iNOS-induced endothelial cell apoptosis and hemorrhage. GCRV infects the vascular endothelial cell and activates the expression of iNOS. A large quantity of NO was produced by iNOS and leads mitochondrial apoptosis to release cytochrome C. The cytochrome C activates the caspase process and leads the vascular endothelial cell apoptosis. The hemorrhage happened when vascular endothelial cells apoptosis. SMT can inhibit the activity of iNOS to produce NO.
4. Materials and Methods
4.1. Ethics Statement
The protocol of animal experiments was approved by the Animal Management and Ethics Committee, Huazhong Agricultural University. The approval number is HZAUFI-2019-005 (Approval date: 23 April 2019). This experiment was conscientiously abided by the ethical principles of animal welfare. All surgery was performed under MS-222 anesthesia to minimize suffering.
4.2. Animal Experiments
A total of 85 rare minnow—weight 0.928 ± 0.107 g, length 4.12 ± 0.218 cm—were bought from the Institute of Hydrobiology, Chinese Academy of Sciences. They were cultured in our laboratory with aerated freshwater at 28 °C and fed with red worm twice a day. A total of 25 rare minnow were used in the pre-test to determine the concentrations of S-methylisothiourea sulfate (SMT, a selective iNOS inhibitor, No. S0008, Beyotime Biotechnology, Shanghai, China) and GCRV in vivo by intraperitoneal injection [52]. A total of 60 rare minnow were randomly divided into 3 groups: Blank group, GCRV group (GCRV infection, GCRV 50 μL), and GCRV+SMT group (GCRV infection and SMT treatment, GCRV 50 μL, SMT 100 mg/kg). The GCRV titer is 2.56 × 10 RNA copies/µL. All samples were collected under MS-222 anesthesia when hemorrhage developed.
4.3. Cloning of iNOS, Plasmids Construction, Cell Culture, and Transfection
The full-length cDNA sequence of grass carp iNOS has been reported (GenBank accession number HQ589354). The full-length coding sequence of iNOS was amplified using PrimeSTAR® Max DNA polymerase (Takara, Kusatsu, Japan) with specific primers (Table 1), which is 3243 bp. The plasmid pCMV-iNOS-3×Flag-CMV-eGFP (pCICE, Supplementary Figure S1) was constructed using a One-Step Cloning Kit (ClonExpress® MultiS One Step Cloning Kit, Vazyme Biotech Co., Ltd., Nanjing, China) by introducing the iNOS coding sequence into the pCMV-3×Flag-CMV-eGFP (pCCE).
Table 1.
The primers for amplifying iNOS.
| Primer Name | Sequence (5′ → 3′) |
|---|---|
| NOS1F | CGTCAGATCGGAATTCGGTACCAATGGGGAACCAGGCCACTAAAGACA |
| NOS1R | GCTGCAAACTTATCGTCCACTGCGTGAG |
| NOS2F | CGCAGTGGACGATAAGTTTGCAGCACT |
| NOS2R | GTCAGCCCGGGATCCTCTAGAGGATCCGAAGATGTCCTCATGGTACCGC |
Fathead minnow (FHM) cells, epithelial cells from fathead minnow and with an ATCC number of CCL-42 [53], were grown in M199 (Gibco, Carlsbad, CA, USA) supplemented with 10% fetal bovine serum (Gibco, Carlsbad, CA, USA). The cells were incubated at 28 °C in a 5% CO2 humidified atmosphere. FHM cells were transfected with 800 ng pCICE in a six-well plate (Thermo Scientific, Waltham, MA, USA). The control group was transfected with 800 ng pCCE. All of the vectors were transfected into FHM cells by using the FuGENE®6 Transfection Reagent (Promega, Madison, WI, USA) according to the manufacturer’s instructions of reagent.
4.4. GCRV Infection and SMT Inhibitor
FHM cells were plated in a six-well plate. The cells were infected with GCRV and treated with five different concentrations of SMT (0, 1 μM, 10 μM, 0.1 mM and 1 mM). These cells were imaged by the light microscope 48 h post-treatment and collected for analyzing the apoptosis rate by using flow cytometry after staining with Annexin V-FITC according to the product information of Annexin V-FITC Apoptosis Detection Kit (eBioscience, BMS500FI/20, Thermo Scientific, Waltham, MA, USA).
4.5. Fluorescence Microscopy
FHM cells were plated in glass-bottomed dishes (Nest, Wuxi, Jiangsu, China) and transfected with 800 ng pCICE in a six-well plate. The control group was transfected with 800 ng pCCE. The samples were collected at 12, 24, 48, and 72 h post-transfection. All of the cells on microscopic glass-bottomed dishes were fixed using 4% formaldehyde for 15 min at 37 °C, followed by incubation in 1 μg/mL Hoechst 33342 (Gibco, Carlsbad, CA, USA) for 15 min in the dark to stain the nuclei. Then, the stained cells were rinsed with phosphate-buffered saline (PBS). Images were taken with the Live Cell Imaging System (PerkinElmer, Waltham, MA, USA).
4.6. Protein Extraction and Western Blot
Rare minnow muscle tissue was homogenized in PBS with 1 mM phenylmethylsulfonyl fluoride (PMSF, Biosharp, Anhui, China). The homogenates were centrifuged at 13,800 g for 15 min at 4 °C. The supernatants were collected for Western blot. As for cell samples, the cells from the six-well plate at 48 h post-transfection were centrifuged at 1000 g for 5 min. The cells were resuspended in 100 μL PBS with 1 mM PMSF. The samples were frozen (−70 °C for 15 min) and thawed (room temperature) 3 times, and centrifuged at 3000 g for 30 min at 4 °C. The supernatants were collected for Western blot.
The supernatant liquid was mixed with 20 μL 5× SDS loading buffer and denatured at 100 °C for 10 min. The mixture was separated by 10% SDS-PAGE and transferred to nitrocellulose membranes (MilliporeSigma, Burlington, MA, USA). Membranes were put in fresh 5% skim milk dissolved in Tris-Buffered Saline Tween-20 (TBST) buffer for 2 h at 4 °C. They were then incubated with primary antibodies for 2 h at room temperature: anti-Flag (monoclonal, 1:5000, Abclonal Technology, Wuhan, China), anti-NOS2 (polyclonal, 1:2000, Abclonal Technology, Wuhan, China), and anti-β-tubulin (polyclonal, 1:5000, Abcam, Cambridge, United Kingdom), respectively. The membranes were then washed 3 times with TBST buffer on the horizontal shaker (15 min each time) and incubated with Ab-HRP for 45 min at room temperature. The signal was obtained by using the ECL reagents (K-12045, PEPTBIO, Wuhan, China) with Amersham Imager 600 (GE, MA, USA).
4.7. Caspase Activity Assay, NO Measure, and Histopathology
The cells and muscle tissue were collected for measuring the production of NO and assaying the activities of caspase-3 and caspase-9 by using NO Content Assay Kit (No. S0021, Beyotime Biotechnology, Shanghai, China) and Caspase Activity Assay Kits (No. C1115, and No. C1157, Beyotime Biotechnology, Shanghai, China) according to the manufacturer’s instructions, respectively. The samples of muscle tissue from all groups were placed in 4% paraformaldehyde. All of the tissue sections were made and imaged by the company Pinuofei Biotechnology (Wuhan, China).
4.8. qRT-PCR Assay
The muscle tissue of rare minnow from all treatment groups was homogenized in TRIZOL (Simgen, Hangzhou, China). Total RNAs were extracted with TRIZOL reagent, and converted to cDNA using the Reverse Transcription Kit HiScript II Q RT SuperMix for qPCR (+gDNA wiper) (Vazyme Biotech Co.,Ltd, Nanjing, China). All the cDNA concentrations were adjusted to 50 ng/μL. The qRT-PCR mixture consisted of 4 μL of cDNA sample, 3.1 μL of nuclease-free water, 7.5 μL of 2× SYBR Green master mix (No. BSB25L1B, BioEasy, Hangzhou, China), and 0.2 μL of each gene-specific primer (10 mM). The PCR cycling conditions were as follows: 1 cycle of 95 °C for 30 s, 45 cycles of 95 °C for 5 s, 60 °C for 30 s, 1 cycle of 95 °C for 15 s, 60 °C for 30 s, followed by dissociation curve analysis to verify the amplification of a single product. mRNA expression levels were normalized to the expression level of β-actin, and the data were analyzed using the 2-△△CT method. The qRT-PCR primers are shown in Table 2.
Table 2.
The primers for qRT-PCR.
| Gene Name | Primer Name | Sequence (5′ → 3′) | Accession Number |
|---|---|---|---|
| Serpinb1 | Sb1F | TCTCTGATGTTCACTCTCGGTTTG | MN326820 |
| Sb1R | TCTTTGATTTTATTCTCCGTCTGC | ||
| Serpinc1 | Sc1F | TCGATAAAGGAGAAGACATCTGACC | MN326821 |
| Sc1R | GCTGGAAGGACTCATTAAAAAGTGTAG | ||
| Serpind1 | Sd1F | GCAGAACTATGACTTGATTGACCAC | MN326822 |
| Sd1R | TGATAAAGGCATGAATCCGATGT | ||
| Serpinf1 | Sf1F | CTCTCCAATACTCTCCACGCAGT | MN326823 |
| Sf1R | CGCTTCCAACCATTCAGACATAC | ||
| Serpinf2b | Sf2bF | ACCTTGATACACTCTGTGATGGGG | MN326824 |
| Sf2bR | GGAAATTATGACATTGGGCTGTT | ||
| Serping1 | Sg1F | TTCCTCTCAGACACTGTTGGTGG | MN326825 |
| Sg1R | GAAGATCAAGTTGGATTTGGGGT | ||
| iNOS | NOSF | CAGGTCTGAAAGGGAATCCTATGA | MN326826 |
| NOSR | TTGGGTTGTCCAGTCTGCCTAG | ||
| Kng-1 | Kng1F | ACCGCTCATTCATTCTTTGGC | MN380324 |
| Kng1R | CCTGGTGCAGTTGCTCTTCTC | ||
| F2 | F2F | GGACCTCAAACCCCACAAATC | MN380325 |
| F2R | CCCACGACACAATGCCAATC | ||
| F3a | F3aF | CAGGCCTACCTGCCCTTCC | MN380326 |
| F3aR | TTTTTCGCTCGCTTTCTTCG | ||
| F3b | F3bF | TTTTCGGTGCTTTTTCTCGC | MN380327 |
| F3bR | TCTGTTTGTCCCTACCAACTCTTG | ||
| F10 | F10F | AGTAAAGTTGCCACACAGGGAGC | MN380328 |
| F10R | CAGTTGGGTAGTTGTAAGAATGTAAAGG | ||
| β-actin | ACTF | AATTGTCCGTGACATCAAAGAGAA | MN562268 |
| ACTR | GATACCGCAAGATTCCATACCC | ||
| VP4 | VP4F | CGAAAACCTACCAGTGGATAATG | ADC81088 |
| VP4R | CCAGCTAATACGCCAACGAC |
4.9. Statistical Analysis
Statistical analyses and presentation graphics were carried out using the GraphPad Prism 6.0 software (GraphPad Software, San Diego, CA, USA). Results were presented as mean ± SD for at least three independent experiments. All data were subjected to one-way ANOVA, followed by an unpaired, two-tailed t test. A p value < 0.05 was considered to be a statistically significant difference (* p < 0.05, ** p < 0.01, *** p < 0.001).
5. Conclusions
In conclusion, the hemorrhage and vascular wall injury were observed after GCRV infection, and these pathological phenomena were both attenuated when the function of iNOS was inhibited. Therefore, iNOS-mediated vascular endothelial cell apoptosis plays a critical role in GCRV-induced hemorrhage. This study is the first to explain the relationship between iNOS-induced cell apoptosis and GCRV-induced hemorrhage; it provides a novel insight and lays a foundation for further mechanistic research of virus-induced hemorrhage.
Acknowledgments
We thank Youliang Rao, Hang Su, Jianfei Ji, Zhiwei Liao, Changsong Wu, and Rui Jiang for helpful discussions and assistance in experiments.
Abbreviations
| bNOS | Bacterial NOS |
| eNOS | Endothelial NOS |
| FHM | Fathead Minnow |
| GCRV | Grass Carp Reovirus |
| iNOS | Inducible Nitric Oxide Synthase |
| kng-1 | Kininogen-1 |
| nNOS | Neuronal NOS |
| NO | Nitric Oxide |
| NOSs | Nitric Oxide Synthases |
| PBS | Phosphate Buffer Saline |
| pCCE | pCMV-3×Flag-CMV-eGFP |
| CICE | pCMV-iNOS-3×Flag-CMV-eGFP |
| PMSF | Phenylmethylsulfonyl fluoride |
| qRT-PCR | Quantitative real-time RT-PCR |
| serpin | Serine protease inhibitor |
| SMT | S-methylisothiourea sulfate |
| TBST | Tris-buffered saline tween-20 |
Supplementary Materials
Supplementary materials can be found at https://www.mdpi.com/1422-0067/20/24/6335/s1.
Author Contributions
Conceptualization, J.S.; Methodology, B.L. and J.S.; Project administration, J.S.; Supervision, J.S.; Validation, B.L.; Writing—original draft, B.L.; Writing—review & editing, J.S.
Funding
This work was funded by the National Key Research and Development Program of China (2018YFD0900504) and National Natural Science Foundation of China (31930114).
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, and in the decision to publish the results.
References
- 1.Gavito-Higuera J., Mullins C.B., Ramos-Duran L., Chacon C.I.O., Hakim N., Palacios E. Fungal infections of the central nervous system: A pictorial review. J. Clin. Imaging Sci. 2016;6:24. doi: 10.4103/2156-7514.184244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Novotny W.E., Dixit A. Pulmonary hemorrhage in an infant following 2 weeks of fungal exposure. Arch. Pediatr. Adolesc. Med. 2000;154:271. doi: 10.1001/archpedi.154.3.271. [DOI] [PubMed] [Google Scholar]
- 3.Zhang Y.M., Zhou Z.M., Pan X.Y. Study on the pathogen of red-skin disease of Aerossocheilus fasciatus. J. Shanghai Ocean Univ. 2010;19:631–634. (In Chinese with English abstract) [Google Scholar]
- 4.Tekedar H.C., Karsi A., Akgul A., Kalindamar S., Waldbieser G.C., Sonstegard T., Schroeder S.G., Lawrence M.L. Complete genome sequence of fish pathogen Aeromonas hydrophila AL06-06. Genome Announc. 2015;3:549–556. doi: 10.1128/genomeA.00368-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cosgriff T.M., Lewis R.M. Mechanisms of disease in hemorrhagic fever with renal syndrome. Kidney Int. Suppl. 1991;35:S72. [PubMed] [Google Scholar]
- 6.Shcheblyakov D., Esmagambetov I., Simakin P., Kostina L., Kozlov A., Tsibezov V., Grebennikova T., Chifanov D., Rumyantseva I., Boyarskaya N., et al. Development and characterization of two GP-specific monoclonal antibodies, which synergistically protect non-human primates against Ebola lethal infection. Antivir. Res. 2019:104617. doi: 10.1016/j.antiviral.2019.104617. [DOI] [PubMed] [Google Scholar]
- 7.Du F., Su J., Huang R., Liao L., Zhu Z., Wang Y. Cloning and preliminary functional studies of the JAM-A gene in grass carp (Ctenopharyngodon idellus) Fish Shellfish Immunol. 2013;34:1476–1484. doi: 10.1016/j.fsi.2013.03.352. [DOI] [PubMed] [Google Scholar]
- 8.Jiang Y.L., Liopo G. Hemorrhagic disease of grass carp: Status of outbreaks, diagnosis, surveillance, and research. Isr. J. Aquac.-Bamidgeh. 2009;61:188–197. [Google Scholar]
- 9.Rao Y., Su J. Insights into the antiviral immunity against grass carp (Ctenopharyngodon idella) reovirus (GCRV) in grass carp. J. Immunol. Res. 2015;2015:670437. doi: 10.1155/2015/670437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mao S., Shao J., Hang Q., Zhang N. On pathogen of hemorrhage of grass carp (Ctenopharyngodon idellus C. ET V.) J. Fish. China. 1989;13:1–4. (In Chinese with English abstract) [Google Scholar]
- 11.Yan C., Xiao J., Li J., Chen H., Liu J., Wang C., Feng C., Feng H. TBK1 of black carp plays an important role in host innate immune response against SVCV and GCRV. Fish Shellfish Immunol. 2017;69:108–118. doi: 10.1016/j.fsi.2017.08.016. [DOI] [PubMed] [Google Scholar]
- 12.Wang T., Liu P., Chen H., Liu H., Yi Y., Guo W. Preliminary study on the susceptibility of Gobiocypris rarus to hemorrhagic virus of grass carp (GCHV) Acta Hydrobiol. Sin. 1994;18:144–149. (In Chinese with English abstract) [Google Scholar]
- 13.Li X., Zeng W.W., Wang Q., Wang Y.Y., Li Y.Y., Shi C.B., Wu S.Q. Progress on grass carp reovirus. Prog. Veter. Med. 2016;37:94–101. (In Chinese with English abstract) [Google Scholar]
- 14.Wang Q., Zeng W., Liu C., Zhang C., Wang Y., Shi C., Wu S. Complete genome sequence of a reovirus isolated from grass carp, indicating different genotypes of GCRV in China. J. Virol. 2012;86:12466. doi: 10.1128/JVI.02333-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wan Q., Su J. Transcriptome analysis provides insights into the regulatory function of alternative splicing in antiviral immunity in grass carp (Ctenopharyngodon idella) Sci. Rep. 2015;5:12946. doi: 10.1038/srep12946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wan Q., Liao Z., Rao Y., Yang C., Ji J., Chen X., Su J. Transferrin Receptor 1-Associated Iron Accumulation and Oxidative Stress Provides a Way for Grass Carp to Fight against Reovirus Infection. Int. J. Mol. Sci. 2019;20:5857. doi: 10.3390/ijms20235857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Förstermann U., Sessa W.C. Nitric oxide synthases: Regulation and function. Eur. Heart J. 2011;33:829–837. doi: 10.1093/eurheartj/ehr304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Oswald I.P., Eltoum I., Wynn T.A., Schwartz B., Caspar P., Paulin D., Sher A., James S.L. Endothelial cells are activated by cytokine treatment to kill an intravascular parasite, Schistosoma mansoni, through the production of nitric oxide. Proc. Natl. Acad. Sci. USA. 1994;91:999–1003. doi: 10.1073/pnas.91.3.999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Xie Q.-w., Cho H.J., Calaycay J., Mumford R.A., Swiderek K.M., Lee T.D., Ding A., Troso T., Nathan C. Cloning and characterization of inducible nitric oxide synthase from mouse macrophages. Science. 1992;256:225–228. doi: 10.1126/science.1373522. [DOI] [PubMed] [Google Scholar]
- 20.Gusarov I., Nudler E. NO-mediated cytoprotection: Instant adaptation to oxidative stress in bacteria. Proc. Natl. Acad. Sci. USA. 2005;102:13855–13860. doi: 10.1073/pnas.0504307102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nathan C.F., Hibbs J.B. Role of nitric oxide synthesis in macrophage antimicrobial activity. Curr. Opin. Immunol. 1991;3:65–70. doi: 10.1016/0952-7915(91)90079-G. [DOI] [PubMed] [Google Scholar]
- 22.Stuehr D.J., Griffith O.W. Mammalian nitric oxide synthases. Biochim. Biophys. Acta Bioenerg. 1999;1411:217–230. doi: 10.1016/S0005-2728(99)00016-X. [DOI] [PubMed] [Google Scholar]
- 23.Bogdan C. Nitric oxide and the immune response. Nat. Immunol. 2001;2:907. doi: 10.1038/ni1001-907. [DOI] [PubMed] [Google Scholar]
- 24.Cau S.B.D.A., Carneiro F.S., Tostes R. Differential modulation of nitric oxide synthases in aging: Therapeutic opportunities. Front. Physiol. 2012;3:218. doi: 10.3389/fphys.2012.00218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Green S.J., Scheller L.F., Marletta M.A., Seguin M.C., Klotz F.W., Slayter M., Nelson B.J., Nacy C.A. Nitric oxide: Cytokine-regulation of nitric oxide in host resistance to intracellular pathogens. Immunol. Lett. 1994;43:87. doi: 10.1016/0165-2478(94)00158-8. [DOI] [PubMed] [Google Scholar]
- 26.Ahmad A., Dempsey S.K., Daneva Z., Azam M., Li N., Li P.-L., Ritter J.K. Role of nitric oxide in the cardiovascular and renal systems. Int. J. Mol. Sci. 2018;19:2605. doi: 10.3390/ijms19092605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Beckman J.S., Koppenol W.H. Nitric oxide, superoxide, and peroxynitrite: The good, the bad, and ugly. Am. J. Physiol.-Cell Physiol. 1996;271:1424–1437. doi: 10.1152/ajpcell.1996.271.5.C1424. [DOI] [PubMed] [Google Scholar]
- 28.Marla S.S., Lee J., Groves J.T. Peroxynitrite rapidly permeates phospholipid membranes. Proc. Natl. Acad. Sci. USA. 1997;94:14243–14248. doi: 10.1073/pnas.94.26.14243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zheng L., Ding J., Wang J., Zhou C., Zhang W. Effects and mechanism of action of inducible nitric oxide synthase on apoptosis in a rat model of cerebral ischemia-reperfusion injury. Anat. Rec. 2016;299:246–255. doi: 10.1002/ar.23295. [DOI] [PubMed] [Google Scholar]
- 30.Murphy M.P. Nitric oxide and cell death. Biochim. Biophys. Acta Bioenerg. 1999;1411:401–414. doi: 10.1016/S0005-2728(99)00029-8. [DOI] [PubMed] [Google Scholar]
- 31.Elmore S. Apoptosis: A review of programmed cell death. Toxicol. Pathol. 2007;35:495–516. doi: 10.1080/01926230701320337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lin J.C., Lin S.C., Chen W.Y., Yen Y.T., Lai C.W., Tao M.H., Lin Y.L., Miaw S.C., Wu-Hsieh B.A. Dengue viral protease interaction with NF-kappaB inhibitor alpha/beta results in endothelial cell apoptosis and hemorrhage development. J. Immunol. 2014;193:1258–1267. doi: 10.4049/jimmunol.1302675. [DOI] [PubMed] [Google Scholar]
- 33.Jiang X., Wang X. Cytochrome C-mediated apoptosis. Annu. Rev. Biochem. 2004;73:87–106. doi: 10.1146/annurev.biochem.73.011303.073706. [DOI] [PubMed] [Google Scholar]
- 34.Miest J.J., Adamek M., Pionnier N., Harris S., Matras M., Rakus K.Ł., Irnazarow I., Steinhagen D., Hoole D. Differential effects of alloherpesvirus CyHV-3 and rhabdovirus SVCV on apoptosis in fish cells. Vet. Microbiol. 2015;176:19–31. doi: 10.1016/j.vetmic.2014.12.012. [DOI] [PubMed] [Google Scholar]
- 35.Sanjeev P., Richa S., Anshu P. Overview of the coagulation system. Indian J. Anaesth. 2014;58:515–523. doi: 10.4103/0019-5049.144643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Katherine H., Michael L., Henderson S.O. Anticoagulation drug therapy: A review. Western J. Emerg. Med. 2015;16:11. doi: 10.5811/westjem.2014.12.22933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Furie B., Furie B.C. Thrombus formation in vivo. J. Clin. Investig. 2005;115:3355. doi: 10.1172/JCI26987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Long A.T., Kenne E., Jung R., Fuchs T.A., Renné T. Contact system revisited: An interface between inflammation, coagulation, and innate immunity. J. Thromb. Haemost. 2016;14:427–437. doi: 10.1111/jth.13235. [DOI] [PubMed] [Google Scholar]
- 39.Di N.M., Middeldorp S., Büller H.R. Direct thrombin inhibitors. Thromb. Res. 2005;353:1028. doi: 10.1056/NEJMra044440. [DOI] [PubMed] [Google Scholar]
- 40.Triplett D.A. Coagulation and bleeding disorders: Review and update. Clin. Chem. 2000;46:1260. [PubMed] [Google Scholar]
- 41.Sergei M., Wan-Ming Z., Komar A.A., Schmaier A.H., Ellen B., Yihua Z., Xincheng L., Takayuki I., Castellino F.J., Guangbin L. Deletion of murine kininogen gene 1 (mKng1) causes loss of plasma kininogen and delays thrombosis. Blood. 2008;111:1274–1281. doi: 10.1182/blood-2007-06-092338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Van Steijn J.H., Van Tol K.M., Van Essen L.H., Gans R.O. Disseminated intravascular coagulation as an unusual presentation of an Epstein-Barr virus infection. Neth. J. Med. 2000;57:169–171. doi: 10.1016/S0300-2977(00)00047-4. [DOI] [PubMed] [Google Scholar]
- 43.Chen L., Huang R., Zhu D., Wang Y., Mehjabin R., Li Y., Liao L., He L., Zhu Z., Wang Y. Cloning of six serpin genes and their responses to GCRV infection in grass carp (Ctenopharyngodon idella) Fish Shellfish Immunol. 2019;86:93–100. doi: 10.1016/j.fsi.2018.11.008. [DOI] [PubMed] [Google Scholar]
- 44.Van R.J., Stangier J., Haertter SLiesenfeld K.H., Wienen W., Feuring M., Clemens A. Dabigatran etexilate--a novel, reversible, oral direct thrombin inhibitor: Interpretation of coagulation assays and reversal of anticoagulant activity. Thromb. Haemost. 2010;103:1116–1127. doi: 10.1160/TH09-11-0758. [DOI] [PubMed] [Google Scholar]
- 45.He L., Zhang A., Pei Y., Chu P., Li Y., Huang R., Liao L., Zhu Z., Wang Y. Differences in responses of grass carp to different types of grass carp reovirus (GCRV) and the mechanism of hemorrhage revealed by transcriptome sequencing. BMC Genom. 2017;18:452. doi: 10.1186/s12864-017-3824-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Su H., Su J. Cyprinid viral diseases and vaccine development. Fish Shellfish Immunol. 2018;83:84–95. doi: 10.1016/j.fsi.2018.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Croen K.D. Evidence for antiviral effect of nitric oxide. Inhibition of herpes simplex virus type 1 replication. J. Clin. Investig. 1993;91:2446–2452. doi: 10.1172/JCI116479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kluck R.M., Bossy-Wetzel E., Green D.R., Newmeyer D.D. The release of cytochrome c from mitochondria: A primary site for bcl-2 regulation of apoptosis. Science. 1997;275:1132–1136. doi: 10.1126/science.275.5303.1132. [DOI] [PubMed] [Google Scholar]
- 49.Satake K., Matsuyama Y., Kamiya M., Kawakami H., Iwata H., Adachi K., Kiuchi K. Nitric oxide via macrophage iNOS induces apoptosis following traumatic spinal cord injury. Mol. Brain Res. 2000;85:114–122. doi: 10.1016/S0169-328X(00)00253-9. [DOI] [PubMed] [Google Scholar]
- 50.Szabó C., Southan G.J., Thiemermann C. Beneficial effects and improved survival in rodent models of septic shock with S-methylisothiourea sulfate, a potent and selective inhibitor of inducible nitric oxide synthase. Proc. Natl. Acad. Sci. USA. 1994;91:12472–12476. doi: 10.1073/pnas.91.26.12472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zheng D., Huang Q., Cai W., Lu H. Histopathological studies on the hemorrage disease of grass carp. J. Fish. China. 1986;10:151–159. [Google Scholar]
- 52.Oztas Y., Uysal B., Kaldirim U., Poyrazoglu Y., Yasar M., Cayci T., Cekli Y., Sadir S., Ozler M., Topal T. Inhibition of iNOS reduces the therapeutic effects of ozone in acute necrotizing pancreatitis: An in vivo animal study. Scand. J. Clin. Lab. Investig. 2011;71:370–377. doi: 10.3109/00365513.2011.572183. [DOI] [PubMed] [Google Scholar]
- 53.Gravell M., Malsberger R. A permanent cell line from the fathead minnow (Pimephales promelas) Ann. N. Y. Acad. Sci. 1965;126:555–565. doi: 10.1111/j.1749-6632.1965.tb14302.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.