Abstract
Background/Aim:
Cecal intubation during colonoscopy is prone to be prolonged in women, which may be related to frequent exposure to pelvic/abdominal surgery. We evaluated the association between Cecal Intubation Time (CIT) and prior episodes of pelvic/abdominal surgery in women.
Patients and Methods:
A cross-sectional study was conducted on screening participants who underwent colonoscopy. Multivariate regression with parameter estimates (β) was performed to determine the factors affecting CIT, including age, body mass index (BMI), bowel preparation, sedation, diverticulosis, experience of colonoscopists, and a surgical history. Also, subgroup analyses according to type of surgery were performed.
Results:
A total of 835 women were enrolled. The mean CIT was 5.82 ± 3.40 min. 323 females (38.7%) had episodes of surgery. The CIT was prolonged in cases performed by non-experienced trainees (β = 3.61, P< 0.001) and with a history of gynecological surgery (β = 0.97, P = 0.001). In the subgroup of non-experienced trainees, lower BMI, poor preparation, and a history of cesarean section significantly prolonged the CIT. Also, the risk for difficult colonoscopy (CIT ≥ 15 min) was increased with a history of cesarean section (odds ratio = 4.43, P= 0.024).
Conclusion:
A prior episode of gynecological surgery prolonged CIT. Also, cesarean section history was associated with difficult colonoscopy in the examination by non-experienced trainees.
Keywords: Cecal intubation time, cesarean section, colonoscopy, gynecological surgery, women
INTRODUCTION
As the incidence of colorectal cancer has continued to rise in Asia, including South Korea,[1] there has been an increased interest in screening colonoscopy – which allows immediate diagnosis for cancer as well as treatment of adenoma. As colonoscopy is performed more actively, naturally, the need for qualitative examination also increases. The cecal intubation rate is one of the quality indicators for colonoscopy along with the degree of bowel preparation and the adenoma detection rate.[2,3] Cecal intubation rate >95% is usually required in qualified screening colonoscopy, which can be reached usually with improvement in endoscopic equipment and techniques.[3] In this situation, efforts are being made to shorten Cecal Intubation Time (CIT) beyond successful insertion. With shortened CIT, patient satisfaction can be improved and the labor of colonoscopists be reduced as well, in addition to the effective operation of endoscopy room. Failed cecal intubation or prolonged CIT is reportedly related with old age, female gender, low body mass index (BMI), a small waist circumference, poor bowel preparation, and lack of colonoscopists' expertise.[4,5,6,7] Besides, there were studies which showed an association between prolonged CITs or difficult colonoscopic examinations with prior episodes of pelvic or abdominal surgery, which induce bowel adhesion frequently,[5,8,9,10] although some studies reported controversial results.[4,7,11] Since the degree and location of post-operative adhesion may vary depending on the type of surgery, it seems unreasonable to regard surgical history per se as a factor affecting prolonged CIT.
The female gender is considered as a risk factor for prolonged CIT.[12] Colonoscopy can be technically more challenging for females than males due to reasons such as higher sensitivity to pain, more frequent bowel angulation and anthropometric factor related to central obesity. In addition, females are prone to have more experiences with pelvic or abdominal surgery.[8] Representatively, the rate of cesarean delivery has increased remarkably.[13] The aim of this study was to evaluate the association between CIT and prior episodes of pelvic or abdominal surgery, according to the type of surgery, in women.
PATIENTS AND METHODS
Study design and population
This cross-sectional study was conducted on consecutive participants in a voluntary health screening program of Dongguk University Ilsan Hospital, between January 2017 and May 2018. Among the women who underwent colonoscopy, the following were excluded: insufficient baseline information, 80 years or older, non-Koreans, previous history of colonic resection, incomplete study due to inadequate preparation or other clinical conditions such as excessive pain or paradoxical reaction to midazolam, and unconfirmed CIT. Information regarding surgical history of pelvis or abdomen was obtained via established questionnaires. The surgical history was classified as gynecological surgery, cesarean section, appendectomy, and other abdominal operation. Gynecological surgery included hysterectomy, operation of ovary or fallopian tubes, and uterine myomectomy. Operations for liver, gallbladder, pancreas, kidney, urinary bladder, spleen, stomach, and peritoneum were classified as other abdominal surgery. BMI was calculated as weight divided by height in meters squared (kg/m2), and divided into three groups (≤22.9, 23.0-24.9, ≥25.0). The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki, as reflected in a prior approval by the institution's human research committee. This study was approved by the Institutional Review Board (DUIH 2018-04-009).
Procedure
All participants were examined using a video colonoscope (Olympus CF-H260 or CF-Q260, Olympus Optical Co., Ltd, Tokyo, Japan) by six expert colonoscopists or five training fellows. All the experts had performed at least 1000 colonoscopic examinations. All of the training fellows had less than one year of endoscopic training and less than 300 colonoscopy experiences. Trainees performed colonoscopy independently or sometimes under minor supervision.
All the subjects received 2L doses of a polyethylene glycol and electrolyte solution (CoolPrep powder, Taejoon Pharm, Seoul, Korea) before the examinations for bowel cleansing. The degree of bowel preparation was assessed using Aronchick scale (excellent, good, fair, poor, or inadequate).[14] Subjects with inadequate preparation were excluded from this study due to incomplete examination. Intravenous midazolam was administered to those who sought sedative endoscopy. The dose was determined according to a unified protocol based on a subject's age and weight. Meperidine was routinely applied as analgesia. CIT was defined as the time interval from the start of an examination until the cecum was reached. The examination was defined as difficult colonoscopy when the CIT was longer than 15 minutes. Abnormal colonoscopic findings such as diverticulosis, and colorectal neoplasms were recorded.
Statistical analyses
Descriptive statistics for CIT were presented as continuous variables (mean ± standard deviation). Episodes of pelvic or abdominal surgery and other covariates were analyzed as categorical variables. Independent sample t-tests or one-way analyses of variances (ANOVA) were used for categorical variables to analyze their relationships with CIT. To determine the factors that affect CIT, multivariate regression analyses for parameter estimates, and beta-coefficients (β), was performed. The regression model included variables with P values <0.2 in the univariate analyses. Finally, the risk of difficult colonoscopy was evaluated using multivariate logistic regression for odds ratios (OR) and 95% confidence intervals (CI). All two-sided P values <0.05 were considered significant. SPSS Statistics 19.0 (IBM, Armonk, NY, USA) was used to perform the statistical analyses.
RESULTS
Population and clinical characteristics
A total of 931 from 3,219 women who participated in the screening program underwent colonoscopy during the study period. After exclusion of 96 ineligible participants, 835 women were included in the final analyses [Figure 1]. The mean age of the study population was 47.4 ± 11.2 years (range, 22-79). The mean level of CIT was 5.82 ± 3.40 min (range, 1.42-19.92). Colorectal polyps were observed in 167 (20.0%) patients and the adenoma detection rate was 13.9% (116/835). Among the participants, 803 patients (96.2%) chose sedation during colonoscopy, and the mean dose of intravenous midazolam was 5.1 ± 1.1 mg (range, 2-10 mg). The mean CIT did not differ according to sedation (P = 0.532) [Table 1].
Figure 1.
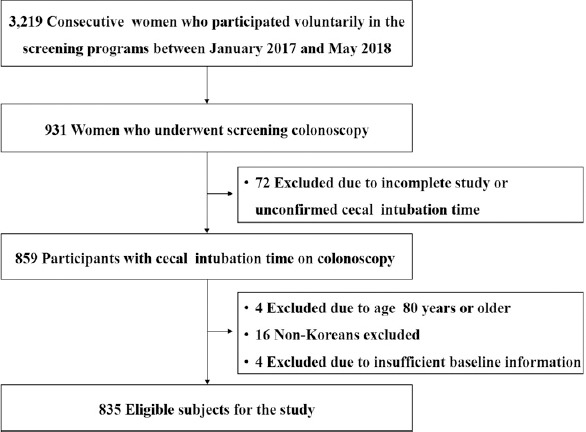
Study population.
Table 1.
Comparison of cecal intubation time based on clinical characteristics
| Variable | n (%) | CIT (Mean±SD) | P | |
|---|---|---|---|---|
| Age, year | ≤59 | 715 (85.6) | 5.78±3.37 | 0.364 |
| ≥60 | 120 (14.4) | 6.08±3.58 | ||
| BMI, kg/m2 | ≤22.9 | 496 (59.4) | 6.18±3.57 | <0.001 |
| 23.0-24.9 | 154 (18.4) | 5.67±3.33 | ||
| ≥25.0 | 185 (22.2) | 4.97±2.81 | ||
| Bowel preparation | Excellent or good | 654 (78.3) | 5.64±3.23 | 0.009 |
| Fair or poor | 181 (21.7) | 6.47±3.90 | ||
| Sedation | No | 32 (3.8) | 6.19±3.46 | 0.532 |
| Yes | 803 (96.2) | 5.81±3.40 | ||
| Colonoscopists | Experienced | 663 (79.4) | 5.05±2.79 | <0.001 |
| Non-experienced | 172 (20.6) | 8.81±3.86 | ||
| Colonic diverticulosis | No | 793 (95.0) | 5.86±3.45 | 0.021 |
| Yes | 42 (5.0) | 5.02±2.16 | ||
| Previous abdominal or pelvic surgery, any | No | 512 (61.3) | 5.70±3.27 | 0.203 |
| Yes | 323 (38.7) | 6.01±3.61 | ||
| Gynecologic surgerya | No | 722 (86.5) | 5.65±3.30 | 0.001 |
| Yes | 113 (13.5) | 6.92±3.36 | ||
| Cesarean section | No | 651 (78.0) | 5.65±3.55 | 0.451 |
| Yes | 184 (22.0) | 5.52±3.40 | ||
| Appendectomy | No | 791 (94.7) | 5.88±3.45 | 0.003 |
| Yes | 44 (5.3) | 4.76±2.25 | ||
| Other abdominal surgeryb | No | 810 (97.0) | 5.83±3.41 | 0.791 |
| Yes | 25 (3.0) | 5.64±3.35 |
BMI:Body Mass Index; CIT:Cecal Intubation Time, SD:Standard Deviation. aIncludes hysterectomy, operation of ovary or fallopian tubes, and uterine myomectomy. bIndicates abdominal surgeries except gynecological surgery, cesarean section, and appendectomy
In terms of the BMI category, the mean CIT level was shortened when the BMI increased (P < 0.001) [Table 1]. The number of examinations performed by non-experienced trainees was 172 (20.6%). The mean level of CIT was different between the experts and the training fellows (5.05 min. vs. 8.81 min., P < 0.001), and it was also different by the degree of bowel preparation (P = 0.009) and colonic diverticulosis (P = 0.021). Any Prior episode of pelvic or abdominal surgery was reported in 323 (38.7%) of the 835 participants. The most common was cesarean section (n = 184, 22.0%) followed by gynecological surgery (n = 113, 13.5%). There was no difference in the mean level of CIT by the episode of pelvic or abdominal surgery in general (P = 0.203), whereas gynecological surgery and appendectomy were associated with prolonged CIT in univariate analyses (P = 0.001 and P = 0.003, respectively).
Factors for prolonged CIT
With multivariate analyses using variables with P values <0.2 in the univariate analyses, the CIT was shortened as BMI increased [Table 2]. Compared to the examinations performed by experienced colonoscopists, those performed by the non-experienced trainees showed increased CIT (β = 3.61, P < 0.001). Gynecological surgery was a significant factor for prolonged CIT (β = 0.97, P = 0.001), but a history of appendectomy was not a significant factor. The degree of bowel preparation and diverticulosis also showed no significance in the multivariate analyses.
Table 2.
Multivariate analyses of factors affecting cecal intubation time
| Variable | Coef.(β) | SE | 95% CI | P | ||
|---|---|---|---|---|---|---|
| BMI, kg/m2 | ≤22.9 | ref | ||||
| 23.0-24.9 | −0.63 | 0.27 | −1.16, −0.09 | 0.022 | ||
| ≥25.0 | −1.24 | 0.26 | −1.75, -0.74 | <0.001 | ||
| Bowel preparation | Excellent or good | ref | ||||
| Fair or poor | 0.46 | 0.25 | −0.03, 0.95 | 0.065 | ||
| Colonoscopists | Experienced | ref | ||||
| Non-experienced | 3.61 | 0.26 | 3.10, 4.11 | <0.001 | ||
| Colonic diverticulosis | No | ref | ||||
| Yes | −0.73 | 0.47 | −1.66, 0.19 | 0.119 | ||
| Gynecologic surgerya | No | ref | ||||
| Yes | 0.97 | 0.30 | 0.37, 1.56 | 0.001 | ||
| Appendectomy | No | ref | ||||
| Yes | −0.76 | 0.46 | −1.67, 0.15 | 0.100 |
BMI:Body Mass Index; CI:Confidence Interval; SE:Standard Error.aIncludes hysterectomy, operation of ovary or fallopian tubes, and uterine myomectomy
Subgroup analyses
Table 3 represents stratified analyses by BMI and the colonoscopists' experience – along with the type of surgery performed. In the subgroups of experienced colonoscopists, gynecological surgery prolonged the CIT, while cesarean section did not affect the CIT. In the subgroup of non-experienced examiners, however, a history of cesarean section prolonged CIT (β = 1.67, P = 0.028), while gynecological surgery did not (β = 0.60, P = 0.411). Appendectomy and other abdominal surgery were not related with prolonged CIT regardless of the BMI category or the experience of colonoscopists.
Table 3.
The effect of abdominal or pelvic surgery on CIT; multivariate analyses in the subgroups
| Subgroups | Gynecological surgerya |
Cesarean section |
Appendectomy |
Other abdominal surgeryb |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | β | SE | 95% CI | n | β | SE | 95% CI | n | β | SE | 95% CI | n | β | SE | 95% CI | |
| BMI ≤22.9 | 59 | 0.79* | 0.44 | -0.06, 1.65 | 112 | −0.09 | 0.34 | −0.76, 0.57 | 31 | −0.89 | 0.58 | −2.03, 0.26 | 12 | −1.17 | 0.92 | −2.98, 0.64 |
| BMI, 23.0-24.9 | 23 | 2.32‡ | 0.64 | 1.06, 3.58 | 33 | 0.53 | 0.56 | −0.57, 1.63 | 6 | −0.94 | 1.17 | −3.24, 1.35 | 4 | −0.58 | 1.41 | −3.35, 2.19 |
| BMI ≥25.0 | 31 | 0.47 | 0.51 | -0.54, 1.47 | 39 | 0.10 | 0.46 | −0.79, 1.00 | 7 | −0.25 | 0.98 | −2.18, 1.68 | 9 | 0.87 | 0.87 | −0.84, 2.57 |
| Experienced | 79 | 1.18‡ | 0.33 | 0.54, 1.82 | 155 | −0.30 | 0.25 | −0.79, 0.19 | 40 | −0.68 | 0.45 | −1.56, 0.19 | 18 | −0.19 | 0.65 | −1.47, 1.10 |
| Non-experienced | 34 | 0.60 | 0.72 | -1.82, 2.02 | 29 | 1.67† | 0.76 | 0.18, 3.15 | 4 | −1.73 | 1.86 | −5.37, 1.91 | 7 | −0.70 | 1.42 | −3.48, 2.08 |
BMI:Body Mass Index; CI:Confidence Interval; CIT:Cecal Intubation Time; SE:Standard Error. β indicates a mean change in CIT of subjects with each surgical history compared to subjects without the surgical history in the subgroups. All regression models were adjusted by body mass index, bowel preparation, expertize of examiners, diverticulosis and each surgical history. aIncludes hysterectomy, operation of ovary or fallopian tubes and uterine myomectomy. bIndicates abdominal surgeries except gynecological surgery, cesarean section and appendectomy. *P<0.1, †P<0.05, ‡P<0.01
Factors for prolonged CIT in non-experienced examiners
Table 4 shows univariate analyses in the subgroup of non-experienced trainees. With multivariate analyses using variables with P value <0.2 in the univariate analyses, BMI, poor or fair bowel preparation, and a history of cesarean section were associated with prolonged CIT [Table 5]. When the CIT was analyzed as a categorical variable, OR of cesarean section for difficult colonoscopy was 4.43 (95% CI, 1.22 to 16.16, P = 0.024) in the subgroup of non-experienced trainees [Table 6]. Meanwhile, there was no association between difficult colonoscopy and BMI, bowel preparation, or a history of gynecological surgery.
Table 4.
Comparison of cecal intubation time in the non-experienced examiners (n=172)
| Variable | n (%) | Mean±SD | P | |
|---|---|---|---|---|
| Age, year | ≤59 | 144 (83.7) | 8.95±3.90 | 0.280 |
| ≥60 | 28 (16.3) | 8.09±3.63 | ||
| BMI, kg/m2 | ≤22.9 | 101 (58.7) | 9.43±4.16 | 0.019 |
| 23.0-24.9 | 35 (20.3) | 8.47±3.62 | ||
| ≥25.0 | 36 (20.9) | 7.39±2.72 | ||
| Bowel preparation | Excellent or good | 123 (71.5) | 8.39±3.69 | 0.023 |
| Fair or poor | 49 (28.5) | 9.86±4.11 | ||
| Sedation | No | 4 (2.3) | 7.40±0.76 | 0.018 |
| Yes | 168 (97.7) | 8.84±3.90 | ||
| Colonic diverticulosis | No | 165 (95.9) | 8.85±3.91 | 0.455 |
| Yes | 7 (4.1) | 7.74±2.56 | ||
| Previous abdominal or pelvic surgery, any | No | 105 (61.0) | 8.50±3.79 | 0.192 |
| Yes | 67 (39.0) | 9.29±3.95 | ||
| Gynecologic surgerya | No | 138 (80.2) | 8.77±3.98 | 0.807 |
| Yes | 34 (19.8) | 8.95±3.39 | ||
| Cesarean section | No | 143 (83.1) | 8.57±3.54 | 0.163 |
| Yes | 29 (16.9) | 9.98±5.07 | ||
| Appendectomy | No | 168 (97.7) | 8.85±3.90 | 0.032 |
| Yes | 4 (2.3) | 7.15±1.02 | ||
| Other abdominal surgeryb | No | 165 (95.9) | 8.86±3.89 | 0.403 |
| Yes | 7 (4.1) | 7.61±3.11 |
BMI:Body Mass Index; SD:Standard Deviation. aIncludes hysterectomy, operation of ovary or fallopian tubes, and uterine myomectomy. bIndicates abdominal surgeries except gynecological surgery, cesarean section, and appendectomy
Table 5.
Multivariate analyses of factors affecting CIT in the non-experienced examiners
| Variable | Coef. (β) | SE | 95% CI | P | |
|---|---|---|---|---|---|
| BMI, kg/m2 | ≤22.9 | ref | |||
| 23.0-24.9 | −0.81 | 0.72 | −2.22, 0.61 | 0.264 | |
| ≥25.0 | −2.04 | 0.72 | −3.45, −0.63 | 0.005 | |
| Bowel preparation | Excellent or good | ref | |||
| Fair or poor | 1.36 | 0.62 | 0.14, 2.58 | 0.029 | |
| Sedation | No | ref | |||
| Yes | 0.79 | 1.87 | −2.88, 4.45 | 0.674 | |
| Cesarean section | No | ref | |||
| Yes | 1.65 | 0.75 | 0.17, 3.13 | 0.029 | |
| Appendectomy | No | ref | |||
| Yes | −1.78 | 1.86 | −5.42, 1.86 | 0.338 |
BMI:Body Mass Index; CI:Confidence Interval; CIT:Cecal Intubation Time; SE:Standard Error
Table 6.
Odds ratios for difficult colonoscopy in the non-experienced examiners
| Variable | CIT <15 min | CIT ≥15 min | Crude OR | 95% CI | P | Adjusted OR | 95% CI | P | |
|---|---|---|---|---|---|---|---|---|---|
| Age, year | ≤59 | 133 (84.2) | 11 (78.6) | ref | ref | ||||
| ≥60 | 25 (15.8) | 3 (21.4) | 1.45 | 0.38, 5.58 | 0.588 | 2.96 | 0.66, 13.42 | 0.159 | |
| BMI, kg/m2 | ≤22.9 | 90 (57.0) | 11 (78.6) | ref | ref | ||||
| >23.0 | 68 (43.0) | 3 (21.4) | 0.36 | 0.10, 1.34 | 0.129 | 0.30 | 0.08, 1.23 | 0.095 | |
| Bowel preparation | Excellent or good | 115 (72.8) | 8 (57.1) | ref | ref | ||||
| Fair or poor | 43 (27.2) | 6 (42.9) | 2.01 | 0.66, 6.12 | 0.221 | 2.58 | 0.77, 8.59 | 0.124 | |
| Gynecologic surgerya | No | 126 (79.7) | 12 (85.7) | ref | ref | ||||
| Yes | 32 (20.3) | 2 (14.3) | 0.66 | 0.14, 3.08 | 0.593 | 0.65 | 0.13, 3.26 | 0.599 | |
| Cesarean section | No | 134 (84.8) | 9 (64.3) | ref | ref | ||||
| Yes | 24 (15.2) | 5 (35.7) | 3.10 | 0.96, 10.06 | 0.059 | 4.43 | 1.22, 16.16 | 0.024 |
BMI:Body Mass Index; CI:Confidence Interval; CIT:Cecal Intubation Time; OR:Odds Ratio. aIncludes hysterectomy, operation of ovary or fallopian tubes, and uterine myomectomy
DISCUSSION
This study confirmed that lower BMI, examinations by non-experienced examiners and a history of gynecological surgery were associated with prolonged CIT in women. This study has strengths in that it provides detailed analysis based on the type of surgical history. Interestingly, the influence of prior cesarean section on the CIT was different between experienced and non-experienced examiners. A history of cesarean section was a meaningful factor for difficult colonoscopy in non-experienced examiners.
As mentioned previously, it is generally thought that prior episodes of pelvic or abdominal surgery would prolong CIT. Pelvic or abdominal surgery include various types according to techniques, sites, and extent, which determine the degree of adhesion. For example, minor operations such as appendectomy may be less likely to cause post-operative adhesion than major operations. The impact of intra-abdominal surgeries, such as gastrectomy or hepatic lobectomy, on colonoscopy, may be different from that of intra-pelvic surgeries like hysterectomy. A recent study reported that pelvic surgery was associated with incomplete insertion of sigmoidoscopy while abdominal surgery was not.[10] After all, pelvic or abdominal surgery encompasses a variety of heterogeneous operations and needs to be classified according to specific types, so as to investigate the association with CIT.
According to our data, gynecological surgery prolonged the CIT significantly. Prolonged CIT in women compared to men is partially associated with the large intra-pelvic volume in women. Furthermore, hysterectomy may increase free space in the pelvic area, which causes more frequent sigmoid looping.[5] Hysterectomy and other gynecological operation may also cause post-operative adhesion, and this may affect the CIT as well. In addition, some patients who experienced pelvic surgery due to ovarian neoplasm might have endometriosis, which already has the potential to cause adhesion in the pelvis.[15,16]
Previous studies found no influence of cesarean section on sigmoidoscopy.[10,17] Interestingly, our subgroup analyses with non-experienced examiners revealed that cesarean section prolonged CIT and was an independent risk factor for difficult colonoscopy. The performance of cesarean section has gradually increased in the countries belonging to the Organization for Economic Cooperation and Development (OECD) and it has reached up to 36% of all deliveries in South Korea.[13] Cesarean section may cause postoperative adhesions frequently, although the extent varies.[18] Recent studies found that pelvic adhesion was developed in 46 to 65% of women who delivered by cesarean section, and the risk of adhesion formation increased with repeated cesarean section.[19,20] Additionally, in a recent cohort study, a history of cesarean section was a factor with increased risk of complications during subsequent hysterectomy, which was only attributable to the presence of adhesion.[21] Since to pass through the sigmoid colon without looping is important for successful cecal intubation, caution should be used when performing colonoscopy in females with a history of cesarean section, especially for non-experienced examiners. There were objective differences in colonoscopy technique between trainee and expert colonoscopists,[22] which may support our results. A previous study has reported that the use of ancillary techniques such as postural change, abdominal hand pressure, and water flush can minimize pain during colonoscopy.[23] Training for appropriate use of the ancillary techniques may reduce sigmoid looping and colonic distension. Understanding of loop formation and resolution through magnetic devices or physical models can also be helpful for trainees.[24,25]
Most studies have found that low BMI was an affecting factor for difficult colonoscopy, although the relationship was not stratified by gender in these studies.[5,11,12,26] Our study showed inverse relationship between BMI and CIT in women as well, which was consistent with the prior studies. There was a study which showed that BMI had a positive association with CIT for women, but had a negative association with CIT for men.[27] In this study, BMI was categorized by 25 and 30, while the categorization based on 23 and 25 was used in our study. It seems reasonable to conclude that an intermediate BMI may be more favorable for colonoscopy compared to being too thin or obese. This is supported by recent studies showing difficult colonoscopy was associated with low or high visceral adipose tissue (VAT) compared to intermediate VAT.[28,29] More difficult colonoscopy that is expected in obese patients may be related to the fact that abdominal pressure or repositioning might have less impact on such patients.
Our study has several limitations. First, we could not exclude selection bias, because this study was performed using check-up data of a single university hospital. Second, since the history of pelvic or abdominal surgery was collected via subjects' memory, recall bias was also possible. In addition, we could not evaluate the interval between the surgery and colonoscopy or whether the cesarean delivery was repeated. Third, the sample size was relatively small for analyses of the subgroups. Fourth, only female subjects were included in our study. Our results need to be verified for men in terms of age, obesity-related factors, and surgical histories. Finally, other factors such as degree of sedation, participants' anxiety or pain sensitivity, colonoscopists' skills, and colonic redundancy can influence the outcome of this study. In addition, we could not achieve a concordance among examiners for assessment of bowel preparation. However, this was unlikely to be a confounding factor since we used a verified scoring system.
CONCLUSION
Prior episodes of gynecological surgery prolonged CIT in women. Also, history of cesarean section was associated with difficult colonoscopy when performed by non-experienced trainees. This study found that cesarean section could make colonoscopy insertion difficult for non-experienced trainees. Therefore, it may be necessary to pay attention to the insertion of the distal colon such as overcoming the pelvic adhesion or minimizing sigmoid looping in women, for guiding trainees.
Financial support and sponsorship
This work was supported by the Dongguk University Research Fund of 2019.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 2.Solad Y, Wang C, Laine L, Deng Y, Schwartz H, Ciarleglio MM, et al. Influence of colonoscopy quality measures on patients' colonoscopist selection. Am J Gastroenterol. 2015;110:215–9. doi: 10.1038/ajg.2014.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rex DK, Schoenfeld PS, Cohen J, Pike IM, Adler DG, Fennerty MB, et al. Quality indicators for colonoscopy. Gastrointest Endosc. 2015;81:31–53. doi: 10.1016/j.gie.2014.07.058. [DOI] [PubMed] [Google Scholar]
- 4.Hsu CM, Lin WP, Su MY, Chiu CT, Ho YP, Chen PC. Factors that influence cecal intubation rate during colonoscopy in deeply sedated patients. J Gastroenterol Hepatol. 2012;27:76–80. doi: 10.1111/j.1440-1746.2011.06795.x. [DOI] [PubMed] [Google Scholar]
- 5.Takahashi Y, Tanaka H, Kinjo M, Sakumoto K. Prospective evaluation of factors predicting difficulty and pain during sedation-free colonoscopy. Dis Colon Rectum. 2005;48:1295–300. doi: 10.1007/s10350-004-0940-1. [DOI] [PubMed] [Google Scholar]
- 6.Cardin F, Minicuci N, Andreotti A, Pinetti E, Campigotto F, Dona BM, et al. Maximizing the general success of cecal intubation during propofol sedation in a multi-endoscopist academic centre. BMC Gastroenterol. 2010;10:123. doi: 10.1186/1471-230X-10-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liang CM, Chiu YC, Wu KL, Tam W, Tai WC, Hu ML, et al. Impact factors for difficult cecal intubation during colonoscopy. Surg Laparosc Endosc Percutan Tech. 2012;22:443–6. doi: 10.1097/SLE.0b013e3182611c69. [DOI] [PubMed] [Google Scholar]
- 8.Eloubeidi MA, Wallace MB, Desmond R, Farraye FA. Female gender and other factors predictive of a limited screening flexible sigmoidoscopy examination for colorectal cancer. Am J Gastroenterol. 2003;98:1634–9. doi: 10.1111/j.1572-0241.2003.07480.x. [DOI] [PubMed] [Google Scholar]
- 9.Chung GE, Lim SH, Yang SY, Song JH, Kang HY, Kang SJ, et al. Factors that determine prolonged cecal intubation time during colonoscopy: Impact of visceral adipose tissue. Scand J Gastroenterol. 2014;49:1261–7. doi: 10.3109/00365521.2014.950695. [DOI] [PubMed] [Google Scholar]
- 10.Wang HM, Chan HH, Wu MJ, Hsu PI, Lin CK, Yu HC, et al. Not only hysterectomy but also cesarean section can predict incomplete flexible sigmoidoscopy among patients with prior abdominal or pelvic surgery. J Chin Med Assoc. 2014;77:122–7. doi: 10.1016/j.jcma.2013.11.007. [DOI] [PubMed] [Google Scholar]
- 11.Jia H, Wang L, Luo H, Yao S, Wang X, Zhang L, et al. Difficult colonoscopy score identifies the difficult patients undergoing unsedated colonoscopy. BMC Gastroenterol. 2015;15:46. doi: 10.1186/s12876-015-0273-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bernstein C, Thorn M, Monsees K, Spell R, O'Connor JB. A prospective study of factors that determine cecal intubation time at colonoscopy. Gastrointest Endosc. 2005;61:72–5. doi: 10.1016/s0016-5107(04)02461-7. [DOI] [PubMed] [Google Scholar]
- 13.Chung SH, Seol HJ, Choi YS, Oh SY, Kim A, Bae CW. Changes in the cesarean section rate in Korea (1982-2012) and a review of the associated factors. J Korean Med Sci. 2014;29:1341–52. doi: 10.3346/jkms.2014.29.10.1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.ASGE Standars of Practice Committee. Bowel preparation before colonoscpy. Gastrointest Endosc. 2015;81:781–94. doi: 10.1016/j.gie.2014.09.048. [DOI] [PubMed] [Google Scholar]
- 15.Vercellini P, Vigano P, Somigliana E, Fedele L. Endometriosis: Pathogenesis and treatment. Nat Rev Endocrinol. 2014;10:261–75. doi: 10.1038/nrendo.2013.255. [DOI] [PubMed] [Google Scholar]
- 16.Matias-Guiu X, Stewart CJR. Endometriosis-associated ovarian neoplasia. Pathology. 2018;50:190–204. doi: 10.1016/j.pathol.2017.10.006. [DOI] [PubMed] [Google Scholar]
- 17.Ramos R, Spencer RJ, O'Brien PC, Hill JR. Effects of patient age and previous operations on completeness of sigmoidoscopy. Dis Colon Rectum. 1974;17:61–3. doi: 10.1007/BF02587539. [DOI] [PubMed] [Google Scholar]
- 18.Wang PH, Tsui KH, Yang SH. Incomplete flexible sigmoidoscopy insertion after cesarean section. J Chin Med Assoc. 2014;77:115–6. doi: 10.1016/j.jcma.2013.12.002. [DOI] [PubMed] [Google Scholar]
- 19.Lyell DJ. Adhesions and perioperative complications of repeat cesarean delivery. Am J Obstet Gynecol. 2011;205:S11–8. doi: 10.1016/j.ajog.2011.09.029. [DOI] [PubMed] [Google Scholar]
- 20.Tulandi T, Agdi M, Zarei A, Miner L, Sikirica V. Adhesion development and morbidity after repeat cesarean delivery. Am J Obstet Gynecol. 2009;201:56.e1–6. doi: 10.1016/j.ajog.2009.04.039. [DOI] [PubMed] [Google Scholar]
- 21.Hesselman S, Hogberg U, Jonsson M. Effect of remote cesarean delivery on complications during hysterectomy: A cohort study. Am J Obstet Gynecol. 2017;217:564.e1–8. doi: 10.1016/j.ajog.2017.07.021. [DOI] [PubMed] [Google Scholar]
- 22.Ende AR, De Groen P, Balmadrid BL, Hwang JH, Inadomi J, Wojtera T, et al. Objective differences in colonoscopy technique between trainee and expert endoscopists using the colonoscopy force monitor. Dig Dis Sci. 2018;63:46–52. doi: 10.1007/s10620-017-4847-9. [DOI] [PubMed] [Google Scholar]
- 23.Kravochunk S, Gao R, Church J. Differences in colonoscpy technique impact quality. Surg Endosc. 2014;28:1588–93. doi: 10.1007/s00464-013-3355-z. [DOI] [PubMed] [Google Scholar]
- 24.Yoshida N, Fernandopulle N, Inada Y, Natio Y, Itoh Y. Training methods and models for colonoscopic insertion, endoscopic mucosal resection, and endoscopic submucosal dissection. Dig Dis Sci. 2014;59:2081–90. doi: 10.1007/s10620-014-3308-y. [DOI] [PubMed] [Google Scholar]
- 25.Shah SG, Brooker JC, Williams CB, Thapar C, Saunders B. Effect of magnetic endoscopic imaging on colonoscopy performance: A randomised controlled trial. Lancet. 2000;356:1718–22. doi: 10.1016/S0140-6736(00)03205-0. [DOI] [PubMed] [Google Scholar]
- 26.Kawasato R, Hashimoto S, Shirasawa T, Goto A, Okamoto T, Nishikawa J, et al. Correlation between obesity and metabolic syndrome-related factors and cecal intubation time during colonoscopy. Clin Exp Gastroenterol. 2017;10:1–7. doi: 10.2147/CEG.S120544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jain D, Goyal A, Uribe J. Obesity and Cecal Intubation Time. Clin Endosc. 2016;49:187–90. doi: 10.5946/ce.2015.079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kashiwagi K, Inoue N, Yoshida T, Bessho R, Yoneno K, Imaeda H, et al. The impact of visceral adipose tissue as best predictor for difficult colonoscopy and the clinical utility of a long small-caliber scope as rescue. PLoS One. 2017;12:e0189817. doi: 10.1371/journal.pone.0189817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moon SY, Kim BC, Sohn DK, Han KS, Kim B, Hong CW, et al. Predictors for difficult cecal insertion in colonoscopy: The impact of obesity indices. World J Gastroenterol. 2017;23:2346–54. doi: 10.3748/wjg.v23.i13.2346. [DOI] [PMC free article] [PubMed] [Google Scholar]


