Abstract
Importance:
In the surgical community, there is concern that general surgery residents are choosing subspecialty training in large numbers because of a crisis in confidence at the end of training. Survey studies are used as evidence to support modifications in the training paradigm.
Objectives:
Confidence is an essential quality of surgeons, and recent studies have attempted to quantify and measure it in graduating general surgery residents. This study was undertaken to systematically review the quality of evidence provided, and to critically analyze the language used to describe the findings using quantitative methods..
Evidence Review:
A systematic review of the PubMed indexed literature on general surgery resident confidence was performed. A summative table of each study’s hypothesis, definition of confidence, quality using MERSQI, influence using Web of Science citations, results and conclusions was created, and qualitative coding was applied to identify emerging themes.
Findings:
Fifteen survey studies have been performed that measure confidence or readiness to practice. Although five studies have neutral or positive conclusions, most studies report low confidence in general surgery graduates. There are conflicting data about definitions of confidence. The relationships between confidence, autonomy, and competence are varied and complex. Comparisons to the past are frequent.
Conclusions and Relevance:
Confidence is difficult to define and measure. Despite limitations, survey studies are used to shape discourse and influence policies. Social and cultural factors influence self-efficacy, and focusing on operative volume and autonomy alone may not address all of the reasons that some residents express concerns about readiness to practice.
Keywords: general surgery, surgery residency, confidence, self-efficacy
General surgery residency training has undergone many changes over the past decade, in response to both external regulatory pressures, such as the 80-hour work-week and increased focus on resident supervision, and to changing patterns in the practice of general surgery itself.1,2 The increasing complexity of operative procedures, adoption of advanced minimally invasive techniques, and need for extensive knowledge of adjuvant treatments have led surgeons to become more subspecialized. Today, more than 80% of graduating general surgery residents in the United States currently choose to pursue additional training in surgical subspecialities.3 Why do so few graduates of surgical training programs go directly into general surgery practice? One often repeated explanation is that the combination of duty hour restrictions, decreased autonomy, and increasing operative complexity has led to a decrease in the confidence of graduating residents over the past 10 years.
Within the community of surgeons, there is little doubt that confidence is an essential quality. In general, we assume that confidence in one’s ability as a surgeon is something that one does not have at the start of training, but that it grows over time with experience. There is a sense, however, that residents’ confidence has deteriorated since the institution of the 80-hour work-week. This is discussed at length at national surgical meetings,4 written about in editorial articles,5 and even debated in the mainstream press and popular blogs.6,7 Whether this sense of decreased confidence corresponds with a decrease in surgical skills has been debated8–10 but is not the focus of this review. Competence and confidence, though closely related, are different. Competence refers to the mastery of the technical and cognitive skills required to be a surgeon, while confidence relates to a surgeon’s belief that he or she possesses and can execute those skills. A surgeon who has one without the other can be dangerous for patients: confidence without competence manifests as hubris, while competence without confidence results in indecision and doubt.
In an attempt to quantify and measure the confidence of general surgery residents and recent graduates, several survey studies have been conducted. The majority of these studies describe a lack of confidence of general surgery residents, finding that both fellowship directors,11 practicing surgeons,12 and residents themselves 13–19 report low confidence in performing general surgical procedures independently at the conclusion of training. Others, including the most recent and one of the largest surveys, refute this claim.20–22 Lack of confidence is being discussed as a significant problem – a crisis, even. As a surgical community, we have responded to this sense of crisis in part by proposing changes to training. One proposal that has already been implemented is the Transition to Practice (TTP) general surgery fellowship.23 This program occurs after general surgery residency, similar to a subspecialty fellowship, but the goal is not to impart new technical skills or deeper understanding of a specialty. Rather, the intention is to fill perceived gaps in training, encourage strong mentorship, and provide gradual autonomy over the course of one year following residency. Other proposals for restructuring training are being considered among leaders of surgical associations that would fundamentally alter the five-year training paradigm. Various configurations are being discussed but all would provide some type of generalized training of the fundamentals of general surgery for 3–4 years followed by more specialization and independent operating during senior residency years and fellowship.4 The discussion centers on ways of providing operative autonomy, with the supposition that providing greater autonomy will result in higher confidence. There is no empiric evidence, however, that these approaches will have the desired effect on trainee confidence.
Surgeons have a sense that confidence is very important to possess, but we have little formal language to discuss it. The social sciences have a more sophisticated understanding of what precisely what is meant when groups speak colloquially about confidence and the factors that influence it. According to the psychologist Albert Bandura, “Confidence is a non-specific term that refers to strength of belief but does not necessarily specify what the certainty is about. Confidence is a catchword rather than a construct embedded in a theoretical system.”24 When someone is asked whether or not they feel confident about something without first defining the term within a shared theoretical construct, it is difficult to interpret the response in a meaningful way.
Within social cognitive theory, the term self-efficacy most closely describes the idea surgeons seem to be attempting to capture when discussing confidence, and Bandura has described in detail the methods to define and measure it.25 Self-efficacy is situation-specific and measurable, whereas confidence is individually understood and interpreted. Social cognitive theory understands individuals’ actions and reactions are strongly influenced by the actions and behaviors of others. Self-efficacy, therefore, is a social phenomenon shaped not only by the objective acquisition of skills and technical expertise but also by the absorption of the attitudes and opinions of others. For surgery trainees, this influence of the surrounding culture has largely not been discussed. Operative autonomy is often singled out as the most important factor contributing to resident confidence, but there is little recognition of the effects of the social dynamics of surgical training. It can be difficult to appreciate the magnitude of influence of social factors, but social scientists recognize and attempt to account for their important contribution when measuring self-efficacy. Interesting observations about the culture of surgery reported by anthropologists and a variety of social scientists26–28 may help us understand that the ways we relate to one another has powerful influence on the surgeons we ultimately become.
This study is a systematic review and content analysis of the published literature that has contributed to the construction of the confidence crisis among graduating general surgery chief residents. The aim of this review is to qualitatively explore published articles that measure trainee or recent graduate confidence within a wider context, considering not only the oft-cited trifecta of duty hour restrictions, decreased autonomy, and increased case complexity, but social and political factors, as well. We closely examine the definitions of confidence provided in each article and analyze the specific survey methods. Future research priorities and areas for potential interdisciplinary collaboration are identified, and a shift in language is suggested away from the broad colloquial construct of confidence and towards self-efficacy.
Methods:
A systematic review and directed qualitative content analysis was done by the single author, delving into the construction of a crisis in resident confidence, and the discourse surrounding that narrative. Drawing heavily on literature from the social science domain on the construction of social problems29 and the social cognitive theory of self-efficacy,24 the existing body of literature in the traditional medical journals (PubMed indexed journals) that have measured surgery resident confidence and readiness for practice in North America were reviewed.
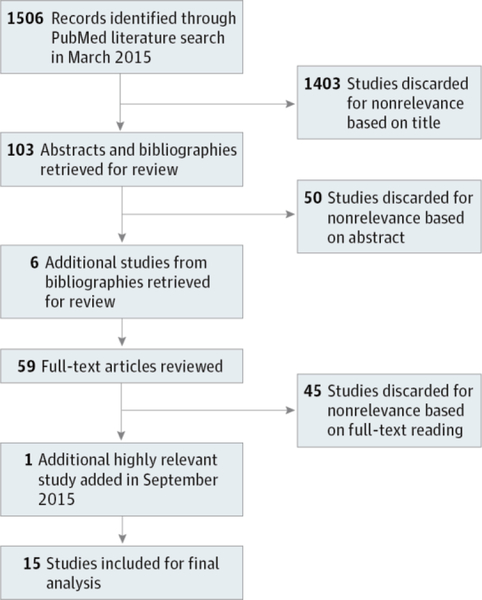
The systematic review was conducted by searching on PubMed with the search terms “confidence” AND “residency training”; “confidence” AND “surgery resident”; “confidence” AND “surgery”; “resident confidence.” No time limit was specified (Figure 1). Over 1500 titles were returned from that searching strategy; all were reviewed. Over 1400 were deemed not relevant based on title alone and of the remaining articles, abstracts and bibliographies were reviewed. From those relevant bibliographies, additional studies were identified as relevant and 59 candidate full length articles were reviewed. Fifteen studies were identified that directly surveyed surgical trainees and/or fully-trained surgeons and made claims about confidence or preparedness for practice. Initially, only articles that used the word confidence in the survey instrument were included but several studies have been cited by others as measuring confidence or something like it, which were included in this analysis. For example, the objective of the article by Foley, et al.30 was to characterize current resident perspectives on the state of residency training. Although the word confidence does not appear in the survey or article, the authors report that 86% of residents felt that they will be prepared to practice. These data were subsequently offered by Fronza, et al.31 as counter-evidence to the claim that residents have low confidence. Because subsequent authors interpreted the concept of preparedness to practice within the construct of trainee confidence, we included a few of the articles that were heavily referenced and helped frame the discourse in the literature. The earliest publication was in 2008. No studies measuring confidence in general surgery trainees were identified that were conducted before the 2003 ACGME duty hour reforms.
Figure 1.
Search Strategy and Results
A comprehensive table was created to compare each study’s hypothesis, population, definition or construct of confidence, survey design, results and conclusions. The Medical Education Research Study Quality Instrument score was calculated for each study to give a measure of the relative quality of each study. 32 The number of times each article has been cited within the Web of Science is provided to show the relative influence of each article. In addition to the summative table, qualitative methods were applied. Each article and accompanying discussions or invited editorials were read repeatedly to achieve immersion. Attention was given to language and content, passages were coded and categorized, and emerging themes were identified. Example quotes and narratives are presented that reflect some of the common themes, controversies, and shared discourses from this literature.
Results:
Qualitative results:
The first level qualitative analysis identified the common themes: authors’ definitions of confidence, relationships between confidence, competence and autonomy, and comparisons to past trainees.
One of the consistent themes is that confidence was defined in detail for the reader of the article, but when the survey instrument was available for analysis, that detailed definition was not provided to the survey taker. For example, Fonseca, et al.14 state, “It is our contention that self-reported confidence [is] a reflection of one’s ability to deal effectively with both the technically and judgment-related aspects of an operation,” and that confidence “in this context means having the skill set to deal in the OR with a variety of surgical problems in a safe and effective manner and the confidence to know when to proceed, when to change plans, and when to ask for help.” The survey, however, asked residents to “Rate your confidence in performing the following procedures…” with no further elaboration, requiring survey-takers to define confidence for themselves prior to answering. The authors17 point to an analogous methodology weakness when it came to the clinical scenarios included in the survey: “We queried residents regarding operative confidence in the control of liver and splenic injuries without describing the nature or extent of the injury...” Despite this acknowledgement, the authors did not identify the lack of a shared definition of confidence between researchers and survey-takers as a weakness of their study.
Many authors linked the extent of an individual’s confidence directly with case volume or autonomy, although there are conflicting data in the articles about case volume and no empirical evidence linking confidence and autonomy. Volume is a straightforward measure, quantified by looking at case logs. Autonomy is mentioned as a target for intervention in several articles that asked for free text, open-ended responses,11–13,19 but as a variable, autonomy is perhaps even more challenging to define and measure than confidence. Some studies22,31 found no correlation between case volume and a residents’ confidence or perception of competence. Others measured case volume and found higher volumes to be correlated with increased confidence.14,17,18,20
Other studies hint at social interactions that influence confidence, but did not attempt to measure or explain these in detail. In particular, authors provided a sense that there are important, unmeasured social factors influencing the disparate answers between men and women in several surveys.14-18,20 For instance, Fonseca, et al.14 note, “these difference in self-assessment may be because of sex differences in socialization,” and Bucholz, et al.15 suggest that “women face different challenges during general surgery than men…[that] may manifest themselves in lower confidence levels.”
Some authors argued that low confidence among surgical residents constitutes a crisis by linking confidence and competence, asserting that they measure roughly the same thing.14,17,18 Other authors cite studies that show that confidence underestimates competence,15,17,31 while another cites studies that confidence overestimates competence.19 It is clear that the two are related, but to what extent competence is reflected in responses to questions about confidence is still unclear.
There is disagreement about what should be the appropriate level of confidence. Surgical outcomes or educational research often includes a targets or benchmarks against which to compare research results. This body of literature, however, provides no sense about how many residents reporting low confidence is too many. Some authors use positive language to describe finding that 70– 94% of residents report confidence in some set of skills or preparedness to practice,19,20,30 while others use negative language in reporting numbers in an overlapping range of 60–75%.11–18 The most recent large survey by Klingensmith, et al. found that more than 90% of recent graduates do express confidence.22
The studies differed in which groups the authors thought were most knowledgeable about trainee confidence and preparedness for practice: residents themselves, their teachers, or future senior partners. They also differed in the design of survey instruments, which hinders comparisons between surveys. Most surveys used a Likert scale, although some used a 5-point scale and others used a 4-point scale with no neutral option. In the studies using a 5-point scale, the “neutral” response was mostly categorized with the “not confident” responders for analysis14–18 with the exception of one study that considered only the lowest category as “not confident”.20
Finally, language indicating a preference for the past is prevalent in this body of literature on confidence among general surgery trainees, both in the texts of the articles themselves and in the transcripts of discussion that surrounds their presentation at surgical meetings. Nostalgic preference, or the belief that past experiences were better than present counterparts is widespread33, and the emotional context of a lived experience can influence how we view the past compared to the present. Mattar, et al.11 write, “no one can deny that in the past, graduating residents were superb,” and Napolitano, et al.12 write, “surgeons commented that their training was extremely rigorous and difficult, but the hard work paid off in terms of their confidence.” Freidell, et al.20 explicitly discuss nostalgia as an underlying sentiment: “There seems to be a common thread with the surveys of the general surgery program directors, the fellowship program directors, and the ACS senior surgeons that today’s trainees are not as qualified as their predecessors were when they graduated. This might reflect the belief that all senior surgeons will have for time immemorial.”
Discussion:
More than ten years have passed since duty hours restrictions began and although most surgeons acknowledge that there are positives aspects to these mandates, there remains a sense of wistfulness for the intense camaraderie among residents during the days of every-other-night call. Surgery training was described as doing daily battle in an ongoing war, with sage and skilled surgeons emerging from the transformative experience. Residents hear this narrative throughout their training, as told by their mentors and teachers. While it is not necessarily a bad thing to talk about the positive aspects of what residency trained used to be, the reminiscing about the past often glosses over the negatives while coloring the present-day experience of being a surgical trainee. If a surgeon is guiding a resident through an operation while simultaneously lamenting that today’s training is inferior to years past, that resident may learn the judgment and skills required to perform the operation but internalize the sense that he or she is performing worse than some historic control. There are no data to support or refute this narrative and there never will be because that historic control existed in a time before the public reporting of quality measures. This may be a self-fulfilling prophecy at the level of the social interactions in training. Social scientists who have observed surgical trainees have observed that this divide between the resident of “back in the day” and the resident of today became profoundly apparent when the 80-hour workweek was introduced.27,34 When we tell residents that their training is worse today than it has ever been, are we really surprised that they provide negative answers when we ask them about their confidence? Nostalgic comparisons offer nothing of value to today’s trainees, and if we are genuinely concerned about the confidence of today’s residents, we would stop making comparisons to the past all together.
Since confidence is a general and colloquial term, and almost none of the published studies provide survey takers with a shared definition of the theoretical construct that the researchers are measuring, the reader is left to wonder what these survey studies have actually quantified. A more precise framework for study is self-efficacy, and future research in this area should use this well-established construct to develop measurable benchmarks. The lack of any data prior to 2008 makes comparisons to past training impossible. Many of the articles describe a deterioration of confidence but none are able to say precisely how confident residents were in the past because no one attempted to measure it prior to the introduction of duty hours. Even if a reader accepts that these surveys have successfully measured trainee confidence, and one accepts the unsupported claims that trainee confidence was higher in the past, it remains unclear whether confidence is lower due to unmeasured social factors, such as the self-fulfilling prophecy of nostalgic comparisons, rather than a deterioration of surgical skills and judgement acquisition.
What the authors of the articles reviewed here are doing is an exercise termed “claims-making” in social research.29,35 There has been a sense in our community that confidence is low, and these surveys were administered to provide evidence to legitimize or refute this claim. In our rigorous scientific field, data in the form of numbers are generally seen as more valid than qualitative narratives, so authors have made an attempt to quantify this feeling by designing and distributing surveys. Unfortunately, few researchers have enlisted help from social scientists with expertise in defining and measuring self-efficacy, so the survey results are generalizations at best. These data are now tabulated and quantified, with p values assigned. Based on this critical review, the lack of a shared definition for the purported measurement of confidence, the influence of individual’s social and political world view, the biased interpretive lens of nostalgia, the lack of benchmarks, and the complex relationship between confidence and competence make the results difficult to use to make strong conclusions. In essence, these authors have created legitimacy for a constructed claim.35 The confidence crisis is a potentially dangerous narrative based on low-quality evidence, one that could affect how we as a community of professionals are perceived by the public, particularly when the articles are discussed in the lay press and internet blogs. A limitation of this current paper is that it is based on one author’s review of the literature and qualitative analysis, but the authors of the most recent survey make a similar observation that the claim may have been overstated.22 Snyder, et al. offer an different interpretation of these studies and praise residents for exercising appropriate caution in today’s practice environment36, which is an alternative way to frame further discussion.
The ideas and policies that have been proposed as a way to restore confidence in our graduates have serious implications for the future of residency training. Many of the proposed changes may increase operative autonomy, but whether addressing autonomy alone will reverse the alleged trend of decreasing confidence is not known. To continue to propagate the confidence crisis narrative as a reason to change residency training is disingenuous for the reasons outlined: (1) Confidence is difficult to define and even more difficult to measure. Self-efficacy is a better construct and future research collaborations with social scientists should be forged; (2) We have no idea if confidence has declined over time. Prior to 2003, no one measured it; (3) Re-arranging training paradigms may lead to more hours in the operating room doing relevant operations and more autonomy, but does nothing to address the social and political factors that influence self-efficacy, such as perceived gender roles and professional role confidence.37 More robust social science research on the culture of surgery is needed to understand these factors so that interventions can be designed that go beyond the skills and knowledge acquisition that have made up the bulk of the conversation to date. We need to continue to work to reform residency training to provide the best possible graduates for the surgery needs of our country, but we should consider taking crisis of confidence out of the discussion. We need to focus on robust methods of measuring self-efficacy, collaborate with social scientists to more deeply understand the underlying social factors related to it, pare down our nostalgic comparisons, and concentrate educational efforts on factors such as operative autonomy that contribute to, but do not wholly explain why some residents express concerns about being prepared for independent practice.
Table 1:
Table of Studies
| Survey population/samp le size |
Hypothesis | Definition or Construct of Confidence |
Questions related to resident confidence |
Result | Citations (as of 4/29/16) |
MERSQI (0–18) |
Conclusion | |
|---|---|---|---|---|---|---|---|---|
| Foley 2008 J Surg Ed30 |
997 responses (~14% of all residents in training that year) 79% from university-based programs | Not hypothesis driven – this is the first study since duty hours regulations todirectly survey residents perceptions of the “state of general surgery training” | “Preparedness for the practice of general surgery” | 7-point Likert scale “I feel I will be prepared for the practice of general surgery at the conclusion of training.” |
85.7% agree |
11 | 7 | Residents are generally positive about the state of surgery today, feel prepared to practice general surgery (86%), “higher among PGY5” |
| “The degree of autonomy is sufficient to prepare for independent practice” | 71% agree | |||||||
| No difference in race or gender | ||||||||
| Yeo 2009 JAMA16 |
2008 ABSITE exam survey 4402 of 5345 categorical residents (82.4% response rate) | Resident attitudes, experiences and expectations may play a role in attrition | “Worry about hurting patients” “I feel my operative skill is appropriate” “Ability to perform procedures by myself before I finish training” |
“I feel like my operating skill level is appropriate” | Strongly agree or agree = 73.5% | 97 | 11 | Residents feel vulnerable at multiple levels, including lack of confidence to perform independently upon completion of training and fears of hurting patients. Responses varied significantly by sex (women are more worried in general) and by PGY year (2 and 3 are toughest) |
| “I worry I will not feel confident enough to perform procedures by myself before I finish training” | Strongly agree or agree = 27.5% | |||||||
| “I worry about hurting patients” | Strongly agree or agree = 63.6% | |||||||
| Bucholz 2011 Arch Surg15 |
2008 ABSITE exam survey 4136/5345 categorical residents (77.4% response rate) | Confidence influences career choices, attrition, and specialization | Self-confidence is an attitude that allows one to have a positive and realistic perception of oneself and one’s abilities. It encompasses enthusiasm, assertiveness, independence, trust, the ability to handle criticism, and emotional maturity. | “I feel like my operating skill level is appropriate” | Overall, 26% of those who answered disagreed, 74% agree PGY5 – 87% agree | 45 | 11 | Gender, race, marital status, children, PGY year, program location type and size all predict confidence. Confidence can be learned and it is mostly personal factors that influence it, although some program factors (fostering collegial relationships with attendings) can be targets for intervention. |
| “I worry I will not feel confident enough to perform procedures by myself before I finish training” | Overall, 27% of those who answered agreed, 73% disagree. PGY5 – 21% agree (79% disagree) | |||||||
| Examined just two questions from Yeo, et al. provided some more detail about those two questions | Authors propose that these two items measure trust in one’s skills and surgical independence | |||||||
| Fronza 2012 J Surg Ed31 |
22 of 26 graduates of 1 general surgery program were surveyed 1 year after graduation (6 year study period) at an academic training program | Today’s general surgery graduates are less capable than a generation ago, and residents themselves are worried about their competence and their ability to adopt to changes. Case volume isrelated to selfperception of competence | Confidence is the “selfperception of competence” for 67 specific operations. Competence in the ability to (1) workup, (2) independently perform operation and (3) postop care was all rolled into one question for each operation | 67 operations were included and surgeons were asked to rate on a 4 point scale: | All these new surgeons agreed that they could do all aspects of 16 of the 67 operations (27%), more than 90% agreed for 35(52%), and more than 50% agreed for 61(91%) of the operations. Highest competence in breast, endocrine, GI. Lowest competence in thoracic and vascular, but 50% believed that those were not relevant to their practice. |
16 | 8 | Case volume was not correlated with selfperception of competence. Graduates do not feel competent for those operations that require subspecialty training by the time they finish general surgery training, but generally express competence for basic core areas. Flexibility is important. |
| “I was well prepared to workup, independently perform the operation, and effectively care for the patient postoperatively” | ||||||||
| Coleman 2013 JACS13 |
Surveys (36 questions) sent to 55 programs, July – December 2011 | Confidence is down because of duty hours, decreased autonomy and increased subspecialization. Early subspecialization tracks within general surgery training will “be appealing to residents” and lead to increased confidence | One is confident if one agrees with the idea that a 5 year general surgery residency fully prepares one to practice general surgery. | 5 point Likert scale “Do you think a 5-year GS residency fully prepared you to practice GS?” |
38% responded “no” or “unsure”, although the number decreased each year: 53% of PGY1 and only 23% of PGY5 | 32 | 7 | Residents have concerns about the way they are trained, and it is possible that a change in the curriculum to early subspecialization may increase confidence. |
| 676 of 1,515 residents responded (45% response rate) | For those planning on fellowship: “Why did you pursue fellowship?” |
97% – interested in that specialty 44% did not agree that a lack of confidence in surgical skills was a reason to pursue fellowship training | ||||||
| 75% University programs, 60% men. | For those not planning on fellowship: “Why are you not doing a fellowship?” |
Already spent too much time in training (highest response category) 63% already established confidence in surgical skills was very or somewhat important factor in their decision. | ||||||
| 108 chief residents responded | ||||||||
| Gillman 2013 Am J Surg38 |
Canadian chief residents surveyed, 64 of 90 residents approached in person at a chief resident conference (71% response rate) 55% doing fellowship, 17% urban practice, 20% rural practice plans, 8% undecided | General surgery residency no longer produces graduates capable of doing rural general surgery, residents perceive a decrease in competence in the skills required to do rural surgery. | At the completion of training, a resident is confident if s/he would schedule and independently perform specific procedures that a rural surgeon might be called upon to do. Included general surgery but also other specialties. | Categorically asked whether the resident would book and independently perform a list of procedures. (23 procedures in 6 categories) Traditional general surgery procedures Advanced laparoscopic Specialized general surgery procedures Orthopedic Ob/Gyn Plastic Surgery |
>90% comfortable with basic general surgery procedures,meaning they answered “yes” that they would book and do it. Less comfortable with specialized or other procedures. Did not differ significantly for rural vs. the rest of the group | 8 | 8.5 | General surgery graduates express comfort with general surgery cases but not advanced general surgery or non-general surgery cases. Rural surgeons have unique challenges, and perhaps a rural surgery fellowship can help residents be more confident in their ability to do rural surgery. |
| Mattar 2013 Ann of Surg11 |
Program directors of fellowships, 91 of 145 (63% response rate) of programs registered with the Fellowship Council. | There are gaps in general surgery training due to outside regulatory forces. Incoming subspecialty fellows lack basic skills and won’t get as much as they could otherwise from fellowship training. | Readiness to enter fellowship as assessed by fellowship program directors | The incoming fellow: “Demonstrates ownership of patients” |
83% agree or strongly agree | 82 | 9.5 | Program directors perceive that incoming fellows have deficits and that they are not confident or prepared to enter fellowship or the surgical marketplace. |
| “Can independently perform laparoscopic cholecystectomy” | 70% agree or strongly agree | |||||||
| “Can perform 30 min of major procedure without supervision” | 34% agree or strongly agree | |||||||
| “Can take general surgery call with rare need for assistance with cases” | 52% agree or strongly agree | |||||||
| Fonseca 2014 JSR17 |
249 programs June 2012. Focus was on PGY5 residents, 1102 surveys distributed to chiefs, 653 (59% response rate) 69% male, 68% university hospital, 51% affiliated with VA | Residents lack confidence in performing open operations, and self-reported confidence is a surrogate for competence | Confidence = self-reported competence on specific operations | Rate operative confidence from 1(not confident) to 5(extremely confident). AND |
95% reported confidence for basic laparoscopy 75% for open surgical cases 57% for advanced laparoscopic | 4 | 10.5 | Resident lack confidence in performing open operations and overall report low confidence in their ability to practice independently after residency training. Increased case volume corresponds to increased confidence, and men were more confident than women. Large program size, university program, future fellowship plans and more laparoscopic cases meant lower confidence. |
| Confidence is a reflection of one’s ability to deal effectively with the technical and judgement related aspects of an operation. Confidence develops over time with deliberate practice, increased exposure and experience | “Which operations do you feel you should be confident in performing but are not” AND |
Most common answers: hepatobiliary, foregut, open vascular surgery 72% said “yes” |
||||||
| “Do you feel confident that you will graduate with the operative skills required to be able to practice independently after residency training?” | ||||||||
| Fonseca 2014 A J Surg14 |
Limited to 76 programs in Northeast, same survey as previous publication (39 questions) in 2011. Responses = 232 of 355 (65% response rate) | Same as above | Same as above | Rate operative confidence from 1(not confident) to 5(extremely confident) AND |
96% confident basic laparoscopy 84% open cases 59% advanced laparoscopic |
7 | 10.5 | Same as above except no geographic variability (survey was only administered in NorthEast) and there was lower overall confidence (52% vs 72%). Men and more volume during chief year were associated with higher confidence. |
| “Do you feel confident that you will graduate with the operative skills required to be able to practice independently after residency training?” |
52% said “yes” |
|||||||
| Friedell 2014 JACS20 |
All programs in May 2013. 297 respondents from 1097 possible (27% RR). 67% male, 76% university program | Most graduating chief residents are satisfied with their training and confident about their skills | Confidence = comfort when asked about specific operations (4 essential common, 4 essential uncommon, 4 complex), then also: “are you illprepared for any aspect of independent practice?” | Rate your “comfort” (1–4) with independently performing: | Any level of comfort (1–3) were lumped and only uncomfortable was counted: | 15 | 8 | Graduating chief residents are confident and optimistic |
| “essential common” (lap colectomy, c-scope with polypectomy, thyroidectomy, mastectomy. | 2–7% said they were “uncomfortable” performing these 4 operations | 7% of those doing fellowship chose to do fellowship because of lack of confidence | ||||||
|
“essential uncommon” (open CBD exploration, gastrectomy, distal pancreatectomy, sentinel node) |
5-14% for all but common bile duct exploration: 27% were uncomfortable | Only 25% of those going into practice interested in TTP fellowship | ||||||
|
“complex” (right hepatic lobectomy, Whipple, esophagectomy, LAR) |
LAR 7% uncomfortable Whipple 38% Hepatic lobectomy 48% Esophagectomy 60% |
|||||||
|
Open ended question asking if there were any aspects the CR felt illprepared for independent practice |
Higher number of cases, region of country and male sex all associated with higher procedural comfort. | |||||||
| Would you be comfortable being on call at level I trauma center? | 80% felt comfortable | |||||||
| Nadler 2014 JSE21 |
Graduating Canadian chief residents asked to fill out a survey in person at a conference over 2 years, 78/104 (75% response rate) in 2012 and 50/95 (53% response rate) in 2013 (overall = 64%) 19% going directly into practice (more in 2013 than in 2012), >40% women. | Little is known about technical skills of residents today – some say fine others say bad. Specific procedural competencies are not defined by the board, so it is hard to know. This was a survey measuring perceived competence, strengths, and weaknesses of operative trainees in Canada | Can independently complete from a list of essential and complex operations – all general surgery | Asked about specific operation – 3 answer choices: “Require assistance for most or part of the operation.” “Require minimal assistance for routine situation.” “Require no assistance in most or all of the operation” |
Most resident identified lap adrenal, neck dissection, thyroidectomy, lap splenectomy, lap LAR, groin dissection in which they require assistance. Most required no or minimal assistance for open and lap right colon, cricothyroidotomy, component separation, open spleen, sentinel node, mastectomy, open LAR. | 1 | 7.5 | Canadian resident pursue fellowships because of genuine interest and career goals, not because of a perceived lack of preparedness for practice. It would be very useful to re-evaluate the educational goals and competency expectations for general surgery residents in Canada |
| They specifically asked reasons for entering fellowship. |
ZERO said “not ready to enter practice” |
|||||||
| Napolitano 2014 JACS12 |
282/2939 surgeons ≤ age 45 978/9800 surgeons > age 45 Overall response rate = 10% |
The goal of general surgery residency is to enable graduates to enter surgical practice directly, and the fact that 80% of graduates do fellowships is concerning. There have been decreased operative experiences and outside regulatory forces in the last 5 years that have altered training. | Readiness to practice independently at the completion of residency, there may be differences between these perceptions between “young” and “older” surgeons. | To young surgeons: Did you feel that you had adequate surgical training to transition to the surgery attending role? Did you feel that you were prepared for the transition to the surgery attending role? Why did you pursue a fellowship (if you did)? How many times did you call a senior partner to help in your first year in practice? |
94% agree or strongly agree 91% agree or strongly agree |
14 | 8 | Young surgeons and older surgeons differ considerably, but both expressed concerns about readiness to practice. Older surgeons had much more negative views of recently graduated trainees than the recently graduated trainees had of themselves. |
|
To older surgeons: The current system of training residents allows chief residents to graduate with significant gaps in their education. |
Really variable, but 71% considered whether there was a senior partner to mentor and support them | |||||||
|
Do you feel that GS chief residents have adequate surgical training to transition to the surgery attending role? Estimate how often you were called in to help your junior colleague in their first year. |
53% agree or strongly agree (specifically asked to think about a young surgeon they had hired) 50% reported this happened 10-40% of cases done by their junior partner. |
|||||||
| Fonseca 2015 JSE18 |
249 programs June 2012. Focus was on PGY5 residents, 1102 surveys distributed to chiefs, 653 (59% response rate) 69% male, 68% university hospital, 51% affiliated with VA Same as previous publication, but separated the specific vascular procedures | Residents have less confidence due to a decline in operative autonomy, duty hours and subspecialization, specifically the endovascular interventions have made it so that open vascular operationsare problematic | Confidence = self-reported competence on specific operations | Rate operative confidence from 1(not confident) to 5(extremely confident) for | 1 | 10.5 | Residents have very little confidence in these vascular maneuvers and it means they may not be able to get out of trouble in the operating room. More simulation could help. Similar predictors toother Fonseca, et al studies: male gender, older age, more volume associated with higher confidence. | |
| Vascular anastomosis | 70% reported confidence | |||||||
| Confidence is a reflection of one’s ability to deal effectively with the technical and judgement related aspects of an operation. Confidence develops over time with deliberate practice, increased exposure and experience | Mid-abdominal aorta, Supraceliac aorta, Inferior Vena Cava, Great vessels of the chest | <25% reported confidence in any of these | ||||||
| Osman 2015 HPB19 |
Hepatobiliary fellows over 2 (2012-2013) years. 19 of 42 fellows (45% response rate) 53% came right from residency, 32% from other fellowship, 16% in practice |
HPB fellows experience challenges during the initial part of their training and there may be things that can be addressed in residency. HPB fellows are ideal to study because their skills are generalizable to the whole of general surgery residents | Expressed level of “comfort” for specific procedures, how much supervision a resident perceives s/he needs for specific operations | Level of comfort for specific procedures, 3 choices: No supervision, minimal supervision, full supervision | 100% comfortable with basic laparoscopic procedures, fewer for complex lap procedures. | 0 | 8 | Fellows felt prepared for fellowship. Fellows expressed less comfort in advanced laparoscopic procedures management of complex hepatobiliary patients. Incoming fellows who had been in general surgery practice for at least a year expressed the same levels of doubt as recent graduates |
| 89% felt adequately prepared for HPB fellowship Most unprepared for preoperative workup and management of pts. | ||||||||
| 21% cited technical skills as greatest fear of entering practice right out residency | ||||||||
| Klingensmith 2015 Ann Surg22 |
All graduates of general surgery programs between 2009–2013. 3354 of 5512 responded (61% response rate) 26% identified as general surgeons, 74% identified as subspecialists | Many authors have defined a “confidence crisis.” The purpose of this study was to better understand the perceived confidence of surgeons who had recently completed training. | Confidence means being able to independently perform, in a safe an efficient manner, as a general surgeon as a whole and then for specific listed procedures | 4? Point Likert scale Confidence to operate independently (global question) |
94% of general surgeons 90% of subspecialist surgeons |
2 | 11 | The vast majority of general surgery graduates are confident in their practices and possess high levels of satisfaction with their practice, whether general or subspecialty surgery. There was no association between case volume during residency and confidence |
| Confidence with specific procedures (16 common core general surgery procedures) | Overall confident, but general surgeons slightly more confident in most procedures queried | |||||||
| 23% of general surgeons said “confidence in current training” was a reason to do general surgery, while 7% of subspecialists said “needed more training to feel confident as a surgeon” was a reason to do fellowship | ||||||||
Acknowledgements
The author would like to thank the following individuals for their contributions, suggestions, and critical reviews: Nora Jacobson, Pamela Lipsett, John Tarpley, Patricia Numann, and Timothy Elfenbein. Dawn Elfenbein had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
The project described was supported by the Clinical and Translational Science Award (CTSA) program, through the NIH National Center for Advancing Translational Sciences (NCATS), grant UL1TR000427. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Presented as a “work in progress” at the Association for Surgical Education annual meeting, Surgical Education Research Fellowship (SERF) Forum, 4/24/2014, Seattle WA
References:
- 1.Page DW. Surgical competence today: what have we gained? What have we lost? Southern medical journal. 2010;103(12):1232–1234. [DOI] [PubMed] [Google Scholar]
- 2.Stain SC, Cogbill TH, Ellison EC, et al. Surgical training models: a new vision. Broad-based general surgery and rural general surgery training. Current problems in surgery. 2012;49(10):565–623. [DOI] [PubMed] [Google Scholar]
- 3.Borman KR, Vick LR, Biester TW, Mitchell ME. Changing demographics of residents choosing fellowships: longterm data from the American Board of Surgery. Journal of the American College of Surgeons. 2008;206(5):782–788; discussion 788–789. [DOI] [PubMed] [Google Scholar]
- 4.Eberlein TJ. A New Paradigm in Surgical Training. Journal of the American College of Surgeons. 2014;218(4):511–518. [DOI] [PubMed] [Google Scholar]
- 5.McKenna DT, Mattar SG. What is wrong with the training of general surgery? Advances in surgery. 2014;48:201–210. [DOI] [PubMed] [Google Scholar]
- 6.Chen PW. Are Today’s New Surgeons Unprepared. Well 2013; http://well.blogs.nytimes.com/2013/12/12/are-todays-new-surgeons-unprepared/? [Google Scholar]
- 7.What? American College of Surgeons establishes “Transition to Practice” fellowships. Skeptical Scalpel 2013; http://skepticalscalpel.blogspot.com/2013/04/what-american-college-of-surgeons.html. [Google Scholar]
- 8.Lipsett PA. Self-confidence and Stereotyping: Maybe They Are Wrong. Comment on “OurTrainees’ Confidence”. Archives of surgery (Chicago, Ill. : 1960). 2011;2011(146(8)):914–915. [Google Scholar]
- 9.Davis DA, Mazmanian PE, Fordis M, Van Harrison R, Thorpe KE, Perrier L. Accuracy of physician self-assessment compared with observed measures of competence: a systematic review. Jama. 2006;296(9):1094–1102. [DOI] [PubMed] [Google Scholar]
- 10.Mehdizadeh L, Sturrock A, Myers G, Khatib Y, Dacre J. How well do doctors think they perform on the General Medical Council’s Tests of Competence pilot examinations? A cross-sectional study. BMJ open. 2014;4(2):e004131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mattar SG, Alseidi AA, Jones DB, et al. General surgery residency inadequately prepares trainees for fellowship: results of a survey of fellowship program directors. Annals of surgery. 2013;258(3):440–449. [DOI] [PubMed] [Google Scholar]
- 12.Napolitano LM, Savarise M, Paramo JC, et al. Are general surgery residents ready to practice? A survey of the american college of surgeons board of governors and young fellows association. Journal of the American College of Surgeons. 2014;218(5):1063–1072.e1031. [DOI] [PubMed] [Google Scholar]
- 13.Coleman JJ, Esposito TJ, Rozycki GS, Feliciano DV. Early subspecialization and perceived competence in surgical training: are residents ready? Journal of the American College of Surgeons. 2013;216(4):764–771; discussion 771–763. [DOI] [PubMed] [Google Scholar]
- 14.Fonseca AL, Reddy V, Longo WE, Udelsman R, Gusberg RJ. Operative confidence of graduating surgery residents: a training challenge in a changing environment. American journal of surgery. 2014;207(5):797–805. [DOI] [PubMed] [Google Scholar]
- 15.Bucholz EM, Sue GR, Yeo H, Roman SA, Bell RH Jr., Sosa JA. Our trainees’ confidence: results from a national survey of 4136 US general surgery residents. Archives of surgery (Chicago, Ill. : 1960). 2011;146(8):907–914. [DOI] [PubMed] [Google Scholar]
- 16.Yeo H, Viola K, Berg D, et al. Attitudes, training experiences, and professional expectations of US general surgery residents: a national survey. Jama. 2009;302(12):1301–1308. [DOI] [PubMed] [Google Scholar]
- 17.Fonseca AL, Reddy V, Longo WE, Gusberg RJ. Graduating general surgery resident operative confidence: perspective from a national survey. The Journal of surgical research. 2014;190(2):419–428. [DOI] [PubMed] [Google Scholar]
- 18.Fonseca AL, Reddy V, Longo WE, Gusberg RJ. Are Graduating Surgical Residents Confident in Performing Open Vascular Surgery? Results of a National Survey. J Surg Educ. 2015. [DOI] [PubMed] [Google Scholar]
- 19.Osman H, Parikh J, Patel S, Jeyarajah DR. Are general surgery residents adequately prepared for hepatopancreatobiliary fellowships? A questionnaire-based study. HPB : the official journal of the International Hepato Pancreato Biliary Association. 2015;17(3):265–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Friedell ML, VanderMeer TJ, Cheatham ML, et al. Perceptions of graduating general surgery chief residents: are they confident in their training? Journal of the American College of Surgeons. 2014;218(4):695–703. [DOI] [PubMed] [Google Scholar]
- 21.Nadler A, Ashamalla S, Escallon J, Ahmed N, Wright FC. Career Plans and Perceptions in Readiness to Practice of Graduating General Surgery Residents in Canada. J Surg Educ. 2014. [DOI] [PubMed] [Google Scholar]
- 22.Klingensmith ME, Cogbill TH, Luchette F, et al. Factors influencing the decision of surgery residency graduates to pursue general surgery practice versus fellowship. Annals of surgery. 2015;262(3):449–455; discussion 454–445. [DOI] [PubMed] [Google Scholar]
- 23.Hoyt DB. Looking forward - February 2013. Bulletin of the American College of Surgeons. 2013;98(2):7–10. [PubMed] [Google Scholar]
- 24.Bandura A. Self-efficacy: the exercise of control. New York: W.H. Freeman; 1997. [Google Scholar]
- 25.Bandura A. Chapter 14: Guide for Constructing Self-Efficacy Scales Self-Efficacy Beliefs of Adolescents: Information Age Publishing; 2006:307–337. [Google Scholar]
- 26.Hinze SW. GENDER AND THE BODY OF MEDICINE OR AT LEAST SOME BODY PARTS. Sociological Quarterly. 1999;40(2):217–239. [Google Scholar]
- 27.Kellogg KC, Breen E, Ferzoco SJ, Zinner MJ, Ashley SW. Resistance to change in surgical residency: an ethnographic study of work hours reform. Journal of the American College of Surgeons. 2006;202(4):630–636. [DOI] [PubMed] [Google Scholar]
- 28.Cassell J. Doing Gender, Doing Surgery: Women Surgeons in a Man’s Profession. Human Organization. 1997;56(1):47–52. [Google Scholar]
- 29.Berger PL. The social construction of reality : a treatise in the sociology of knowledge / by Peter L. Berger and Thomas Luckmann. 1st Irvington ed ed. New York: :: Irvington Publishers,; 1980, c1966. [Google Scholar]
- 30.Foley PJ, Roses RE, Kelz RR, et al. The state of general surgery training: a different perspective. J Surg Educ. 2008;65(6):494–498. [DOI] [PubMed] [Google Scholar]
- 31.Fronza JS, Prystowsky JP, DaRosa D, Fryer JP. Surgical residents’ perception of competence and relevance of the clinical curriculum to future practice. J Surg Educ. 2012;69(6):792–797. [DOI] [PubMed] [Google Scholar]
- 32.Reed DA, Cook DA, Beckman TJ, et al. Association Between Finding and Quality of Published Medical Education Research. JAMA.2007;298(9):1002–1009 [DOI] [PubMed] [Google Scholar]
- 33.Morewedge CK. It Was a Most Unusual Time: How Memory Bias Engenders Nostalgic Preferences. Journal of Behavioral Decision Making. 2013;26(4):319–326. [Google Scholar]
- 34.Brooks JV, Bosk CL. Remaking Surgical Socialization: Work Hour Restrictions, Rites of Passage, and Occupational Identity. Social science & medicine (1982). 2012;75(9):1625–1632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Franzosi R. From words to numbers : narrative, data, and social science / Roberto Franzosi. New York: : Cambridge University Press; 2004. [Google Scholar]
- 36.Snyder RA, Terhune KP, Williams DB. Are today’s surgical residency graduates less competent or just more cautious? JAMA surgery. 2014;149(5):411–412. [DOI] [PubMed] [Google Scholar]
- 37.Cech E, Rubineau B, Silbey S, Seron C. Professional Role Confidence and Gendered Persistence in Engineering. American Sociological Review. 2011;76(5):641–666. [Google Scholar]
- 38.Gillman LM, Vergis A. General surgery graduates may be ill prepared to enter rural or community surgical practice. American journal of surgery. 2013;205(6):752–757. [DOI] [PubMed] [Google Scholar]