Abstract
Background: We aimed to develop a causal model of family well-being with health literacy (HL) as a mediator and to compare models between male and female spouses in urban and rural communities.
Study design: A cross-sectional study.
Methods: The samples included 2000 spouses at risk of non-communicable diseases (NCDs) by stratified randomly sampled in 2018. Data were collected Likert questionnaires with reliability of 0.79-0.93, and analyzed via confirmatory factor analysis (CFA), and multi-group structural equation modeling (MSEM).
Results: A causal model for the overall group was consistent with the data .Causal factors had direct effects on health behavior including social norms, positive attitude toward health, psychological capital, and HL (β=0.11, 0.14, 0.30, and 0.41, P<0.05 respectively). Health behavior and positive attitudes towards health had direct effects on family well-being (β=0.36 and 0.42, P<0.05, respectively). All factors could predict health behavior and family well-being with variance of 70 %and 50%. Invariance analysis of models showed no difference between male and female spouses. In addition, the mean comparison of latent variables showed that the positive attitudes towards health were lower in women than men. HL and positive attitudes towards health of spouses in urban were lower than in rural communities.
Conclusion: Thai adult families in cities were at higher risk with NCDs. Therefore, health providers need to address HL and positive attitude toward health which were the main causal factors.
Keywords: Psychological factors, Social norm, Healthy behavior, Health literacy, Well-being
Introduction
WHO highlighted concern about the growing incidence of non-communicable diseases (NCDs) worldwide, reporting that globally 70% of deaths each year are attributable to NCDs and the main four NCDs are cardiovascular diseases, cancers, chronic respiratory diseases, and diabetes accounting for 80% of all NCD deaths1.
Developing health literacy (HL) is regarded as core to improving health and well-being. HL is defined as cognitive and social skills which determine the motivation of individuals to access, understand and use information in ways which maintain good health2. Individuals with adequate levels of HL displayed more appropriate health behavior and better health outcomes than those with inadequate HL3,4. Patients with high HL could control their blood sugar levels 2.03 times better than patients with low HL5. Patients' levels of education and disease knowledge influenced their HL and their HL influenced their health behavior6. WHO in Shanghai prioritised increasing HL globally7. Worldwide surveys of population HL confirmed that it was problematic with low levels found in 32.5% of the population of USA8, New Zealand (56.2%)9, Bulgaria (62.1%), Spain (58.3%), Austria (56.4%), Germany (46.3%), Greece (44.8%), Poland (44.6%), Ireland (40%), the Netherlands (28.7%)10, and Japan (25.3%)11. Particularly low HL is reported among the elderly, the poorly educated, indigenous people, and in rural communities12,13. In Western cultures, social norms are an important factor influencing health behavior14. In an Asian collectivist culture the family plays a role in developing HL15. In Thailand, from 2000 to 2014, hypertension prevalence increased fivefold and diabetes by 11%16. In 2014, Thais had the second highest rate of obesity in the Association of Southeast Asian Nations17. In 2016, a national survey of 15,278 Thai adults found that 49% had low HL, 5.5% high HL, and 63% unhealthy behavior18.
The definition of well-being is taken from positive psychology as" a positive state of living, meaning to pursue one's goals, and being satisfied with one's life"19.. Character strengths influenced well-being20,21. Psychological capital is defined as “an individual’s positive psychological state consisting of self-efficacy, optimism, hope and resilience” 22. The pathway model of health guided the choice of variables to be included in the current study23. From this model relevant variables were the use of healthcare services, having healthy behavior, self-monitoring, attitudes, social norms, selfefficacy, and HL. The Individual and Family Selfmanagement Theory (IFSM) which specifies the causes of health outcomes and well-being guided the choice of variables such as self-efficacy, social support, community culture, and family and individual context variables24.
The aims of the study were to develop a causal model of family well-being and to compare models by moderating between male and female spouses in urban and rural areas.
Methods
Data for this cross-sectional study were collected via a survey designed to assess the variables identified in the literature review as being relevant to HL and health behaviour. The Thai adult participants between 35-59 year old were selected through a quota-stratified random sampling technique to make sure that both women and men from both urban or semi-urban and rural communities near the country's borders were selected equally. A previous survey18 identified ten provinces covering the north, south, northeast, and central Thailand where levels of HL were low and risks of NCDs were high. Data were used to randomly select 200 people from each province via the public health database, giving a total sample of 2000 adults, equally divided between rural and urban areas and men and women. Data were collected between Jan and Apr 2018. The sample size was based on the size required to confirm a causal model, between 100 and 200 people in each group25. The research assistants contacted participants by asking the Village Health Volunteers (VHVs) to set up times to meet with them in their own homes.
The survey was administered by four well-trained research assistants to ensure that meaningful data could be collected even if literacy levels were low or if there were difficulties in understanding any of the questions. Husbands and wives completed the survey separately
The Thai Adults Health Questionnaire was developed as a culturally appropriate measure of HL and health behavior .The HL elements were based on the General Health Literacy Scale13 developed with an Australian population with a very well-developed health care system so was not totally applicable to the Thai context. This scale was modified to assure cultural relevance in Thailand18 .For this study, it was expanded further to make a more comprehensive assessment of HL, health status and associated health behavior. These additional components were informed by reviewing the literature on HL models13,23
The questionnaire began with demographic information relating to age, gender, educational level, primary employment, years married or cohabiting, record of any medical problems, and checklist of symptoms relating to NCDs. Next competency in dealing with health-related issues, perceived ease of access to information and services, verification processes used for knowledge and services, communication, management of own and family health, availability of social support, social norms including health-related cultural wisdom and their influence, family role models, attitudes towards health-related behaviours and an assessment of the well-being of the family. All items were rated on a five-point Likert scale and scores were summated.
The questionnaire was assessed for breadth and relevance of content and cultural match by five experts in the field of health behavior, and psychology with high levels of agreement reached. The content analysis of items with index of item-objective congruence (IOC) were between 0.80-1.00. The internal reliability of the questionnaire was satisfactory with Cronbach’s alpha values ≤0.70 and the construct validity by the second confirmatory factor analysis (CFA) was satisfactory with factor loading of items ≤ 0.4026.
Pre-analysis checks were carried out on the data set on missing data, outliers, linearity, skewness, kurtosis, P>0.05 and multivariate normality25 and no problems were found. Demographic descriptive data was computed for all the variables. Then Confirmatory factor analysis (CFA) and multi-group structural equation modeling (MSEM) were computed to test the generated causal relationship model's applicability and to compare the latent variable mean by using LISREL program. Moreover, statistical values included the absolute fit index, Chi-Square (χ2) Goodness of Fit Index: GFI ≤0.90, Root Mean Squared Error Approximation: RMSEA ≥0.05, SRMR ≥ 0.05, NNFI, GFI ≤0.90 [Incremental fit index], and adjusted goodness of Fit Index: AGFI ≤0.90, and χ2/df ≤5. [Parsimony fit indices]26
Documented assent was obtained from all participants who could not provide written consent. The study was approved by the IRB of Srinakharinwirot University (Certificate of approval No. SWUEC/E-264/2560).
Results
The mean age of the rural sample was males =47.04, SD=7.56; females=45.99, SD=7.45, and the urban sample was males =48.45, SD=7.37; females=47.00, SD=7.17. The modal values for occupational group was farmers (33.8%), for education was elementary education (54.5%), and the duration of living together was 21–25yrs (18.7%). In terms of health risk for NCDs, 75.6% of the sample were not exercising and were overweight. High levels of health literacy were reported in 26% of the sample while 58.5% had levels rated as being inadequate but good levels of family well-being were reported by 61.0% of the sample. The demographics for each sample are shown in Table 1. The mean and standard derivation for each variable were computed. Cronbach's alphas were calculated for each scale and subscale and were satisfactory between 0.77-0.94. The construct validity by CFA with factor loading of items were between 0.45 and 0.87 (Table 2).
Table 1. Comparison of Sample demographics between the rural and urban populations and men and women .
| Demographics | Men, n=1000 | Women, n=1000 | Urban, n=1000 | Rural, n=1000 | ||||
| n | % | n | % | n | % | n | % | |
| Age (yr) | ||||||||
| 35-40 | 214 | 21.4 | 266 | 26.6 | 212 | 21.2 | 268 | 26.8 |
| 41-45 | 168 | 16.8 | 185 | 18.5 | 179 | 17.9 | 174 | 17.4 |
| 46-50 | 198 | 19.8 | 204 | 20.4 | 197 | 19.7 | 205 | 20.5 |
| 51-55 | 216 | 21.6 | 211 | 21.1 | 223 | 22.3 | 204 | 20.4 |
| 56-59 | 204 | 20.4 | 134 | 13.4 | 189 | 18.9 | 149 | 14.9 |
| Educational level | ||||||||
| None | 47 | 4.7 | 42 | 4.2 | 25 | 2.5 | 64 | 6.4 |
| Elementary | 551 | 55.1 | 539 | 53.9 | 526 | 52.6 | 564 | 56.4 |
| Middle school | 125 | 12.5 | 150 | 15.0 | 133 | 13.3 | 142 | 14.2 |
| High school or certificate | 157 | 15.7 | 124 | 12.4 | 149 | 14.9 | 132 | 13.2 |
| Associate degree | 50 | 5.0 | 51 | 5.1 | 58 | 5.8 | 43 | 4.3 |
| Bachelor's degree or higher | 70 | 7.0 | 94 | 9.4 | 109 | 10.9 | 55 | 5.5 |
| Occupation | ||||||||
| Agricultural | 363 | 36.3 | 314 | 31.4 | 325 | 32.5 | 352 | 35.2 |
| Shopkeeper | 219 | 21.9 | 223 | 22.3 | 115 | 11.5 | 327 | 32.7 |
| Government official | 82 | 8.2 | 85 | 8.5 | 88 | 8.8 | 79 | 7.9 |
| Employee or workers | 105 | 10.5 | 117 | 11.7 | 163 | 16.3 | 59 | 5.9 |
| Not in paid employment | 231 | 23.1 | 261 | 26.1 | 309 | 30.9 | 183 | 18.3 |
| Time couples married/cohabiting (yr) | ||||||||
| 0-5 | 84 | 8.4 | 78 | 7.8 | 49 | 4.9 | 113 | 11.3 |
| 6-10 | 109 | 10.9 | 112 | 11.2 | 89 | 8.9 | 132 | 13.2 |
| 11-15 | 122 | 12.2 | 137 | 13.7 | 138 | 13.8 | 121 | 12.1 |
| 16-20 | 145 | 14.5 | 151 | 15.1 | 168 | 16.8 | 128 | 12.8 |
| 21-25 | 190 | 19.0 | 184 | 18.4 | 186 | 18.6 | 188 | 18.8 |
| 26-30 | 181 | 18.1 | 168 | 16.8 | 207 | 20.7 | 142 | 14.2 |
| >30 | 169 | 16.9 | 170 | 17.0 | 163 | 16.3 | 176 | 17.6 |
Table 2. Means and standards deviation of each latent variable and its constituent scales and Cronbach's alphas for each scale .
| Variables | Rural | Urban | Cronbach’s α | Factor loading | ||
| Mean | SD | Mean | SD | |||
| Latent variable; HL was measured by 5observable variables | ||||||
| Access to health information and services | 3.64 | 0.81 | 3.76 | 0.69 | 0.82 | 0.46-0.75 |
| Understanding of health information and services | 3.59 | 0.86 | 3.76 | 0.73 | 0.83 | 0.51-0.80 |
| Verification of health information and services | 3.73 | 0.73 | 3.78 | 0.72 | 0.77 | 0.57-0.78 |
| Communication skill | 3.78 | 0.73 | 3.75 | 0.70 | 0.89 | 0.49-0.78 |
| Self-health management | 3.30 | 0.70 | 3.24 | 0.65 | 0.79 | 0.66-0.78 |
| Social support | 3.81 | 0.75 | 3.81 | 0.70 | 0.89 | 0.61-0.83 |
| Social norms | 3.87 | 0.72 | 3.69 | 0.69 | 0.83 | 0.66-0.87 |
| Positive attitude toward health | 3.77 | 0.72 | 3.74 | 0.63 | 0.84 | 0.58-0.84 |
| Psychological capital was measured by 4 observable variables | ||||||
| Hope | 3.91 | 0.76 | 3.88 | 0.72 | 0.93 | 0.72-0.79 |
| Optimism | 3.89 | 0.70 | 3.91 | 0.73 | 0.94 | 0.65-0.86 |
| Self-efficacy | 3.82 | 0.75 | 3.81 | 0.70 | 0.93 | 0.60-0.81 |
| Resilience | 3.95 | 0.76 | 3.95 | 0.69 | 0.93 | 0.70-0.80 |
| Health behavior was measured by 2 observable variables | ||||||
| Self-care | 3.47 | 0.89 | 3.69 | 0.71 | 0.87 | 0.45-0.79 |
| Participation in health activities | 3.55 | 0.90 | 3.68 | 0.89 | 0.87 | 0.75-0.75 |
| Family well-being was measured by 3 observable variables | ||||||
| Health status of family members | 4.07 | 0.75 | 4.08 | 0.69 | 0.89 | 0.65-0.77 |
| Parents' integrity | 4.12 | 0.82 | 4.10 | 0.76 | 0.89 | 0.67-0.85 |
| Family relationships | 4.08 | 0.82 | 4.16 | 0.80 | 0.88 | 0.77-0.86 |
The results of the hypothesis testing with empirical data showed that the influence and test statistical significance were not significant. The researchers adjusted the model by allowing tolerances to measure if the variables were related. The adjusted model results were as follows:
1) Testing the adjusted model A causal relationship model of social norm and psychology capital affecting health behavior and family well-being by mediating HL in overall group was consistent with the empirical data ꭓ2 =228.57, df =67 (P=0.00), ꭓ2 /df =3.41, RMSEA =0.03, SRMR = 0.02, GFI =0.99, NNFI =99, and AGFI =0.97. In addition, causal factors had direct effects on health behavior including social norm, positive attitudes, psychology capital, and HL (β=0.11, 0.14, 0.30, and 0.41, P<0.05 respectively). Besides, health behavior, and positive attitudes had direct effects on family well-being (β=0.36 and 0.42, P<0.05 respectively). Total causal variables had indirect effects on family wellbeing such as psychology capital, social support, HL, social norm, and positive attitudes were 0.16, 0.15, 0.15, 0.06, and 0.05, P<0.05 respectively. All factors could predict health behavior and family well-being with variance of 70% and 50% (Figure 1 and Table 3).
Figure 1.
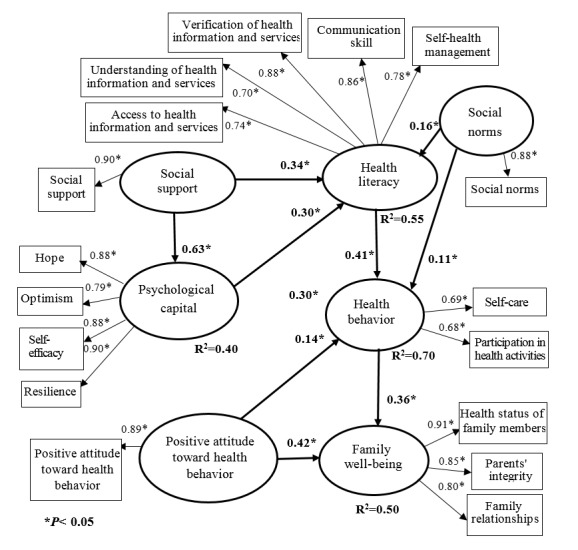
Causal relationship model of social norm and psychological instead capital effects on health behavior and family well-being by mediating HL of spouses at risk of NCDs, in overall group (n=2000)
Table 3. Influence coefficient (β) in the adjusted model effected on health behavior and family well-being by mediating HL in overall group .
| Causal variables |
Psychological capital
(R2= 0.40) |
Health literacy
(R2= 0.55) |
Health behavior
(R2= 0.70) |
Family well-being
(R2= 0.50) |
||||||||
| DE | IE | TE | DE | IE | TE | DE | IE | TE | DE | IE | TE | |
| Social support | 0.63 | 0.00 | 0.63 | 0.34 | 0.19 | 0.53 | 0.00 | 0.41 | 0.41 | 0.00 | 0.15 | 0.15 |
| Social norms | 0.00 | 0.00 | 0.00 | 0.16 | 0.00 | 0.16 | 0.11 | 0.07 | 0.18 | 0.00 | 0.06 | 0.06 |
| Psychological capital | 0.00 | 0.00 | 0.00 | 0.30 | 0.00 | 0.30 | 0.30 | 0.13 | 0.43 | 0.00 | 0.16 | 0.16 |
| Health literacy | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.41 | 0.00 | 0.41 | 0.00 | 0.15 | 0.15 |
| Positive attitude toward health | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.14 | 0.00 | 0.14 | 0.42 | 0.05 | 0.47 |
| Health behavior | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.36 | 0.00 | 0.36 |
DE = Direct effect, IE = Indirect effect, TE =Total effect
2) Differences in responding in the model between male and female spouses and between urban and rural respondents were examined by testing the invariance of causal models and comparing the means of the latent variables. The results indicated no differences in the causal models between men and women (Δc2= 13.22, Δ df= 10, P-value= 0.21) In terms of the direct and indirect influences of the causal factors on health behavior, and family well-being there were no difference between male and female spouses. There were statistically significant differences in the causal models between spouses in the urban and rural communities (Δc2= 93.31, Δdf= 10, P=0.001). These differences in effect size and factor loading on some of the paths in the causal model are shown in Figure 2.
Figure 2.
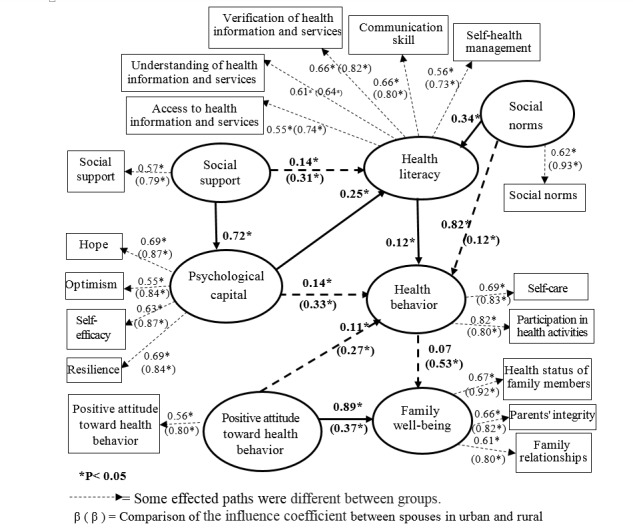
Results of influence coefficient estimation in when comparing the causal relationship model affecting health behavior and family well-being by mediating HL between spouses in urban (n=1000) and rural (n=1000)
3) Comparison of the means of the latent variables showed that positive attitudes toward health in women was lower than in men (d= 0.06, SE= 0.03, t-value= 2.08, P<0.05). There were no significant differences in the mean scores between men and women for social support, social norms, psychological capital, HL, health behavior and family well-being (Table 4). There were significant difference in mean scores HL (d= 0.11, SE= 0.02, t-value=5.64), positive attitudes toward health (d= 0.10, SE= 0.03, t-value= 3.34), and family well-being (d= -0.09, SE= 0.03, t-value= 2.93) of spouses were lower in urban than rural communities (Table 5).
Table 4. Comparison of the latent variable average in the causal relationship model affecting to health behavior and family well-being by mediating HL between male and female spouses .
| Latent variables | Average difference (d) | Standard error (SE) | t value |
| Social support | 0.05 | 0.03 | 1.90 |
| Social norms | 0.04 | 0.03 | 1.46 |
| Psychological capital | 0.02 | 0.03 | 0.82 |
| Health literacy | 0.01 | 0.02 | 0.70 |
| Positive attitude toward health | 0.06 | 0.03 | 2.08* |
| Health behavior | 0.02 | 0.03 | 0.75 |
| Family well-being | 0.02 | 0.03 | 0.68 |
* P<0.05, Average difference= Mean of latent variable in men- Mean in women group
Table 5. Comparison of the latent variable average in causal relationship model affecting to health behavior and family well-being by mediating HL between spouses in urban and rural communities .
| Latent variables | Average difference (d) | Standard error (SE) | t value |
| Social support | 0.00 | 0.03 | -0.01 |
| Social norms | -0.02 | 0.03 | -0.67 |
| Psychological capital | 0.00 | 0.02 | 0.17 |
| Health literacy | 0.11 | 0.02 | 5.64* |
| Positive attitude toward health | 0.10 | 0.03 | 3.34* |
| Health behavior | 0.03 | 0.03 | 1.03 |
| Family well-being | 0.09 | 0.03 | 2.93* |
* P<0.05, Average difference=Mean of latent variable in rural - urban spouses
Discussion
We found that all factors could significantly predict health behavior, and family well-being of Thai adult families in these communities. According to the logic model23 and systems theory that predict health behavior and health outcome well-being increased with higher health literacy24. In this model for the overall group, 70% of health behavior and 50% of family well-being could be explained by the all factors. HL had highest direct influence on health behavior, psychology capital, positive attitudes, and social norm, respectively. Both men and women with higher HL, psychology capital, positive attitudes, and social norm reported better health. They participated in health activities and maintained self-care in higher level too. HL directly influenced the health behavior of diabetic patients5. Critically, HL influenced obesity preventive behaviors, and motivation, with functional HL associated with diet in type 2 diabetics27. Including, health literacy development, the activities focused on ways of searching for correct health information, health information access skills, using social media safely, and exchanging health information to improve self-care behavior and encourage patients to self-care28. Additionally, health literacy had indirect effect on well-being measured by participating in social activities18. Health knowledge and understanding had an indirect effect on participating in social activities via mediation managing their health condition, media literacy, appropriate decision-making, and maintaining in health behaviors.
Psychological capital affected directly health behavior and indirectly family well-being (β =0.30, 0.16 respectively). Psychological capital refers to an individual's positive psychological strengths which lead to behavior change22. Therefore, psychological capital represents an individual's positive characteristics such as self-efficacy, hope, optimism, and resilience developed and used to motivate an individual to work effectively. Developing psychological capital such as hope, efficacy, resilience, and optimism in college students significantly increased their positive health29. This supports a German study that highlighted the association between psychological factors (Positive and negative affect, life satisfaction, optimism, self-esteem, self-efficacy, and self-regulation) and frequent attendance in primary care of 7,446 people with aged 40. This is consistent with similar research in Thailand30.
Positive attitudes toward health and social norms influenced health behavior. The theory of planned behavior was strongly supported in this study with positive attitudes and subjective norm as predictors of health behavior14. These findings are supported by a study of an educational intervention on attitude, subjective norms, parental control, and behavioral control31 that produced significant reductions in risky sexual and reproductive health behavior. Social support directly influenced HL in the study. Similarly, social support was the strongest predictor of interactive and critical health literacy of 650 Chinese students aged 7-9 yr32. Social support is an important health variable previously shown to improve the psychosocial health status of soldiers and reduce their levels of depression33. Social support similarly predicted lower depression in the elderly in a community study31. The presence of social support and the introduction of activities to generate such support are important to improve health and wellbeing.
Comparisons of the effect sizes and latent variable averages in the causal relationship models by gender were not significant, nor were the invariance models. Factors such as social support, social norms, psychological capital, and positive attitude toward health influence health behavior and family well-being by mediating health literacy, This applies for, men, women and the overall group. Thus, gender had no interaction with any latent variables in this model. Hence, common activities addressing the same variables can be implemented for men and women to promote healthy behavior and well-being. While, no differences in the causal models was found between spouses in the urban and rural areas and HL; positive attitudes toward health and family well-being were lower in urban spouses than in rural communities. Many rural areas of Thailand have recently changed to become urban areas. However, medical provision in these areas has not been fully developed yet. This may help to explain the lower scores in these recently urbanized areas compared with the rural areas where services are more established. This result is inconsistent with a population surveys of Chinese adults where the prevalence of metabolic syndrome (MS) whith raised fasting glucose and raised blood pressure was significantly higher in rural residents than in their urban counterparts. They looked, at newly urbanized Chinese areas similar to those found in this study and found that as urbanization progressed and health services were introduced health improved in theses previously rural areas34. This demonstrates the impact of community health care services. In Thailand rural health care is well developed but is poorer in the more recently urbanized areas. Health providers need to be aware of the urgent need to provide local health care services as urban areas expand to support the development of health literacy and promote wellbeing in theses urbanised communities. While the urban or semi-urban and rural communities share features such as the prevalence of NCDs and socio-psychological risk factors, the differences found may be partly explained by lifestyle factors and the population changes as people move to urban areas. Given the high prevalence of NCDs in Thai adults intervention strategies are required to address these rural-urban disparities.
Conclusion
The majority of the Thai adult families had health risks by not exercising, being overweight, and having inadequate HL levels. All factors; psychology capital, social support, HL, social norms, and positive attitudes predicted health behavior. Moreover, good health behavior and positive attitude toward health had positive direct effects on family well-being. There was no difference in the causal relationship model of HL and family well-being between male and female spouses although women had less positive attitudes towards health than men.
Acknowledgements
The authors thank all participants include the health provider as research assistants and the chief of medical officers as gatekeeper of the target communities in this study.
Conflict of interest statement
This work is original and has not been published elsewhere nor is it currently under consideration for publication elsewhere. The authors declare no conflict of interest.
Funding
This study, as a part of multi-phase project, was supported the Newton Advanced Fellowships, financially supported via the British Academy (Grant No. AF170002/2017), United Kingdom and Thailand Research Fund (DBG61/2561).
Highlights
Health literacy and attitude are key factors affecting health behaviors and well-being.
Health literacy and character development improve well-being sustainably.
Health providers should use these results to designing NCDs prevention interventions.
Citation: Intarakamhang U, Macaskill A. Multi-group Causal Model of Health Literacy and Behaviors on Family Well-being among Thai Adults at Risk of NonCommunicable Diseases (NCDs). J Res Health Sci. 2018; 18(4): e00429.
References
- 1. World Health Organization. Global status report on non-communicable diseases 2014. Geneva: WHO; 2014.
- 2. Kanj M, Mitic W. Health literacy and health promotion: Definitions, concepts and examples in the Eastern Mediterranean Region, Individual empowerment conference working document at 7thGlobal Conference on Health Promotion. Geneva: WHO; 2009.
- 3. Institute of Medicine Committee. Health literacy: A prescription to end confusion. Washington DC: National Academies Press; 2004. [PubMed]
- 4.Schillinger D, Barton LR, Karter AJ, Wang F, Adler N. Does literacy mediate the relationship between education and health outcomes? A study of a low-income population with diabetes. Public Health Reports. 2006;121(3):245–54. doi: 10.1177/003335490612100305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schillinger D, Grumbach K, Piette J, Wang F, Osmond D, Daher C, Palacios J, Sullivan GD, Bindman AB. Association of health literacy with diabetes outcomes. JAMA. 2002;288(4):475–82. doi: 10.1001/jama.288.4.475. [DOI] [PubMed] [Google Scholar]
- 6.Sun Ying, Paulus Dominique, Eyssen Maria, Maervoet Johan, Saka Omer. Systematic review and meta-analysis of acute stroke unit care: What’s beyond the statistical significance? BMC Med Res Methodol. 2013;13:132. doi: 10.1186/1471-2288-13-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. World Health Organization. Promoting health in the SDGs. Report on the 9th Global Conference for Health Promotion, Shanghai2016. Geneva: WHO; 2017.
- 8. U.S. Department of Health & Human Service. America's health literacy: Why we need accessible health information. Washington DC. Available from: https://health.gov/communication/literacy/issuebrief/.
- 9. Marama K. Health literacy and Maori: Results from the 2006 adult literacy and life skills survey. Wellington: Ministry of Health; 2010.
- 10.Sørensen K, Van den Broucke S, Fullam J, Doyle G, Pelikan J, Slonska Z. et al. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health. 2012;12:80. doi: 10.1186/1471-2458-12-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nakayama K, Osaka W, Togari T, Ishikawa H, Yonekura Y, Sekido A. Comprehensive health literacy in Japan is lower than in Europe: A validated Japanese-language assessment of health literacy. BMC Public Health. 2015;15:505. doi: 10.1186/s12889-015-1835-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Intarakamhang U, Intarakamhang P. Health literacy scale and causal model of childhood overweight. J Res Health Sci. 2017;17(1):e00368. [PubMed] [Google Scholar]
- 13.Osborne RH, Batterham RW, Elsworth GR, HawkinsM HawkinsM, Buchbinder R. The grounded psychometric development and initial validation of the health literacy questionnaire (HLQ) BMC Public Health. 2013;13:658. doi: 10.1186/1471-2458-13-658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ajzen I. The theory of planned behavior. Organizational Behavior and Human Decision Processes. 1991;50(2):179–211. [Google Scholar]
- 15. ASEAN Secretariat. ASEAN socio-cultural community blueprint. Jakarta: ASEAN Secretariat; 2009.
- 16. Aekplakorn W. 5th Thai national health examination survey in 2014. Health Systems Research Institute. Bangkok: Aksorn Graphic & Design Publishing, 2015. [in Thai].
- 17. Center for the Study of Social Policy. Policy matters: Setting and measuring benchmarks for state polies. Washington DC: CSSP; 2004.
- 18.Intarakamhang U, Kwanchuen Y. The development and application of the ABCDE-health literacy scale of Thais. Asian Biomedicine. 2016; 10(6):575–82. [Google Scholar]
- 19. McGregor A. Researching well-being: From concepts to methodology, in Gough I. McGregor A (Eds) Well-being in Developing Countries: From theory to research. Cambridge: Cambridge University Press; 2007.
- 20.Intarakamhang U, Ekpanyaskul C. Effect of positive psychology and cultural social norm on healthy behavior and family well-being by mediated health literacy of family in the semi-urban community: Mixed methods. Journal of Behavioral Science. 2018; 24(1):1–22. [Google Scholar]
- 21.Macaskill A. Review of positive psychology applications in clinical medical populations. Healthcare. 2016;4:66. doi: 10.3390/healthcare4030066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Luthans F, Youssef CM, Avolio BJ. Psychological capital. NY: Oxford University Press; 2007.
- 23.Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Viera A, Crotty K, Holland A, Brasure M, Lohr KN, Harden E, Tant E, Wallace I, Viswanathan M. Health literacy interventions and outcomes: An updated systematic review. Evid Rep Technol Assess. 2011; 199:1–941. [PMC free article] [PubMed] [Google Scholar]
- 24.Ryan P, Sawin KJ. The individual and family self-management theory: Background and perspectives on context, process and outcomes. Nurs Outlook. 2009;57(4):217–25. doi: 10.1016/j.outlook.2008.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hair JF, Black WC, Babin BJ, Anderson RE. Multivariate data analysis. Upper Saddle River, NJ: Perason Education International; 2010.
- 26. Schumacker RE, Lomax RG. A beginner’s guide to structural equation modelling. New York: Routledge; 2010.
- 27.Juul L, Rowlands G, Maindal HT. Relationships between health literacy, motivation an, diet and physical activity in people with type 2 diabetes participating in peer-led support groups. Prim Care Diabetes. 2018;12(4):331–7. doi: 10.1016/j.pcd.2018.02.005. [DOI] [PubMed] [Google Scholar]
- 28.Wolf MS, Davis TC, Curtis LM, Webb JA, Bailey SC, Shrank WH. et al. Effect of standardized, patient-centered label instructions to improve comprehension of prescription drug use. Medical Care. 2011;49(1):96–100. doi: 10.1097/MLR.0b013e3181f38174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Selvaraj PR, Bhat CS. Predicting the mental health of college students with psychological capital. J Ment Health. 2018;7:1–9. doi: 10.1080/09638237.2018.1469738. [DOI] [PubMed] [Google Scholar]
- 30.Hajek A, Bock JO, König HH. Association of general psychological factors with frequent attendance in primary care: a population-based cross-sectional observational study. BMC Fam Pract. 2017;18(1):48. doi: 10.1186/s12875-017-0621-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Darabi F, Yaseri M, Kaveh MH, Khalajabadi F, Majlessi F, Shojaeizadeh D. The Effect of a theory of planned behavior-based educational intervention on sexual and reproductive health in Iranian adolescent girls: A randomized controlled trial. J Res Health Sci. 2017;17(4):e00400. [PubMed] [Google Scholar]
- 32. Guo S, Davis E, Yu X, Naccarella L, Armstrong R, Abel T, Browne G, & Shi Y. Measuring functional, interactive and critical health literacy of Chinese secondary school students: reliable, valid and feasible? Glob Health Promot 2018; 1757975918764109. [In press]. [DOI] [PubMed]
- 33.Nosratabadi M, Halvaiepour Z. A structural equation modeling of the relationships between depression, drug abuse and social support with suicidal ideation among soldiers in Iran in 2015. J Res Health Sci. 2016;16(4):212–6. [PMC free article] [PubMed] [Google Scholar]
- 34.Shaoyong Xu, Jie Ming, Chao Yang, Bin Gao, Yi Wan, Ying Xing, Lei Zhang, and Qiuhe J. Urban, semi-urban and rural difference in the prevalence of metabolic syndrome in Shaanxi province, northwestern China: a population-based survey. BMC Public Health. 2014;14:104. doi: 10.1186/1471-2458-14-104. [DOI] [PMC free article] [PubMed] [Google Scholar]


