Abstract
Introduction
Smoking prevalence is high in Vietnam, yet tobacco dependence treatment (TDT) is not widely available.
Methods
We conducted a quasiexperimental study that compared the effectiveness of health care provider advice and assistance (ARM 1) versus ARM 1 plus village health worker (VHW) counseling (ARM 2) on abstinence at 6-month follow-up. This study was embedded in a larger two-arm cluster randomized controlled trial conducted in 26 community health centers (CHCs) in Vietnam. Subjects (N = 1318) were adult patients who visited any participating CHC during the parent randomized controlled trial intervention period and were self-identified as current tobacco users (cigarettes and/or water pipe).
Results
At 6-month follow-up, abstinences rates in ARM 2 were significantly higher than those in ARM 1 (25.7% vs. 10.5%; p < .001). In multivariate analyses, smokers in ARM 2 were almost three times more likely to quit compared with those in ARM 1 (adjusted odds ratio [AOR] = 2.96, 95% confidence interval [CI] = 1.78% to 4.92%). Compared to cigarette-only smokers, water pipe–only smokers (AOR = 0.4, 95% CI = 0.26% to 0.62%) and dual users (AOR = 0.62, 95% CI = 0.45% to 0.86%) were less likely to achieve abstinence; however, the addition of VHW counseling (ARM 2) was associated with higher quit rates compared with ARM 1 alone for all smoker types.
Conclusion
A team approach in TDT programs that offer a referral system for health care providers to refer smokers to VHW-led cessation counseling is a promising and potentially scalable model for increasing access to evidence-based TDT and increasing quit rates in low middle-income countries (LMICs). TDT programs may need to adapt interventions to improve outcomes for water pipe users.
Implications
The study fills literature gaps on effective models for TDT in LMICs. The addition of VHW-led cessation counseling, available through a referral from primary care providers in CHCs in Vietnam, to health care provider’s brief cessation advice, increased 6-month biochemically validated abstinence rates compared to provider advice alone. The study also demonstrated the potential effectiveness of VHW counseling on reducing water pipe use. For LMICs, TDT programs in primary care settings with a referral system to VHW-led cessation counseling might be a promising and potentially scalable model for increasing access to evidence-based treatment.
Introduction
Vietnam has one of the highest rates of tobacco use worldwide.1 On the basis of 2015 Global Adult Tobacco Survey (GATS), 45.3% of adult men are current smokers, 36.7% use cigarettes, 13.7% use water pipe, and less than 2% use smokeless tobacco.2 The smoking rate among women is only 1.1%, which reflects a persistent gender norm that cigarette smoking is less acceptable among women.2,3
Article 14 of the World Health Organization’s (WHO) Framework Convention on Tobacco Control requires Parties to implement effective strategies to “promote cessation of tobacco use and adequate treatment for tobacco dependence.”4 Despite the large body of evidence supporting the effectiveness and affordability of a range of health care setting (eg, clinician brief advice to quit) and population-based tobacco cessation interventions (eg, national quitlines), progress in implementing Article 14 has been slow, particularly in low middle-income countries (LMICs).5,6
There is also a large literature demonstrating effective strategies for overcoming barriers to implementing tobacco dependence treatment (TDT) guidelines in primary care settings.7,8 For example, integrating a system to facilitate referrals to more intensive counseling through either national quitlines or local programs can enhance provider adherence to guideline-recommended TDT and increase smoking abstinence rates.9–11 However, these studies have been largely conducted in high-income countries. More research is needed to develop effective models for implementing TDT in low-resource settings.12
When this study was launched in 2014, Vietnam did not have a national quitline. However, in Vietnam, as in other LMICs, there are infrastructure elements, including a robust public health delivery system with an extensive network of community health workers (CHWs), called village health workers (VHWs) in Vietnam. CHWs are highly respected members of the community and health care system and have a successful record of effectively delivering preventative services and increasing the reach of health programs.13–20 Thus, it is surprising that few studies have evaluated the role of CHWs as a resource for increasing access to evidence-based smoking cessation services or analyzed the effectiveness of CHW-led cessation interventions, particularly in LMICs.21–23
To fill this gap, we conducted a quasiexperimental study that was embedded in a larger two-arm cluster randomized controlled trial (RCT) conducted in community health centers (CHCs) in Vietnam. The purpose of this study was to compare the effectiveness of health care provider advice and cessation assistance (brief cessation counseling and educational materials [ARM 1] vs. ARM 1 plus a referral to VHW-led 3-session in-person cessation counseling [ARM 2]). The primary outcome was 6-month carbon monoxide (CO)–confirmed tobacco abstinence. High rates of water pipe use in the study population also provided an opportunity to compare outcomes by type of smoker and thus address the dearth of literature on effective cessation interventions for water pipe use and dual tobacco use (cigarettes and water pipe).24
Methods
Study Setting
This study was conducted in CHCs located in Thai Nguyen province, which is in a rural region north of the Vietnam capital, Hanoi. The public health system in Vietnam consists of four administrative levels: national, provincial or municipal, district, and commune (ie, community). Each commune has 15–20 villages and a population of 6000–10 000 people. There is one CHC per commune. CHCs are staffed by 5–6 health care providers and supported by the 8–20 VHWs who are each assigned to one village. Depending on the village population, VHWs serve 300–600 people. They implement national health promotion and disease prevention programs and work with CHC providers to conduct home-based follow-up to ensure that patients are adhering to treatment and prevention plans. There are more than 100 000 VHWs working with communities and CHCs in Vietnam.
Study Design
We conducted a quasiexperimental study embedded in a larger two-arm cluster RCT in which 26 CHCs were randomized in three waves to one of two models to enhance implementation of TDT guidelines into routine care: (1) Ask (screen for tobacco use), Advise to quit, Assess readiness to quit, and Assist (brief counseling and educational materials) (4As/ARM 1) versus (2) 4As plus a system for providers to refer smokers to a trained VHW for three sessions of in-person cessation counseling (4As+R/ARM 2). The intervention components were based on US Public Health Services (PHS)25 and WHO guidelines4 for treating tobacco use, and a growing literature that supports the effectiveness of integrating lay health workers as members of the health care team to improve access to preventive services.19,23,26,27 The primary outcome of the parent RCT is provider adherence to TDT guidelines. Details regarding the study design of the RCT have been described in a previous article.28
This quasiexperimental study compares, at the individual patient level, the effectiveness of health care provider–delivered 4As with 4As+R among patients who visited study sites during the intervention period of the parent RCT. The main outcome was 6-month, 7-day point prevalence abstinence with CO confirmation.29 The study was approved by the institutional review boards of the Institute of Social Medical Studies in Vietnam and the New York University School of Medicine.
Subject Eligibility
Subjects were adult patients who visited the participating CHCs enrolled in waves 1 and 2 (n = 18 CHCs) during the parent RCT period and self-reported current tobacco use (ie, water pipe use and/or cigarette smoking in past 7 days). In ARM 2 sites, eligibility also required that patients were willing to be referred to a VHW for additional cessation counseling.
Study Conditions
All health care providers working in study sites in both study arms attended a 2-day training informed by the US PHS guideline for Treating Tobacco Use and Dependence25 and the WHO Tobacco Control Package for Building Capacity for Tobacco Control in primary care,30 and addressed core competences defined by the Association for the Treatment of Tobacco Use and Dependence.31 Providers at each site also attended a 1-day booster training 3 months after the start of the intervention. Additional materials were developed as part of a tool kit to support provider and patient behavior change (ie, poster in examination rooms to prompt providers to ask about tobacco use and offer brief counseling, patient educational brochures, and a desktop guide for providers outlining standard cessation counseling content) (see http://vquit.vn/en/professional-documents/ for materials).
ARM 1: Smokers who visited the ARM 1 sites during the intervention period were screened for tobacco use (Ask), offered advice to quit, assessed for readiness, and offered cessation assistance (ie, brief counseling and educational brochures) (4As).
ARM 2: Smokers who visited the ARM 2 sites received the 4As and were offered a referral to a VHW for additional three-session cessation counseling. In each of the 9 ARM 2 study sites, we chose 6–8 VHWs who met eligibility criteria to serve as counselors (n = 65). These criteria included having worked as a VHW at that site for a year or more, not a current smoker, and willing to participate in the required components of the study intervention (ie, training and providing three sessions of counseling to eligible smokers). VHW counselors worked with participants who lived in their assigned village and 1–2 contiguous villages depending on the number of referred smokers.
VHWs received a 4-day training. The training included all of the components in the health care provider training with additional training on how to use the three-session manual. The manual was informed by the theory of behavior change,32 incorporated a motivational interviewing and social cognitive skills building approach (eg, identifying triggers, coping strategies) and, through formative research,25,33 was culturally adapted for a rural population of Vietnamese smokers.28,34 During their weekly visit to the CHCs, VHWs picked up referral forms that were completed by CHC providers and contacted smokers within 5 days of patient’s CHC visit to schedule the first counseling session. All three counseling sessions were conducted by VHWs in-person at the participant’s home and each session lasted approximately 30–40 minutes. The goals of session 1 were to assess smoking history and knowledge about the risks of smoking and benefits of quitting, provide education, explore ambivalence and specific pros and cons of quitting, elicit individual (eg, low self-efficacy) and social (eg, experiencing pressure to smoking when offered a cigarette by a friend or coworker) barriers to quitting, foster readiness by eliciting strategies for coping with challenges, and to start developing a quit plan including making their home smoke-free. Sessions 2–3 continued to foster readiness, and for those who had quit, to help prevent relapse by reinforcing strategies for dealing with challenges and triggers to smoke and building coping skills through role play and personalized feedback (eg, role-playing refusal skills).
To enhance fidelity, VHWs attended a 1-day booster training session and were given a packet with the three-session field manual outlining the content for each session, short handouts that provided more information about specific topics covered during the session that were given to the smoker (eg, benefits of quitting), and a checklist to complete for each patient interaction. Although guided by a manual to assure consistency of the intervention, counselors were trained to tailor the content to the participant’s current level of motivation to quit.
Measures
The primary outcome for this study was 7-day point prevalence smoking abstinence at 6-month follow-up was assessed with an in-person survey and CO validation, conducted by research staff.29 For dual users, this was defined as smoking abstinence for both water pipe and cigarettes.
The type of smoker was assessed at baseline with two questions which asked the participant if he or she smoked cigarettes or a water pipe on some days, every day, or not at all. Cigarette-only smokers responded that they smoked cigarettes on “some days” or “every day” AND “not at all” for water pipe smoking. Water pipe–only smokers reported water pipe use on “some days” or “every day” AND “not at all” for cigarette smoking. Dual users reported smoking “some days” or “every day” for both cigarettes and water pipe. Respondents reported the number of cigarettes smoked per day, and the number of times they used a water pipe per day.
Demographic variables included age, gender, educational attainment, marital status, and occupation.
Statistical Analyses
Of 1318 participants who completed a baseline survey, 99 did not complete a 6-month follow-up survey and 63 participants who self-reported abstinence at 6 months did not complete a CO test. Using an intent-to-treat approach for the analysis, we assumed these 162 participants were not abstinent from smoking at 6-month follow-up. We used descriptive statistics to summarize the sample characteristics at baseline by study ARM. We compared baseline sample characteristics using Fisher exact tests for categorical variables and Wilcoxon rank sum tests for continuous variable (ie, age). To estimate the impact of VHW counseling on smoking abstinence, we used generalized linear mixed-effects models (GLMMs),35 with ARM 2 patients nested within 1 of 65 VHWs, all patients nested within 1 of the 18 communes, and randomly varying intercepts. Covariates, measured at baseline, included age, gender, education attainment, marital status, occupation, type of smoker (ie, cigarette-only, water pipe–only, and dual users), cigarette consumption per day, and water pipe smoking session per day. To address a modest amount of missing data on covariates, we used multiple imputation with the mice package of the R statistical computing environment.36–38 A total of 20 imputed datasets were generated, with GLMM analyses repeated for each imputation and then pooled. CO-confirmed smoking abstinence was regressed on covariates as well as a study ARM indicator variable. The lme4 package of the R statistical computing environment was used for GLMM analysis. All tests of statistical significance were two-tailed, and p < .05 was considered statistically significant.
Results
Table 1 shows the characteristics of the samples by study ARM. Most respondents were males (99.4%), with an average age of 47.9 (SD = 14.3) years for ARM 1 and 48.4 (SD = 13.2) years for ARM 2. Less than a quarter of subjects had a high school education. Most were cigarette-only smokers (42.4% in ARM 1; 44.4% in ARM 2). However, water pipe smoking was prevalent: 57.6% of participants in ARM 1 reported water pipe smoking (including 20.5% water pipe–only smokers and 37.1% dual users who smoked both cigarettes and water pipe) and 55.5% were water pipe smokers in ARM 2 (including 18.2% water pipe–only smokers and 37.3% dual users).
Table 1.
Characteristics of Sample by Study ARM
| ARM 1a (n = 537) |
ARM 2b (n = 781) |
p | |||
|---|---|---|---|---|---|
| n | (%) | n | (%) | ||
| Age, mean (SD) | 517 | 47.9 (14.3) | 718 | 48.4 (13.2) | .796 |
| Gender | 1.00 | ||||
| Female | 3 | (0.6 | 5 | (0.7) | |
| Male | 516 | (99.4 | 713 | (99.3 | |
| Education attainment | <.001 | ||||
| Primary or less | 42 | (10.6 | 79 | (11.1 | |
| Secondary school | 192 | (48.6 | 417 | (58.4 | |
| High school | 86 | (21.8 | 161 | (22.5 | |
| Vocational or advanced | 75 | (19.0 | 57 | (8.0 | |
| Marital status | .141 | ||||
| Married | 357 | (89.9 | 664 | (92.6 | |
| Other | 40 | (10.1 | 53 | (7.4 | |
| Occupation | .001 | ||||
| Farmer or Fisherman | 267 | (67.6 | 523 | (72.8 | |
| Government employee | 40 | (10.1 | 32 | (4.5 | |
| Other | 88 | (22.3 | 163 | (22.7 | |
| Type of smokerc | .636 | ||||
| Cigarette-only smoker | 168 | (42.4 | 319 | (44.4 | |
| Water pipe–only smoker | 81 | (20.5 | 131 | (18.2 | |
| Dual user | 147 | (37.1 | 268 | (37.3 | |
| Cigarettes smoked per day, mean (SD) | 517 | 10.9 (9.6) | 718 | 11.1 (9.4) | .657 |
| Water pipe session per day, mean (SD) | 517 | 8.1 (10.8) | 718 | 7.6 (9.9) | .449 |
aParticipants in ARM 1 received health care provider–delivered 4As.
bParticipants in ARM 2 4As plus a referral to village health workers for 3-session in-person cessation counseling.
cCigarette-only smokers reported cigarette smoking on “some days” or “every day” AND “not at all” for water pipe smoking; water pipe–only smokers reported water pipe use on “some days” or “every day” AND “not at all” for cigarette smoking; dual users reported “some days” or “every day” for both cigarette and water pipe smoking.
We assessed the number of VHW counseling sessions completed using data from the intervention tracking booklet that VHWs were trained to use to document each counseling session. Among the 781 participants in ARM 2, 97.4% completed at least one session (1.8% completed one, 2.9% completed two, and 92.7% completed three counseling sessions; data not shown).
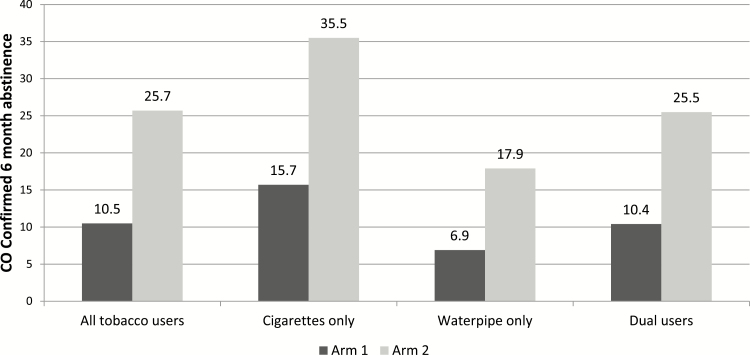
Figure 1 shows the CO-validated abstinence rate at 6 months by study ARM and by the type of smoker self-reported at baseline. The overall abstinence rate was significantly higher in ARM 2 than in ARM 1 (25.7% vs. 10.5%, p < .001). When analyzed by type of smoker, cigarette smokers had higher quit rates than water pipe and dual users. However, the addition of VHW counseling (ARM 2) was associated with higher quit rates compared with 4As (ARM 1) alone for all smoker types.
Figure 1.
Carbon monoxide-confirmed abstinence at 6-month follow-up by study ARM and type of smoker (self-report at baseline).
Table 2 shows the multivariate analysis of the factors associated with CO-validated abstinence at 6 months. Smokers in ARM 2 had greater adjusted odds of abstinence than those in ARM 1 (adjusted odds ratio [AOR] = 2.96, 95% confidence interval [CI] = 1.78% to 4.92%), controlling for age, gender, education, marital status, occupation, and type of smoker. Older age was associated with greater likelihood of abstinence (AOR = 1.03, 95% CI = 1.02% to 1.04%). Compared with cigarette-only smokers, water pipe–only smokers (AOR = 0.4, 95% CI = 0.26% to 0.62%) and dual users (AOR = 0.62, 95% CI = 0.45% to 0.86%) were less likely to be abstinent. However, when we tested the interaction between type of smoker and ARM, it was not significant [F(2, 1631.447) = 0.146, p = .864] indicating, as illustrated in Figure 1, that although water pipe–only smokers and dual users were less likely to quit than cigarette-only smokers (main effect of type of smoker), the intervention was equally effective across all three types of smokers.
Table 2.
Multivariable Logistic Regression Model for Smoking Abstinence at 6-Month Follow-up
| Carbon monoxide–validated smoking abstinence at 6-month follow-up | |||
|---|---|---|---|
| AOR | 95% CI | p | |
| ARMa | |||
| ARM 1 | 1.00 | ||
| ARM 2 | 2.96 | 1.78% to 4.92% | <.001 |
| Age (y) | 1.03 | 1.02% to 1.04% | <.001 |
| Gender | |||
| Female | 1.00 | ||
| Male | 1.15 | 0.24% to 5.41% | .507 |
| Education attainment | |||
| Primary or less | 1.00 | ||
| Secondary school | 0.96 | 0.59% to 1.57% | .875 |
| High school | 0.80 | 0.45% to 1.40% | .434 |
| Vocational or advanced | 1.06 | 0.55% to 2.07% | .858 |
| Marital status | |||
| Married | 1.00 | ||
| Other | 1.24 | 0.74% to 2.07% | .412 |
| Occupation | |||
| Farmer/Fisherman | 1.00 | ||
| Government employee | 1.37 | 0.74% to 2.56% | .319 |
| Other | 0.99 | 0.68% to 1.45% | .977 |
| Type of smokerb | |||
| Cigarette-only smoker | 1.00 | ||
| Water pipe–only smoker | 0.40 | 0.26% to 0.62% | <.001 |
| Dual user | 0.62 | 0.45% to 0.86% | .004 |
AOR = adjusted odds ratio; CI = confidence interval.
aParticipants in ARM 1 received health care provider–delivered 4As; participants in ARM 2 4As plus a referral to village health workers for 3-session in-person cessation counseling.
bCigarette-only smokers reported cigarette smoking on “some days” or “every day” AND “not at all” for water pipe smoking; water pipe–only smokers reported water pipe use on “some days” or “every day” AND “not at all” for cigarette smoking; dual users reported “some days” or “every day” for both cigarette and water pipe smoking.
We conducted several sensitivity analyses that demonstrated similar odds of abstinence when comparing the two study conditions. With no covariates and no imputation, participants in ARM 2 had greater odds of abstinence than those in ARM 1 (odds ratio [OR] = 2.73). When each ARM 1 participant was optimally matched on covariates to an ARM 2 participant, participants in ARM 2 had greater odds of abstinence (OR = 2.77).39 When type of smoker was replaced with quantity of cigarette and water pipe smoking, participants in ARM 2 had greater odds of abstinence (OR = 2.95).
Discussion
This study demonstrated that the addition of multisession cessation counseling, delivered by a VHW, can enhance abstinence rates compared with health care provider advice and brief counseling alone. Quit rates associated with provider advice and brief counseling were comparable to a large literature demonstrating an effect for this intervention in promoting cessation.5
Our findings are also consistent with studies showing that multisession cessation counseling can increase quit rates beyond brief health care provider counseling5 and add to literature demonstrating that trained VHWs can effectively deliver preventive care, including smoking cessation interventions.21,23 In a pilot RCT conducted in India, Thankappan et al.40 found that physician’s 5A counseling, education materials, plus CHWs’ counseling resulted in higher 1-year saliva cotinine–validated smoking abstinence compared with physician’s 5A counseling plus education materials alone (AOR = 3.35, 95% CI = 1.82% to 6.18%). In another RCT, Louwagie et al.23 found that among current adult smokers who were newly diagnosed with tuberculosis in South Africa, brief motivational interviewing delivered by lay health care workers plus usual cessation care (tuberculosis nurses’ short standardized smoking cessation message) was associated with higher 6-month cessation rates than nurse counseling alone (21.5% vs. 9.3%, adjusted RR = 2.33, 95% CI = 1.11% to 4.90%).
A recent analysis of the affordability of evidence-based interventions that promote cessation concluded that brief health care provider advice and self-help materials were affordable for most LMICs, but that in-person counseling may not be affordable for low-income countries.5 However, a task shifting model, such as the one tested in this study, may overcome the cost barriers by integrating VHWs into the workflow for delivering TDT in both Vietnam and other LMICs. The model, similar to offering clinicians the option of referring patients to a state or national quitline, creates an opportunity for health care providers to delegate the more time-consuming role of offering multisession counseling. Studies have already demonstrated the cost-efficiency of using CHWs in delivering primary and secondary health care services.41 Therefore, training health care providers and VHWs to offer cessation counseling and providing support for these activities through evidence-based system changes (eg, referral systems, defining workflow, and team roles) and ongoing technical assistance may be a cost-effective strategy for rapid scale up of cessation interventions in LMICs.
Further research is needed to explore how a TDT referral program that includes VHWs can optimize reach and be successfully sustained overtime. Moreover, with WHO promoting quitlines globally, as well as integration of quitline referral systems into health care settings, it is important to analyze how the model tested in this study compares to one in which providers are referring patients to a national quitline. Vietnam implemented a national quitline in September 2015. Research that compares the reach and effectiveness of integrating VHWs and quitlines as referral resources into health care systems may help inform allocation of resources and delineate the potential advantages of continuing to finance a VHW-driven program.
Water pipe use was prevalent in this study population. This may be related to the rural setting where, in Vietnam, water pipe use is higher.1 Despite the growth in water pipe use globally, there is a lack of data on effective cessation interventions.24 A recent systematic review that included five RCTs found an overall lack of evidence for most interventions.
Overall, we found that quit rates among water pipe users and dual users were lower than those of cigarette smokers. This may, in part, be due to training curriculum and use of a cessation counseling manual that was adapted from standard counseling approaches for helping cigarette smokers quit. However, when analyzing the intervention by smoker type, the findings suggest that VHW-led in-person multicessation counseling plus brief health care provider counseling may be more effective among water pipe/dual users compared with provider brief counseling alone. It is not clear what degree of tailoring is needed; however, given the vastly different sociocultural dimensions of water pipe use, research is needed to explore the value of further tailor interventions to optimize quit rates for water pipe users.
Our finding of lower quit rates among water pipe users may also be affected by a broader tobacco control policy environment in Vietnam that is focused exclusively on reducing cigarette smoking (ie, counteradvertising, tax- and smoke-free air policies). As a backdrop to health care system interventions, these policies and programs work synergistically to increase quit rates.42 There is a need to develop similarly effective policies and programs (eg, social marketing campaigns) that target water pipe use in addition to cigarette smoking.
This study has several limitations. First, our trial was conducted in a rural region in Vietnam and included only eight female smokers, reflecting the very low smoking rate among women. Therefore, findings may not be generalized to smokers living in the urban areas and female smokers. Second, the intervention was adapted from evidence-based approaches for increasing cessation among cigarette smokers, and therefore may not have addressed factors that perpetuate water pipe use. Third, although 6 months is an accepted timeframe for assessing abstinence in clinical trials, an additional measure at 12 months would have addressed duration of effect. Fourth, the intervention did not specifically address the role gender norms may continue to play in promoting and sustaining tobacco use among men in LMICs such as Vietnam, or how these norms may vary by type of tobacco used.43,44 This deserves further study. Finally, due to the quasiexperimental design, the population studied may have had differences that affected quit rates. However, several sensitivity analyses, including an unadjusted estimate with no imputation, optimal matching, and alternative covariates to characterize cigarette and water pipe quantity at baseline, yielded very similar estimates of the effect of VHWs’ multisession cessation counseling on smoking abstinence.
Despite the limitations, our findings suggest that VHWs represent a sustainable resource for ensuring widespread access to effective cessation services in Vietnam and other LMICs that integrate a VHW workforce into public health care programs.
Conclusion
Our findings support a team approach in TDT that offers a referral system in health care settings for providers to refer smokers to VHW-led smoking cessation counseling. The integration of VHWs in TDT programs represents a promising and potentially scalable model for increasing access to evidence-based cessation treatment and increasing quit rates in LMICs. Additional efforts are needed to ensure that TDT programs are designed to effectively address the use of a full range of tobacco products rather than focusing on cigarette smoking exclusively.
Funding
This work was supported by a grant from the National Institute of Cancer (R01CA175329).
Declaration of Interests
All authors declare that they have no conflicts of interest.
References
- 1. Van Minh H, Giang KB, Ngoc NB, et al. Prevalence of tobacco smoking in Vietnam: findings from the Global Adult Tobacco Survey 2015. Int J Public Health. 2017;62 (suppl 1):121–129. [DOI] [PubMed] [Google Scholar]
- 2. GATS. Global Adult Tobacco Fact Sheet: Viet Nam 2015. http://www.who.int/tobacco/surveillance/survey/gats/VN-2015_FactSheet_Standalone_E_Oct2016.pdf?ua=1. Accessed January 13, 2017. [Google Scholar]
- 3. Morrow M, Ngoc DH, Hoang TT, Trinh TH. Smoking and young women in Vietnam: the influence of normative gender roles. Soc Sci Med. 2002;55(4):681–690. [DOI] [PubMed] [Google Scholar]
- 4. World Health Organization. Guidelines for Implementation of Article 14 of the WHO Framework: Demand Reduction Measures Concerning Tobacco Dependence and Cessation. 2017. http://www.who.int/fctc/Guidelines.pdf?ua=1. Accessed January 15, 2017. [Google Scholar]
- 5. West R, Raw M, McNeill A, et al. Health-care interventions to promote and assist tobacco cessation: a review of efficacy, effectiveness and affordability for use in national guideline development. Addiction. 2015;110(9):1388–1403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Nilan K, Raw M, McKeever TM, Murray RL, McNeill A. Progress in implementation of WHO FCTC Article 14 and its guidelines: a survey of tobacco dependence treatment provision in 142 countries. Addiction. 2017;112(11):2023–2031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Papadakis S, McDonald P, Mullen KA, Reid R, Skulsky K, Pipe A. Strategies to increase the delivery of smoking cessation treatments in primary care settings: a systematic review and meta-analysis. Prev Med. 2010;51(3–4):199–213. [DOI] [PubMed] [Google Scholar]
- 8. Waltz TJ, Powell BJ, Matthieu MM, et al. Use of concept mapping to characterize relationships among implementation strategies and assess their feasibility and importance: results from the Expert Recommendations for Implementing Change (ERIC) study. Implement Sci. 2015;10:109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Shelley D, Cantrell J. The effect of linking community health centers to a state-level smoker’s quitline on rates of cessation assistance. BMC Health Serv Res. 2010;10:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sheffer MA, Baker TB, Fraser DL, Adsit RT, McAfee TA, Fiore MC. Fax referrals, academic detailing, and tobacco quitline use: a randomized trial. Am J Prev Med. 2012;42(1):21–28. [DOI] [PubMed] [Google Scholar]
- 11. Bentz CJ, Bayley KB, Bonin KE, et al. Provider feedback to improve 5A’s tobacco cessation in primary care: a cluster randomized clinical trial. Nicotine Tob Res. 2007;9(3):341–349. [DOI] [PubMed] [Google Scholar]
- 12. McRobbie H, Raw M, Chan S. Research priorities for article 14–demand reduction measures concerning tobacco dependence and cessation. Nicotine Tob Res. 2013;15(4):805–816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Singh P, Chokshi DA. Community health workers—a local solution to a global problem. N Engl J Med. 2013;369(10):894–896. [DOI] [PubMed] [Google Scholar]
- 14. Program for Appropriate Technology in Health (PATH). Promoting Household Water Treatment Through Local Health Workers in Vietnam. 2011. https://www.path.org/publications/files/CP_vietnam_hwts_pilot_fs.pdf. Accessed January 24, 2017. [Google Scholar]
- 15. Bittencourt L, Scarinci IC. Is there a role for community health workers in tobacco cessation programs? Perceptions of administrators and health care professionals. Nicotine Tob Res. 2014;16(5):626–631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wewers ME, Shoben A, Conroy S, et al. Effectiveness of two community health worker models of tobacco dependence treatment among community residents of Ohio Appalachia. Nicotine Tob Res. 2017;19(12):1499–1507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Landers SJ, Stover GN. Community health workers—practice and promise. Am J Public Health. 2011;101(12):2198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Balcázar HG, de Heer HD. Community health workers as partners in the management of non-communicable diseases. Lancet Glob Health. 2015;3(9):e508–e509. [DOI] [PubMed] [Google Scholar]
- 19. Ogedegbe G, Gyamfi J, Plange-Rhule J, et al. Task shifting interventions for cardiovascular risk reduction in low-income and middle-income countries: a systematic review of randomised controlled trials. BMJ Open. 2014;4(10):e005983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Rosenthal EL, Brownstein JN, Rush CH, et al. Community health workers: part of the solution. Health Aff (Millwood). 2010;29(7):1338–1342. [DOI] [PubMed] [Google Scholar]
- 21. Jeet G, Thakur JS, Prinja S, Singh M. Community health workers for non-communicable diseases prevention and control in developing countries: evidence and implications. PLoS One. 2017;12(7):e0180640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Jayakrishnan R, Uutela A, Mathew A, Auvinen A, Mathew PS, Sebastian P. Smoking cessation intervention in rural Kerala, India: findings of a randomised controlled trial. Asian Pac J Cancer Prev. 2013;14(11):6797–6802. [DOI] [PubMed] [Google Scholar]
- 23. Louwagie GM, Okuyemi KS, Ayo-Yusuf OA. Efficacy of brief motivational interviewing on smoking cessation at tuberculosis clinics in Tshwane, South Africa: a randomized controlled trial. Addiction. 2014;109(11):1942–1952. [DOI] [PubMed] [Google Scholar]
- 24. Maziak W, Jawad M, Jawad S, et al. Interventions for waterpipe smoking cessation. Cochrane Database Syst Rev. 2016;(7):CD005549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Tobacco Use and Dependence Guideline Panel. Treating Tobacco Use and Dependence: 2008 Update. Rockville, MD: US Department of Health and Human Services, Public Health Service; 2008. [Google Scholar]
- 26. Holtrop JS, Dosh SA, Torres T, Thum YM. The community health educator referral liaison (CHERL): a primary care practice role for promoting healthy behaviors. Am J Prev Med. 2008;35 (5 suppl):S365–S372. [DOI] [PubMed] [Google Scholar]
- 27. Brownstein JN, Chowdhury FM, Norris SL, et al. Effectiveness of community health workers in the care of people with hypertension. Am J Prev Med. 2007;32(5):435–447. [DOI] [PubMed] [Google Scholar]
- 28. Shelley D, VanDevanter N, Cleland CC, Nguyen L, Nguyen N. Implementing tobacco use treatment guidelines in community health centers in Vietnam. Implement Sci. 2015;10:142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hughes JR, Keely JP, Niaura RS, Ossip-Klein DJ, Richmond RL, Swan GE. Measures of abstinence in clinical trials: issues and recommendations. Nicotine Tob Res. 2003;5(1):13–25. [PubMed] [Google Scholar]
- 30. World Health Organization. Strengthening health systems for treating tobacco dependence in primary care: Building Capacity for Tobacco Control: Training Package. 2013. http://www.who.int/tobacco/publications/building_capacity/training_package/treatingtobaccodependence/en/. Accessed January 3, 2018. [Google Scholar]
- 31. Association for the Treatment of Tobacco Use and Dependence 2018. https://www.attud.org/. Accessed January 3, 2018.
- 32. Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211. [Google Scholar]
- 33. Hettema J, Steele J, Miller WR. Motivational interviewing. Annu Rev Clin Psychol. 2005;1:91–111. [DOI] [PubMed] [Google Scholar]
- 34. Shelley D, Nguyen L, Pham H, VanDevanter N, Nguyen N. Barriers and facilitators to expanding the role of community health workers to include smoking cessation services in Vietnam: a qualitative analysis. BMC Health Serv Res. 2014;14:606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Stroup WW. Generalized Linear Mixed Models: Modern Concepts, Methods and Applications. CRC Press; 2012. [Google Scholar]
- 36. The R Foundation. R: The R Project for Statistical Computing. Vienna, Austria; 2018. https://www.R-project.org/. Accessed October 15, 2018.
- 37. van Buuren S. Flexible Imputation of Missing Data. Boca Raton, FL: Chapman and Hall/CRC; 2012. [Google Scholar]
- 38. van Buuren S, Groothuis-Oudshoorn K. Mice: multivariate imputation by chained equations in R. J Stat Software. 2011;45(3):1–67. [Google Scholar]
- 39. Hansen BB, Klopfer SO. Optimal full matching and related designs via network flows. J Comput Graph Stat. 2006;15(3):609–627. [Google Scholar]
- 40. Thankappan KR, Mini GK, Hariharan M, Vijayakumar G, Sarma PS, Nichter M. Smoking cessation among diabetic patients in Kerala, India: 1-year follow-up results from a pilot randomized controlled trial. Diabetes Care. 2014;37(12):e256–e257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Viswanathan M, Kraschnewski J, Nishikawa B, et al. Outcomes of Community Health Worker Interventions. Evidence Report/Technology Assessment No. 181. AHRQ Publication No. 09-E014. Rockville: MD: Agency for Healthcare Research and Quality; 2009. [PMC free article] [PubMed] [Google Scholar]
- 42. Centers for Disease Control and Prevention. Best Practices for Comprehensive Tobacco Control Programs—2014. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. [Google Scholar]
- 43. Mahalik JR, Burns SM, Syzdek M. Masculinity and perceived normative health behaviors as predictors of men’s health behaviors. Soc Sci Med. 2007;64(11):2201–2209. [DOI] [PubMed] [Google Scholar]
- 44. Ng N, Weinehall L, Ohman A. “If I don’t smoke, I’m not a real man”—Indonesian teenage boys’ views about smoking. Health Educ Res. 2007;22(6):794–804. [DOI] [PubMed] [Google Scholar]