Abstract
Study Objectives
To document trends in self-reported sleep duration for the noninstitutionalized U.S. civilian population from 2004 to 2017 and examine how sleep trends vary by race/ethnicity.
Methods
We use data from the National Health Interview Survey (NHIS) for U.S. noninstitutionalized adults aged 18–84 from 2004 to 2017 (N = 398 382). NHIS respondents were asked how much they slept in a 24-hour period on average, which we categorized as ≤6 hr (short sleep), 7–8 hr (adequate sleep), and ≥9 hr (long sleep). We used multinomial logistic regression models to examine trends in self-reported sleep duration and assess race/ethnic differences in these trends. Our models statistically adjusted for demographic, socioeconomic, familial, behavioral, and health covariates.
Results
The prevalence of short sleep duration was relatively stable from 2004 to 2012. However, results from multinomial logistic regression models indicated that there was an increasing trend toward short sleep beginning in 2013 (b: 0.09, 95% CI: 0.05–0.14) that continued through 2017 (b: 0.18, 95% CI: 0.13–0.23). This trend was significantly more pronounced among Hispanics and non-Hispanic blacks, which resulted in widening racial/ethnic differences in reports of short sleep.
Conclusions
Recent increases in reports of short sleep are concerning as short sleep has been linked with a number of adverse health outcomes in the population. Moreover, growing race/ethnic disparities in short sleep may have consequences for racial and ethnic health disparities.
Keywords: sleep duration, trends, race/ethnicity, disparities, sleep
Statement of Significance
Inadequate sleep remains a public health concern. Recent social, economic, and technological changes may have increased the risk of inadequate sleep for the U.S. adult population and especially for racial/ethnic minorities. Using data from the 2004–2017 National Health Interview Survey, we document self-reported sleep duration trends for the U.S. adult population and by race/ethnicity after adjusting for demographic, socioeconomic, and behavioral health covariates. We find increasing reports of short sleep duration from 2013 to 2017 driven primarily by increasing short sleep among black and Hispanic adults. These trends are worrisome as they could exacerbate racial/ethnic health inequalities. Future research should examine how societal-level changes in the economy and technology are related to trends in short sleep duration among U.S. adults.
Introduction
Sufficient sleep is essential for daily functioning as well as physical and mental wellbeing. Short sleep duration, often defined as less than 7 hr, is associated with obesity [1], decreased cognitive functioning [2], dementia [3], heart disease [4], diabetes [5], and mortality [6, 7]. About one-third of Americans report experiencing short sleep according to estimates from the 2014 Behavioral Risk Factor Surveillance System [8]. The importance of sleep for health has generated considerable interest in determining if sleep duration has changed over time, but research findings have been mixed [9]. Studies using daily time use data document a decreasing prevalence of short sleep in the U.S. adult population from the 1980s to the mid-2000s [10], but also find an increase in short sleep among full-time workers [11]. Much of the research linking sleep to health is based on studies of self-reported habitual sleep duration. One study of self-reported sleep duration found a decline in sleep duration from the 1980s to the early 2000s, but very little change from 2004 to 2012 [12], whereas another study found an increase in short sleep among some workers between 2004 and 2007 [13]. Although one study using daily time diary data has reported an increase in sleep duration from 2003 to 2016 [14], trends in reported sleep since 2012 have yet to be examined.
Social, economic, and technological changes in recent years, however, may have resulted in a decline in sleep duration among U.S. adults. For example, the recent recession led to housing loss, increased financial stress [15, 16], and a restructured labor market that included more precarious work [17], factors which are associated with shorter sleep [18–20]. Additionally, there was a rapid rise in smart phones and tablets over this 5 yr period; the number of Americans with a smart phone increased from 35% in 2011 to 77% in 2016 [21]. Americans now spend more time looking at a screen, and, due to the mobile nature of these devices, technology has increasingly entered the bedroom [22, 23]. Technology use, especially smart phones, has been linked to inadequate and poor sleep [24] as well as daytime sleepiness [25]. Finally, Americans have reported increased levels of extreme stress in recent years [26], and researchers have found a robust association between stress and poor sleep outcomes [27, 28]. These changes may have had consequences for recent secular trends in reported sleep duration and we expect that the reported prevalence of short sleep has increased in the population in recent years.
Importantly, these social, economic, and technological trends may disproportionately affect the sleep of racial/ethnic minority populations that are already at greater risk for short sleep [29]. Non-Hispanic black (hereafter black(s)) and Hispanic adults, for instance, tend to report shorter sleep than non-Hispanic white adults [30, 31] (hereafter white(s)) and these disparities may have widened following the recent recession, which had larger negative impacts on the economic wellbeing of black and Hispanic adults compared with their white counterparts [32]. Furthermore, racial and ethnic minorities are more likely to experience race-related discrimination and vigilance, which have been linked to poor sleep [33]. Although reports of generalized stress have increased among all U.S. adults, this is particularly true with respect to heightened stress due to police violence towards minorities [34], suggesting a potential race-based stressor for sleep. In addition, researchers have found that the negative influence of screen time on children’s sleep duration is significantly stronger among blacks and Hispanics [35]. Increasing use of mobile technology and social media could also differentially affect the sleep duration of racial and ethnic minority adults. Prior research using longitudinal data from the Alameda County Study found a much larger increase in reported short sleep duration among black and Hispanic adults compared with white adults from the 1960s through the 1990s [36]. We know little, however, about how reported sleep duration may have changed in more recent years across racial/ethnic groups in the United States.
This study examines trends in self-reported sleep duration from 2004 to 2017 and how these trends vary by race/ethnicity. Given recent major social, economic, and technological changes, we hypothesize that the proportion of U.S. adults reporting short sleep has increased since 2012, and that this increase has been larger for black and Hispanic adults.
Methods
Data
We used data from the National Health Interview Survey (NHIS) [37], a nationally representative sample of the noninstitutionalized U.S. population, that includes annual interviews from tens of thousands of Americans. To compare our results with prior studies [12] and to explicitly examine when, if at all, risk for short sleep increased, we used data from 2004 through 2017. After limiting the sample to adults aged 18–84 (NHIS top codes age at 85) who provided valid information regarding their sleep duration (just over 2% were missing data on sleep duration), the analytic sample consisted of 398 382 U.S. adults. We imputed the missing nonresponses (household income had the highest amount of item nonresponse at 9.0%) using the mi impute command with chained equations in Stata v15. We produced 20 datasets. The analyses were replicated across the 20 datasets using the mi estimate command.
Measures
To measure sleep duration, respondents in the NHIS were asked “On average, how many hours of sleep do you get in a 24-hour period?” with responses recorded to the nearest hour. We categorized sleep duration into 6 or fewer hours (1), 7 to 8 hr (2), and 9 or more hours (3), consistent with consensus recommendations provided by the American Academy of Sleep Medicine (AASM) and Sleep Research Society (SRS) [38]. We considered the sensitivity of this specification by further examining sleep duration using a more detailed five-category specification used in prior research [31]: 5 or fewer hours, 6 hr, 7 hr, 8 hr, and 9 or more hours. We also examined sleep duration using a continuous specification of hours of sleep. The substantive results of these alternative specifications were consistent with results that utilized the consensus recommendation and are presented in Supplementary Tables S3–S5 as well as Supplementary Figure S1.
We examined the relationship between sleep and survey year and determined that sleep duration changed in a nonlinear fashion over this 13 yr period. Therefore, we coded year as a categorical variable with 2004 as the referent. 2004 was the year that the NHIS began consistently asking about sleep duration and this approach is consistent with prior sleep research that used NHIS data [12]. To examine how sleep trends may differ by race/ethnicity, we categorized self-reported race/ethnicity as non-Hispanic white (referent), non-Hispanic black, Hispanic, and non-Hispanic other (hereafter other), and estimated models that included an interaction term between years and race/ethnicity.
In our multivariable models, we included covariates that may confound the relationship between survey years and sleep duration. The means and proportions of these covariates are presented in Supplementary Table S1. We included linear age [39] and quadratic age to account for the nonlinear relationship between age and sleep duration found in prior studies, current Census region of residence (Northeast, Midwest, South, and West), gender (male or female) [40], marital status [41] (married (referent), divorced/separated, widowed, and never married), and number of children [42]. Socioeconomic status included educational attainment (high school degree [referent], less than high school, some college, and college or more), annual household income (US$0–US$34 999 [referent], US$35 000–US$74 999, and ≥US$75 000), and employment status using a measure of the number of hours per week worked [43] (0 hr worked [referent], 0–39 hr worked, 40 hr worked, and 40 or more hours worked). Health behaviors and health outcomes included smoking [44] (never smokers [referent], former smokers, current someday smokers, and current everyday smokers); alcohol drinking behavior [45] (abstainers, former drinkers, and current drinkers), body mass index (BMI) calculated using self-reported indicators of weight and height [46] (normal weight [referent, BMI: 18.5–29.9], underweight [0–18.49], and obese [≥30]), self-reported health (fair or poor versus good, very good, or excellent), and psychological distress measured using the validated Kessler-6 scale (Cronbach’s alpha = 0.84).
Statistical approach
We began by estimating age-adjusted sleep duration by year from 2004 until 2017. Next, we estimated multinomial logistic regression models predicting sleep duration, with adequate sleep duration [38, 47] (7 to 8 hr) as the base category. These models adjusted for demographic characteristics, socioeconomic status, and health, and health behaviors. We then estimated models that included interaction terms between year and race/ethnicity to determine if trends in sleep duration varied by race/ethnicity. Our analyses accounted for the complex sampling design of the NHIS, and we provide the weighted estimates. Finally, we used the margins command in Stata to calculate marginal-predicted probabilities of short sleep by race/ethnicity at each survey year after adjustment for all covariates to assist with model interpretation.
Results
Table 1 shows the age-adjusted distribution of sleep duration (adjusted to the age distribution of 2004). The reported sleep duration distribution is remarkably consistent from 2004 to 2006, with about 28.6% of respondents sleeping 6 or fewer hours, about 63.0% sleeping 7 to 8 hr, and about 8.5% sleeping 9 or more hours. In 2007, the proportion of respondents who reported sleeping 6 or fewer hours of sleep declined slightly, while the proportion who reported sleeping 7 to 8 hr increased to 65.0%. The decline in short sleep duration in this period is not surprising given this was during the recession, when many Americans lost their jobs and had more time to sleep [48, 49]. By 2010, the rate of short sleep largely stabilized to levels seen prior to 2007. In 2013, however, the proportion of respondents who reported sleeping, on average, 6 or fewer hours increased to 30.9% while the proportion who reported sleeping 7 to 8 hours declined to 60.8%. By 2017, almost 33.0% of respondents reported sleeping 6 or fewer hours, about 59.8% reported sleeping 7 to 8 hours, and 7.3% reported sleeping 9 or more hours. Although the absolute increases in short sleep duration are nontrivial (a 4% increase in short sleep duration among noninstitutionalized U.S. adults corresponds to more than 9 million American adults or the population size of New York City), the relative differences are stark, a 15% increase between 2004 and 2017 that was concentrated largely from 2013 to 2017.
Table 1.
Age-adjusted self-reported sleep duration, by year 2004–2017, National Health Interview Survey, sample adults aged 18–84
| Hours of sleep | ≤6 hr | 7–8 hr | ≥9 hr | N |
|---|---|---|---|---|
| 2004 | 28.6% | 62.9% | 8.5% | 29 949 |
| 2005 | 28.6% | 62.8% | 8.6% | 30 023 |
| 2006 | 28.7% | 63.0% | 8.3% | 23 121 |
| 2007 | 27.0% | 65.0% | 8.1% | 22 220 |
| 2008 | 28.5% | 62.8% | 8.7% | 20 810 |
| 2009 | 28.5% | 62.5% | 9.0% | 26 765 |
| 2010 | 28.9% | 61.8% | 9.3% | 26 058 |
| 2011 | 29.1% | 62.3% | 8.5% | 31 866 |
| 2012 | 29.3% | 62.4% | 8.4% | 33 108 |
| 2013 | 30.9% | 60.8% | 8.3% | 32 487 |
| 2014 | 30.9% | 61.1% | 8.0% | 34 517 |
| 2015 | 32.2% | 59.7% | 8.1% | 31 419 |
| 2016 | 32.5% | 60.4% | 7.2% | 30 997 |
| 2017 | 32.9% | 59.8% | 7.3% | 25 042 |
| N = 398 382 |
Source: National Health Interview Survey, 2004–2017.
Data are weighted to be representative of the U.S. population. Age distribution is adjusted to the 2004 age distribution in the U.S.
Table 2 provides log-odds from multinomial logistic models that predict sleep duration with adequate sleep (7 to 8 hr) as the base category. Importantly, these models are adjusted for demographic, behavioral health, health, familial, and socioeconomic factors. The full results, including controls, are presented in Supplementary Table S2. The results between 2004 and 2012 are consistent with prior research [12, 50]. Even with added statistical controls, there was little change in sleep duration from 2004 to 2012. We did, however, find a statistically significant increased risk for short sleep duration from 2013 to 2017 relative to 2004. We also examined the linear trend in sleep duration over time (results not shown) and found a statistically significant annual increase in reports of short sleep (b: 0.02, 95% CI: 0.02–0.02), corresponding to a roughly 2% increase (e.02) per year in the relative risk ratio of short sleep reports relative to normal duration sleep.
Table 2.
Log-odds from multinomial regression models predicting sleep duration, sample adults aged 18–84, National Health Interview Survey, 2004–2017
| ≤6 vs. 7–8 hr | ≥9 vs. 7–8 hr | |||||||
|---|---|---|---|---|---|---|---|---|
| b | P | 95% Confidence interval | b | P | 95% Confidence interval | |||
| Year | ||||||||
| 2004 (Ref) | ||||||||
| 2005 | 0.00 | −0.04 | 0.05 | 0.01 | −0.06 | 0.09 | ||
| 2006 | 0.00 | −0.05 | 0.05 | −0.01 | −0.10 | 0.08 | ||
| 2007 | −0.08 | −0.14 | −0.03 | −0.08 | −0.17 | 0.00 | ||
| 2008 | −0.03 | −0.08 | 0.03 | 0.00 | −0.08 | 0.08 | ||
| 2009 | −0.02 | −0.07 | 0.03 | 0.02 | −0.06 | 0.10 | ||
| 2010 | 0.01 | −0.03 | 0.06 | 0.08 | 0.00 | 0.16 | ||
| 2011 | 0.01 | −0.03 | 0.06 | −0.02 | −0.09 | 0.06 | ||
| 2012 | 0.05 | 0.00 | 0.10 | −0.01 | −0.09 | 0.07 | ||
| 2013 | 0.09 | *** | 0.05 | 0.14 | 0.00 | −0.08 | 0.07 | |
| 2014 | 0.11 | *** | 0.07 | 0.16 | −0.03 | −0.12 | 0.06 | |
| 2015 | 0.16 | *** | 0.12 | 0.21 | 0.01 | −0.07 | 0.09 | |
| 2016 | 0.17 | *** | 0.12 | 0.21 | −0.12 | *** | −0.21 | −0.04 |
| 2017 | 0.18 | *** | 0.13 | 0.23 | −0.08 | −0.16 | 0.01 | |
| Constant | −1.83 | *** | 1.93 | −1.73 | −1.19 | *** | −1.36 | −1.02 |
| N = 398 382 |
*p < 0.05; **p < 0.01; ***p < 0.001.
Source: National Health Interview Survey, 2004–2017.
Model includes controls for respondent: Age, Age2 Gender, Race/Ethnicity, Marital Status, Number of Children, Region of Residence, Smoking Status, Alcohol Consumption, Body Mass Index, Self-Reported Health, Kessler-6 Scale, Educational Attainment, Household Income, and Hours Worked Per Week. Full results are presented in Supplementary Table S2. Data are weighted to be representative of the U.S. Population.
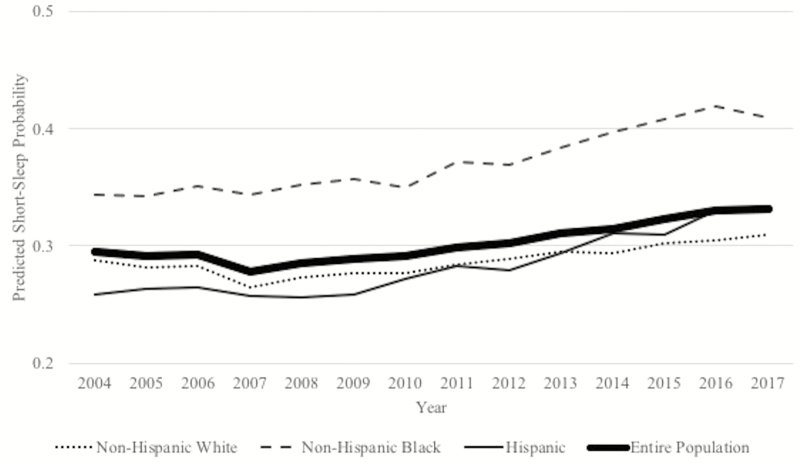
We next examined how sleep duration varied by race/ethnicity by interacting race/ethnicity and year. We present log-odds from the multinomial interaction models in Table 3 and the corresponding predicted marginal probabilities in Figure 1. For white adults, the probability of sleeping 6 or fewer hours declined from 2006 to 2007, and then slowly increased through 2017 to almost 31.0%, an absolute increase of about 2 percentage points from 2004. Black adults had higher probabilities of short sleep duration than white adults across the entire period; from 2004 to 2009, their probability of short sleep was around 35%, but after 2010, their probability of short sleep began to increase, reaching a high of 41.8% in 2016 and then slightly subsiding in 2017. As a result, by 2017 there was a 10-percentage point black-white difference, compared with a 5.6-percentage point difference in 2004. Conversely, Hispanic adults had a lower probability of short sleep duration than white adults in 2004 (25.9% versus 28.7%, respectively), but they experienced a marked increase in short sleep from 2009 to 2016 so that by 2017 they were slightly more likely than white adults to report short sleep (32.9% versus 30.9%). We also examined the change in short sleep duration relative to 2004 for each race/ethnic group in order to illustrate the relative amount of change that occurred over time for each group and we show this in Supplementary Figure S2.
Table 3.
Log-odds from multinomial regression models predicting sleep duration, with race/ethnicity × year interaction, sample adults aged 18–84, National Health Interview Survey, 2004–2017
| ≤6 vs. 7–8 hr | ≥9 vs. 7–8 hr | |||||||
|---|---|---|---|---|---|---|---|---|
| b | P | 95% Confidence interval | b | P | 95% Confidence interval | |||
| Year | ||||||||
| 2004 (Ref) | ||||||||
| 2005 | −0.01 | −0.06 | 0.05 | 0.01 | −0.08 | 0.11 | ||
| 2006 | −0.01 | −0.07 | 0.05 | 0.03 | −0.08 | 0.13 | ||
| 2007 | −0.10 | ** | −0.17 | −0.03 | −0.08 | −0.19 | 0.02 | |
| 2008 | −0.04 | −0.10 | 0.03 | 0.02 | −0.08 | 0.12 | ||
| 2009 | −0.04 | −0.10 | 0.02 | 0.06 | −0.04 | 0.16 | ||
| 2010 | −0.01 | −0.06 | 0.05 | 0.12 | * | 0.02 | 0.22 | |
| 2011 | −0.01 | −0.07 | 0.04 | 0.02 | −0.07 | 0.11 | ||
| 2012 | 0.04 | −0.02 | 0.10 | 0.05 | −0.06 | 0.15 | ||
| 2013 | 0.06 | * | 0.00 | 0.12 | 0.03 | −0.07 | 0.13 | |
| 2014 | 0.06 | * | 0.00 | 0.12 | 0.02 | −0.09 | 0.14 | |
| 2015 | 0.12 | *** | 0.06 | 0.18 | 0.09 | −0.01 | 0.19 | |
| 2016 | 0.13 | *** | 0.07 | 0.19 | −0.07 | −0.17 | 0.02 | |
| 2017 | 0.14 | *** | 0.09 | 0.20 | −0.03 | −0.13 | 0.07 | |
| Race/Ethnicity | ||||||||
| Non-Hispanic white (Ref) | ||||||||
| Non-Hispanic black | 0.33 | *** | 0.24 | 0.43 | 0.33 | *** | 0.16 | 0.49 |
| Hispanic | −0.11 | * | −0.21 | −0.02 | 0.06 | −0.06 | 0.19 | |
| Year × Non-Hispanic black | ||||||||
| 2005 × Non-Hispanic black | 0.03 | −0.09 | 0.16 | −0.02 | −0.24 | 0.21 | ||
| 2006 × Non-Hispanic black | 0.03 | −0.11 | 0.18 | −0.15 | −0.39 | 0.09 | ||
| 2007 × Non-Hispanic black | 0.07 | −0.09 | 0.22 | 0.05 | −0.14 | 0.25 | ||
| 2008 × Non-Hispanic black | 0.10 | −0.05 | 0.24 | −0.12 | −0.36 | 0.13 | ||
| 2009 × Non-Hispanic black | 0.10 | −0.04 | 0.25 | −0.11 | −0.35 | 0.12 | ||
| 2010 × Non-Hispanic black | 0.08 | −0.06 | 0.21 | −0.13 | −0.34 | 0.09 | ||
| 2011 × Non-Hispanic black | 0.13 | 0.00 | 0.26 | −0.23 | * | −0.44 | −0.02 | |
| 2012 × Non-Hispanic black | 0.05 | −0.08 | 0.19 | −0.30 | * | −0.52 | −0.07 | |
| 2013 × Non-Hispanic black | 0.19 | ** | 0.05 | 0.32 | −0.05 | −0.27 | 0.17 | |
| 2014 × Non-Hispanic black | 0.21 | *** | 0.07 | 0.34 | −0.14 | −0.38 | 0.10 | |
| 2015 × Non-Hispanic black | 0.18 | ** | 0.04 | 0.31 | −0.26 | * | −0.49 | −0.02 |
| 2016 × Non-Hispanic black | 0.15 | * | 0.00 | 0.29 | −0.12 | −0.37 | 0.14 | |
| 2017 × Non-Hispanic black | 0.08 | −0.07 | 0.24 | −0.27 | −0.54 | 0.01 | ||
| Year × Hispanic | ||||||||
| 2005 × Hispanic | 0.02 | −0.11 | 0.15 | −0.05 | −0.23 | 0.12 | ||
| 2006 × Hispanic | 0.02 | −0.12 | 0.17 | −0.19 | −0.40 | 0.02 | ||
| 2007 × Hispanic | 0.10 | −0.05 | 0.25 | −0.02 | −0.21 | 0.18 | ||
| 2008 × Hispanic | 0.02 | −0.12 | 0.17 | −0.07 | −0.28 | 0.15 | ||
| 2009 × Hispanic | 0.05 | −0.08 | 0.18 | −0.09 | −0.28 | 0.11 | ||
| 2010 × Hispanic | 0.08 | −0.05 | 0.20 | −0.13 | −0.32 | 0.06 | ||
| 2011 × Hispanic | 0.11 | −0.02 | 0.24 | 0.03 | −0.16 | 0.22 | ||
| 2012 × Hispanic | 0.03 | −0.09 | 0.16 | −0.10 | −0.29 | 0.10 | ||
| 2013 × Hispanic | 0.10 | −0.03 | 0.23 | −0.12 | −0.33 | 0.08 | ||
| 2014 × Hispanic | 0.21 | *** | 0.08 | 0.34 | −0.20 | −0.40 | 0.01 | |
| 2015 × Hispanic | 0.15 | * | 0.02 | 0.28 | −0.17 | −0.37 | 0.03 | |
| 2016 × Hispanic | 0.14 | −0.01 | 0.29 | −0.25 | * | −0.50 | 0.00 | |
| 2017 × Hispanic | 0.21 | *** | 0.07 | 0.36 | −0.06 | −0.30 | 0.19 | |
| Constant | −1.80 | *** | −1.90 | −1.70 | 1.22 | *** | −1.40 | −1.05 |
| N = 398 382 |
*p < 0.05; **p < 0.01; ***p < 0.001.
Source: National Health Interview Survey, 2004–2017.
Model includes controls for respondent: Age, Age2 Gender, Race/Ethnicity, Marital Status, Number of Children, Region of Residence, Smoking Status, Alcohol Consumption, Body Mass Index, Self-Reported Health, Kessler-6 Scale, Educational Attainment, Household Income, and Hours Worked Per Week. Data are weighted to be representative of the population.
Figure 1.
Marginal predicted probability of sleeping 6 or fewer hours per 24 hr, by race/ethnicity. Americans aged 18–84, National Health Interview Survey, 2004–2017. Calculated marginal-predicted probability based on fully adjusted model.
Discussion
Our findings indicate that there has been an increase in the prevalence of U.S. adults who report sleeping 6 or fewer hours in recent years. Fully one-third of U.S. adults reported short sleep in 2017, representing a 15% increase since 2004. Consistent with prior research [12, 13, 50], we found no evidence of change in short sleep from 2004 to 2012, but by extending the analysis of sleep duration trends through 2017, we observed an increase in short sleep beginning in 2013. The increase we observed corresponds to a period of economic instability, a rise in societal stress [26], and greater use of technology, such as smartphones, that have been shown to affect sleep [21].
Alarmingly, we found the largest increases in short sleep duration were concentrated among black and Hispanic adults. The probabilities of short sleep increased 6.5 percentage points between 2004 and 2017 for blacks and 7 percentage points for Hispanics, compared with an increase of only two percentage points among whites. Race/ethnic differences in sleep duration were not explained by markers of social advantage, such as income and education, or differences in physical and mental health. Previous research has found higher odds of short sleep for black and Hispanic adults compared with white adults [30, 31], and we show that these inequalities are widening, which is consistent with other recent research on sleep duration trends [14]. Growing race/ethnic inequalities in sleep duration are concerning as they could worsen already large and persistent race/ethnic health disparities [51, 52].
There is relatively limited research on sleep duration trends in the U.S. population and few studies with which we can compare our results. We replicated findings from previous research on reported sleep duration in the NHIS that found no change in sleep duration between 2004 and 2012 [12, 13]. Our findings suggest that the increasing risk of short sleep duration has emerged relatively recently and thus would not have been observed in these prior studies. This contrasts with a recent study using American Time Use Survey (ATUS) data that examined sleep duration trends from 2003 through 2016 and reported a total increase in daily sleep duration of about 19 min on weekdays and 10 min on weekends [14]. It is unclear, however, if the increase reflects additional time spent sleeping or more time spent in bed [53]. ATUS interviewers are instructed to code up to 30 min after respondents say they went to bed as time spent sleeping, though some of this time was most likely spent trying to fall asleep [54]. This may be one of the reasons our findings differ from those published using ATUS data. Our results may also differ if self-reported sleep duration captures quality as well as quantity of sleep. For instance, Americans may be sleeping the same amount, but if their sleep quality has declined in recent years, they may feel that they are getting less sleep. Nevertheless, prior research documenting the adverse health consequences of sleep at the population level has largely relied on studies using self-reported sleep measures [55], including the NHIS [56, 57], and evidence of increasing reports of short sleep in the population may have implications for population health trends.
There are important limitations to this study. First, we relied on self-reports of habitual sleep duration, which tend to overestimate sleep time relative to more objective measures of sleep such as actigraphy and polysomnography [58–60] and underestimate sleep time relative to measures of sleep duration obtained from time use studies [61]. Although measurement bias in the NHIS sleep measure may have changed over time, it is unlikely there was a sudden shift in the later years that would account for the increase in short sleep observed in recent years. Importantly, white adults tend to overestimate their sleep time to a greater extent than black adults [59], which may explain some of the race gap in sleep duration. However, race differences in reporting bias were unlikely to have shifted substantially after 2012 when the race gap in sleep duration began to widen. Furthermore, we also found an increasing gap between whites and Hispanics, a population that overestimates their sleep duration at similar levels to whites [59].
There are several sources of potential measurement error in the NHIS sleep duration measure. For instance, respondents tend to round sleep to the nearest hour when asked to report on the typical amount of sleep they get, which can result in a loss of precision, with prior research finding a tendency to heap responses at 6, 7, and 8 hr of sleep [62]. Sleep duration in the NHIS is rounded to the nearest hour, for all respondents, which may exacerbate this loss of precision. In addition, NHIS asks a single question about one’s average sleep duration in a 24 hr period and does not distinguish between weekday and weekend sleep, which has been shown to vary substantially [14, 62] in time use studies. Finally, the context of the survey can introduce social desirability bias in respondent sleep reports. Prior research suggests that respondents would be embarrassed to report inadequate sleep in a survey of health [62]; thus, sleep duration may be overestimated in the NHIS.
Although we included a number of controls for social, economic, household, and health characteristics in multivariable analysis, we could not account for other important factors associated with sleep such as the use of sleep medications, screen time, media consumption around bedtime, or everyday stressors that may have shifted over time. And although we note that the recent increase in short sleep coincides with a period of economic instability following the recent recession, as well as a rise in use of technology near bedtime, we did not investigate these factors directly. Nevertheless, our findings of an increasing trend in short sleep duration in the population in recent years suggest there that have been important macro-level changes that should be investigated.
Discrepant findings across major national studies utilizing different measures of sleep make it difficult to determine the direction and magnitude of change in sleep duration across the U.S. population. With improvements to the accessibility and cost of sleep-tracking technology, such as wearable devices, national surveys can conduct additional studies to investigate potential sources of error in their sleep measures. Calibration across measures derived from respondent reports and actigraphy, for instance, could be used to determine if trends in sleep duration reflect actual change, change in perception, or merely measurement error. Furthermore, results could be calibrated more easily across studies if more objective sleep data, such as from actigraphy, were collected. However, data would need to be collected on a sufficiently large sample, so within-group differences could be examined.
This study highlights the importance of continued surveillance of population-level sleep trends among vulnerable populations, particularly following major social, economic, and technological changes. Much of the existing literature on sleep trends has not examined how sleep has changed across racial and ethnic groups [50, 58]. Our findings are the first to show increasing race/ethnic disparities in self-reported sleep duration. Because inadequate sleep is a proximate determinant of poor health [58], these trends may have important consequences for population health and race/ethnic health disparities.
Funding
We thank the National Institute of Aging grants (T32 AG000037 and R00 AG039528) for support, the University of Minnesota and Integrated Public Use Microdata Series (IPUMS) for making the NHIS data available to the public and two anonymous reviewers for their comments. The contents of this manuscript are solely the responsibility of the author and do not represent the views of the National Institute of Aging, the University of South Carolina, the University of Southern California or Arizona State University.
Conflict of interest statement. None declared.
Supplementary Material
Work Performed: Statistical analysis was performed at the University of Southern California. Drafting of Manuscript was conducted at each institution.
References
- 1. McAllister EJ, et al. Ten putative contributors to the obesity epidemic. Crit Rev Food Sci Nutr. 2009;49(10):868–913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kronholm E, et al. Self-reported sleep duration and cognitive functioning in the general population. J Sleep Res. 2009;18(4):436–446. [DOI] [PubMed] [Google Scholar]
- 3. Fetveit A, et al. Sleep duration during the 24-hour day is associated with the severity of dementia in nursing home patients. Int J Geriatr Psychiatry. 2006;21(10):945–950. [DOI] [PubMed] [Google Scholar]
- 4. Ayas NT, et al. A prospective study of sleep duration and coronary heart disease in women. Arch Intern Med. 2003;163(2):205–209. [DOI] [PubMed] [Google Scholar]
- 5. Cappuccio FP, et al. Quantity and quality of sleep and incidence of type 2 diabetes. Diabetes Care.. 2010;33(2): 414–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gallicchio L, et al. Sleep duration and mortality: a systematic review and meta-analysis. J Sleep Res. 2009;18(2):148–158. [DOI] [PubMed] [Google Scholar]
- 7. Ferrie JE, et al. A prospective study of change in sleep duration: associations with mortality in the Whitehall II cohort. Sleep. 2007;30(12):1659–1666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Liu Y. Prevalence of healthy sleep duration among adults—United States, 2014. MMWR Morb Mortal Wkly Rep.. 2016;65:137–141. [DOI] [PubMed] [Google Scholar]
- 9. Bin YS, et al. Secular trends in adult sleep duration: a systematic review. Sleep Med Rev. 2012;16(3):223–230. [DOI] [PubMed] [Google Scholar]
- 10. Bin YS, et al. Sleeping at the limits: the changing prevalence of short and long sleep durations in 10 countries. Am J Epidemiol. 2013;177(8):826–833. [DOI] [PubMed] [Google Scholar]
- 11. Knutson KL, et al. Trends in the prevalence of short sleepers in the USA: 1975–2006. Sleep. 2010;33(1):37–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ford ES, et al. Trends in self-reported sleep duration among US adults from 1985 to 2012. Sleep. 2015;38(5):829–832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Luckhaupt SE, et al. The prevalence of short sleep duration by industry and occupation in the National Health Interview Survey. Sleep. 2010;33(2):149–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Basner M, et al. Sleep duration in the United States 2003–2016: first signs of success in the fight against sleep deficiency? Sleep. 2018. https://doi.org/ 10.1093/sleep/zsy012 [DOI] [PubMed] [Google Scholar]
- 15. Riumallo-Herl C, et al. Job loss, wealth and depression during the Great Recession in the USA and Europe. Int J Epidemiol. 2014;43(5):1508–1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bell DN, et al. Young people and the Great Recession. Oxf Rev Econ Policy. 2011;27(2):241–267. [Google Scholar]
- 17. Elsby MW, et al. The Labor Market in the Great Recession. Cambridge, MA:National Bureau of Economic Research; 2010. [Google Scholar]
- 18. Perales F, et al. Losing ground, losing sleep: local economic conditions, economic vulnerability, and sleep. Soc Sci Res. 2017;62:189–203. [DOI] [PubMed] [Google Scholar]
- 19. Khubchandani J, et al. Association of job insecurity with health risk factors and poorer health in American workers. J Community Health. 2017;42(2):242–251. [DOI] [PubMed] [Google Scholar]
- 20. Cannuscio CC, et al. Housing strain, mortgage foreclosure, and health. Nurs Outlook. 2012;60(3):134–42, 142.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Pew Research Center. Mobile Fact Sheet; 2018. http://www.pewinternet.org/fact-sheet/mobile/ Accessed June 7, 2018.
- 22. Thomée S, et al. Computer use and stress, sleep disturbances, and symptoms of depression among young adults–a prospective cohort study. BMC Psychiatry. 2012;12(1):176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Neilson Company. The Total Auidence Report: Q1 2016; 2016. http://www.nielsen.com/us/en/insights/reports/2016/ the-total-audience-report-q1-2016.html?afflt= ntrt15340001&afflt_uid=kwPABJ3OSL4.ZbyiP71kgPIgRB_kBm8tRl7YyLCTSblb&afflt_uid_2=AFFLT_ID_2.
- 24. Chang AM, et al. Evening use of light-emitting eReaders negatively affects sleep, circadian timing, and next-morning alertness. Proc Natl Acad Sci U S A. 2015;112(4):1232–1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Carter B, et al. Association between portable screen-based media device access or use and sleep outcomes: a systematic review and meta-analysis. JAMA Pediatr. 2016;170(12):1202–1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. American Psychological Association. 2015 Stress in America https://www.apa.org/news/press/releases/stress/2015/snapshot.aspx. Accessed October 2018.
- 27. Akerstedt T, et al. Impaired sleep after bedtime stress and worries. Biol Psychol. 2007;76(3):170–173. [DOI] [PubMed] [Google Scholar]
- 28. Hall M, et al. Acute stress affects heart rate variability during sleep. Psychosom Med. 2004;66(1):56–62. [DOI] [PubMed] [Google Scholar]
- 29. Grandner MA, et al. Sleep disparity, race/ethnicity, and socioeconomic position. Sleep Med. 2016;18:7–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hale L, et al. Racial differences in self-reports of sleep duration in a population-based study. Sleep. 2007;30(9):1096–1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Krueger PM, et al. Sleep duration in the United States: a cross-sectional population-based study. Am J Epidemiol. 2009;169(9):1052–1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kochanek KD, et al. How did cause of death contribute to racial differences in life expectancy in the United States in 2010. NCHS Data Brief. 2013;125:1–8. [PubMed] [Google Scholar]
- 33. Hicken MT, et al. “Every shut eye, ain’t sleep”: the role of racism-related vigilance in racial/ethnic disparities in sleep difficulty. Race Soc Probl. 2013;5(2):100–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. American Psychological Association. Stress in America 2017 Snapshot: Coping with Change. Washington, DC: Author; https://www.apa.org/news/press/releases/stress/2016/coping-with-change.PDF. Accessed October 2018. [Google Scholar]
- 35. Falbe J, et al. Sleep duration, restfulness, and screens in the sleep environment. Pediatrics. 2015;135(2):e367–e375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Stamatakis KA, et al. Short sleep duration across income, education, and race/ethnic groups: population prevalence and growing disparities during 34 years of follow-up. Ann Epidemiol. 2007;17(12):948–955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Blewett LA, et al. IPUMS Health Surveys: National Health Interview Survey, Version 6.2. Minneapolis, MN: University of Minnesota; 2016. [Google Scholar]
- 38. Watson NF, et al. Recommended amount of sleep for a healthy adult: a joint consensus statement of the American Academy of Sleep Medicine and sleep research society. J Clin Sleep Med. 2015;11(6):591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Stephan Y, et al. Subjective age and sleep in middle-aged and older adults. Psychol Health. 2017; 32(9):1–12. [DOI] [PubMed] [Google Scholar]
- 40. Burgard SA, et al. Gender and time for sleep among U.S. Adults. Am Sociol Rev. 2013;78(1):51–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Chen JH, et al. Marriage, relationship quality, and sleep among U.S. Older adults. J Health Soc Behav. 2015;56(3):356–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Chapman DP, et al. Household demographics and perceived insufficient sleep among US adults. J Community Health. 2012;37(2):344–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Nakashima M, et al. Association between long working hours and sleep problems in white-collar workers. J Sleep Res. 2011;20(1 Pt 1):110–116. [DOI] [PubMed] [Google Scholar]
- 44. Stipelman BA, et al. The relationship among smoking, sleep, and chronic rheumatic conditions commonly associated with pain in the National Health Interview Survey. J Behav Med. 2013;36(5):539–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Ebrahim IO, et al. Alcohol and sleep I: effects on normal sleep. Alcohol Clin Exp Res. 2013;37(4):539–549. [DOI] [PubMed] [Google Scholar]
- 46. Meyer KA, et al. Sleep duration and BMI in a sample of young adults. Obesity (Silver Spring). 2012;20(6):1279–1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Hoffmann JP. Generalized Linear Models: An Applied Approach. Reading, MA:Addison-Wesley Longman; 2004. [Google Scholar]
- 48. Keyes KM, et al. The great sleep recession: changes in sleep duration among US adolescents, 1991–2012. Pediatrics. 2015;135(3):460–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Brochu P, et al. The ‘trendiness’ of sleep: an empirical investigation into the cyclical nature of sleep time. Empir Econ. 2012;43(2):891–913. [Google Scholar]
- 50. Youngstedt SD, et al. Has adult sleep duration declined over the last 50+ years? Sleep Med Rev. 2016;28:69–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Hummer RA, et al. Race/ethnicity and U.S. adult mortality: progress, prospects, and new analyses. Du Bois Rev. 2011;8(1):5–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Williams DR. Miles to go before we sleep: racial inequities in health. J Health Soc Behav. 2012;53(3):279–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Ogilvie RP, Patel SR. Changing national trends in sleep duration: did we make America sleep again? Sleep. 2018. https://doi.org/ 10.1093/sleep/zsy055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Bureau of Labor Statistics. American Time Use Survey, Frequently Asked Questions.2018. https://www.bls.gov/tus/atusfaqs.htm#36 Accessed October 2018.
- 55. Matricciani L, et al. Past, present, and future: trends in sleep duration and implications for public health. Sleep Health. 2017;3(5):317–323. [DOI] [PubMed] [Google Scholar]
- 56. Shankar A, et al. Sleep duration and self-rated health: the National Health Interview Survey 2008. Sleep. 2011;34(9):1173–1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Sabanayagam C, et al. Sleep duration and cardiovascular disease: results from the National Health Interview Survey. Sleep. 2010;33(8):1037–1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Lauderdale DS, et al. Sleep duration: how well do self-reports reflect objective measures? The CARDIA Sleep Study. Epidemiol Camb Mass. 2008;19(6):838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Jackson CL, et al. Agreement between self-reported and objectively measured sleep duration among white, black, Hispanic, and Chinese adults in the United States: multi-Ethnic Study of Atherosclerosis. Sleep. 2018. https://doi.org/ 10.1093/sleep/zsy057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Cespedes EM, et al. Comparison of self-reported sleep duration with actigraphy: results from the Hispanic community health study/study of Latinos sueño ancillary study. Am J Epidemiol. 2016;183(6): 561–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Miller CB, et al. Agreement between simple questions about sleep duration and sleep diaries in a large online survey. Sleep Health. 2015;1(2):133–137. [DOI] [PubMed] [Google Scholar]
- 62. Kaplan R, et al. Contrasting Stylized Questions of Sleep with Diary Measures from the American Time Use Survey. Washington, DC: Office of Survey Methods Research, Bureau of Labor Stratistics; 2018. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.