Abstract
Objective
Epilepsy management especially in developing country is challenging. Seizures recurrence can be caused by both drug and non-drug related problems such as inadequate antiepileptic regimens, adverse drug reaction and poor adherence. Patient treatment satisfaction also affects the treatment out comes by improving medication adherence. This study aimed to assess drug therapy problems (DTPs) and treatment satisfaction among ambulatory epileptic patients at Tikur Anbessa Specialized Hospital.
Methods
A prospective cross-sectional study was conducted on 291 epileptic patients. Data was collected through patient interview and medical charts review. DTPs were identified based on the standard treatment guidelines and Micromedex® was used as drug interaction checker. Cipolle DTPs classification was used to classify the DTPs and Treatment Satisfaction with Medicine Questionnaire (SATMED-Q) was used to assess treatment satisfaction. Binary logistic regressions were utilized to identify the associated factors.
Results
Phenobarbital 195 (67%) and phenytoin 97 (33.3%) were the most frequently prescribed antiepileptic medications as monotherapy or combination therapy. Only 54 (18.6%) of the study participants had controlled seizure. DTP was found in 205(70.4%) of the study participants. From 352 DTPs identified, adverse drug reaction 146 (41.5%) was the leading DTPs followed by ineffective drugs 98 (27.8%) drug interaction 45 (12.8%) and inappropriate dose 42(11.9%). Headache, depression and epigastric pain were frequently reported adverse drug reaction. Among the study participants 167 (57.3%) were adherent to their medications. The number of medications taken by the patients had significant association with occurrence of DTPs, whereas source of medication and seizure free periods were found to have significant association with poor adherence. The global patient satisfaction was (67.4%) and lower satisfaction rate was found with regard to impact on daily activities (62.0%), treatment effectiveness (64.7%) and medical care (65.9%).
Conclusion
Prevalence of DTPs among ambulatory epileptic patients was high and about half of the patients were nona-dherent for their medication. The overall treatment satisfaction of the patients was suboptimal.
Introduction
Epilepsy is a neurologic disorder characterized by an enduring predisposition to generate epileptic seizures [1]. In epilepsy treatment, the ultimate goal is to prevent seizure episode without side effects and having an optimal quality of life [2]. The management should therefore be individualized to eliminate or reduce seizure frequency, while avoiding drug-related harms and complications [3, 4]. However, about 90% of epileptic patients in developing countries are not receiving appropriate treatment due to cultural attitudes, lack of prioritization, poor health care system and inadequate supply of antiepileptic drugs (AEDs) [5]. Moreover, pharmacokinetics of most AEDs is complex, which makes dosing and monitoring very difficult. Complexity of medical problems and co-medications given with AEDs can increase drug-related problems (DRPs) & drug interactions, which can affect seizure control and toxicity [6]. Enzyme-inducing AEDs such as carbamazepine (CBZ) may accelerate the metabolism of many drugs including antiretroviral, anti-tuberculosis (anti-TB), and hormonal contraceptives thereby reducing their concentration by up to 50% [7].
DTP is any undesirable event experienced by a patient that involves or suspected to involve drug therapy, and that interferes with achieving the desired goals of therapy. An infinite number of DTPs exist because of rapidly expanding array of drugs available, increasing number of diseases being diagnosed and number of patients entering the healthcare system [8].
AEDs-related DTP studies are sparse in the literature. The studies so far made are either on utilization or adherence of AEDs. AEDs utilization study carried out in Bishoftu hospital, Ethiopia, identified under dosing (16.5%), incorrect duration (12.7%), and drug-drug interactions (5%) to be the major therapy related problems [9]. Non-adherence to medication accounts for substantial worsening of disease, death and increased health care costs [10]. Previous studies regarding AEDs adherence produced varied results. Adherence was higher in India (98.6%) [11] and Palestine (85.3%) [12]. It was relatively lower in China (51.9%) [13], Jimma hospital, Ethiopia (58.5%) [10] and the UK (59%) [14]. Moderate adherence was reported from the USA (71%) [15] and Gondar hospital, Ethiopia (70.8%) [16]. Several lines of evidence indicate that adherence to AEDs is suboptimal [17]. Collectively, these reports suggest that identification of common DTPs is an important component of drug therapy and contributes to reduction of drug-related morbidity and mortality.
Regarding consequences of low treatment satisfaction, one half of patients with chronic illness end up making medication related decisions without seeking medical advice, becoming non-adherent that may compromise the effectiveness of treatment. Furthermore, patients having better satisfaction on the treatment are more tend to adhere their medication and improve the treatment out comes [18].
Therefore, this study was carried out to determine the prevalence of DTPs and associated factors and treatment satisfaction among epileptic ambulatory patients in a tertiary care teaching hospital of Ethiopia.
Material and Methods
Study design and population
A prospective cross-sectional study was conducted among ambulatory epileptic patients at neurology clinic of Tikur Anbessa Specialized Hospital (TASH), which is the largest referral and teaching hospital in the country. Patients having epilepsy, had complete medical records and willing to participate in the study were included. Data were collected from 4th June to 28th August 12, 2017.
Sampling
Sample size was computed based on single population proportion formula. The total epileptic patients at TASH were 1100. Using correction formula, 291 patients were recruited by systematic random sampling. Pretest was conducted on 5% of the sample size to ensure relevance of the instruments and appropriate modifications were performed accordingly.
Data collection
Patient information was collected through interview and chart review by trained nurses and clinical pharmacists, respectively. The relevant information about each patient (demographic data, patients’ clinical characteristics and patients’ treatment satisfaction) was collected from patient interview following neurology clinic visit. Laboratory results, current medications and co-morbidities were collected from patients’ medical chart.
Appropriateness of medical therapy was evaluated using guidelines of National Institute for Health and Care Excellence, American Academy of Neurology, and Ethiopian treatment guideline for general hospitals 2014. Micromedex® (Micromedex 2.0. Truven Health Analytics Inc.) drug interaction checker was used to identify drug interactions and only absolute contraindications and major drug interactions were considered as significant interactions. The identified DTPs were classified using DTP registration format adopted from Cipolle et al. [16] with slight modification. Adherence was measured using Morisky Medication Adherence (Morisky Green Levine test[19] which is online available for free http://www.pmidcalc.org/?sid=3945130&newtest=Y). Patients’ treatment satisfaction was assessed by using treatment Satisfaction with Medicines Questionnaire (SATMED-Q) which is composed of 17 items investigating 6 dimensions (undesirable side effects, treatment effectiveness, convenience to use, impact on daily activity, medical care and global satisfaction.
Data analysis
Data were entered using Epi Info version 7.2.1 and analysed with Statistical Package for Social Science version 21. Descriptive statistics was used to summarize patients’ characteristics. Tables and charts were used to present the findings. Prevalence of DTP was calculated by dividing the number of patients who had at least one DTP with the study participants. Multivariable binary logistic regression analysis was used to assess association of the independent variables with DTPs and medication adherence after univariable analysis (p<0.2) to control confounders. P value < 0.05 was considered statistically significant. Regarding treatment satisfaction, the sum of the direct score of each dimension was changed to a more intuitive and easier to understand metric with a minimum of 0 and a maximum of 100%.
Ethics approval
The study was approved by Institutional Review Board of College of Health Sciences, Addis Ababa University (Protocol number = 002/17/SPharma). A written informed consent was obtained from all study participants before the data collection.
Results
Socio-demographic characteristics
The mean age was 30.2 ±11.4 years and about half of them 154(50.2%) were young adults. Majority of them were single 185(63.6%) and from Addis Ababa 238(81.1%). Around 105(36%) had secondary school education, while 16(5.5%) had no formal education. Almost half 140(48.1%) of the patients got their medication for free (Table 1).
Table 1. Socio demographic characteristics of epileptic patients attending at the neurology clinic of TASH, 2017.
| Variables | Number (n) | Percentage (%) | |
|---|---|---|---|
| Sex | Male | 154 | 52.9 |
| Female | 137 | 47.1 | |
| Age | Adolescent (<18) | 39 | 13.4 |
| Young adult (18–30) | 146 | 50.2 | |
| Adult (31–60) | 99 | 34.0 | |
| Elderly (>60) | 7 | 2.4 | |
| Marital status | Single | 185 | 63.6 |
| Married | 97 | 33.3 | |
| Divorced | 5 | 1.7 | |
| Widowed | 4 | 1.4 | |
| Residential area | Addis Ababa | 238 | 81.8 |
| Out of Addis Ababa | 53 | 18.2 | |
| Educational status | No formal | 16 | 5.5 |
| Primary | 88 | 30.2 | |
| Secondary | 105 | 36.1 | |
| Tertiary | 82 | 28.2 | |
| Occupation | Unemployed | 112 | 38.5 |
| Employed | 69 | 23.7 | |
| Private/ merchant | 49 | 16.8 | |
| Student | 50 | 17.2 | |
| Daily labourer | 2 | 0.7 | |
| Farmer | 6 | 2.1 | |
| Others* | 3 | 1.0 | |
| Source of medication | Free | 140 | 48.1 |
| Payment | 151 | 51.9 | |
* retired
Clinical characteristics
Generalized tonic clonic seizure (GTCS) was the commonest 193(66.3%) seizure type among the participants and 191(65.6%) had seizure free period less than a year. About 116(40%) had 1–5 seizure episodes per year and 35(12.7%) of them had more than ten seizure episode in the previous one year. Only 54 (18.6%) patients had controlled seizure (seizure free period of two years or longer). Almost a quarter (23.4%) of them had chronic comorbid conditions, HIV infection and hypertension being the commonest ones (Table 2).
Table 2. Clinical characteristics of epileptic patients attending at the neurology clinic of TASH, 2017.
| Variables | Number (n) | Percentage (%) | ||
|---|---|---|---|---|
| Types of seizure | Generalized seizure | 197 | 67.7 | |
| GTCS | 193 | 66.3 | ||
| Myoclonic | 3 | 1.0 | ||
| Absence | 1 | 0.3 | ||
| Partial seizure | 71 | 24.4 | ||
| Simple partial | 19 | 6.5 | ||
| Complex partial | 23 | 7.9 | ||
| Focal with secondary generalization | 29 | 10.0 | ||
| Unclassified* | 23 | 7.9 | ||
| Follow up years | < 2 years | 49 | 16.8 | |
| 2–5 years | 53 | 18.2 | ||
| 6–10 years | 69 | 23.7 | ||
| >10 years | 120 | 41.2 | ||
| Seizure free period | < 1 year | 191 | 65.6 | |
| 1–2 years | 46 | 15.8 | ||
| 2–5 years | 33 | 11.3 | ||
| >5 year | 21 | 7.7 | ||
| Number of seizure episode per year | None | 102 | 35.1 | |
| 1–5 | 120 | 41.2 | ||
| 6–10 | 32 | 11.0 | ||
| >10 | 37 | 12.7 | ||
| Co-morbid conditions | HIV | 20 | 6.9 | |
| CRVHD/CHF | 8 | 2.7 | ||
| Major depressive disorder | 10 | 3.4 | ||
| Migraine headache | 3 | 1.0 | ||
| Mental retardation | 5 | 1.7 | ||
| HTN | 12 | 4.1 | ||
| Stroke | 7 | 2.4 | ||
| Others | 14 | 4.8 | ||
“*Unclassified seizure”, a seizure which is diagnosed by the physician as “Epilepsy” or “seizure disorder”; GTCS, Generalized Tonic Clonic Seizure; HIV, human immune virus; CHF, Congestive Heart Failure; CRVHD, Chronic Rheumatic Valvular Heart Disease.
Pattern of antiepileptic drug use
Regarding AEDs use, monotherapy was the common (58.8%) mode of therapy and phenobarbital 93(32%) and phenytoin 32(92%) were the drug of choices. Dual and triple therapy accounted for 33.3% and 7.2%, respectively. Phenobarbital + phenytoin 30(10.3%), phenobarbital + carbamazepine 17(5.6%), and Phenobarbital + valproic acid 15(5.3%) were the most frequently used dual therapy regimen. One fourth (25.1%) of the study participants were taking more than two medications, with mean and SD of 2.03±1.27 medications per day (Table 3).
Table 3. Pattern of medication use among epileptic patients attending at the neurology clinic of TASH, 2017.
| Variables | Number (N) | Percentage (%) | |
|---|---|---|---|
| Number of AEDs used | One | 171 | 58.8 |
| Two | 97 | 33.3 | |
| Three | 21 | 7.2 | |
| Four | 2 | 0.7 | |
| AEDs use Pattern | PHB | 93 | 32.0 |
| PHT | 35 | 12.0 | |
| CBZ | 32 | 11.0 | |
| VPA | 17 | 5.8 | |
| LTG | 1 | 0.3 | |
| PHB+ PHT | 30 | 10.3 | |
| PHB+CBZ | 17 | 5.6 | |
| PHB+VPA | 15 | 5.2 | |
| PHB+LTG | 1 | 0.3 | |
| PHT+CBZ | 13 | 4.5 | |
| PHT+VPA | 9 | 3.1 | |
| CBZ+VPA | 7 | 2.4 | |
| PHB+PHT+CBZ | 4 | 1.4 | |
| CBZ+VPA+PHB | 4 | 1.4 | |
| PHB+PHT+VPA | 1 | 0.3 | |
| PHB+PHT+CLONA | 1 | 0.3 | |
| Others * | 11 | 3.8 | |
|
Total number of drugs (AEDs + others) |
1 | 120 | 41.2 |
| 2 | 97 | 33.3 | |
| >2 | 74 | 25.5 | |
Others *, different combination of the above AEDs including quadruple therapy; PHB, phenobarbital; PHT, phenytoin; CBZ, carbamazepine; VPA, Valproic acid; LTG, Lamotrigine; CLONA, Clonazepam.
Analysis of drug use based on seizure type revealed that while phenobarbital and phenytoin were frequently used for generalized seizure, carbamazepine and phenobarbital for partial seizure. Phenobarbital was also frequently used for unclassified seizure and the use of valproic acid for any seizure was low.
Drug therapy problems
A total of 352 DTPs were identified from 205 participants, giving rise to a prevalence of 70.4%. One DTP was identified in 102 (49.8%), 2 DTPs in 73 (35.6%) and >2 DTPs in 30 (14.6%) participants. Average number of DTPs per patient was 1.2 ± 0.4. Adverse drug reactions (ADRs) followed by inappropriate drug selection and drug interaction were the major DTPs found in the present study (Table 4). DTPs appeared to be common in patients with uncontrolled seizure (r = -0.264, P = 0.000). The proportion was 76% for uncontrolled and 52% for controlled seizure.
Table 4. Types of drug therapy problems identified from epileptic patients attending at the neurology clinic of TASH, 2017.
| DTPs | No. of DTPs | Total | (%) | |
|---|---|---|---|---|
| Drug interaction | 45 | 45 | 12.8 | |
| Adverse drug reaction | Undesired effect | 144 |
146 |
41.5 |
| Contraindications | 2 | |||
| Ineffective drugs | Inappropriate drug selection | 80 |
98 |
27.8 |
| Condition refractory to the drug | 18 | |||
| Need additional therapy | Untreated medical condition | 13 |
18 |
5.1 |
| Need synergistic/potentiating | 5 | |||
| Inappropriate dose | Dose too low | 24 |
42 |
11.9 |
| Dose too high | 18 | |||
| Unnecessary drug therapy | No medical indication | 2 |
3 |
0.9 |
|
Duplicate therapy |
1 |
|||
| Total | 352 | 100 |
DTP: Drug Therapy Problems
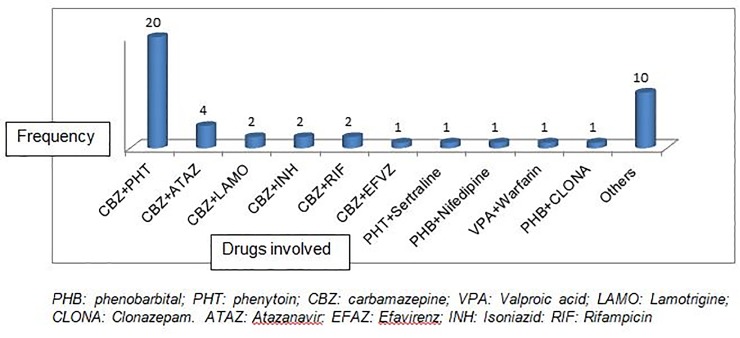
A total of 45 significant drug interactions were identified in 38 (13.1%) study participants and carbamazepine was the culprit in majority of the cases (Fig 1).
Fig 1. Type of drugs involved in drug interaction and their frequency.
One hundred forty four 144(49.5%) of the participants experienced at least one ADR that could possibly be associated with AEDs. Headache 39(13.4%), depression 36(12.4%), epigastric pain 35(12%), and hypersomnia 28(9.6%), were the top four ADRs reported.
Medication adherence and possible reasons for non-adherence
Adherence was found to be 55.7%. The major reason for poor adherence was forgetfulness followed by patient feeling as cured, medication unavailability, patient belief on drug effectiveness, fear of side effects, and switching to traditional medicines.
Predictors of occurrence of drug therapy problems
Number of medications was shown to be a risk factor for DTPs. Patients who were on more than 2 medications were 3.8 times more likely to develop DTPs as compared on single medication (AOR = 3.810 CI 1.409–10.30) (Table 5).
Table 5. Predictors of occurrence of drug therapy problems in epileptic patients attending at neurology clinic of TASH, 2017.
| Variables | category | DTPs (%) |
COR (95% CI) |
AOR (95% CI) |
P-Value | |
|---|---|---|---|---|---|---|
| Yes | No | |||||
| Gender | Male | 106(73.6) | 48(32.7) | 1.00 | 1.00 | |
| Female | 38(23.6) | 99(67.3) | 1.18(0.711–1.957) | 1.19(.667–2.13) | 0.552 | |
| Age | <18 | 33(16.1) | 6(7.0) | 1.00 | 1.00 | |
| 18–30 | 104(50.7) | 42(48.8) | 0.450(0.176–1.153) | 0.371(0.129–1.068 | 0.066 | |
| 30–60 | 65(31.7) | 34(39.5) | 0.348(0.133–0.911) | 0.256(0.089–0.790 | 0.057 | |
| >60 | 3(1.5) | 4(4.7) | 0.136(0.024–0.770) | 0.135(0.017–1.081 | 0.059 | |
| Number of medications | 1 | 73(35.6) | 47(54.7) | 1.00 | 1.00 | |
| 2 | 71(34.6) | 26(30.2) | 1.758(0.985–3.140) | 1.350(0.687–2.652) | 0.383 | |
| >2 | 61(29.8) | 13(15.1) | 3.273(1.594–6.719) | 3.810(1.409–10.30) | 0.008* | |
| Co-morbidities | No | 155(75.6) | 68(79.1) | 1.00 | 1.00 | |
| Yes | 50(24.4) | 18(20.9) | 1.22(0.662–2.242) | 1.475(0.286–1.607) | 0.378 | |
COR, crude odds ratio; AOR, adjusted odds ratio; CI, confidence interval
Predictors of non-adherence
Source of medication and seizure free period were shown to be predictors of non-adherence. The odds of being non-adherent was higher by 2.3 fold (AOR = 1.360–3.943) for patients getting medication for free than paying ones. Non-adherence significantly decreased by 64% and 54% in patients with seizure free period of 1–2 years and 2–5 years, respectively, as compared to those with below one year (Table 6).
Table 6. Determinant factors associated with medication adherence among epileptic patients attending at neurology clinic of TASH, 2017.
| Variable | Category | Adherence N (%) |
COR (95% CI) |
AOR (95% CI) |
P-Value | |
|---|---|---|---|---|---|---|
| Non adherent | Adherent | |||||
| Educational status | No formal | 4 (3.1) | 12 (7.4) | 1.00 | 1.00 | |
| Primary | 40(31.0) | 48(29.6) | 2.500(0.748–8.358) | 2 .848(0. 824–9.839) | 0.098 | |
| Secondary | 46(35.7) | 59(36.4) | 2.339(0.708–7.730) | 3.266(0. 939–11.355) | 0.063 | |
| Tertiary | 39(30.2) | 43(2 6.6) | 2.721(0.810–9.141) | 5.177(1.412–18.584) | 0.013 | |
| Seizure free years | < 1 | 98(76.0) | 93(57.4) | 1.00 | 1.00 | |
| 1–2 | 14(10.9) | 32(19.8) | 0.415(0.208–0.827) | 0.359 (0.170–0.761) | 0.007* | |
| 2–5 | 11(8.5) | 22(13.6) | 0.474(0.218–1.032) | 0.455 (0.198–1.044) | 0.043* | |
| >5 | 6(4.6) | 15(9.2) | 0.380(0.141–1.020) | 0.368 (0.129–1.050) | 0.062 | |
| Source of medication | Paying | 55(42.6) | 96(59.3) | 1.00 | 1.00 | |
| Free | 74(57.4) | 66(40.7) | 1.957(1.224–3.128) | 2.316(1.360–3.943) | 0.002* | |
| Number of mediations | 1 | 45(34.9) | 75(46.3) | 1.00 | 1.00 | |
| 2 | 45(34.9) | 52(32.1) | 1.442(0.837–2.485) | 1.295(0.731–2.298) | 0.098 | |
| >2 | 39(30.2) | 35(21.6) | 1.912(1.060–3.449) | 1.728(0.939–11.355) | 0.063 | |
| Occurrence of ADRs | No | 60(46.5) | 87(53.7) | 1.00 | 1.00 | |
| Yes | 69(53.5) | 75(46.3) | 1.334(0.839–2.121) | 1.273(0.784–2.080) | 0.327 | |
COR, crude odds ratio; AOR, adjusted odds ratio; CI, confidence interval
Patients’ treatment satisfaction among the study participants
The global satisfaction was 67.4% and it was above 50% with regard to all the six dimensions (Table 7).
Table 7. Patients’ treatment satisfaction among epileptic patients attending at neurology clinic of TASH, 2017.
| SATMED-Q dimension | Satisfaction score (Mean ± SD) |
|---|---|
| Undesirable side effects (0–100) | 87.1 ± 20.9 |
| Treatment effectiveness (0–100) | 64.7 ± 21.9 |
| Convenience of use (0–100) | 72.7 ± 17.0 |
| Impact on daily activities (0–100) | 62.0 ± 23.3 |
| Medical care (0–100) | 65.9 ± 20.7 |
| Global satisfaction (0–100) | 67.4 ± 17.5 |
| Total composite score (0–100) | 70.2 ± 12.5 |
SATMED-Q: Satisfaction with Medicines Questionnaire
Discussion
GTCS was found to be the commonest seizure type encountered, which is in line with studies conducted in Saudi Arabia (65%) [20] and Bangladesh (74%) [21]. Choice of the most appropriate AEDs depends on proper classification of seizures type. Lack of proper seizure classification affects AEDs selection and treatment outcome [22, 23]. About 8% of the study participants had uncategorized seizure type, which could possibly have contributed to inappropriate drug selection and poor treatment outcomes. Monotherapy was the preferred treatment modality and this is in concordance with some [23] but discordant with others [9]. The reason for the discrepancy could be attributed to settings, as this was conducted in a tertiary hospital, where complicated and uncontrolled seizures are referred that might need combination therapy.
Although phenobarbital is not recommended as a first choice for any seizure type, it was the most frequently prescribed agent both as monotherapy and combination therapy. In other studies, agents like phenytoin [11], valproic acid [20], and carbamazepine [21] were the most commonly used ones. The use of phenobarbital despite the recommendation might be associated with cost issues. The study demonstrated that treatment was suboptimal, as the rate of seizure free period of less than a year was quite high (65.6%). This is similar with reports coming out from other developing countries [5] and could be attributed to DTPs like non-adherence and inappropriate selection of AEDs. This notion could be reinforced by the high rate of use of phenobarbital as a preferred agent.
About 70% of the study participants had at least one DTP, in which ADR (41.5%) was the most frequently encountered DTP. Several studies have identified ADR as the commonest problem, with a higher (82%) [24] or lower (31%) [25] rate than the present report that could probably related to methodological differences. Moreover, similar ADR profiles to this report have also been identified in other studies conducted in Ethiopia, [9]indicating action should be taken to relegate phenobarbital.
The second most common DTP identified was in-effective drug (27.8%). According to Cipolle et al. [24] DTP classification, this category has two major components (inappropriate drug selection and condition is refractory to the drug). Inappropriateness is commonly due to drug selection problem with regard to seizure type. For example, patients were taking phenobarbital for focal seizure, while phenytoin and carbamazepine are first line agents according to guidelines. Another example is the use of narrow spectrum AEDs for unclassified seizure type instead of valproic acid, as it is the AEDs of choice for unclassified seizure. The reasons for high rate of ineffective drug use might be drug cost, availability problems and lack of local treatment guidelines for tertiary hospital.
Carbamazepine was the most frequently involved AED in drug-interaction due to its potent liver enzyme inducing properties. Generally, AEDs have a wide range of drug interactions among themselves and with other drugs due to enzyme induction/inhibition or competition for plasma protein binding. Such drug interaction might cause ADRs, therapeutic failure and drug-related harm to patients [7]. Carbamazepine’s interactions with anti-TB and antiretrovirals could likely cause treatment failure or drug resistance. Therefore, changing the medication or dose adjustment is recommended. Furthermore, the interaction of phenobarbital with nifedipine, and valproic acid with warfarin could also have resulted in uncontrolled hypertension and increase in INR value, respectively. Potential drug-drug interactions should be ruled out prior to initiating AEDs.
The principle of seizure treatment is starting with low dose and escalating to a maximum dose based on treatment response and tolerability. The rate of inappropriate dosing was 11.9%, with phenobarbital and carbamazepine administered with high and low dose, respectively. Since most of the neurologic side effects are dose-related, AEDs don’t have acceptable safety profile. Patients on high dose of AEDs should therefore be monitored for toxicity and determining serum concentration is required for patients with uncontrolled seizure.
The most common untreated conditions in this study were epigastric pain, migraine headache and anaemia. Epigastric pain is a cause for poor adherence and its management could help to improve quality of life and medication adherence. Identification of risk factors for DTPs is helpful in finding patients at risk and taking action to avoid overt DTPs. This study demonstrated that the number of medications taken by a patient was an important risk factor for DTPs (Table 5) and this is supported also by other studies [26, 27].
AEDs adherence was 55.7%, which is similar with other studies in Ethiopia (58.5%) [10], China (51.9%) [13] and Saudi Arabia (62.7%) [20]. The rate was, however, lower than Palestine (85.3%) [12], India (98.6%) [11] and the USA (71%) [15]. The discrepancies could be due to differences in culture, belief, education and physicians approach to their patients. Source of medication was significantly associated with poor adherence. Free patients were 2.3 times more non-adherent than paying patients (Table 6). This might be due to the fact that medication supply in the hospital was inadequate and most free patients couldn’t afford to buy from outside. The findings also showed that seizure free year was associated with adherence of patients. Longer seizure free years would make patients to be more adherent to their medications possibly by increasing patients’ belief on medication effectiveness and this is in line with other studies [13].
The present study revealed that, global satisfaction of (67.4%) similar with the finding of Palestine (68.4%) [12]. Patient satisfaction with regard to impact of the medication therapy on daily activity was only 62.0%. This might be due about 38.5% of the participants are unemployed and treatment with AEDs restrict them from some daily activities like working with machineries. The satisfaction on treatment effectiveness (64.7%) and medical care (65.9%) was also low. The reasons could be most (65.6%) of the study participants had a seizure free period below one year and high number of patient flow that will compromise the quality of medical care.
The cross-sectional nature of the study and self-reported measure of adherence that could lead to overestimation of adherence could be among limitations of the study. Nevertheless, the optimal sample size, randomized sampling techniques from a tertiary hospital, use of both patient interview and medical chart review could offset the limitations and enhance generalizability the study.
Conclusion
The findings clearly indicate that there is a high prevalence of DTPs, which could negatively affect management of epileptic patients. The problems largely emanated from inefficient supply system, absence of clinical pharmacy services, poor patient health education, and lack of tailored guideline. Consequently, the overall patients’ treatment satisfaction was suboptimal. Measures should therefore be taken to circumvent these problems so that patients could enjoy seizure free lives.
Supporting information
(DOCX)
Acknowledgments
The authors would like to thank all the pharmacists and nurses who were participated in the data collection and we would like to extend our sincere thanks to all research participants.
Abbreviations
- ADR
Adverse Drug Reaction
- AEDs
Anti-Epileptic Drugs
- AOR
Adjusted Odds Ratio
- CBZ
Carbamazepine
- CLONA
Clonazepam
- COR
Crude Odds Ratio
- DRPs
Drug Related Problems
- DTPs
Drug Therapy Problems
- GTCS
Generalized Tonic Clonic Seizure
- LTG
Lamotrigine
- MMAS
Morisky Medication Adherence Scale
- PHB
Phenobarbital
- PHT
Phenytoin
- SATMED-Q
Scaling and Scoring of the Treatment Satisfaction with Medicines Questionnaire
- TASH
Tikur Anbessa Specialized Hospital
- VPA
Valproic acid
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported by Addia Ababa University (Medication therapy management thematic project (https://portal.aau.edu.et/) to BBN, ABB, EE and MAW. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Fisher RS, Boas WvE, Blume W, Elger C, Genton P, Lee P, et al. Epileptic seizures and epilepsy: definitions proposed by the International League Against Epilepsy (ILAE) and the International Bureau for Epilepsy (IBE). Epilepsia 2005, 46(4):470–472. 10.1111/j.0013-9580.2005.66104.x [DOI] [PubMed] [Google Scholar]
- 2.Kerr M, Scheepers M, Arvio M, Beavis J, Brandt C, Brown S, et al. Consensus guidelines into the management of epilepsy in adults with an intellectual disability. Journal of Intellectual Disability Research 2009, 53(8):687–694. 10.1111/j.1365-2788.2009.01182.x [DOI] [PubMed] [Google Scholar]
- 3.Rout SK, Kar DM. A review on antiepileptic agents, current research and Future prospectus on conventional and traditional drugs. Int J Pharm Sci Rev Res 2010, 3(2):19–23. [Google Scholar]
- 4.Henry TR, Conway J. Antiepilepsy drugs: mechanisms of action and pharmacokinetics. Epilepsy Board Rev Man 2012, 1(5):1–11. [Google Scholar]
- 5.Scott RA, Lhatoo SD, Sander JW. The treatment of epilepsy in developing countries: where do we go from here? Bulletin of the World Health Organization 2001, 79(4):344–351. [PMC free article] [PubMed] [Google Scholar]
- 6.Perucca E. Clinically relevant drug interactions with antiepileptic drugs. British journal of clinical pharmacology 2006, 61(3):246–255. 10.1111/j.1365-2125.2005.02529.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blume WT. Diagnosis and management of epilepsy. Canadian Medical Association Journal 2003, 168(4):441–448. [PMC free article] [PubMed] [Google Scholar]
- 8.Cipolle RJ, Strand L, Morley P: Pharmaceutical care practice: the patient-centered approach to medication management McGraw Hill Professional; 2012. [Google Scholar]
- 9.Rishe W, Seifu MF, Gelaw BK, Gunasekaran T, Tadesse E, Gebremariam MAM. Drug use evaluation of antiepileptic drugs in outpatient epilepsy clinic of bishoft general hospital, East Shoa, Ethiopia. Indo American Journal of Pharm Research 2015, 5. [Google Scholar]
- 10.Getachew H, Dekema N, Awol S, Abdi A, Mohammed M. Medication adherence in epilepsy and potential risk factors associated with non adherence in tertiary care teaching hospital in southwest Ethiopia. Gaziantep Medical Journal 2014, 20(1):59–65. [Google Scholar]
- 11.Sebastian J, Adepu R, Keshava B, Harsha S. Assessment of antiepileptic drugs usage in a South Indian tertiary care teaching hospital. Neurology Asia 2013, 18(2). [Google Scholar]
- 12.Sweileh WM, Ihbesheh MS, Jarar IS, Taha ASA, Sawalha AF, Sa'ed HZ, et al. Self-reported medication adherence and treatment satisfaction in patients with epilepsy. Epilepsy & Behavior 2011, 21(3):301–305. [DOI] [PubMed] [Google Scholar]
- 13.Liu J, Liu Z, Ding H, Yang X. Adherence to treatment and influencing factors in a sample of Chinese epilepsy patients. Epileptic disorders 2013, 15(3):289–294. 10.1684/epd.2013.0588 [DOI] [PubMed] [Google Scholar]
- 14.Jones R, Butler J, Thomas V, Peveler R, Prevett M. Adherence to treatment in patients with epilepsy: associations with seizure control and illness beliefs. Seizure 2006, 15(7):504–508. 10.1016/j.seizure.2006.06.003 [DOI] [PubMed] [Google Scholar]
- 15.Hovinga CA, Asato MR, Manjunath R, Wheless JW, Phelps SJ, Sheth RD, et al. Association of non-adherence to antiepileptic drugs and seizures, quality of life, and productivity: survey of patients with epilepsy and physicians. Epilepsy & Behavior 2008, 13(2):316–322. [DOI] [PubMed] [Google Scholar]
- 16.Abula T, Worki A. Patient non-compliance with drug regiments for chronic diseases in northwest Ethiopia. Ethiopian Journal of Health Development 2001, 15(3):185–192. [Google Scholar]
- 17.Tsiropoulos I, Andersen M, Hallas J. Adverse events with use of antiepileptic drugs: a prescription and event symmetry analysis. Pharmacoepidemiology and drug safety 2009, 18(6):483–491. 10.1002/pds.1736 [DOI] [PubMed] [Google Scholar]
- 18.Atkinson MJ, Sinha A, Hass SL, Colman SS, Kumar RN, Brod M, et al. Validation of a general measure of treatment satisfaction, the Treatment Satisfaction Questionnaire for Medication (TSQM), using a national panel study of chronic disease. Health and quality of life outcomes 2004, 2(1):12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Medical care 1986:67–74. 10.1097/00005650-198601000-00007 [DOI] [PubMed] [Google Scholar]
- 20.Gabr WM, Shams ME. Adherence to medication among outpatient adolescents with epilepsy. Saudi Pharmaceutical Journal 2015, 23(1):33–40. 10.1016/j.jsps.2014.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Habib M, Khan SU, Hoque MA, Mondal MBA, Hasan AH, Chowdhury RN, et al. Antiepileptic drug utilization in Bangladesh: experience from Dhaka Medical College Hospital. BMC research notes 2013, 6(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Azar NJ, Abou-Khalil BW. Considerations in the choice of an antiepileptic drug in the treatment of epilepsy In: Seminars in neurology: 2008: © Thieme Medical Publishers; 2008: 305–316. [DOI] [PubMed] [Google Scholar]
- 23.Gurshaw M, Agalu A, Chanie T. Anti-epileptic drug utilization and treatment outcome among epileptic patients on follow-up in a resource poor setting. Journal of Young Pharmacists 2014, 6(3):47–54 [Google Scholar]
- 24.Wassenaar M, van Heijl I, Leijten FS, van der Linden P, Uijl SG, Egberts A,et al. : Treatment of epilepsy in daily clinical practice: have outcomes improved over the past 10 years? Journal of neurology 2013, 260(11):2736–2743. 10.1007/s00415-013-7058-0 [DOI] [PubMed] [Google Scholar]
- 25.Manan MM, Rusli RA, Ang WC, Al‐Worafi Y, Ming LC. Assessing the pharmaceutical care issues of antiepileptic drug therapy in hospitalised epileptic patients. Journal of Pharmacy Practice and Research 2014, 44(3):83–88. [Google Scholar]
- 26.Hussein M, Lenjisa J, Woldu M, Tegegne G, Umeta G. Assessment of Drug Related Problems Among Hypertensive Patients on Follow up in Adama Hospital Medical College, East Ethiopia. Clinic Pharmacol Biopharmaceut 2014, 3(122):2. [Google Scholar]
- 27.Ayalew MB, Megersa TN, Mengistu YT. Drug-related problems in medical wards of Tikur Anbessa specialized hospital, Ethiopia. Journal of research in pharmacy practice 2015, 4(4):216 10.4103/2279-042X.167048 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.