Abstract
Purpose
This clinical pilot study was performed to determine the effectiveness of dual-energy cone-beam computed tomography (DE-CBCT) in measuring bone mineral density (BMD).
Materials and Methods
The BMD values obtained using DE-CBCT were compared to those obtained using calibrated multislice computed tomography (MSCT). After BMD calibration with specially designed phantoms, both DE-CBCT and MSCT scanning were performed in 15 adult dental patients. Three-dimensional (3D) Digital Imaging and Communications in Medicine data were imported into a dental software program, and the defined regions of interest (ROIs) on the 3-dimensional surface-rendered images were identified. The automatically-measured BMD values of the ROIs (g/cm3), the differences in the measured BMD values of the matched ROIs obtained by DE-CBCT and MSCT 3D images, and the correlation between the BMD values obtained by the 2 devices were statistically analyzed.
Results
The mean BMD values of the ROIs for the 15 patients as assessed using DE-CBCT and MSCT were 1.09±0.07 g/cm3 and 1.13±0.08 g/cm3, respectively. The mean of the differences between the BMD values of the matched ROIs as assessed using DE-CBCT and calibrated MSCT images was 0.04±0.02 g/cm3. The Pearson correlation coefficient between the BMD values of DE-CBCT and MSCT images was 0.982 (r=0.982, P<0.001).
Conclusion
The newly developed DE-CBCT technique could be used to measure jaw BMD in dentistry and may soon replace MSCT, which is expensive and requires special facilities.
Keywords: Bone Mineral Density, Cone-Beam Computed Tomography, Dual Energy, Phantoms
Introduction
Currently, cone-beam computed tomography (CBCT) is widely used in dental implant procedures. CBCT can also be used for the detection of dental caries, root fracture and resorption, periapical lesions, temporomandibular joint pathologies, and soft-tissue lesions such as gingival swelling, salivary gland inflammation, and calcifications. CBCT provides 3-dimensional (3D) diagnostic images, which can be used for treatment planning and prognostic evaluation. However, measurements of bone mineral density (BMD) made using CBCT have been regarded as inaccurate1,2,3,4 because CBCT can fail to provide a reliable BMD reading due to inaccuracies in the process of correcting local and conversion errors when obtaining gray values.5
BMD is clinically used instead of bone density, which is difficult to measure using many types of X-ray imaging. Dual-energy X-ray absorptiometry (DXA) is a representative radiological technique used to measure the BMD of the spine. However, unlike CBCT, DXA does not provide 3D images. Quantitative computed tomography (QCT) is a well-recognized technique for the volumetric measurement of BMD in the lumbar spine, and it does provide 3D images. However, QCT is expensive and requires special facilities; therefore, dental clinics typically avoid using QCT for measuring BMD.
In dental implantology, BMD is one of the most important factors to consider for treatment planning. CBCT is useful in dental implantology since it can provide 3D images while administering a lower dose of radiation than multislice computed tomography (MSCT),6 but as mentioned above, it cannot directly provide information regarding BMD.
Therefore, dual-energy CBCT (DE-CBCT) has been developed, and its effectiveness at measuring the BMD of the jaw was assessed by comparing it to calibrated MSCT. This is the first report on the clinical effectiveness of DE-CBCT.
Materials and Methods
This study was conducted under the approval of the Institutional Review Board of Seoul National University Dental Hospital (IRB No. CDE18007). To investigate the effectiveness of DE-CBCT at measuring the BMD of the jaw, patients who required dental interventions were enrolled in this clinical study. Because this was a pilot study, the sample size was 15. The inclusion criteria were: 1) age between 19 and 85 years; 2) general good health; 3) being scheduled for a dental intervention, such as implant placement; and 4) the voluntary provision of informed consent. The exclusion criteria were: 1) pregnancy or lactation, 2) evaluation the day before or on the same day as the patient was to undergo CT scanning, 3) the inability to read or write or the presence of a cognitive impairment, and 4) lack of suitability for this clinical trial as judged by the principal investigator.
After informed consent was obtained from the participants, their demographic variables, past medical histories, vital signs, and pregnancy status for women (determined via human chorionic gonadotropin testing) were collected. On the first visit, DE-CBCT (RCT720, Ray Co., Ltd., Seongnam, Korea) was performed (Fig. 1). The second visit was scheduled within 1 month after the first, and the calibrated MSCT (Siemens AG, Erlangen, Germany) was obtained with settings of 120 kVp, 80 mA, and 0.75-mm-thick slices; for female participants, this followed confirmation of a negative pregnancy test. After MSCT imaging, the adverse effects of nausea, vomiting, skin changes, loss of hair, oral infection, or mucositis were evaluated and recorded.
Fig. 1. The newly developed dual-energy cone-beam computed tomography (RCT720, Ray Co., Ltd., Seongnam, Korea) in this study.

The DE-CBCT and MSCT devices were calibrated on a daily basis, and three 3D images of phantoms were obtained to perform BMD calibration and to convert from Hounsfield units (HU)7 to BMD (g/cm3). Fig. 2 shows a cylindrical phantom designed according to ISO 9001 standards with a diameter of 70 mm and a length of 70 mm (QRM, Moehrendorf, Germany). The cylindrical phantom consisted of 8 inserts containing calcium hydroxyapatite that were used to simulate BMD values, of which the specific inserts used were HA0, HA400, HA800, HA1000, and HA1200. The dimensions of the inserted BMD phantom were 16 mm×75 mm.
Fig. 2. The phantoms available for use in this study. Of these, HA0, HA400, HA800, HA1000, and HA1200 are used.

Digital Imaging and Communications in Medicine data from the DE-CBCT and MSCT images were imported into OnDemand3D® (CyberMed, Seoul, Korea) dental software. Oral and maxillofacial radiologists identified 3 regions of interest (ROIs) on 3D surface-rendered images of the same patient. Either the maxillary tuberosity or the retromolar trigone was used as the reference ROI. For each ROI, the BMD (g/cm3) was automatically measured by the software. For the anatomically matched ROIs, the differences between the BMDs determined using DE-CBCT and MSCT were statistically analyzed, using P<0.05 as the threshold for statistical significance.
Statistical analyses were performed using SPSS version 21.0 (IBM Corp., Armonk, NY, USA). A between-group comparison of the BMD values of the matched ROIs was conducted using the paired Student t-test (P<0.05). In addition, the differences between measurements were plotted against the average BMD using Bland-Altman analysis, and the Pearson correlation coefficient was calculated.
Results
Fifteen healthy patients (7 men and 8 women; mean age, 58.6 years; range, 24–75 years) participated in this study between December 2018 and March 2019. No adverse effects associated with the clinical investigation were reported. For each patient, 3 ROIs were selected, resulting in a total of 45 BMD values. Of these, 1 BMD value was excluded due to the presence of a metal artifact, and the remaining 44 BMD values were analyzed.
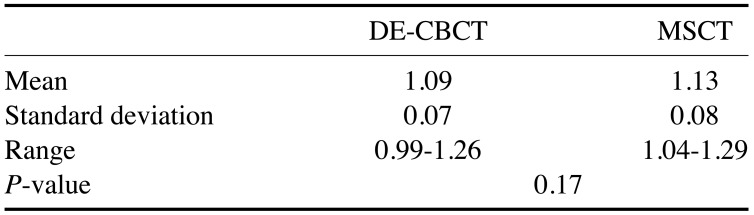
The mean BMD values of the 15 patients as obtained using DE-CBCT and MSCT 3D imaging were 1.09±0.07 g/cm3 and 1.13±0.08 g/cm3, respectively. The BMD ranges for DE-CBCT and MSCT were 0.99–1.26 g/cm3 and 1.04–1.29 g/cm3, respectively. No statistically significant difference was found between the values obtained using the 2 imaging techniques (P=0.17, Table 1).
Table 1. Mean, standard deviation, and range of bone mineral density (g/cm3) for dual-energy cone-beam computed tomography (DE-CBCT) and multislice computed tomography (MSCT), with the P-value of the comparison between the 2 techniques.
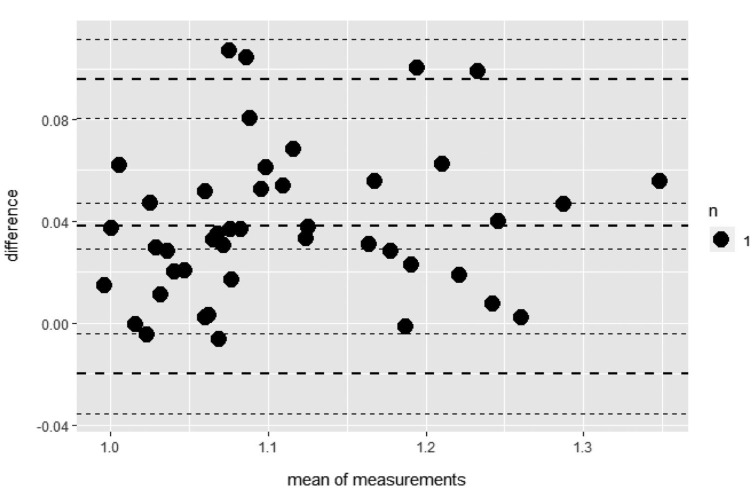
Fig. 3 shows the Bland-Altman analysis of the BMD values of the ROIs. This analysis was conducted using the mean and standard deviation of the differences between the BMD values as determined using DE-CBCT and MSCT. The resulting graph is an XY scatter plot, where the y-axis shows the difference between the 2 paired BMD measurements (DE-CBCT-MSCT), and the x-axis represents the average BMD. For the matched ROIs, the mean of the differences between the BMD values obtained using DE-CBCT and calibrated MSCT was 0.04±0.02 g/cm3. Therefore, in the evaluation of BMD, the mean difference between DE-CBCT and MSCT was close to zero (mean=0.04).
Fig. 3. Bland-Altman analysis of bone mineral density (g/cm3) as measured with dual-energy cone-beam computed tomography (DE-CBCT) and multislice computed tomography (MSCT). The upper and lower limits of agreement are 0.10 and −0.02, respectively.
For the entire group of 15 patients, the Pearson correlation coefficient between the BMD values obtained with DE-CBCT and MSCT was 0.982 (r=0.982, P<0.05).
Discussion
The main results of this study revealed no statistically significant difference between BMD values as measured by DE-CBCT and MSCT; additionally, DE-CBCT showed no adverse effects on safety during 2 visits for all patients.
CBCT has many advantages over MSCT, including a lower cost, a lower dose of radiation exposure, and the need for less space. As a result, CBCT is routinely used in dental implantology because 3D images and BMD values of alveolar bone are fundamental for treatment planning and facilitating good patient outcomes. However, the BMD values (in HU) derived from CBCT have been regarded as unreliable8,9 and have been associated with unpredictable outcomes of dental implants.10,11,12,13 Additionally, CBCT has limitations, including image noise, motion artifacts, and poor soft-tissue contrast.14 Due to the improved contrast in the images it provides, DE-CBCT may useful for the evaluation of temporomandibular joint disorders and the accurate identification of salivary stones.
In this study, jaw BMD values determined using DE-CBCT were compared to those determined with calibrated MSCT. DE-CBCT for 3D imaging of the jaw utilizes projections at both a high and a low energy level. X-ray exposure should be clinically justified for each patient based on a radiation dose as low as reasonably achievable, a guideline supported by the American Dental Association.15 Even though DE-CBCT uses dual energy levels, the radiation dose is only 62.2% of single-energy CBCT (Ray Co., Ltd., Seongnam, Korea), according to a technical report on radiation safety.
A new BMD calibration method was derived from calibrated HU values obtained from the images at different dual-energy levels. The projection images were acquired with the HA phantoms of different densities inserted into the acrylic base at different kVp levels, and the CT volumes were reconstructed separately. The voxels of the CT images at different kVp levels were correlated point by point. The mean values of the phantom regions and the air region were used to estimate a line of density values, and the correlated points of the regions were projected onto the density line. The parameters for mapping density in g/cm3 to HU were determined using the known HU values of the HA phantoms. Then, we calculated the new HU values from the CT volumes measured at different kVp levels.
The strength of this pilot study was its comparison of the BMD of 3 maxillary or mandibular reference regions in images obtained using DE-CBCT and MSCT in the same patients. An oral radiologist handled the DE-CBCT and MSCT images.
However, this study has several limitations. First, it is a pilot study with a relatively small number of patients. We are planning to confirm our findings through a pivotal clinical trial by calculating the required sample size based on this study. Second, the differences between DE-CBCT and MSCT were mostly positive, with most values being both positive and directional. Counterintuitively, this suggests that the newly developed DE-CBCT technique has high specificity. We plan to calibrate the DE-CBCT software to increase its sensitivity in addition to the already-high specificity.
The mean BMD values were not significantly different between DE-CBCT and MSCT. In addition, the correlation between the values was 98%. Therefore, this indicates that the newly developed DE-CBCT technique could be used to assess jaw BMD instead of the more expensive MSCT method. Nevertheless, this study also had the limitation of a small sample size. Further clinical validation of BMD measurements obtained using DE-CBCT is needed.
Footnotes
This work was supported by a Korea Evaluation Institute of Industrial Technology (KEIT) grant funded by the Korean Ministry of Trade, Industry, and Energy (MOTIE) (No. 10063356).
Conflicts of Interest: Two of the authors (Sungho Chang and Sang Chul Lee) invented the DE-CBCT and are still working for the company (Ray Co., Ltd., Seongnam, Korea) that developed it. The other authors have no conflict of interest to declare. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- 1.Campos MJ, de Souza TS, Mota Júnior SL, Fraga MR, Vitral RW. Bone mineral density in cone beam computed tomography: only a few shades of gray. World J Radiol. 2014;6:607–612. doi: 10.4329/wjr.v6.i8.607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cassetta M, Stefanelli LV, Pacifici A, Pacifici L, Barbato E. How accurate is CBCT in measuring bone density? A comparative CBCT-CT in vitro study. Clin Implant Dent Relat Res. 2014;16:471–478. doi: 10.1111/cid.12027. [DOI] [PubMed] [Google Scholar]
- 3.Pauwels R, Jacobs R, Singer SR, Mupparapu M. CBCT-based bone quality assessment: are Hounsfield units applicable? Dentomaxillofac Radiol. 2015;44:20140238. doi: 10.1259/dmfr.20140238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Razi T, Niknami M, Alavi Ghazani F. Relationship between Hounsfield unit in CT scan and gray scale in CBCT. J Dent Res Dent Clin Dent Prospects. 2014;8:107–110. doi: 10.5681/joddd.2014.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim DG. Can dental cone beam computed tomography assess bone mineral density? J Bone Metab. 2014;21:117–126. doi: 10.11005/jbm.2014.21.2.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Miracle AC, Mukherji SK. Conebeam CT of the head and neck, part 1: physical principles. AJNR Am J Neuroradiol. 2009;30:1088–1095. doi: 10.3174/ajnr.A1653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aranyarachkul P, Caruso J, Gantes B, Schulz E, Riggs M, Dus I, et al. Bone density assessments of dental implant sites: 2. Quantitative cone-beam computerized tomography. Int J Oral Maxillofac Implants. 2005;20:416–424. [PubMed] [Google Scholar]
- 8.Nackaerts O, Maes F, Yan H, Couto Souza P, Pauwels R, Jacobs R. Analysis of intensity variability in multislice and cone beam computed tomography. Clin Oral Implants Res. 2011;22:873–879. doi: 10.1111/j.1600-0501.2010.02076.x. [DOI] [PubMed] [Google Scholar]
- 9.Silva IM, Freitas DQ, Ambrosano GM, Bóscolo FN, Almeida SM. Bone density: comparative evaluation of Hounsfield units in multislice and cone-beam computed tomography. Braz Oral Res. 2012;26:550–556. doi: 10.1590/s1806-83242012000600011. [DOI] [PubMed] [Google Scholar]
- 10.Turkyilmaz I, Tözüm TF, Tumer C. Bone density assessments of oral implant sites using computerized tomography. J Oral Rehabil. 2007;34:267–272. doi: 10.1111/j.1365-2842.2006.01689.x. [DOI] [PubMed] [Google Scholar]
- 11.Shapurian T, Damoulis PD, Reiser GM, Griffin TJ, Rand WM. Quantitative evaluation of bone density using the Hounsfield index. Int J Oral Maxillofac Implants. 2006;21:290–297. [PubMed] [Google Scholar]
- 12.Fuh LJ, Huang HL, Chen CS, Fu KL, Shen YW, Tu MG, et al. Variations in bone density at dental implant sites in different regions of the jawbone. J Oral Rehabil. 2010;37:346–351. doi: 10.1111/j.1365-2842.2010.02061.x. [DOI] [PubMed] [Google Scholar]
- 13.Aksoy U, Eratalay K, Tözüm TF. The possible association among bone density values, resonance frequency measurements, tactile sense, and histomorphometric evaluations of dental implant osteotomy sites: a preliminary study. Implant Dent. 2009;18:316–325. doi: 10.1097/ID.0b013e31819ecc12. [DOI] [PubMed] [Google Scholar]
- 14.Jain S, Choudhary K, Nagi R, Shukla S, Kaur N, Grover D. New evolution of cone-beam computed tomography in dentistry: combining digital technologies. Imaging Sci Dent. 2019;49:179–190. doi: 10.5624/isd.2019.49.3.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.American Academy of Oral and Maxillofacial Radiology. Clinical recommendations regarding use of cone beam computed tomography in orthodontics. [corrected]. Position statement by the American Academy of Oral and Maxillofacial Radiology. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;116:238–257. doi: 10.1016/j.oooo.2013.06.002. [DOI] [PubMed] [Google Scholar]