Abstract
Background:
Potentially avoidable Emergency Department (ED) visits are a significant source of excess healthcare spending. Despite improvement in postoperative readmissions, 20% of bariatric surgery patients utilize the ED postoperatively. Many of these visits may be appropriately managed in lower-acuity centers.
Objective:
We sought to evaluate the economic impact of shifting potentially avoidable ED visits following bariatric surgery to lower-acuity centers.
Setting:
Statewide quality improvement collaborative.
Methods:
We performed an observational study of patients who underwent bariatric surgery between 2011- 2017 using a linked data registry including clinical data from a large quality improvement collaborative and payment data from a statewide value collaborative. Postoperative ED visits and readmission rates were determined. 90-day ED and Urgent Care Center (UCC) visit claims were matched to a clinical registry. Price-standardized payments for UCC and ED visits without admission were compared.
Results:
Among the 36,071 patients who underwent bariatric surgery, 8.4% presented to the ED postoperatively. Approximately 50% of these visits resulted in readmission. 388 ED visits without readmission (i.e. “potentially avoidable ED visits”) and 110 UCC encounters with claims data were identified. Triaging a potentially avoidable ED visit to an UCC would generate a savings of $4,238 per patient, reducing spending in this cohort by $1.6 million.
Conclusion:
Shifting potentially avoidable ED visits following bariatric surgery could result in significant cost savings. Efforts to improve patients’ selection of healthcare setting and increase utilization of lower-acuity centers may serve as a template for appropriately meeting the needs of patients and containing spending following bariatric surgery.
Keywords: Bariatric Surgery, Emergency Department Visit, Nonurgent ED Visit, Urgent Care Center, Health Policy, Cost Containment
INTRODUCTION
The current healthcare system is inadequately designed to meet the demands of postoperative patients, especially those with intermediate needs. The Emergency Department (ED) is the default site for unplanned postoperative care, driven in part by limited surgical clinic hours and a lack of alternative postoperative care settings. In bariatric surgery, the recent policy emphasis on readmissions resulted in substantially decreased postoperative re-hospitalizations.1–5 However, 1 in 5 postoperative patients still presents to the ED with as many as 75% not readmitted.6,7 ED visits that do not result in readmission may be “potentially avoidable” and highlight an additional opportunity for improvement.
The potential cost saving of shifting these postoperative patients out of the ED and to lower-acuity centers is unknown. In non-surgical patients, triaging 20% of non-emergent ED visits to lower-acuity settings would translate to $4.4 billion in annual savings.8–10 Whether these findings are generalizable to surgical patients is unclear. On one hand, common treatments that postoperative bariatric surgery patients receive in the ED are available in settings such as Urgent Care Centers (UCCs).11 UCCs are also more desirable from a patient’s perspective given shorter wait times and lower out of pocket costs.12 Alternatively, unfamiliarity with this patient population may lead to excess testing, over treatment, poor quality of care, and marginal cost savings. Understanding both the clinical and financial impact of shifting “potentially avoidable” ED visits to lower-acuity settings is necessary. These efforts could lead to optimally redesigning the healthcare system to more appropriately meet the needs of patients while reducing surgical episode spending.
In this context, we utilized the Michigan Bariatric Surgery Collaborate and Michigan Value Collaborative to explore the difference in spending between postoperative Emergency Department visits not resulting in readmission (“potentially avoidable” visits) and Urgent Care Center encounters within 90-days of bariatric surgery.
METHODS
Data Sources
This study is an analysis of bariatric surgery cases in a linked data registry that includes clinical metrics and outcomes from the Michigan Bariatric Surgery Collaborative (MBSC, http://www.michiganbsc.org) and adjudicated complete claims payment from the Michigan Value Collaborative (MVC, http://michiganvalue.org). The MBSC is a clinical registry that includes information from >95% of patient undergoing bariatric surgery in the State of Michigan.13,14 This collaborative includes 45 hospitals and employs trained data abstractors that perform extensive chart review regarding patients’ demographics, comorbidities, perioperative care and process details, and postoperative outcomes for multiple bariatric operations. Institutional review boards at each participating hospital have approved data collection and participation in the MBSC.
The MVC is a 75-hospital statewide consortium whose claims-based registry contains complete episode payment data from Medicare fee-for-service beneficiaries and Blue Cross Blue Shield of Michigan (BCBSM) Preferred Provider Organization patients. Employing algorithms developed by researchers for the Dartmouth Atlas of Healthcare, claims data are price-standardized to account for geographic, timing, and contractual differences in payments to hospitals.15 All payments are presented in price-standardized, inflation-adjusted dollars according to the 2012 to 2016 Medicare payment schedule.
Study Sample
For this study, we first identified all patients ≥ 18 years old in the MBSC registry undergoing primary Roux-en-Y gastric bypass (RYGB) or sleeve gastrectomy (SG) between January 1, 2007 and December 31, 2017. Patients undergoing revisional surgery were excluded from this analysis. For assessment of episode spending, patients who underwent primary RYGB or SG between October 11, 2011 and May 23, 2017 were identified. For these patients, MBSC clinical data were linked to MVC claims data using surgery facility, surgical procedure, date of surgery, patient gender, date of birth, and payer category. Medicare fee-for-service beneficiaries were excluded from this analysis.
Independent Variable
Location of service was defined as “Emergency Department” (ED) or “Urgent Care Center” (UCC). UCC encounter in the MVC professional claims database was defined as encounters that occurred within 90 days from the index operation and included an urgent care setting provider type code (code ‘UC’). ED visit with hospital readmission was defined as an encounter with claims data that included an Emergency Medicine physician provider type code (93) or Emergency Medicine specific CPT code (M3) and readmission code (0450, 0451, 042, 0981) with Emergency Medicine visit category code (‘ip_readmit3190d’) on the same date of service. ED visit without inpatient readmission was defined as an encounter that included an Emergency Medicine physician provider type code (93) or Emergency Medicine specific CPT code (M3) with no linked readmission code on the same date of service. ED visits that did not result in readmission were classified as “potentially avoidable ED visits”.
Outcomes and Explanatory Variables
Our primary outcome for this study was price-standardized total episode spending for 90-day potentially avoidable ED visits and UCC encounters. Total episode spending included both facility and professional claims. We evaluated 30-day ED utilization and readmission rates in the MBSC from 2007 to 2017 as a secondary outcome. Explanatory variables included demographic information (such as age, gender, body mass index (BMI), race, education level and annual income), comorbid conditions (such as diabetes, cardiovascular disease, hypertension and psychological disorders), type of surgical procedure (RYGB or SG), and 30-day postoperative outcomes including mortality, all complications and serious complications. Grade I complications are non-life-threatening and include surgical site infection (wound infections treated with antibiotics and/or wound opening), anastomotic stricture, bleeding (transfusion ≤ 4 units), pneumonia (if treated with antibiotics), hospital-acquired infections (urinary tract infection, C. difficile infection), and postoperative esophagogastroduodenoscopy. Grade II complications include abdominal abscess formation (requiring drainage/reoperation), bowel obstruction/hernia (requiring operation), anastomotic leak, bleeding (transfusion > 4 units), respiratory failure (requiring intubation for 2-7 days), renal failure (requiring in-hospital dialysis), wound infection/dehiscence and venous thromboembolism. Finally, Grade III complications include myocardial infarction, cardiac arrest, renal failure (requiring long-term dialysis), respiratory failure (requiring intubation for >7 days or tracheostomy), and death. Serious complications were defined as Grade II and Grade III complications.
Statistical Analysis
We utilized independent sample t-tests for continuous variables (age, baseline BMI, etc.) and chi-square comparison for categorical variables (gender, income, hypertension, etc.) to assess whether patient characteristics were independent of the assigned 90-day postoperative care setting variable. For risk adjustment, we performed a stepwise regression to evaluate the covariate-adjusted association between setting of care and 30-day clinical outcomes. Adjustment covariates included gender, white race, private insurance, hypertension, hyperlipidemia, diabetes, GERD, coronary artery disease, sleep apnea, mobility limitations, asthma, mental health disorder, musculoskeletal disorder, kidney disease, liver disease, and surgical procedure performed (RYGB or SG). Factors that were statistically significantly in univariate analysis were included as risk-adjusted variables. We then compared “potentially avoidable ED visit” to UCC encounters using risk-adjusted 30-day surgical outcomes.
Episode spending data did not conform to a normal distribution. Therefore, we performed non-parametric Mann-Whitney/Wilcoxon rank sum tests to assess differences in episode spending between the assigned 90-day postoperative care setting variable.
All reportedp values are 2-sided, andp < 0.05 was considered statistically significant. All statistical analyses were performed using SAS 9.4 (SAS Institute, Cary, North Carolina).
RESULTS
Patients and Postoperative Healthcare Utilization
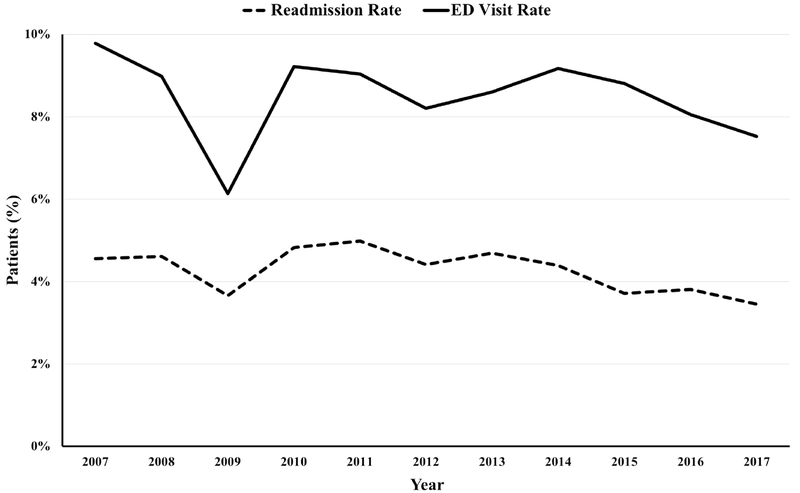
62,271 patients underwent primary RYGB or SG at 45 hospitals between January 1, 2007 and December 31, 2017. During this time period the 30-day readmission rate decreased from 4.6% to 3.5% postoperative ED visits decreased from 9.8% to 7.5%. (Figure 1)
Figure 1.
Postoperative emergency department visit and readmission rates from 2007 to 2017.
Between October 1, 2011 and May 23, 2017, 36,071 patients underwent primary RYGB or SG. Among this MBSC cohort, 3,030 patients (8.4%) presented to the ED and 46.6% of these visits resulted in readmission (1,412 patients). 650 patients matched to MVC claims data. Among these patients 900 ED or UCC encounters within 90-days of the index operation were identified. Specifically, 402 ED visits with inpatient readmission, 388 potentially avoidable ED visits, and 110 UCC encounters were identified. Of the patients who received care in an ED or UCC, 24% had multiple encounters; however, no patients in the cohort had a documented UCC and ED encounter on the same day.
Patient characteristics of UCC and potentially avoidable ED visits are shown in Table 1. The patients who presented to an UCC were more likely to have undergone RYGB (79.1% vs. 36.9%; P =0.0097) and have a diagnosed hepatic comorbidity (20.0% vs. 9.5%; P = 0.0027). There was no difference between the two groups in age (40.8 vs 40.7 years; P = 0.9108), gender (% male, 20.9% vs 15.7%; P = 0.1997), preoperative BMI (48.7 vs 47.7; P = 0.2505), number of comorbidities or specific comorbidities excluding liver disease. Additionally, there was no difference between UCC and potentially avoidable ED visit patients’ education level (% college education, 18.6% vs. 13.0%; P = 0.1485), employment status (% not working, 16.7% vs. 20.5%; P = 0.3897), marital status (% not married or living with significant other, 30.4% vs 39.2%; P = 0.1066), or annual income level.
Table 1.
Patient characteristics of potentially avoidable Emergency Department (ED) visits and Urgent Care Center encounters.
| Potentially Avoidable ED Visit | Urgent Care Center Encounter | P value | |
|---|---|---|---|
| Encounters, No. | 388 | 110 | |
| Age, mean (SD), years | 40.7 (11.7) | 40.8 (9.4) | 0.91 |
| Preoperative BMIa mean (SD), kg/m2 | 47.7 (8.6) | 48.7 (8.3) | 0.25 |
| Male, No. (%) | 61 (15.7) | 23 (20.9) | 0.20 |
| Raceb, No. (%) | |||
| White Non-Hispanic/Latino | 265 (75.1) | 73.0 | 0.98 |
| Black Non-Hispanic/Latino | 80 (22.7) | 23.0 | |
| Other/Multiracial | 8 (2.3) | 2.0 | |
| Annual Income Levelc, No. (%) | |||
| < $10,000 | 20 (5.7) | 2 (2.0) | 0.15 |
| $10,000 - $24,999 | 40 (11.4) | 8 (8.0) | |
| $25,000 - $44,999 | 103 (29.4) | 26 (26.0) | |
| $45,000 - $75,000 | 91 (26.0) | 37 (37.0) | |
| >$75,000 | 96 (27.4) | 27 (27.0) | |
| Education Leveld, No. (%) | |||
| No College | 46 (13.0) | 19 (18.6) | 0.15 |
| Some College / College Graduate | 309 (87.0) | 83 (81.4) | |
| Employment Statuse, No. (%) | |||
| Not Working | 73 (20.5) | 17 (16.7) | 0.39 |
| Working Full- or Part-Time | 283 (79.5) | 85 (83.3) | |
| Marital Statusf, No. (%) | |||
| Not Married or Living with Significant Other | 139 (39.2) | 31 (30.4) | 0.11 |
| Married or Living with Significant Other | 216 (60.9) | 71 (69.7) | |
| Procedure, No. (%) | |||
| Roux-en-Y Gastric Bypass | 143 (36.9) | 26 (23.6) | 0.01 |
| Sleeve Gastrectomy | 245 (63.1) | 84 (76.4) | |
| Number of Comorbidities, No. (%) | |||
| 0 | 7 (1.8) | 0 (0.0) | 0.10 |
| 1 | 19 (4.9) | 10 (9.1) | |
| ≥2 | 362 (93.3) | 100 (90.9) | |
| Comorbidities, No. (%) | |||
| Hypertension | 167 (43.0) | 48 (43.6) | 0.91 |
| Hyperlipidemia | 163 (42.0) | 48 (43.6) | 0.76 |
| Diabetes Mellitus | 89 (22.9) | 31 (28.2) | 0.26 |
| Obstructive Sleep Apnea | 171 (44.1) | 53 (48.2) | 0.44 |
| Cardiovascular disease | 178 (45.9) | 52 (47.3) | 0.80 |
| Coronary Artery Disease | 13 (3.4) | 3 (2.7) | 0.74 |
| Gastroesophageal Reflux Disease | 213 (54.9) | 60 (54.6) | 0.95 |
| Asthma | 92 (23.7) | 24 (21.8) | 0.68 |
| Kidney Disease | 1 (0.3) | 0 (0.0) | 0.59 |
| Liver Disease | 37 (9.5) | 22 (20.0) | 0.003 |
| Psychological Disorder | 225 (58.0) | 63 (57.3) | 0.89 |
| Venous Thromboembolism | 13 (3.4) | 0 (0.0) | 0.08 |
| Mobility Limitations | 11 (2.8) | 2 (1.8) | 0.56 |
BMI; Body Mass Index (kg/m2),
Data missing on 47 encounters,
Data missing on 48 encounters,
Data missing on 41 encounters,
Data missing on 40 encounters,
Data missing on 41 encounters
Patients with potentially avoidable ED visits were more likely to have experienced a complication (20.5% vs 11.3%; P = 0.013) or a serious complication (8.2% vs 3.0%; P=0.022). However, there was no difference between the two groups with respect to mortality (0.03% vs 0.0%; P = 0.893) or any specific post-operative complication. (Table 2)
Table 2.
Risk-adjusted clinical outcomes of patients with potentially avoidable Emergency Department (ED) visits and Urgent Care Center encounters.
| Potentially Avoidable ED Visit | Urgent Care Center Encounter | P value | |
|---|---|---|---|
| Encounters, No. | 388 | 110 | |
| Mortality, % | 0.2 | 0.0 | 0.90 |
| Any Complication, % | 20.5 | 11.3 | 0.01 |
| Grade I Complicationa | 11.9 | 6.6 | 0.11 |
| Grade II Complicationb | 7.9 | 3.1 | 0.02 |
| Grade III Complicationc | 0.03 | 0.0 | 0.90 |
| Serious Complicationd % | 8.2 | 3.0 | 0.02 |
| Specific Complications, % | |||
| Cardiac | 0.03 | 0.0 | 0.89 |
| Respiratory | 0.6 | 2.3 | 0.18 |
| Venous Thromboembolism | 1.4 | 0.7 | 0.37 |
| Hemorrhage | 7.1 | 3.6 | 0.38 |
| Leak or Perforation | 2.3 | 0.0 | 0.78 |
| Anastomotic Leak | 0.9 | 0.0 | 0.99 |
| Wound Complication | 3.7 | 3.6 | 0.97 |
| Obstruction | 1.2 | 0.0 | 0.85 |
| Small Bowel Obstruction | 0.1 | 0.0 | 0.87 |
Grade I Complication: surgical site infection (wound infections treated with antibiotics and/or wound opening), anastomotic stricture, bleeding (transfusion ≤ 4 units), pneumonia (if treated with antibiotics), hospital-acquired infections (urinary tract infection, C. difficile infection), postoperative esophagogastroduodenoscopy.
Grade II Complications: abdominal abscess formation (requiring drainage/reoperation), bowel obstruction/hernia (requiring operation), anastomotic leak, bleeding (transfusion > 4 units), respiratory failure (requiring intubation for 2-7 days), renal failure (requiring in-hospital dialysis), wound infection/dehiscence, venous thromboembolism.
Grade III Complications: myocardial infarction, cardiac arrest, renal failure (requiring long-term dialysis), respiratory failure (requiring intubation for > 7 days or tracheostomy), death.
Serious complications: Grade II and Grade III complications.
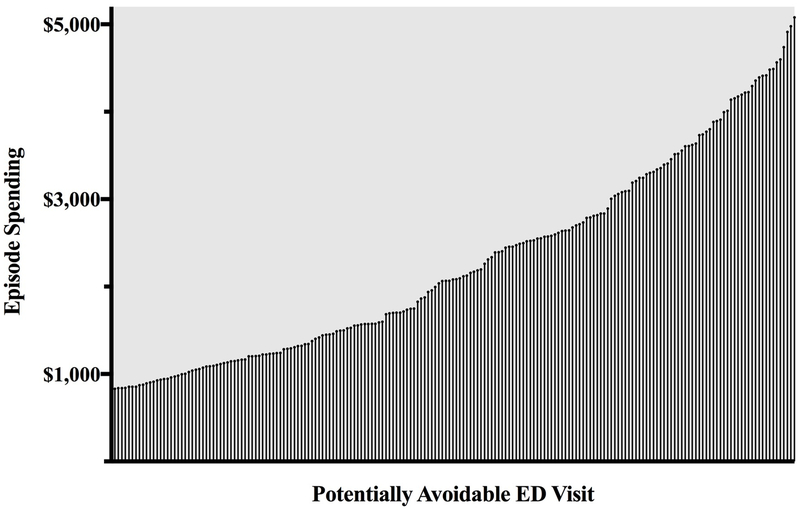
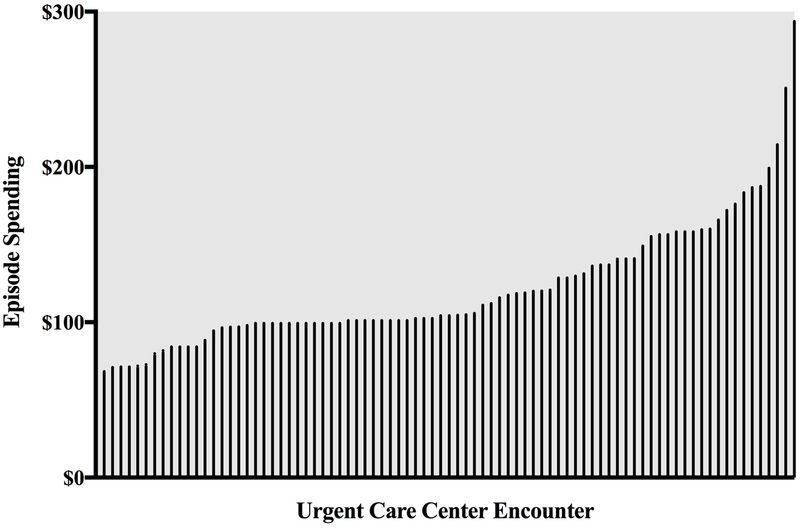
Postoperative Care Setting and Episode Payments
Figure 2 depicts the interquartile range of spending for potentially avoidable ED visits. The average spending for potentially avoidable ED visits was $4,351. Spending for UCC encounters was significantly lower with an average payment of $113 (P < 0.001). (Figure 3) Triaging a potentially avoidable ED visit to an UCC would generate an average savings of $4,238. In our cohort of MBSC and MVC matched patients, shifting all potentially avoidable ED visits to an UCC would result in a net savings of $1.6 million, with much higher potential savings ($6.0 million) when we extrapolate to all 30-day potentially avoidable ED visits captured in the MBSC database during this time period.
Figure 2.
Interquartile range of potentially avoidable Emergency Department visit episode spending.
Figure 3.
Interquartile range of potentially avoidable Urgent Care Center visit episode spending.
DISCUSSION
This study of unplanned postoperative care following bariatric surgery has two key findings. First, we found that nearly 50% of ED visits following bariatric surgery did not result in readmission. These encounters may reflect non-emergent problems and “potentially avoidable” ED visits that could be managed in lower-acuity care centers. Notably, complications were more common among patients with “potentially avoidable” ED visits. However, the timing of diagnosis is unknown, and the fact that these patients were discharged from the ED suggests that some complications may have been diagnosed during the index admission and not during the ED episode. Second, spending for a postoperative “potentially avoidable” ED visit was $4,238 more than an Urgent Care Center encounter. Taken together, these results suggest that the ED may not be the ideal care setting for a large portion of postoperative patients seeking treatment. Redesigning our current postoperative processes to identify and triage appropriate patients to lower-acuity centers may result in significant cost savings.
Postoperative readmission has been a key focus of recent policy efforts and a highly scrutinized quality metric.1,5,16,17 Previous work in bariatric surgery led to substantial reductions in the frequency of these costly post-discharge encounters.2–5,18 However, despite a decrease in postoperative readmissions, postoperative ED visits remain high with minimal improvement.6,7,18–21 In some studies, up to 15% of bariatric surgery patients visit the ED without readmission, and nearly 75% of 30-day postoperative ED visits do not result in readmission.6,7 Our results are consistent with these findings as 50% of ED visits in our cohort did not result in readmission. The expanding gap between postoperative readmission rates and ED visits reflect a fixed patient population that may not require costly ED care. “Potentially avoidable” ED visits are a source of significant economic burden, and in non-surgical patients shifting only 20% of “potentially avoidable” ED visit to lower-acuity centers could result in savings of $4.4 billion annually.10 Our results in a single surgical population demonstrate that shifting a “potentially avoidable” postoperative bariatric ED visit to an UCC would result in a net savings of $4,238. If all “potentially avoidable” ED visits were shifted to lower cost settings it could result in annual savings of approximately $1 million in this single state cohort. Further, given the consistently increasing volume of bariatric surgery in the US, triaging bariatric surgery patients with intermediate needs to lower-acuity centers could lead to annual savings of at least $29.5 million.22
It would be unethical to suggest that in order to decrease ED utilization, postoperative patients with non-emergent issues should not seek medication attention. Further, recommending that all patients seek care at lower-acuity care centers first is inappropriate. While additional work is needed to identify which patients may be appropriate for care in lower-acuity settings, there may be some general concepts that could help. Enhancing communication between patients and surgical providers regarding selection of care settings may result in better matching of patients’ needs and clinical venue. A prior study revealed that 75% of bariatric surgery patients who self-referred to the ED and were not readmitted presented outside of traditional office hours, and many had a chief complaint of incisional concerns, headache, anxiety, dehydration, and dizziness.11 Improving communication processes between patients and surgical teams and assisting patients in triaging concerns may lead to improved matching of clinical concerns with care setting and decreased frequency of potentially avoidable ED visits. Importantly, in order to maintain quality of care, surgeons must remain intimately involved in patient management regardless of the clinical setting and may prefer that certain subsets of patients (e.g. those with acute onset abdominal pain) always be evaluated in a fully resourced setting with computerized tomography (CT) scanners. For patients not requiring ED evaluation, workflow processes and direct lines of communication between providers and patients need to be established prior to triaging patients out of the ED. Additionally, as some UCC providers may not equipped to handle bariatric patients, interventions to shift patients to lower-acuity settings should be piloted with pre-identified centers after targeted and robust education on the management of bariatric patients.
UCCs may be a practical option for triaging patients with intermediate needs given their widespread availability, ability to provide common treatments such as intravenous fluids, and their extended hours and suitable staffing.11 However, some payers restrict access to outpatient CT scanners, outpatient infusion centers, and home health care.23 In order to decrease potentially avoidable ED visits payers must begin to cover specific services delivered outside of the ED. For example, in a patient with persistent nausea following a sleeve gastrectomy, IV hydration and a non-emergent CT scan may be warranted. Without payers covering use of outpatient imaging and infusion services this patient will likely be referred to the ED, leading to more expensive care that does not best match the patient’s clinical needs. While certain complaints require fully resourced EDs for evaluation, unless all payers begin to cover outpatient and alternative care setting services, other non-emergent postoperative concerns may continue to be automatically evaluated in the ED.
The present study should be interpreted in the context of a number of limitations. First, we included patients from a single state and therefore the results may not be fully generalizable. However, patients in Michigan are unlikely to systematically vary from bariatric surgery patients across the country. Second, we evaluated postoperative spending from an individual payer which limits generalizability to other payers. Nonetheless, it is unlikely that spending for “potentially avoidable” ED visits and UCC encounters from other payers significantly differs. Third, the chief complaint and treatment decisions for patients who presented to the ED and UCC are unknown. A portion of the postoperative care episodes captured in our analysis may be unrelated to the bariatric surgery. Additionally, we are unable to identify patient factors associated with appropriateness for lower-acuity settings.
CONCLUSION
In summary, our findings demonstrate that a significant portion of postoperative ED visits following bariatric surgery do not result in readmission and may be “potentially avoidable.” Triaging patients who do not require ED level care to lower-acuity settings may serve as a template for containing spending after bariatric surgery and more appropriately matching patients’ needs with the ideal healthcare setting. Several implications for both policy and practice emerge from our results. First, given the substantial cost savings of managing non-emergent patients in UCCs, payers should consider incentivizing efforts that increase utilization of appropriate care settings such as improving communication with patients to minimize self-referral to the ED. These efforts are particularly salient for bariatric surgeons and reimbursement as payers continues to shift toward value-based payment models for global episodes of care, including services up to 90 days after discharge.24 Additionally, a critical component of shifting “potentially avoidable” visits out of the ED involves establishing alternative high-quality options. Developing specific partnerships between surgeons, other providers, and local lower-acuity care centers may lead to comprehensive high-quality care delivered in non-traditional settings for patients with intermediate needs. Ultimately, providing high-quality care for postoperative patients must remain the priority over financial savings and future research into effective methods of delivering high-quality care in lower-acuity settings is needed.
Highlights.
50% of patients presenting to the Emergency Department following bariatric surgery are not readmitted.
Patients who present to the Emergency Department and not readmitted (i.e. “potentially avoidable ED visit”) may be appropriately managed in alternative care settings.
Triaging a potentially avoidable ED visit to an Urgent Care center would generate a savings of $4,238 per patient.
Improving patients’ selection of healthcare setting may appropriately meet the needs of postoperative patients and contain spending following bariatric surgery.
Acknowledgments
Conflicts of Interest and Sources of Funding Research Support:
Margaret E Smith is supported by funding from the National Institute of Health Obesity Surgery Scientist Training Grant (T32-DK-108740). Dr. Oliver Varban, Dr. Jonathan Finks, Dr. Arthur Carlin, and Dr. Amir Ghaferi obtain salary support from Blue Cross Blue Shield for participating in quality improvement initiates and the Executive Committee of the Michigan Bariatric Surgery Collaborative.
Conflicts of Interest: Dr. Oliver Varban, Dr. Jonathan Finks, Dr. Arthur Carlin, and Dr. Amir Ghaferi obtain salary support from Blue Cross Blue Shield for participating in quality improvement initiates and the Executive Committee of the Michigan Bariatric Surgery Collaborative. Dr. Margaret Smith and Mr. Aaron Bonham have nothing to disclose.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Presented in part at the Society of American Gastrointestinal and Endoscopic Surgeons 2018 Annual Meeting, Seattle, WA, April 11, 2018.
REFERENCES
- 1.Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program. https://www.facs.org/quality-programs/mbsaqip. Accessed March 19, 2018.
- 2.Abraham CR, Werter CR, Ata A, et al. Predictors of Hospital Readmission after Bariatric Surgery. J Am Coll Surg. 2015;221(1):220–227. [DOI] [PubMed] [Google Scholar]
- 3.Encinosa WE, Bernard DM, Du D, Steiner CA. Recent improvements in bariatric surgery outcomes. Med Care. 2009;47(5):531–535. [DOI] [PubMed] [Google Scholar]
- 4.Mora-Pinzon MC, Henkel D, Miller RE, et al. Emergency department visits and readmissions within 1 year of bariatric surgery: A statewide analysis using hospital discharge records. Surgery. 2017;162(5):1155–1162. [DOI] [PubMed] [Google Scholar]
- 5.Morton J The first metabolic and bariatric surgery accreditation and quality improvement program quality initiative: decreasing readmissions through opportunities provided. Surg Obes Relat Dis. 2014;10(3):377–378. [DOI] [PubMed] [Google Scholar]
- 6.Chen J, Mackenzie J, Zhai Y, et al. Preventing Returns to the Emergency Department FollowingBariatric Surgery. Obesity Surg. 2017;27(8):1986–1992. [DOI] [PubMed] [Google Scholar]
- 7.Cho M, Kaidar-Person O, Szomstein S, Rosenthal RJ. Emergency room visits after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Surg Obes Relat Dis. 2008;4(2): 104–109. [DOI] [PubMed] [Google Scholar]
- 8.Mehrotra A, Liu H, Adams JL, et al. Comparing costs and quality of care at retail clinics with that of other medical settings for 3 common illnesses. Ann Interm Med. 2009;151(5):321–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thygeson M, Van Vorst KA, Maciosek MV, Solberg L. Use and costs of care in retail clinics versus traditional care sites. Health Aff (Millwood). 2008;27(5):1283–1292. [DOI] [PubMed] [Google Scholar]
- 10.Weinick RM, Burns RM, Mehrotra A. Many emergency department visits could be managed at urgent care centers and retail clinics. Health Aff (Millwood). 2010;29(9):1630–1636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stevens H, Wells E, Ross R, Stricklen A, Ghaferi AA. Patient perspectives on emergency department self-referral after bariatric surgery. Surg Obes Relat Dis. 2018. [DOI] [PubMed] [Google Scholar]
- 12.Coster JE, Turner JK, Bradbury D, Cantrell A. Why Do People Choose Emergency and Urgent Care Services? A Rapid Review Utilizing a Systematic Literature Search and Narrative Synthesis. Acad Emerg Med. 2017;24(9):1137–1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Birkmeyer NJ, Dimick JB, Share D, et al. Hospital complication rates with bariatric surgery in Michigan. JAMA. 2010;304(4):435–442. [DOI] [PubMed] [Google Scholar]
- 14.Scally CP, Varban OA, Carlin AM, Birkmeyer JD, Dimick JB. Video Ratings of Surgical Skill and Late Outcomes of Bariatric Surgery. JAMA Surg. 2016;151(6):e160428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gottlieb DJ, Zhou W, Song Y, Andrews KG, Skinner JS, Sutherland JM. Prices don’t drive regional Medicare spending variations. Health Aff (Millwood). 2010;29(3):537–543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dimick JB, Birkmeyer NJ, Finks JF, et al. Composite measures for profiling hospitals on bariatric surgery performance. JAMA Surg. 2014;149(1):10–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418–1428. [DOI] [PubMed] [Google Scholar]
- 18.Telem DA, Yang J, Altieri M, et al. Rates and Risk Factors for Unplanned Emergency Department Utilization and Hospital Readmission Following Bariatric Surgery. Ann Surgery. 2016;263(5):956–960. [DOI] [PubMed] [Google Scholar]
- 19.Kellogg TA, Swan T, Leslie DA, Buchwald H, Ikramuddin S. Patterns of readmission and reoperation within 90 days after Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2009;5(4):416–423. [DOI] [PubMed] [Google Scholar]
- 20.Macht R, George J, Ameli O, Hess D, Cabral H, Kazis L. Factors associated with bariatric postoperative emergency department visits. Surg Obes Relat Dis. 2016;12(10):1826–1831. [DOI] [PubMed] [Google Scholar]
- 21.Willson TD, Gomberawalla A, Mahoney K, Lutfi RE. Factors influencing 30-day emergency visits and readmissions after sleeve gastrectomy: results from a community bariatric center. Obesity Surg. 2015;25(6):975–981. [DOI] [PubMed] [Google Scholar]
- 22.Surgery ASfMaB. Estimate of Bariatric Surgery Numbers, 2011-2014. http://asmbs.org/resources/estimate-of-bariatric-surgery-numbers.
- 23.Healthcare Finance. New Anthem policy cuts hospital outpatient payment for MRIs, CT scans in 5 states. https://www.healthcarefinancenews.com/news/new-anthem-policy-cuts-hospital-outpatient-payment-mris-ct-scans-5-states. Accessed June 9, 2019.
- 24.Centers for Medicare & Medicaid Services. Bundled payments for care improvement (BPCI) initiative: general information. https://innovation.cms.gov/initiatives/bundled-payments/. Accessed February 16, 2018.