Abstract
Purpose of Review
In the setting of rotatory knee instability following anterior cruciate ligament (ACL) reconstruction, there has been a resurgence of interest in knee’s anterolateral complex (ALC). Reconstruction or augmentation of the ALC with procedures such as a lateral extra-articular tenodesis (LET) has been proposed to reduce rotatory knee instability in conjunction with ACL reconstruction. The current review investigates the recent literature surrounding the role of the ALC in preventing rotatory knee instability.
Recent Findings
The knee’s anterolateral complex (ALC) is a complex structure composed of the superficial and deep portions of the iliotibial band, the capsulo-osseous layer, and the anterolateral capsule. Distally, these various layers merge to form a single functional unit which imparts stability to the lateral knee. While the iliotibial band and the capsule-osseous layer have been shown to be primary restraints to rotatory motion after ACL injury, the biomechanical role of the anterolateral capsule remains unclear. Biomechanical studies have shown that the anterolateral capsule and the anterolateral thickening of this capsule act as a sheet of fibrous tissue which does not resist motion around the knee as other longitudinally oriented ligaments do.
Summary
Augmentation of the ALC, with LET, has been performed globally for over 30 years. This procedure can decrease rotatory knee instability, but long-term studies have found little difference in patient-reported outcomes, osteoarthritis, or ACL reconstruction failure with the addition of LET. Further research is needed to clarify indications for the clinical use of ALC-based procedures.
Keywords: ACL, Rotatory stability, Anterolateral capsule, Extra-articular tenodesis
Introduction
There has been increasing focus on the anterolateral structures of the knee following the re-discovery of a discrete anatomical ligament along the lateral aspect of the knee capsule [7, 56]. There is conflicting literature for the proposed anterolateral ligament (ALL) with regard to its existence, significance, and the role for its reconstruction in the setting of injury [12, 16, 50]. There is currently consensus among international ACL reconstruction experts that the proposed ALL is a structure within the anterolateral capsule of the knee. The iliotibial band (ITB) with its superficial, deep, and Kaplan fibers and the anterolateral capsule make up the anterolateral complex (ALC). The ALC will be discussed for the remainder of this review [12]. The purpose of the current review is to present the recent literature on the ALC and its role in rotatory knee instability of the knee.
Anatomy
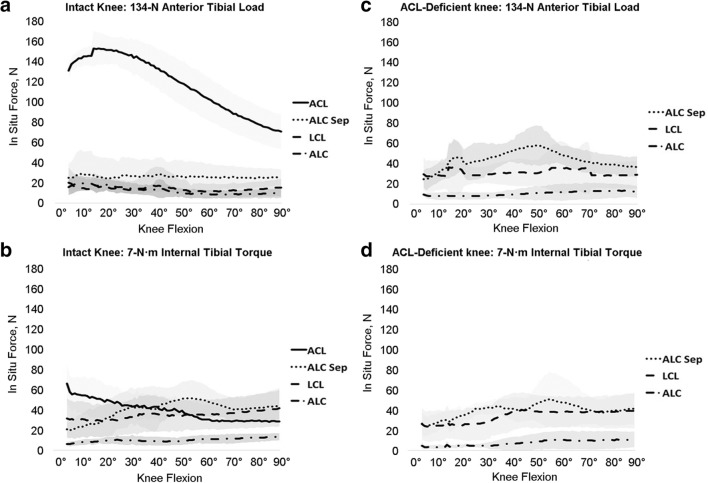
Meticulous layer-by-layer anatomical dissections on adult fresh frozen cadavers showed an identifiable thickening of the ALC in 35% of specimens with no adult specimens having a discrete ligamentous structure (Fig. 1) [17]. Anatomical assessment of fetal knee tissue revealed no distinct ligamentous structure along the anterolateral capsule between the fibular collateral ligament and the patellar tendon, and confirmed via histology that only loose disorganized collagen, consistent with capsular tissue, was present in this region of the fetal anterolateral capsule [43].
Fig. 1.
Lateral view on a left knee of a 46-year-old specimen. To enable visualization of the anterolateral structures, the iliotibial band was carefully dissection from the underlying tissue, a starting proximally and b ending with the transection from the Gerdy tubercle. ALC, anterolateral capsule; FH, fibula head; ITB, iliotibial band; LCL, lateral collateral ligament. (Adapted from Guenther D et al. The Anterolateral Capsule of the Knee Behaves Like a Sheet of Fibrous Tissue. The American Journal of Sports Medicine. 2012; 45(4), 849–855. 10.1177/0363546516674477)
There is variability in the recently published literature about the anatomical characteristics of the ALC. Careful anatomical dissection of fresh frozen human cadavers has revealed multiple distinct layers of the ALC (from superficial to deep): the superficial and deep iliotibial band, the capsulo-osseous layer of the iliotibial band, and the anterolateral capsule of the knee [17]. A systematic review found that most anatomic studies determined the thickening of the anterolateral capsule had its femoral origin anterior and distal to the origin of the lateral collateral ligament on the lateral epicondyle, but some finding variation in the thickening with the origin posterior to the lateral collateral ligament [1, 32, 42, 55]. The tibial insertion of thickening in the ALC is consistently noted to be between Gerdy’s tubercle and the fibular head [1].
Biomechanics of the ALC and Residual Rotatory Knee Instability
The primary goal of ACL reconstruction is to restore function to the knee, reducing the anterior tibial translation and rotatory knee instability seen in the ACL-deficient knee. While in most cases, anatomic reconstruction of the ACL reduces rotatory knee instability, the etiology of residual rotatory knee instability following anatomic ACL reconstruction remains unclear [62]. In this regard, residual rotatory knee instability or a high-grade pivot shift pre-operatively have been proposed as indications for ALC reconstruction [53, 57].
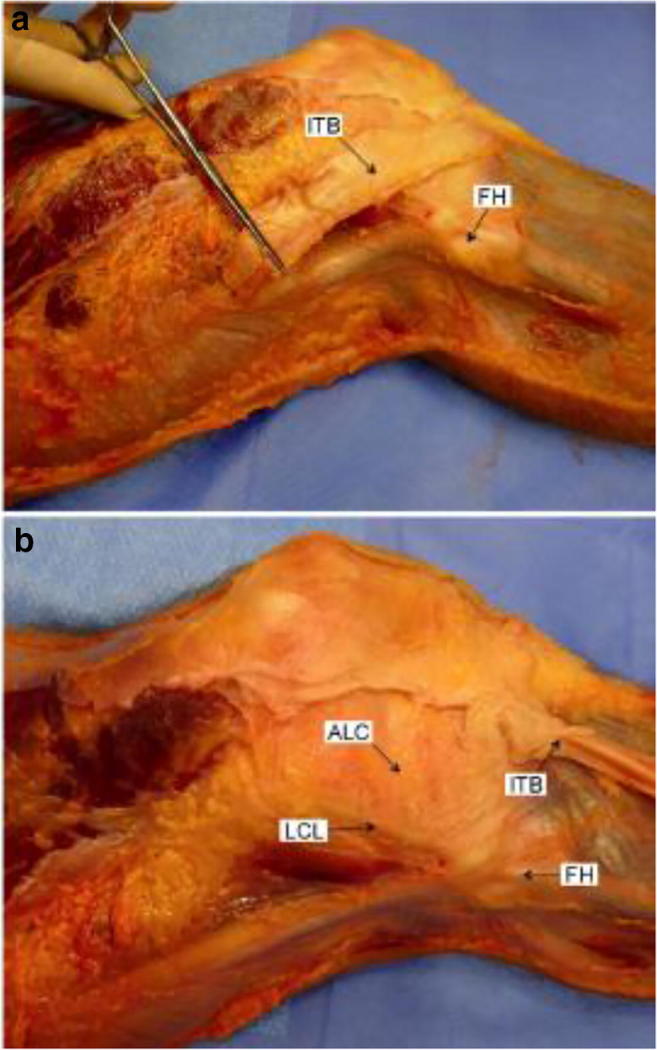
When rotatory knee instability is encountered following ACL reconstruction, it remains unclear whether ALC injury plays a contributing role [35]. While some cadaveric biomechanical studies analyzing a simulated pivot shift maneuver demonstrated increased rotatory knee instability in the setting of concomitant ALC injury, other have failed to demonstrate significant increases in rotatory knee instability or other changes to knee kinematics (Fig. 2) [20, 24, 27, 35, 39, 44, 51, 54, 58]. Ex vivo biomechanical studies have demonstrated that, in cases of ACL deficiency with known concomitant injury to the ALC, ACL reconstruction alone may not fully restore knee stability [18, 22].
Fig. 2.
In situ forces in response to a a 134-N anterior tibial load and b a 7-Nm internal tibial torque in the intact knee and in response to c a 134 anterior tibial load and d a 7-Nm internal tibial roque in the ACL-deficient knee. ACL, anterior cruciate ligament; ALC, anterolateral capsule; ALC Sep, anterolateral capsule separation (forces transmitted between anterolateral capsular regions); LCL, lateral collateral ligament. The areas shaded represent the SDs. (Adapted from Guenther D et al. The Anterolateral Capsule of the Knee Behaves Like a Sheet of Fibrous Tissue. The American Journal of Sports Medicine. 2012; 45(4), 849–855. 10.1177/0363546516674477)
The differences in rotatory knee instability may be in part due to differing levels of resection of the iliotibial band during simulated ALC injury, with the iliotibial band consistently acting as a primary stabilizer to tibial internal rotation [24, 34]. At greater than 30° of flexion, where the pivot shift is measured during clinical examinations, the superficial, deep, and capsulo-osseous layers of the iliotibial band act as the primary stabilizers of rotatory stability. Additionally, following ACL injury, the iliotibial band is the primary restraint to tibial internal rotation during a simulated pivot shift [24]. Similar biomechanical studies have found that the ALC experiences the highest in situ forces and resists rotatory knee instability at 90° of flexion and insignificant in situ force at 30° of flexion where rotatory knee instability is normally assessed [4, 60].
Residual rotatory knee instability following anatomic ACL reconstruction may be addressed via different anterolateral procedures, of which a lateral extra-articular tenodesis (LET) represents one option. Biomechanically, in the setting of confirmed ALC injury, the addition of a LET has been demonstrated to play a role in restoring pre-injury kinematics [18, 22]. However, concerns regarding potential over-constraint exist following the results of recent biomechanical studies which demonstrated decreased tibial internal rotation with a LET procedure [18].
Biomechanical studies have demonstrated that the ALC may not function as a ligamentous structure. In a systematic dissection of the anterolateral knee, only negligible longitudinal forces were noted within the anterolateral capsule [14]. This suggests that the anterolateral capsule responds biomechanically like a sheet of tissue rather than a longitudinally oriented ligamentous structure.
Although the proposed role of a discrete ligamentous structure within the ALC is variable in recent biomechanical literature, the role of the ALC (iliotibial band, lateral capsule, lateral meniscus) has been reported as preventing rotatory knee instability [12, 20, 31, 34]. When injury or insufficiency of the ALC is present, surgical fixation or reconstruction might be performed to prevent rotatory knee instability by restoring native anatomy.
Residual Rotatory Knee Instability
Restoring translational and rotatory knee stability to the knee is the primary goal of ACL reconstruction. Non-anatomic ACL reconstruction can lead to residual rotatory knee instability or anterior laxity, and critical review of radiographs may reveal signs of non-anatomic tunnel placement [2, 3, 47]. Residual rotatory knee instability in the setting of anatomic ACL reconstruction may be secondary to injury to other ligamentous structures around the knee or may be related to the bony morphology of the individual patient, which has been associated with findings such as a high-grade pivot shift [30, 31, 37, 38, 49, 59]. In the setting of combined ACL and ALC injury where the patient experiences persistent rotatory knee instability, biomechanical studies have suggested that the addition of LET may reduce rotatory knee instability to a greater degree than isolated ACL reconstruction [11, 28].
Multiple methods for performing LET have been described, including the Lemaire, modified Lemaire, MacIntosh, Zarins and Rowe, Müller, and Marcacci and Zaffagnini, and other techniques. The noted techniques do not encompass all described LETs, but represent multiple approaches, grafts, and tensioning techniques for performing an additional anterolateral procedure [6, 10, 25, 26, 29, 64]. Relatively few studies exist, which directly compare these various techniques. In a biomechanical comparison of a proposed ALL reconstruction with Lemaire, and Macintosh LET techniques, the proposed reconstruction was not found to result in increased stability, while Macintosh and Lemaire techniques were noted to prevent rotatory knee instability [22]. Similarly, cadaveric models have noted the addition of a Müller type LET to restore rotatory stability in the setting of combined ACL + ALC injury better than ACL reconstruction alone [45]. Finally, a systematic review of biomechanical literature on ACL reconstruction + LET suggested that several LET techniques restored or even over-constrained rotatory knee motion following ACL reconstruction. No significant biomechanical differences noted between specific techniques in this study [46].
Outcomes of LET and ALC Procedures
Multiple retrospective and prospective studies have looked at patient outcomes in ACL reconstruction and ACL + LET [9, 13, 36, 48, 63]. A meta-analysis of ACL reconstruction versus ACL + LET in human subjects found the LET decreased the pivot shift phenomenon, but did not result in changes in IKDC scores or KT-1000 measurements [19].
LET results in decreased rotatory knee motion suggestive of over-constraint in some biomechanical studies [11]. Biomechanical findings have raised concerns regarding whether LET may predispose the knee to degenerative changes. However, it is too early to report clinical findings of premature osteoarthritis. One examination with long-term follow-up of 421 patients did not note an increase in rates of osteoarthritis following LET. However, the authors did note that concomitant meniscal injury, common with ACL injury, may increase the risk for development of osteoarthritis at long-term follow-up [8, 15]. A second study with 10-year follow-up of patients undergoing combined ACL reconstruction and LET demonstrated reduced rates of rotatory knee instability, improved IKDC activity scores, and found no increased risk for arthritic changes compared with ACL reconstruction alone [9].
LET may help to reduced rotatory knee instability and forces experienced by graft tissue following ACL reconstruction; therefore, it has been theorized that ACL reconstruction with LET could reduce re-rupture rates. However, a meta-analysis of eight randomized control trials between ACL reconstruction and ACL + LET did not demonstrate a significance decreased in re-rupture rates with only isolated clinical trials noting reduced rates of graft failure with combined ACL + LET [33, 40].
There is a lack of high-quality evidence with long-term (> 5 year) follow-up regarding ALL reconstruction procedure. Further, recently published results of such studies are often conflicting. In a single-surgeon, prospective cohort of 502 patients undergoing ACL reconstruction with bone-patellar tendon-bone autograft, hamstring autograft, or hamstring autograft with concomitant ALL reconstruction, there was significantly lower graft failure in the hamstring + ALL reconstruction group (4.1% failure) compared with the isolated ACL reconstructions [52]. However, in this study, the reported rates of failure for isolated ACL reconstruction (11% hamstring, 17% bone-patellar tendon-bone) were higher than reported in previous literature, suggesting a secondary factor may have played a role in the difference in failure rates between treatment groups in this cohort [23, 61].
A similar study retrospectively reviewed professional athletes undergoing combined ACL reconstruction and proposed ALL reconstruction [41]. In this study, ALL reconstruction again was noted to decrease side-to-side laxity and pivot shift findings, with a reported return to sport rate of 85.7% at 1 year. However, at 4-year follow-up, greater than 20% of subjects were noted to have retired from professional sport participation [41]. In a randomized controlled trial of ALL reconstruction, 110 patients with a minimum grade 2 pivot shift were randomly assigned to either isolated ACL reconstruction or combined ACL and ALL reconstruction [21]. At 27 months average follow-up, patients demonstrated similar pivot shift, Lachman, and anterior drawer findings. The combined reconstruction group was superior to the isolated ACL group only in instrumented laxity as measured on the KT-1000 and no clinical differences noted between groups [21]. In summary, some authors have noted short-term benefits to LET or ALL reconstruction in the setting of persistent rotatory knee instability following treatment of an ACL injury. However, the noted effect of extra-articular procedures have been reported with a great degree of variability, offering little generalizability of results from single-surgeon studies.
In an effort to better study the effects of LET, a large multi-center trial is ongoing aimed at determining the difference between ACL reconstruction and ACL + LET [5]. In this study, patients 25 years or younger with noted “high-risk” criteria are randomized to either isolated ACL hamstring reconstruction versus ACL reconstruction with a Lemaire-type LET procedure. LET is performed with a strip of IT band passed deep to the lateral collateral ligament. High-risk criteria for patient enrollment include a pivot shift of grade II or greater, clinical evidence of ligamentous laxity (i.e., a medium to high Beighton’s score), and plan to return to higher risk activity such as participation in cutting sports. While the study is still ongoing, interim reports have suggested a benefit to the addition of LET in this subset of patients, with lower rates of graft failure noted in those randomized to receive both an ACL reconstruction and Lemaire-type LET.
Conclusion
In conclusion, the anterolateral complex (ALC) of the knee is a complex structure comprised of a confluence of the knee’s lateral stabilizers, which function to provide rotatory stability to the knee. While not completely understood, reports suggest a role for surgical management of the ALC in certain situations where persistent rotatory knee instability is encountered following ACL reconstruction. However, until more concrete indications for such procedures can be identified by high-level studies, management of rotatory knee instability likely will continue to emphasize the need for a well-performed, anatomic ACL reconstruction. Further, with regard to non-anatomic procedures, concerns for over-constraint have been documented historically, warranting further investigation of long-term outcomes. Though still in their infancy, several such high-level studies are ongoing, which may help to elucidate the true role of ALC reconstruction in the management of rotatory knee instability.
Compliance with Ethical Standards
Conflict of Interest
Volker Musahl, Elan Golan, Robert Tischman, Theresa Diermeier, Ravi Vaswani, and Kevin Byrne declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on ACL; Risk Factors, Outcomes, Preventions
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Elan J Golan, Email: ejgolan@gmail.com.
Robert Tisherman, Email: Tishermanr@upmc.edu.
Kevin Byrne, Email: kjb65@pitt.edu.
Theresa Diermeier, Email: resi.diermeier@gmx.de.
Ravi Vaswani, Email: vaswanirs@upmc.edu.
Volker Musahl, Email: musahlv@upmc.edu.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Ariel de Lima D, Helito CP, Lacerda de Lima L, de Castro Silva D, Costa Cavalcante ML, Dias Leite JA. Anatomy of the anterolateral ligament of the knee: a systematic review. Arthroscopy. 2019. [DOI] [PubMed]
- 2.Astur DC, Santos CV, Aleluia V, Astur Neto N, Arliani GG, Kaleka CC, Skaf A, Cohen M. Characterization of cruciate ligament impingement: the influence of femoral or tibial tunnel positioning at different degrees of knee flexion. Arthroscopy. 2013;29:913–919. doi: 10.1016/j.arthro.2013.01.008. [DOI] [PubMed] [Google Scholar]
- 3.Bedi A, Maak T, Musahl V, Citak M, O’Loughlin PF, Choi D, Pearle AD. Effect of tibial tunnel position on stability of the knee after anterior cruciate ligament reconstruction: is the tibial tunnel position most important? Am. J. Sports Med. 2011;39:366–373. doi: 10.1177/0363546510388157. [DOI] [PubMed] [Google Scholar]
- 4.Bell KM, Rahnemai-Azar AA, Irarrazaval S, Guenther D, Fu FH, Musahl V, Debski RE. In situ force in the anterior cruciate ligament, the lateral collateral ligament, and the anterolateral capsule complex during a simulated pivot shift test. J. Orthop. Res. 2018;36:847–853. doi: 10.1002/jor.23676. [DOI] [PubMed] [Google Scholar]
- 5.•• Bryant D, Getgood A, Litchfield R, McCormack RG, Heard M, Macdonald PB, Spalding T, Verdonk P, Peterson D, Bardana D, Rezansoff A, Group SS. Predictors of poor outcome Following ACL reconstruction with or without lateral extra-articular tenodesis: the stability experience. In: ISAKOS Biennial Congress.; 2019:Paper #130. Study constitutes the first randomized, high level investigation of outcomes following the addition of a LET procedure to ACL reconstruction
- 6.Christel P, Djian P. [Anterio-lateral extra-articular tenodesis of the knee using a short strip of fascia lata]. Rev. Chir. Orthop. Reparatrice Appar. Mot. 2002;88:508–513. [PubMed] [Google Scholar]
- 7.Claes S, Vereecke E, Maes M, Victor J, Verdonk P, Bellemans J. Anatomy of the anterolateral ligament of the knee. J. Anat. 2013;223:321–328. doi: 10.1111/joa.12087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Devitt BM, Bouguennec N, Barfod KW, Porter T, Webster KE, Feller JA. Combined anterior cruciate ligament reconstruction and lateral extra-articular tenodesis does not result in an increased rate of osteoarthritis: a systematic review and best evidence synthesis. Knee Surgery. Sport. Traumatol. Arthrosc. 2017;25:1149–1160. doi: 10.1007/s00167-017-4510-1. [DOI] [PubMed] [Google Scholar]
- 9.Ferretti A, Monaco E, Ponzo A, Basiglini L, Iorio R, Caperna L, Conteduca F. Combined Intra-articular and Extra-articular Reconstruction in Anterior Cruciate Ligament-Deficient Knee: 25 Years Later. Arthroscopy. 2016;32:2039–2047. doi: 10.1016/j.arthro.2016.02.006. [DOI] [PubMed] [Google Scholar]
- 10.Galway R, Beaupre A, MacIntosh DL. Pivot shift: a clinical sign of symptomatic anterior cruciate insufficiency. J Bone Jt. Surg Br. 1972;54:763–764. [Google Scholar]
- 11.Geeslin AG, Moatshe G, Chahla J, Kruckeberg BM, Muckenhirn KJ, Dornan GJ, Coggins A, Brady AW, Getgood AM, Godin JA, LaPrade RF. Anterolateral knee extra-articular stabilizers: a robotic study comparing anterolateral ligament reconstruction and modified Lemaire lateral extra-articular tenodesis. Am. J. Sports Med. 2018;46:607–616. doi: 10.1177/0363546517745268. [DOI] [PubMed] [Google Scholar]
- 12.• Getgood A, Brown C, Lording T, Amis A, Claes S, Geeslin A, Musahl V. The anterolateral complex of the knee: results from the International ALC Consensus Group Meeting. Knee Surg. Sports Traumatol. Arthrosc. 2019;27:166–176. Summary of consensus understanding of the anterolateral complex of the knee including definitions of known anatomy, definitions of proposed structures, and clinical concerns for laterally based procedures. [DOI] [PubMed]
- 13.Getgood A, Litchfield R, Hewison C, Bryant DM, McCormack RG, Heard M, Macdonald PB, Spalding T, Verdonk P, Peterson D, Bardana D, Rezansoff A. Anterior cruciate ligament reconstruction with or without a lateral extra-articular tenodesis – assessment of failure at one year from the ISAKOS sponsored stability study. Arthroscopy. 2017;33:e120. [Google Scholar]
- 14.Guenther D, Rahnemai-Azar AA, Bell KM, Irarrazaval S, Fu FH, Musahl V, Debski RE. The anterolateral capsule of the knee behaves like a sheet of fibrous tissue. Am. J. Sports Med. 2017;45:849–855. doi: 10.1177/0363546516674477. [DOI] [PubMed] [Google Scholar]
- 15.Hagino T, Ochiai S, Senga S, Yamashita T, Wako M, Ando T, Haro H. Meniscal tears associated with anterior cruciate ligament injury. Arch. Orthop. Trauma Surg. 2015;135:1701–1706. doi: 10.1007/s00402-015-2309-4. [DOI] [PubMed] [Google Scholar]
- 16.Helito CP, do Amaral C, da Nakamichi YC, Gobbi RG, Bonadio MB, Natalino RJM, Pécora JR, Cardoso TP, Camanho GL, Demange MK. Why do authors differ with regard to the femoral and meniscal anatomic parameters of the knee anterolateral ligament? Orthop. J. Sport. Med. 2016. [DOI] [PMC free article] [PubMed]
- 17.Herbst E, Albers M, Burnham JM, Fu FH, Musahl V. The anterolateral complex of the knee. Orthop. J. Sport. Med. 2017;5:2325967117730805. doi: 10.1177/2325967117730805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Herbst E, Arilla FV, Guenther D, Yacuzzi C, Rahnemai-Azar AA, Fu FH, Debski RE, Musahl V. Lateral extra-articular tenodesis has no effect in knees with isolated anterior cruciate ligament injury. Arthroscopy. 2018;34:251–260. doi: 10.1016/j.arthro.2017.08.258. [DOI] [PubMed] [Google Scholar]
- 19.Hewison CE, Tran MN, Kaniki N, Remtulla A, Bryant D, Getgood AM. Lateral extra-articular tenodesis reduces rotational laxity when combined with anterior cruciate ligament reconstruction: a systematic review of the literature. Arthroscopy. 2015;31:2022–2034. doi: 10.1016/j.arthro.2015.04.089. [DOI] [PubMed] [Google Scholar]
- 20.Huser LE, Noyes FR, Jurgensmeier D, Levy MS. Anterolateral ligament and iliotibial band control of rotational stability in the anterior cruciate ligament-intact knee: defined by tibiofemoral compartment translations and rotations. Arthroscopy. 2017;33:595–604. doi: 10.1016/j.arthro.2016.08.034. [DOI] [PubMed] [Google Scholar]
- 21.Ibrahim SA, Shohdy EM, Marwan Y, Ramadan SA, Almisfer AK, Mohammad MW, Abdulsattar WS, Khirat S. Anatomic reconstruction of the anterior cruciate ligament of the knee with or without reconstruction of the anterolateral ligament: a randomized clinical trial. Am. J. Sports Med. 2017;45:1558–1566. doi: 10.1177/0363546517691517. [DOI] [PubMed] [Google Scholar]
- 22.Inderhaug E, Stephen JM, Williams A, Amis AA. Biomechanical comparison of anterolateral procedures combined with anterior cruciate ligament reconstruction. Am. J. Sports Med. 2017;45:347–354. doi: 10.1177/0363546516681555. [DOI] [PubMed] [Google Scholar]
- 23.Kaeding CC, Pedroza AD, Reinke EK, Huston LJ, Spindler KP. Risk factors and predictors of subsequent ACL injury in either knee after ACL reconstruction: prospective analysis of 2488 primary ACL reconstructions from the MOON cohort. Am. J. Sports Med. 2015;43:1583–1590. doi: 10.1177/0363546515578836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kittl C, El-Daou H, Athwal KK, Gupte CM, Weiler A, Williams A, Amis AA. The role of the anterolateral structures and the ACL in controlling laxity of the intact and ACL-deficient knee. Am. J. Sports Med. 2016;44:345–354. doi: 10.1177/0363546515614312. [DOI] [PubMed] [Google Scholar]
- 25.Lemaire M, Combelles F. Plastic repair with fascia lata for old tears of the anterior cruciate ligament (author’s transl) Rev. Chir. Orthop. Reparatrice Appar. Mot. 1980;66:523–525. [PubMed] [Google Scholar]
- 26.Marcacci M, Zaffagnini S, Iacono F, Neri MP, Loreti I, Petitto A. Arthroscopic intra- and extra-articular anterior cruciate ligament reconstruction with gracilis and semitendinosus tendons. Knee Surg. Sports Traumatol. Arthrosc. 1998;6:68–75. doi: 10.1007/s001670050075. [DOI] [PubMed] [Google Scholar]
- 27.Monaco E, Fabbri M, Mazza D, Daggett M, Redler A, Lanzetti RM, De Carli A, Ferretti A. The effect of sequential tearing of the anterior cruciate and anterolateral ligament on anterior translation and the pivot-shift phenomenon: a cadaveric study using navigation. Arthroscopy. 2018;34:1009–1014. doi: 10.1016/j.arthro.2017.09.042. [DOI] [PubMed] [Google Scholar]
- 28.Monaco E, Maestri B, Conteduca F, Mazza D, Iorio C, Ferretti A. Extra-articular ACL reconstruction and pivot shift: In vivo dynamic evaluation with navigation. Am. J. Sports Med. 2014;42:1669–1674. doi: 10.1177/0363546514532336. [DOI] [PubMed] [Google Scholar]
- 29.Muller W. The Knee: Form, Function, and Ligament Reconstruction. New York: Springer; 1983. [Google Scholar]
- 30.• Musahl V, Burnham J, Lian J, Popchak A, Svantesson E, Kuroda R, Zaffagnini S, Samuelsson K, Sheean A, Burnham JM, Lian J, Smith C, Popchak A, Herbst E, Pfeiffer T, Araujo P, Oostdyk A, Guenther D, Ohashi B, Irrgang JJ, Musahl V, Fu FH, Nagamune K, Kurosaka M, Hoshino Y, Kuroda R, Grassi A, Muccioli GMM, Lopomo N, Signorelli C, Raggi F, Zaffagnini S, Svantesson E, Senorski EH, Sundemo D, Bjoernsson H, Ahlden M, Desai N, Samuelsson K, Karlsson J. High-grade rotatory knee laxity may be predictable in ACL injuries. Knee Surgery, Sport. Traumatol. Arthrosc. 2018. Clinical series suggesting a correlation between changes to lateral knee kinematics and those sustaining an ACL injury with concomitant lateral meniscus damage [DOI] [PubMed]
- 31.Musahl V, Rahnemai-Azar AA, Costello J, Arner JW, Fu FH, Hoshino Y, et al. The influence of meniscal and anterolateral capsular injury on knee laxity in patients with anterior cruciate ligament injuries. Am. J. Sports Med. 2016. [DOI] [PubMed]
- 32.Neri T, Palpacuer F, Testa R, Bergandi F, Boyer B, Farizon F, Philippot R. The anterolateral ligament: anatomic implications for its reconstruction. Knee. 2017;24:1083–1089. doi: 10.1016/j.knee.2017.07.001. [DOI] [PubMed] [Google Scholar]
- 33.Noyes FR, Barber SD. The effect of an extra-articular procedure on allograft reconstructions for chronic ruptures of the anterior cruciate ligament. J. Bone Joint Surg. Am. 1991;73:882–892. [PubMed] [Google Scholar]
- 34.Noyes FR, Huser LE, Levy MS. Rotational knee instability in ACL-deficient knees: role of the anterolateral ligament and iliotibial band as defined by tibiofemoral compartment translations and rotations. J. Bone Joint Surg. Am. 2017;99:305–314. doi: 10.2106/JBJS.16.00199. [DOI] [PubMed] [Google Scholar]
- 35.Parsons EM, Gee AO, Spiekerman C, Cavanagh PR. The biomechanical function of the anterolateral ligament of the knee. Am. J. Sports Med. 2015;43:669–674. doi: 10.1177/0363546514562751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pernin J, Verdonk P, Si Selmi TA, Massin P, Neyret P. Long-term follow-up of 24.5 years after intra-articular anterior cruciate ligament reconstruction with lateral extra-articular augmentation. Am. J. Sports Med. 2010;38:1094–1102. doi: 10.1177/0363546509361018. [DOI] [PubMed] [Google Scholar]
- 37.Pfeiffer TR, Burnham JM, Hughes JD, Kanakamedala AC, Herbst E, Popchak A, Shafizadeh S, Irrgang JJ, Debski RE, Musahl V. An increased lateral femoral condyle ratio is a risk factor for anterior cruciate ligament injury. J. Bone Jt. Surg. 2018;100:857–864. doi: 10.2106/JBJS.17.01011. [DOI] [PubMed] [Google Scholar]
- 38.Rahnemai-Azar AA, Abebe ES, Johnson P, Labrum J, Fu FH, Irrgang JJ, Samuelsson K, Musahl V. Increased lateral tibial slope predicts high-grade rotatory knee laxity pre-operatively in ACL reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2017;25:1170–1176. doi: 10.1007/s00167-016-4157-3. [DOI] [PubMed] [Google Scholar]
- 39.Rasmussen MT, Nitri M, Williams BT, Moulton SG, Cruz RS, Dornan GJ, Goldsmith MT, LaPrade RF. An in vitro robotic assessment of the anterolateral ligament, Part 1: Secondary role of the anterolateral ligament in the setting of an anterior cruciate ligament injury. Am. J. Sports Med. 2016;44:585–592. doi: 10.1177/0363546515618387. [DOI] [PubMed] [Google Scholar]
- 40.Rezende Fernando Cury, de Moraes Vinicius Ynoe, Martimbianco Ana Luiza Cabrera, Luzo Marcus Vinícius, da Silveira Franciozi Carlos Eduardo, Belloti João Carlos. Does Combined Intra- and Extraarticular ACL Reconstruction Improve Function and Stability? A Meta-analysis. Clinical Orthopaedics and Related Research®. 2015;473(8):2609–2618. doi: 10.1007/s11999-015-4285-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rosenstiel N, Praz C, Ouanezar H, Saithna A, Fournier Y, Hager J-P, Thaunat M, Sonnery-Cottet B. Combined Anterior Cruciate and Anterolateral Ligament Reconstruction in the Professional Athlete: Clinical Outcomes From the Scientific Anterior Cruciate Ligament Network International Study Group in a Series of 70 Patients With a Minimum Follow-Up of 2 Years. Arthroscopy. 2019;35:885–892. doi: 10.1016/j.arthro.2018.09.020. [DOI] [PubMed] [Google Scholar]
- 42.Runer A, Birkmaier S, Pamminger M, Reider S, Herbst E, Künzel KH, et al. The anterolateral ligament of the knee: a dissection study. Knee. 2016. [DOI] [PubMed]
- 43.Sabzevari S, Rahnemai-Azar AA, Albers M, Linde M, Smolinski P, Fu FH. Anatomic and histological investigation of the anterolateral capsular complex in the fetal knee. Am. J. Sports Med. 2017;45:1383–1387. doi: 10.1177/0363546517692534. [DOI] [PubMed] [Google Scholar]
- 44.Saiegh Y, Al SEM, Guenther D, Hawi N, Decker S, Krettek C, Citak M, Omar M. Sectioning the anterolateral ligament did not increase tibiofemoral translation or rotation in an ACL-deficient cadaveric model. Knee Surg. Sports Traumatol. Arthrosc. 2017;25:1086–1092. doi: 10.1007/s00167-015-3787-1. [DOI] [PubMed] [Google Scholar]
- 45.Samuelson M, Draganich LF, Zhou X, Krumins P, Reider B. The effects of knee reconstruction on combined anterior cruciate ligament and anterolateral capsular deficiencies. Am. J. Sports Med. 1996;24:492–497. doi: 10.1177/036354659602400414. [DOI] [PubMed] [Google Scholar]
- 46.Slette EL, Mikula JD, Schon JM, Marchetti DC, Kheir MM, Turnbull TL, LaPrade RF. Biomechanical results of lateral extra-articular tenodesis procedures of the knee: a systematic review. Arthroscopy. 2016;32:2592–2611. doi: 10.1016/j.arthro.2016.04.028. [DOI] [PubMed] [Google Scholar]
- 47.Sommer C, Friederich NF, Muller W. Improperly placed anterior cruciate ligament grafts: correlation between radiological parameters and clinical results. Knee Surg. Sports Traumatol. Arthrosc. 2000;8:207–213. doi: 10.1007/s001670000125. [DOI] [PubMed] [Google Scholar]
- 48.Song GY, Hong L, Zhang H, Zhang J, Li Y, Feng H. Clinical outcomes of combined lateral extra-articular tenodesis and intra-articular anterior cruciate ligament reconstruction in addressing high-grade pivot-shift phenomenon. Arthroscopy. 2016;32:898–905. doi: 10.1016/j.arthro.2015.08.038. [DOI] [PubMed] [Google Scholar]
- 49.Song GY, Zhang H, Wang QQ, Zhang J, Li Y, Feng H. Risk Factors associated with grade 3 pivot shift after acute anterior cruciate ligament injuries. Am. J. Sports Med. 2016. [DOI] [PubMed]
- 50.Sonnery-Cottet B, Daggett M, Fayard JM, Ferretti A, Helito CP, Lind M, Monaco E, de Pádua VBC, Thaunat M, Wilson A, Zaffagnini S, Zijl J, Claes S. Anterolateral Ligament Expert Group consensus paper on the management of internal rotation and instability of the anterior cruciate ligament - deficient knee. J. Orthop. Traumatol. 2017;18:91–106. doi: 10.1007/s10195-017-0449-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sonnery-Cottet B, Lutz C, Daggett M, Dalmay F, Freychet B, Niglis L, Imbert P. The involvement of the anterolateral ligament in rotational control of the knee. Am. J. Sports Med. 2016;44:1209–1214. doi: 10.1177/0363546515625282. [DOI] [PubMed] [Google Scholar]
- 52.Sonnery-Cottet B, Saithna A, Cavalier M, Kajetanek C, Temponi EF, Daggett M, Helito CP, Thaunat M. Anterolateral ligament reconstruction is associated with significantly reduced ACL graft rupture rates at a minimum follow-up of 2 years: a prospective comparative study of 502 patients from the SANTI Study Group. Am. J. Sports Med. 2017;45:1547–1557. doi: 10.1177/0363546516686057. [DOI] [PubMed] [Google Scholar]
- 53.Sonnery-Cottet B, Thaunat M, Freychet B, Pupim BHB, Murphy CG, Claes S. Outcome of a combined anterior cruciate ligament and anterolateral ligament reconstruction technique with a minimum 2-year follow-up. Am. J. Sports Med. 2015;43:1598–1605. doi: 10.1177/0363546515571571. [DOI] [PubMed] [Google Scholar]
- 54.Spencer L, Burkhart TA, Tran MN, Rezansoff AJ, Deo S, Caterine S, Getgood AM. Biomechanical analysis of simulated clinical testing and reconstruction of the anterolateral ligament of the knee. Am. J. Sports Med. 2015;43:2189–2197. doi: 10.1177/0363546515589166. [DOI] [PubMed] [Google Scholar]
- 55.Stijak L, Bumbasirevic M, Radonjic V, Kadija M, Puskas L, Milovanovic D, Filipovic B. Anatomic description of the anterolateral ligament of the knee. Knee Surg. Sports Traumatol. Arthrosc. 2016;24:2083–2088. doi: 10.1007/s00167-014-3422-6. [DOI] [PubMed] [Google Scholar]
- 56.Terry GC, Hughston JC, Norwood LA. The anatomy of the iliopatellar band and iliotibial tract. Am. J. Sports Med. 1986;14:39–45. doi: 10.1177/036354658601400108. [DOI] [PubMed] [Google Scholar]
- 57.Thaunat M, Clowez G, Saithna A, Cavalier M, Choudja E, Vieira TD, Fayard J-M, Sonnery-Cottet B. Reoperation rates after combined anterior cruciate ligament and anterolateral ligament reconstruction: a series of 548 patients from the SANTI Study Group with a minimum follow-up of 2 years. Am. J. Sports Med. 2017;45:2569–2577. doi: 10.1177/0363546517708982. [DOI] [PubMed] [Google Scholar]
- 58.Thein R, Boorman-Padgett J, Stone K, Wickiewicz TL, Imhauser CW, Pearle AD. Biomechanical Assessment of the Anterolateral Ligament of the Knee: A Secondary Restraint in Simulated Tests of the Pivot Shift and of Anterior Stability. J. Bone Joint Surg. Am. 2016;98:937–943. doi: 10.2106/JBJS.15.00344. [DOI] [PubMed] [Google Scholar]
- 59.Tisherman R, Meredith S, Vaudreuil N, de Sa D, Musahl V. Instability following ACL rupture: what do we need to restore during reconstruction. Ger. J. Sport. Med. 2019;70:31–36. [Google Scholar]
- 60.Vaudreuil NJ, Rothrauff BB, de Sa D, Musahl V. The pivot shift: current experimental methodology and clinical utility for anterior cruciate ligament rupture and associated injury. Curr. Rev. Musculoskelet. Med. 2019;12:41–49. doi: 10.1007/s12178-019-09529-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wright RW, Magnussen RA, Dunn WR, Spindler KP. Ipsilateral graft and contralateral ACL rupture at five years or more following ACL reconstruction: a systematic review. J. Bone Joint Surg. Am. 2011;93:1159–1165. doi: 10.2106/JBJS.J.00898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zaffagnini Stefano, Signorelli Cecilia, Grassi Alberto, Hoshino Yuichi, Kuroda Ryosuke, de SA Darren, Sundemo David, Samuelsson Kristian, Musahl Volker, Karlsson Jon, Sheean Andrew, Burnham Jeremy M., Lian Jayson, Smith Clair, Popchak Adam, Herbst Elmar, Pfeiffer Thomas, Araujo Paulo, Oostdyk Alicia, Guenther Daniel, Ohashi Bruno, Irrgang James J., Fu Freddie H., Nagamune Kouki, Kurosaka Masahiro, Marcheggiani Muccioli Giulio Maria, Lopomo Nicola, Raggi Federico, Svantesson Eleonor, Hamrin Senorski Eric, Bjoernsson Haukur, Ahlden Mattias, Desai Neel. Anatomic Anterior Cruciate Ligament Reconstruction Using Hamstring Tendons Restores Quantitative Pivot Shift. Orthopaedic Journal of Sports Medicine. 2018;6(12):232596711881236. doi: 10.1177/2325967118812364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zaffagnini S, Signorelli C, Lopomo N, Bonanzinga T, Muccioli GMM, Bignozzi S, Visani A, Marcacci M. Anatomic double-bundle and over-the-top single-bundle with additional extra-articular tenodesis: an in vivo quantitative assessment of knee laxity in two different ACL reconstructions. Sport. Traumatol. Arthrosc: Knee Surgery; 2012. [DOI] [PubMed] [Google Scholar]
- 64.Zarins B, Rowe CR. Combined anterior cruciate-ligament reconstruction using semitendinosus tendon and iliotibial tract. J. Bone Joint Surg. Am. 1986;68:160–177. [PubMed] [Google Scholar]