Abstract
Purpose of Review
Forward head posture (FHP) is the most common cervical postural fault in the sagittal plane that is found with different severity levels in almost all populations. Despite claims that FHP may be related to neck pain, this relation seems to be controversial. Thus, our purpose is to determine whether FHP differs between asymptomatic subjects and those with neck pain and to investigate if there is a relationship between head posture and neck pain.
Recent Findings
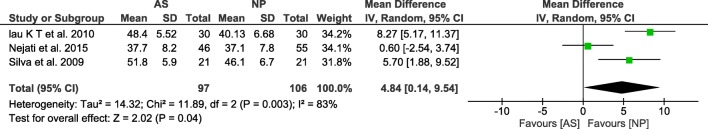
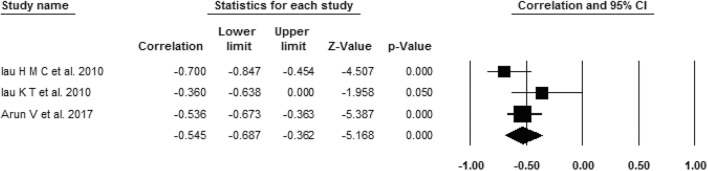
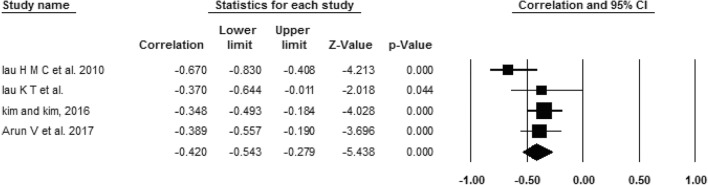
A total of 15 cross-sectional studies were eligible for inclusion for this systematic review and meta-analysis. Ten studies compared FHP between a group of asymptomatic participants and a group of participants with neck pain and an overall mean difference (MD) of 4.84 (95% CI = 0.14, 9.54), indicating a significant between-group difference, contrary to adolescent (MD = − 1.05; 95% CI = − 4.23, 2.12). Eight studies showed significant negative correlations between FHP and neck pain intensity (r = − 0.55; 95% CI = − 0.69, − 0.36) as well as disability (r = − 0.42; 95% CI = − 0.54, − 0.28) in adults and older adults, while in adolescents, only lifetime prevalence and doctor visits due to neck pain were significant predictors for FHP.
Summary
This systematic review found that age played an important role as a confounding factor in the relation between FHP and neck pain. Also, the results showed that adults with neck pain show increased FHP when compared to asymptomatic adults and that FHP is significantly correlated with neck pain measures in adults and older adults. No association was found between FHP and most of neck pain measures in adolescents.
Keywords: Systematic review, Meta-analysis, Neck pain, Forward head, Posture
Introduction
Neck pain is a common complaint in the population, with a considerable impact on individuals and their families, communities, health-care systems, and businesses [1, 2, 3•]. The estimated 1-year incidence of neck pain ranges between 10.4 and 21.3%, and the overall prevalence of neck pain in general population can be as high as 86.8% [2, 3•]. Neck pain has an episodic occurrence with variable recovery between episodes [4], and it is considered the most persistent musculoskeletal pain syndrome [5]. Neck pain can be associated to serious conditions such as neurological conditions, infections, neoplasms, and fractures of the cervical spine, or it can be idiopathic (neck pain without unknown cause) [6].
Strong evidence was found to relate neck pain with female gender, older age, being an ex-smoker, high job demands, and low social or work support [7, 8]. Regarding physical work factors, neck pain was significantly associated with holding the neck in a forward bent posture for a prolonged time and making repetitive movements [9]. In addition, the increasing use of new information and communication technologies has led to an increase in time spent texting messages on mobile phones or using computers, which might have a long-term impact on neck pain, potentially due to prolonged periods of neck flexion [10•].
Neck flexion may facilitate forward head posture (FHP) [11], which refers to forward placement of the head in relation to the shoulder. This is the most common cervical postural fault in the sagittal plane that is found with different severity levels in almost all populations [12]. Greater FHP has been associated with greater deficits in cervical range of motion, particularly neck rotation and flexion [13, 14]. Also, FHP seems to have a negative impact on static balance control in asymptomatic adults [15]. Despite claims that FHP may be related to neck pain, existing evidence seems controversial, since some previous studies have reported no significant associations between neck pain and FHP [16–18], whereas other studies have reported an association between FHP and neck pain [19–21].
A previous systematic review compared surrogate measures for head posture in individuals with and without neck pain. This review did not reach a clear conclusion as the included studies reported contradictory results [22]. These contradictory results may be explained by the poor methodological quality and inadequate reporting of data of included studies [22, 23]. Hence, it is necessary to update the systematic review of Silva et al. [22] to determine whether the latest published research can clarify this controversy. Thus, the primary aim of this study was to determine whether FHP differs between neck pain and asymptomatic subjects. A secondary aim was to investigate if there is a relationship between head posture and neck pain.
Methods
This systematic review was registered on PROSPERO (PROSPERO 2017: CRD CRD42018081494) and conducted according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [24].
Information Sources and Search Strategy
The electronic databases EMBASE, MEDLINE/PubMed, Cochrane Library Web search, Physiotherapy Evidence Database (PEDro), and CINAHL were searched for observational studies published in English and indexed from 2009 to April 2017, and updated search was performed on 19 September 2018. The search strategy consisted of a mix of free-text terms and Medical Subject Headings (MeSH). The details of the search strategy are shown in Appendix Table 4. Reference lists of the relevant articles were also searched.
Table 4.
Search strategy and number of founded papers in each database
| Database | No. of papers | Keywords |
|---|---|---|
| PubMed | 786 | ((((((((((((((cervical posture) OR cervical postures) OR forward head posture) OR forward head postures) OR forward posture) OR forward postures) OR head posture) OR head postures) OR neck posture) OR neck postures) OR neck posturing) OR forward head tilt) AND (“2009/01/01”[PDat]: “2018/09/19”[PDat]) AND English[lang])) AND ((((((((((((((neck pain) OR cervical pain) OR neck ach) OR neck disability) OR Bournemouth Neck Questionnaire) OR Cervical Spine Outcomes Questionnaire) OR Copenhagen Neck Functional Disability Scale) OR (Neck Pain and Disability Scale)) OR Northwick Park Neck Pain Questionnaire) OR Neck disability index) OR acute neck pain) OR chronic neck pain) OR “Neck Pain”[Mesh]) AND (“2009/01/01”[PDat]: “2018/09/19”[PDat]) AND English[lang]) |
| Cochrane | 241 | Neck pain or cervical pain or neck ach or neck disability or “Bournemouth Neck Questionnaire” or “Cervical Spine Outcomes Questionnaire” or “Copenhagen Neck Functional Disability Scale” or “Neck Pain and Disability Scale” or “Northwick Park Neck Pain Questionnaire” or “Neck disability index” or MeSH descriptor: [Neck Pain] explode all trees AND cervical posture or forward head posture or forward posture or head posture or neck posture or forward head tilt AND Publication Year from 2009 to 2018, in Trials and Methods Studies (Word variations have been searched) |
| PEDro | 5 | Key words (head posture*AND neck pain) advanced search, Publication Year from 2009, clinical trials, Subdiscipline: musculoskeletal, topic: chronic pain, body parts: head or neck |
| EMBASE | 164 | (‘neck’:ab,ti AND ‘pain’:ab,ti OR ‘cervical pain’:ab,ti OR ‘neck ach’:ab,ti OR ‘neck disability’:ab,ti OR ‘bournemouth neck questionnaire’:ab,ti OR ‘cervical spine outcomes questionnaire’:ab,ti OR ‘copenhagen neck functional disability scale’:ab,ti OR (‘neck pain’:ab,ti AND ‘disability scale’:ab,ti) OR ‘northwick park neck pain questionnaire’:ab,ti OR ‘neck disability index’:ab,ti) AND (‘head and posture’:ab,ti OR ‘cervical posture’:ab,ti OR ‘forward head posture’:ab,ti OR ‘forward posture’:ab,ti OR ‘neck posture’:ab,ti OR ‘forward head tilt’:ab,ti OR ‘head position’:ab,ti) AND [English]/lim AND [2009-2018]/py |
| CINAHL | 95 | ((((((((((((((((neck pain) OR cervical pain) OR neck ach) OR neck disability) OR Bournemouth Neck Questionnaire) OR Cervical Spine Outcomes Questionnaire) OR Copenhagen Neck Functional Disability Scale) OR (Neck Pain and Disability Scale)) OR Northwick Park Neck Pain Questionnaire) OR Neck disability index) OR acute neck pain) OR chronic neck pain)) AND (((((((((((((cervical posture) OR cervical postures) OR forward head posture) OR forward head postures) OR forward posture) OR forward postures) OR head posture) OR head postures) OR neck posture) OR neck postures) OR neck posturing) OR forward head tilt)); published date: 2009 January 1 to 2018 December 31, language: English |
We searched the databases from 2009 because this systematic review is considered an update of a previously published review [22] and is being undertaken in the light of the publication as a significant new research with some modifications in the research questions as well as inclusion and exclusion criteria. The inclusion and exclusion criteria are shown in (Table 1).
Table 1.
Eligibility criteria of the included studies
| Studies were eligible for inclusion if | |
|
• Transversal or longitudinal studies evaluating the relationship between sagittal head posture and idiopathic neck pain (observational studies) • Investigating FHP in individuals with idiopathic neck pain (described as neck pain of unknown origin and described as a posterior pain perceived in the region below the superior nuchal line, above the spine of the scapula) [4] • The comparison group included pain-free subject (described with no history or current neck pain) • Involving individuals with acute or chronic idiopathic neck pain of any age group • The primary outcome of interest was FHP (measured as distances or angles between anatomical landmarks). Secondary outcomes include neck pain measures (e.g., severity, frequency, duration, and/or disability) assessed using validated instruments | |
| Studies were excluded if | |
|
• Neck pain has a specific underlying pathology such as fractures, rheumatoid arthritis, osteoporosis, or whiplash injuries as well as neck pain associated with radiculopathy • Including the assessment of dynamic FHP (during working or using visual display terminals) • Including participants with neck pain and other concomitant complaints (e.g., patients who suffered from neck pain and headache) • In languages other than English • Conference proceedings, editorials, letters, and poster presentations |
Study Selection
All titles and abstracts were imported into Mendeley Desktop© (version 1.17.6) through which we removed duplicates and irrelevant articles that did not meet the inclusion criteria. Two reviewers (NF and KH) independently identified papers as relevant based on eligibility criteria. Lists from both reviewers were compared, and papers identified by both authors were obtained in full text. Discrepancies in judgment were resolved by consensus. A third reviewer (AGS) acted as arbiter.
Data Extraction
Two reviewers (NF and KH) independently extracted the appropriate data. They compared their findings to verify whether all appropriate data were successfully extracted. We also contacted the primary authors for additional data and/or clarification of data, when needed.
Quality Assessment
Three researchers (AGS, KH, and NF) independently assessed the quality of selected articles by using an adapted form of the Effective Public Health Practice Project (EPHPP) assessment tool which was developed by Thomas et al. [25]. This tool was chosen because it had been used previously in adapted form for recording quality of similar studies [22, 26]. To avoid conflict of interest, 2 articles were assessed by 2 researchers only (KA and NF) as the third researcher (AGS) was one of the authors of these two articles [27, 28]. Discrepancies in assessment were solved by discussion until consensus was reached.
The quality assessment tool has eight components: sample selection, study design, confounders, blinding of outcome assessors and participants, reliability and validity of data collection tools, appropriateness of sample size, withdrawals, dropouts, and accuracy of data analysis. Each component was rated strong, moderate, or weak according to the adapted EPHPP. Each paper then received a global rating. This global rating was “strong, moderate, and weak.” All studies were included in this review regardless of its quality.
Statistical Methods
For comparative meta-analyses, we analyzed data from the included studies using Review Manager (RevMan, version 5.2; Nordic Cochrane Center, Cochrane Collaboration, Copenhagen, Denmark) and Microsoft Excel 2010 (Microsoft Corp., Redmond, WA, USA). A formal meta-analysis was conducted for all comparative outcomes. We expressed pooled continuous effect measures as the mean difference (MD) with 95% CI through random-effects model. We explored and quantified between-study statistical heterogeneity using the I2 test (which describes true variation across studies as a percentage, where values around 25% indicate low, 50% medium, and 75% high heterogeneity among studies) [29]. Subgroup analyses were performed with the studies that used the same age group. We categorized the studies into adolescent (less than 18 years), adults (18 years to 50 years), and older adults (above 50 years).
For correlative outcomes, we did meta-analyses according to Goh et al.’s [30] methodology by using comprehensive meta-analysis software (version 3). The correlation coefficient from each study was Fisher z transformed to be suitable for pooling. Standard error and 95% CI were calculated for each r value; then, the weighted mean was calculated (weight depended on the sample size). z and χ2 values were then calculated to determine the p value of the overall effect across the studies. All z-transformed r values and their CI were reversed again for representation. Heterogeneity across the studies was determined using Cochran’s Q which was transformed into I2 percent with its p value. Publication bias could not be tested because of the small number of included studies [30].
Results
Search Results
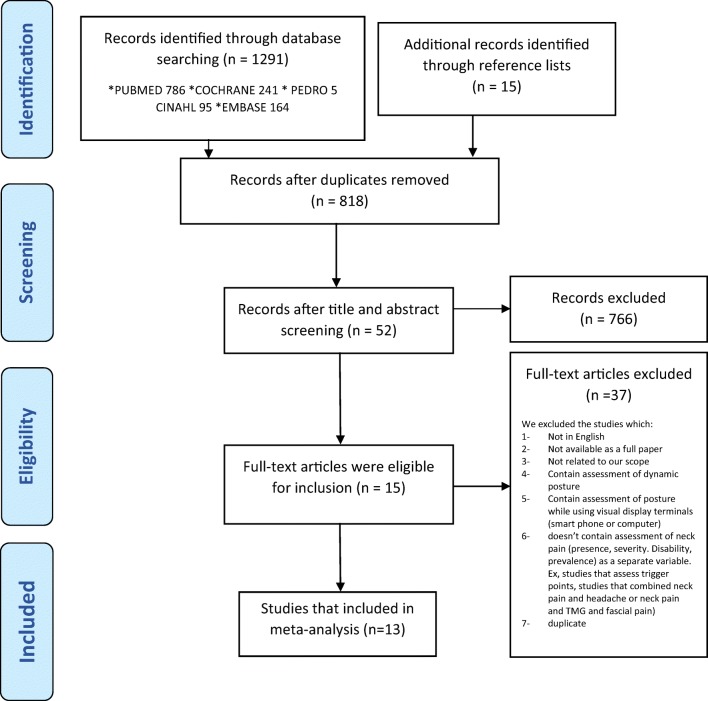
The search of selected databases provided a total of 1292 references. After excluding for duplicates as well as title, abstract, and full-text review finally, a total of 15 studies were eligible to be included in this review (Fig. 1). The agreement between the 2 reviewers who screened the references was 81%. Thirteen of the 15 studies provided data for meta-analysis.
Fig. 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow chart
Characteristics of Included Studies
Ten studies were cross-sectional studies (compared FHP between a group of participants with neck pain and a group of asymptomatic participants) [27, 28, 31–38], while four papers were cross-sectional without a comparison group (presented correlation data between FHP and neck pain) [39–42] and one study investigated the correlation between four postural clusters and neck pain [43]. Of the ten studies that presented comparative data, 3 studies presented correlational data also [28, 32, 33]. A summary of the retrieved data of the included articles is presented in Table 2.
Table 2.
Summary of demographic data of participants, methodology, and results of the eligible studies
| Studies | Design of study | Demographic of symptomatic and asymptomatic subjects | FHP measures | Position | NP assessment measures | NP characteristics | AS characteristics | Statistical tests | Results | Conclusion |
|---|---|---|---|---|---|---|---|---|---|---|
| Silva et al. (2009) | Cross section with comp |
NP group: N = 40 (6 M 34 F) Age = 50.2 ± 7.9 (33–69) H = 159.0 ± 7.0 cm W = 69.0 ± 11.0 kg |
Craniocervical angle (CVA) and gaze angle by video camera | Standing | VAS, frequency, duration, and pain location within preceding week (special questionnaire) | Current NP for more than 6 months | No current NP and reported they had never had NP for more than 3 consecutive days | MANOVA |
For CVA • Older (NP, 44.8° ± 7.1°; PF, 45.1° ± 6.7°) • Younger (NP, 46.1° ± 6.7°; PF, 51.8° ± 5.9°)* • All participants (NP, 45.4° ± 6.8°; PF 48.6° ± 7.1°)* • For gaze angle (NP, 21.0° ± 6.4°; PF, 18.8° ±7.7°) |
Patients with chronic non-traumatic NP aged 50 years or below had a more forward standing head posture than pain-free individuals, whereas there was no difference between these groups for older participants. No difference was found between groups for head extension |
|
AS group: N = 40 (6 M 34 F) Age = 50.2 ± 7.9 (34–68) H = 160.0 ± 8.2 cm W = 65.5 ± 12.7 kg | ||||||||||
| Oliveira and Silva (2016) | Cross section with comp |
NP group: N = 35 (25 F, 10 M) Age = 16.6 ± 0.7 H = 168.4 ± 8.9 W = 59.9 ± 11.2 |
CVA by goniometer and a bubble level | Standing | VAS at the moment, frequency in the previous week, duration, disability (single question) | Chronic idiopathic NP that was present at least once a week during the last 3 months | AS had no current pain and reported that they had never had NP | MANOVA, Spearman’s correlation |
FHP (NP, 46.62° ± 4.92°; AS, 44.18° ± 3.64°)*, correlation • FHP and pain duration = 0.13 • FHP and pain frequency = 0.10 • FHP and pain intensity = 0.12 |
Adolescents with NP have less FHP compared to asymptomatic participants, but no relation between FHP and NP duration, frequency, and intensity |
|
AS group: N = 35 (22 F, 13 M) Age = 16.7 ± 0.7 H = 167.0 ± 9.6 W = 64.5 ± 14.4 | ||||||||||
| Nagai et al. (2014) | Cross section with comp |
NP group: N = 27 M Age = 34.5 ± 6.4 (18–55) H = 176.9 ± 7.1 W = 84.8 ± 11.2 |
CROM | Sitting | NPRS and NDI as well as duration (days) were reported for the worst episode of NP in the past 12 months | A history of NP and over 100 flight hours in the past 12 months | Without a history of NP and over 100 flight hours in the past 12 months | Either paired t tests or Wilcoxon signed-rank tests | NP = 22.1 (1.5), AS = 21.7 (1.6) cm | No significant difference between both groups |
|
AS group: N = 27 M Age = 34.3 ± 6.1 H = 177.3 ± 8.5 W = 83.0 ± 12.0 | ||||||||||
| Mani et al. (2017) | Cross section with comp |
NP group: N = 16 (2 M, 14 F) Age = 27.9 ± 16.0 (10–65) H = 1.56 ± 0.11 m W = 60 ± 19.50 kg BMI =24.31 ± 6.50 |
CVA and gaze angle by photo | Standing | Who experienced neck pain in the 6 months prior to the study were recruited? | No history of neck pain in the 6 months prior to the commencement of the study | Independent-samples t test |
Sagittal head tilt angle (gaze angle) (NP = 19.89 ± 5.56, AS = 16.35 ± 8.33)* CVA (NP = 43.54 ± 6.63, AS = 47.43 ± 7.97) |
The CCA was lower in subjects with neck pain than normal subjects indicating FHP. Subjects with NP demonstrated high sagittal head tilt angle indicating greater upper cervical extension | |
|
AS group: N = 15 (5 M, 10 F) Age = 24.73 ± 6.3 (17–40) H = 1.60 ± 0.09 m W = 57 ± 16.4 kg BMI =22.5 ± 8.50 | ||||||||||
| Lau et al. (2010) | Cross section with comp |
NP group: N = 30 (20 F, 10 M) Age = 36.77 (23–46) |
CVA by photo | Sitting | NPRS and NPQ | NP intensity > 3 on the NPRS; they had a score > 10% on the NPQ | Not suffered from NP in the past 6 months; they scored 0 on NPRS and less than 10% on NPQ | t test; Spearman’s correlation; with the control of age and gender, multiple logistic and linear regression |
• CVA (AS = 48.40 ± 5.52, NP = 40.13 ± 6.68)* • The CVA was negatively correlated with the presence of neck pain (r = − 0.56) • Significantly negative correlation between the NPRS and NPQ, with CV angle (0.36, 0.37) • The upper thoracic angle (OR = 1.37) and the CV angle (OR = 0.86) were significant predictors for the presence of neck pain |
Subjects with NP had a smaller CV angle. CVA was an acceptable predictor for the presence of neck pain. The cervical spine had a significant correlation with NP severity and disability |
|
AS group: N = 30 (13 F, 17 M) Age = 34.50 (24–47) | ||||||||||
| Dunleavy et al. (2015) | Cross section with comp |
NP group: N = 20 F Age-51.8 (35–69) H = 65.9 (2.7) in. W = 157.3 (34.9) kg |
Upper cervical angle (UCA), distance by CROM | Habitual sitting posture | NDI | If they reported NP of ≥ 3/10 NDI for more than 3 months | Independent-samples t tests |
• FHP distances [AS = 17.5 (3), NP = 16.2 (2.7)] (cm) • The UCA measurements [AS = 93.4 (7.2), NP = 99.1 (6.6)]* (°) |
Individuals with pain exhibited a significantly more extended UCA than age-matched asymptomatic individuals without pain, while there were no differences in FHP distances between the groups | |
|
AS group: N = 20 F Age = 51.7 (35–69) H = 64.7 (2) in. W = 161 (33) | ||||||||||
| Cheung et al. (2010) | Cross section with comp |
NP group: N = 30 (13 M, 17 F) Age = 14.47 ± 0.2 (13–18) H = 1.62 (1.77) W = 52.36 (1.43) BMI = 19.90 (0.38) |
CVA by HPSCI | Standing | VAS and NPQ | Had experienced pain over the neck region in the past 3 months | ANOVA | The unloaded CVA (NP = 60.03 ± 9.05, AS = 57.10 ± 5.00) | There was no significant difference (p > 0.05) in the unloaded CV angles between the neck pain group and non-neck pain | |
|
AS group: N = 30 (17 M, 13 F) Age = 14.43 ± 0.18 H = 1.65 (1.43) W = 57.25 (2.14) | ||||||||||
| Negati et al. (2015) | Cross section with comp |
NP group: N = 55 (40 F, 15 M) Age = 38 (all 39 ± 8) H = 169.00 W = 70.00 |
CVA by photo | Sitting | Location and duration of NP by survey | Chronic NP for a period of over 3 months | All the other employees were included in the asymptomatic group | Independent-samples t test, ANOVA, MANOVA, univariate and multivariate analyses |
• CVA (NP = 37.1 ± 7.8, AS = 37.70 ± 8.20) • HTA (NP = 118.3 ± 7.9, AS = 117.00 ± 8.60) • There were also correlations between the sagittal posture of cervical and thoracic spine (CVA, HTA) and neck pain |
No significant difference between both groups during looking forward |
|
AS group: N = 46 (33 F, 13 M) Age = 39 H = 165.00 W = 68.00 | ||||||||||
| Helgadottir et al. (2011) | Cross section with comp |
NP group: N = 21 (19 F and 2 M) Age = 35.23 (25–54) H = 170.5 W = 73.01 |
Cranial, cervical angles, by a 3-space FasTrak device | Sitting | NDI and VAS over the past 7 days | A score of at least 10 on the NDI and neck symptoms of more than 6 months | No cervical and shoulder dysfunction and a score below 10 on the NDI are scored as “no disability” | General linear model one-way ANOVA, the correlation (NR) |
• A significant difference was also observed in the cranial angle (p < 0.01) and a tendency in the cervical angle (p = 0.07) • The correlation between the dependent variables and the scores on the NDI and VAS was found to be weak (r < 0.50) • Significantly decreased cranial angle in the IONP group (p = 0.02) and the WAD group (p = 0.03) compared with the control group |
Reduced cranial angle in patients with NP compared with asymptomatic subjects |
|
AS group: N = 20 (17 F and 3 M) Age = 29.7 (21–51) H = 171.83 W = 69.30 | ||||||||||
| Ruivo et al. (2014) | Cross section with comp |
N = 275 (122 M, 153 F) Age = 15–17 (15.76 ± 1.08) |
CVA and gaze angle by photo | Standing | Presence of NP by single question | Independent-samples t test; a chi-square test was used to assess the relationship between the forward head and cervical pain |
• The overall mean CVA (NP = 46.5 ± 5.6, AS = 47.9 ± 4.79) * • HT angle (NP = 16.4 ± 5.7, AS = 17.6 ± 5.7) • Adolescents with FH than adolescents without FH (29.8% vs 8.4%) • Girls cervical angle (NP = 45.81 ± 5.6, AS = 47.38 ± 4.76°)* |
• The overall NP group showed a significantly lower mean CV angle • No statistically significant difference was found between patients and pain-free participants for the HT angle • Neck pain was more prevalent in adolescents with FH than adolescents without FH • Girls with NP also reported a significantly lower cervical angle than the girls without NP |
||
| Kim and Kim (2016) | Cross section |
N = 126 (95 M, 31 F) Age = 19–24 (23.9 ± 1.5) H = 172.3 ± 6.4 cm W = 69.1 ± 13.9 kg |
CVA by photo | Standing and sitting | NDI | NR | NR | Pearson’s correlation |
• NDI (mild disability range) • Correlation CVA and NDI in standing position (r = − 0.35)* • Correlation CVA and NDI in sitting (r = − 0.33) |
A significant negative correlation of CVA (standing or sitting) with NDI |
| Lau et al. (2010) | Cross section |
N = 30 (14 M, 16 F) Age = 46.7 ± 9.5 (27–59) |
CVA and AHT by EPHI and X-ray | Standing | NP rating scale (NPRS) and the Chinese version of (NPQ) | Mechanical NP for at least 3 m without referral | Pearson’s correlation |
• AHT with NPQ (r = 0.39) • AHT with NPRS (r = 0.49) • CVA with NPQ (r = − 0.67) • CVA with NPRS (r = − 0.70) |
• Moderate positive correlation of AHT with NPQ and NPRS and a negative correlation of CV angle with NPQ and NPRS | |
| Dolphens et al. (2012) | Cross section |
N = 1196 (639 M and 557 F) Boys’ age = 12.6 ± 0.54 (11.4–15.0) years Girls’ age = 10.6 ± 0.47 (9.6–13.0) years |
CVA by photo | Standing | Questionnaire (lifetime and 1 month prevalence and doctor visit of NP) | Univariate analysis and binary logistic regression |
• In boys, a lifetime prevalence of NP: the CVA (OR = 0.954; 95% CI = 0.924–0.985; p = 0.004) • In girls, a doctor visit for NP: the CVA (OR = 0.905; 95% CI = 0.824–0.994; p = 0.037) |
• In boys, the CVA and the trunk lean angle are significant predictors of lifetime prevalence of NP. • In girls, the CVA is a significant predictor of doctor visit for NP |
||
| Richards et al. (2016) | Cross section as a part of cohort |
N = 1108 (548 F, 560 M) Age = 17.0 ± 0.2 H = 172 (9) cm W = 67 (14) BMI = 23 (4) |
Neck flexion, cervicothoracic, craniocervical angle and head displacement By photo |
Sitting |
The questionnaire (adapted from the NPQ) included the following: • Presence • Persistent NP • NP worse with sitting |
Multivariable logistic regression after adjusting for the potential confounding variables |
• Presence of persistent NP and posture clusters (p = 0.741) • Neck pain made worse by sitting and posture clusters (p = 0.262) |
There was no significant difference between the clusters and the presence of persistent NP. Also, the odds of neck pain made worse by sitting did not differ among the clusters | ||
| Arun et al. (2017) | Cross section |
N = 84 (57 M, 27 F) Age = 20–40 |
CVA by MHPSCI | Sitting | VAS, NPQ | Mild to moderate neck pain subjects | A Pearson’s correlation coefficient |
• The CV angle with the VAS (r = − 0.536)* • The CV angle with the NPQ (r = − 0.389)* |
A significantly moderate negative correlation of CVA with NP intensity and a significantly weak negative correlation with disability |
Craniovertebral angle = C7, tragus, and horizontal/cervical angle = neck flexion angle = C7, tragus, and vertical/tragus, eye, and horizontal = gaze angle = sagittal head angle (HT)/tragus, eye, and vertical = cranial angle = head flexion angle
comp comparison, NP neck pain, VAS visual analogue scale, NDI Neck Disability Index, NPQ Neck Pain Questionnaire, AHT anterior head translation, HPSCI Head Posture Spinal Curvature Instrument, MHPSCI Modified Head Posture Spinal Curvature Instrument, CROM cervical range of motion device
Each (*) in the table refer to significant effect size and it explained in the (conclusion) column
Quality Assessment
Results from using the EPHPP quality assessment tool are shown in Table 3. Eight studies were rated of moderate quality while 7 were rated of weak quality. The most common limitations include the following: not using an appropriate sample size, uncontrolled confounding factors, and using a neck pain assessment tool that was not shown to be valid. Eight studies used appropriate sample size [27, 33, 35, 36, 40–43], and only two of them performed a priori sample size calculation [27, 33].
Table 3.
Quality assessment of the included studies
| Studies | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | Final rating |
|---|---|---|---|---|---|---|---|---|---|
| Silva et al. (2009) | W | S | S | M | M | S | S | S | Moderate |
| Oliveira and Silva (2016) | M | M | S | W | S | W | S | S | Moderate |
| Nagai et al. (2014) | W | M | S | W | M | W | S | M | Weak |
| Mani et al. (2017) | W | M | W | W | W | W | S | W | Weak |
| Lau et al. (2010) | W | M | S | W | S | W | S | S | Weak |
| Dunleavy et al. (2015) | W | M | S | W | S | W | S | M | Weak |
| Cheung et al. (2010) | S | S | M | M | M | W | S | M | Moderate |
| Nejati et al. (2015) | M | M | M | W | W | M | S | M | Moderate |
| Helgadottir et al. (2011) | W | S | S | M | W | S | S | M | Moderate |
| Ruivo et al. (2014) | M | M | M | M | M | M | S | M | Moderate |
| Kim and Kim (2016) | W | M | W | W | W | M | S | M | Weak |
| Lau et al. (2010) | W | M | W | M | S | W | S | M | Weak |
| Dolphens et al. (2012) | S | M | M | W | W | M | S | S | Moderate |
| Richards et al. (2016) | S | M | S | W | W | M | S | S | Moderate |
| Arun et al. (2017) | W | M | W | W | M | M | S | M | Weak |
1, selection bias; 2, study design; 3, controlling confounders; 4, blinding; 5, data collection methods; 6, sample size; 7, withdrawals; 8, analyses (S = strong, M = moderate, W = weak)
Included studies controlled for different confounding factors: six studies controlled for both age and sex [27, 32–34, 37, 43], while two studies controlled for sex only [35, 40] or for age only [28] and six studies did not control for sex or age [31, 36, 38, 39, 41, 42].
Three studies did not measure or report on the reliability of the FHP measuring tool [33, 40, 41], while six studies did not use a valid instrument to assess neck pain [34–36, 38, 40, 43].
Meta-Analysis
Overall FHP Difference Between Neck Pain and Asymptomatic Participants
A total of 10 articles performed comparisons between neck pain and asymptomatic groups: seven out of these 10 articles measured the craniovertebral angle (CVA; the angle between C7, tragus, and horizontal) [27, 28, 31, 32, 35, 36, 38], one study measured the complementary angle of CVA (angle between C7, tragus, and vertical) [33], and 2 studies used a cervical range of motion (CROM) device to measure FHP distance and upper cervical angle (UCA), which represents the angle between vertical, occipite, and nose, measured by a sagittal inclinometer on the CROM device [34, 37].
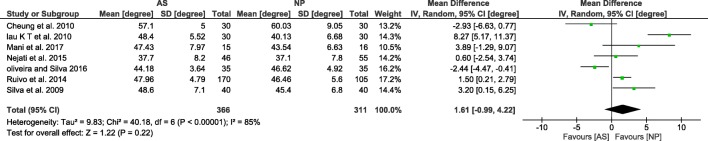
The data of seven studies (n = 677 participants) which compared CVA between asymptomatic and neck pain subjects with different age groups showed high heterogeneity across studies. The pooled MD was 1.61 (95% CI = − 0.99, 4.22), which indicates that there was no statistically significant difference in the FHP between asymptomatic and neck pain subjects (Fig. 2).
Fig. 2.
Overall CVA difference between asymptomatic (AS) and neck pain (NP) participants
Helgadottir et al. [33] also compared the FHP between asymptomatic and neck pain adults and found no statistically significant difference between the 2 groups (p = 0.07), although the exact data was not reported [33]; we contact the author of this study, but we did not receive response; therefore, this study was not included in the meta-analysis.
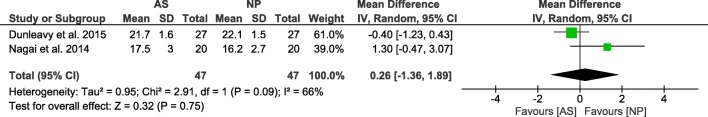
Nagai et al. [34] and Dunleavy et al. [37] investigated the combined sample of adults and older adults using the CROM device. The pooled mean difference was 0.26 (95% CI = − 1.36, 1.89), which showed no statistically significant difference in FHP by using the CROM device [34, 37]. The heterogeneity across studies was moderate (Fig. 3). Unexpectedly, Dunleavy et al. [37] found a significant difference on the same sample for the UCA as a surrogate measure for FHP.
Fig. 3.
Forest plot of comparison. Comparison between asymptomatic (AS) and neck pain (NP) adult and older adults, using the CROM device
Subgroup Analysis According to Age of Studies that Measured CVA and Pooled Results
Of the seven studies that measured CVA, 3 studies included adolescents [28, 31, 35], 2 studies included adults [32, 36], one study included adults and older adults with subgroup analysis [27], and one study included a wide age range sample (adolescent, adults, and older adults); therefore, this study was not included in subgroup analysis [38].
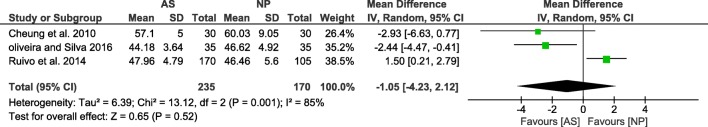
FHP in Adolescent
The data showed high heterogeneity across studies (3 studies, n = 405). The pooled mean difference was − 0.05 (95% CI = − 4.23, 2.12), indicating no statistically significant difference in FHP between adolescents with and without neck pain (Fig. 4).
Fig. 4.
Forest plot of comparison. Comparison between asymptomatic (AS) and neck pain (NP) participants (outcome: CVA in adolescents)
FHP in Adults
The data showed high heterogeneity across studies (3 studies, n = 203). The pooled mean difference was 4.84 (95% CI = 0.14, 9.54), indicating that there was a statistically significant difference in FHP between adults with neck pain and asymptomatic adults; i.e., adults with neck pain showed a more FHP than asymptomatic adults (Fig. 5).
Fig. 5.
Forest plot of comparison. Comparison between asymptomatic (AS) and neck pain (NP) participants (outcome, 1.1 CVA in adults)
FHP in Older Adults
Only one of the eligible studies (n = 38) performed a subgroup analysis using age as a factor and reported that CVA was not significantly different between asymptomatic and neck pain adults aged more than 50 years old (NP, mean ±SD = 44.8° ± 7.1°; AS, mean ± SD = 45.1° ± 6.7°; F1,36 < 1.0, p > 0.05) [27].
Upper Cervical Posture
The angle between the tragus, the eye, and the horizontal (or its complementary angle) is believed to reflect the posture of the upper cervical spine and is called gaze angle or sagittal head angle. Four studies compared this angle between asymptomatic and neck pain subjects [27, 33, 35, 38]. Each study showed data for a different age group; Ruivo et al. [35] included adolescents, Helgadottir et al. [33] included adults, Silva et al. [27] included adults and older adults, while Mani et al. [38] included broad unmatched age range (adolescents, adults, and older adults). Three studies showed no between-group significant difference, and one study found a statistically significant increased head extension in the neck pain group compared with the asymptomatic group (p = 0.02) [33].
Correlation Between FHP and Neck Pain Measures
Correlation in Adolescents
Three studies measured the relationship between CVA and pain measures in adolescents. Oliveira and Silva [28] measured the relationship between neck pain intensity and CVA in adolescent, and the results showed no significant correlation (r = 0.12, p > 0.05). Beside intensity, there is absence of significant correlations between pain duration and frequency in the previous week and CVA. Another study examined 1108 adolescents as follow-up to the Pregnancy Cohort Study (http://www.rainestudy.org.au), which classified head posture into 4 clusters: upright, intermediate, slumped thorax/forward head, and erect thorax/forward head. In this study, multivariable logistic regression was used, adjusting for the potential confounding variables, to estimate associations between posture clusters and persistent neck pain as well as to investigate whether sitting worsened neck pain. The results showed no association between pain measures and posture clusters [43], while Dolphens et al. [40] used logistic regression analyses on 639 boys and 557 girls to study the association between CVA and lifetime prevalence, 1-month prevalence, and doctor visits due to neck pain. The results showed that the CVA was a significant predictor for lifetime prevalence and doctor visits due to neck pain. The increased CVA was associated with an approximately 5% decrease in odds of lifetime prevalence of neck pain in boys (OR = 0.95; 95% CI = 0.92–0.99; p = 0.004). Also, a 1° increase in CVA had a 9.0% decrease in odds of having sought medical help for neck pain in girls (OR = 0.91; 95% CI = 0.82–0.99; p = 0.04) [40]. The variability of neck pain measures, methodology, and analysis procedure prevented us from performing a meta-analysis.
Correlation in Adults and Older Adults Between CVA and Neck Pain Intensity
Three cross-sectional studies (n = 144) reported negative correlation coefficients between neck pain intensity and CVA in adults and older adults. The pooled correlation was significant (r = − 0.55; 95% CI = − 0.69, − 0.36; p < 0.001). The heterogeneity across studies was insignificant (Q = 3.26; p = 0.195; I2 = 38.74%) in a random-effect model. Lau et al. [32] also found that the CVA was negatively correlated (r = − 0.56; p < 0.01) with the presence of neck pain. The CVA was a predictor for the presence of neck pain (OR = 0.86; p = 0.04) after adjusting for age and gender (Fig. 6).
Fig. 6.
Meta-analysis of the correlation between neck pain intensity and CVA in adults and old age
Correlation in Adults and Older Adults Between CVA and Neck Pain Disability
Four cross-sectional studies (n = 270) reported negative correlation coefficients between neck pain disability and CVA in adults and older adults. The pooled correlation was significant (r = − 0.420; 95% CI = − 0.543, − 0.279; p < 0.001). The heterogeneity across studies was insignificants (Q = 4.539; p = 0.209; I2 = 33.906%) in a random-effect model (Fig. 7).
Fig. 7.
Meta-analysis of correlation between neck pain disability and CVA in adults and older adults
No study measured the relation between neck pain intensity/disability and FHP in older adults separately, but Lau et al. [39] measured this relation in a combined sample of adults and older adults and found a significant negative correlation between CVA and neck pain intensity and disability (r = − 0.7 and r = − 0.67; p < 0.001), respectively, and a positive correlation between anterior head translation (AHT) and pain intensity (r = 0.49; p = 0.006) as well as disability (r = 0.39; p = 0.033).
Discussion
The purpose of the current review was to determine whether FHP differs between neck pain and asymptomatic subjects and to investigate if there is a relationship between head posture and neck pain. The results showed that adults with neck pain have significantly more FHP than asymptomatic adults. In contrast, no significant difference was found for FHP between adolescents with and without neck and between adults with and without neck pain who aged 50 years old or more. In addition, a significant correlation between FHP and neck pain intensity/disability in adults and older adults was also found, but not in adolescents except for neck pain lifetime prevalence and number of doctor visits.
FHP Difference Between Subjects With and Without Neck Pain
The absence of a significant difference for FHP between adolescents with and without neck pain compares favorably with the results of a recent systematic review targeting studies on adolescents only [44••]. However, there was a statistically significantly high heterogeneity (I2 = 85%) among studies, which decreases the confidence on results. The high heterogeneity may be due to different assessment methods and characteristics of neck pain measures in each study.
In adults, the meta-analysis showed adults with neck pain to have increased FHP. However, the high heterogeneity (I2 = 83%) among studies decreases the confidence on these results. A previous systematic review [22] was inconclusive about this difference in adults due to contradictory results of the retrieved studies. Recent studies included in the present review were of better quality than those included in the review of Silva et al. [22]. Recent studies are better at reporting the characteristics of neck pain, exclusion criteria, and selection process. In addition, recent studies are also better in terms of using valid and reliable methods to measure FHP. Nevertheless, some of these recent studies still lack controlling for confounders.
The findings of the current study suggest that increasing FHP in adults with neck pain but no difference in adolescents may be due to adults who presume more flexed posture than young when performing the same tasks [45]. Maintaining a high flexion angle of the neck during work leads to an increase in the weight of the head [46] which put extra load on the spine and lead to changes in ligaments, tendons, and muscle which may progressively cause permanent changes of posture in the form of FHP [47].
Despite adolescents potentially spending more time hunched on visual display terminals as cell phone or maintaining neck flexion during studying [48], the short-term effects are not noticeable [49•]. In contrast, there are appears to be long-term effects in terms of decreased neck muscle flexibility and endurance in adolescent predisposing to neck pain in adults [48].
Increasing FHP in adults with neck pain may be associated with lower endurance of the deep neck flexors and extensors and with a higher activity of superficial muscles compared with those without neck pain [50, 51]. A systematic review by Andias and Silva [44••] also reported a significant difference in muscle function between adolescents with and without neck pain, but the magnitude of changes tends to be lower than that found in adults.
Also, FHP is related to decreased cervical range of motion (ROM) [13, 14]. Adults showed progressively decreased cervical ROM through aging especially in the third and fourth decades [52]. Differences in ROM between subjects with and without neck pain are different in adults and in adolescent. Adults with neck pain have significantly decreased ROM for all cervical movements when compared with asymptomatic participants [53•]. In contrast, in adolescents, neck pain is associated with decreased ROM for some neck movements but no for others [44••].
Among Adults aged 50 years or older, there was no difference for FHP between asymptomatic and neck pain subjects. This result is based on one study only, which performed subgroup analysis according to participants’ age [27]. This result may be explained by the progressive deterioration of the cervicothoracic posture with age in both subjects with and without neck pain. This deterioration peaks during the fourth decade in subjects with neck pain and no further deterioration in the fifth decade [54].
Different surrogate measures of FHP may also influence the results. The study of Dunleavy et al. [37] showed contradictory results for the same sample when using different posture assessment methods. In this study, individuals with pain exhibited a significantly more extended UCA (CROM) than age-matched asymptomatic individuals without pain, while there were no differences in CROM FHP distances between the groups. The results from this study do not support the use of CROM FHP measurements in naturally assumed seated postures based on moderate criterion validity and reliability and minimal detectable change values.
Correlation Between FHP and Neck Pain Measures
A total of 8 articles presented correlation data between pain measures and FHP. In adolescents, three studies showed no significant correlation between FHP and pain measures (presence, intensity, duration, frequency, 1-month prevalence). Even though each study reported different combinations of neck pain measures, there was consistency among the reported results. The quality of these studies was moderate and based on a large sample size (n = 2339). Only lifetime prevalence and doctor visits due to neck pain were significant predictors for FHP, and these two measures were sex dependent.
Despite the high prevalence of neck pain in adolescents, which was reported in the previous epidemiological studies [2], our data suggested that most of neck pain measures in adolescent are not associated with static posture. That may be because natural head posture reproducibility is still high in this age group and decreases with increasing age [55] or the neck pain related to psychological distress or decreased fitness [5].
But in adults and older adults, we found a significant correlation between FHP and neck pain intensity (r = − 0.545; I2 = 38.74) as well as disability (r = − 0.42; I2 = 33.9), indicating that increased neck pain is associated with increased FHP. The magnitude of this correlation seems to increase for older participants (r = − 0.7 for intensity and r = − 0.67 for disability) [39], suggesting that age affects the strength of the correlation between FHP and neck pain, but more studies are needed to confirm these findings.
Since all the eligible studies were cross-sectional, the causal relationship is not possible to establish. Future longitudinal studies are needed to answer the temporality question; which come first, neck pain or FHP. To our knowledge, this is the first systematic review and meta-analysis aiming to quantify the strength of the relationship between FHP and neck pain measures.
It has been clear that age impacts the association between neck pain and FHP. Several authors considered age an important confounding factor affecting this relation [17, 54, 56–58]. However, age was not controlled in many of the included studies either by matching age between groups or statistically [31, 35, 36, 38–42]. It was considered a source of bias and may affect results. Raine and Twomey [56] reported that 19% of the measurement variation of FHP could be accounted for by the effect of increasing age in asymptomatic subjects. Further studies are needed to clarify the changes of CVA and other FHP measures through the life span measuring specific age ranges.
Most studies in this review (thirteen out of fifteen articles) measured the craniocervical posture by CVA or its complementary. A decrease in this angle indicates a more FHP, and it is considered an accurate measure to discriminate FHP severity [59]. However, it does not provide an indication of the exact shape of the cervical spine (i.e., lordotic or non-lordotic) [60•]. Future studies are needed to study the relation between cervical posture subtypes and neck pain.
Concerning upper cervical posture, three of four studies investigated the upper cervical extension [27, 33, 38], but the difference was significant only in one of them which included only adults [33]. However, the age group (adolescents) and the unequal sample size between groups might have had an effect on the results of this study [35]. This finding is comparable to previous systematic review by Silva et al. [22] which reported similar contradictory results.
The definitions of subjects with and without neck pain were not consistent across included studies. The variability in definition possibly contributed to some heterogeneity between studies which was observed in the pooled analysis. Some of the included studies investigated current idiopathic neck pain experienced in the last 3 months or 6 months while other studies investigated a history of neck pain over 6 months or even a year which predisposes the results to recall bias and others identified presence of neck pain by a single (yes/no) question (Table 2).
Strengths and Limitations
One of the main strengths of this review was that we were able to provide a meta-analysis of differences of FHP between subjects with and without neck pain for different age groups, which was not provided in previous systematic reviews. Also, to the authors’ knowledge, this is the first systematic review estimating the relationship between neck pain measures and FHP.
The limitations in this review includes the studies in languages other than English, unpublished studies, and studies from non-indexed journals which may have been missed. Also, we contacted some original study authors for clarifications but received no response. Studies of low and moderate methodological quality were included in the meta-analysis, and subgroup analysis according to sex, position of assessment, instrumentations, and quality of the studies was not feasible because of the small number of retrieved studies.
Future Research
Despite the results that showed a significant difference of FHP between adults with and without pain and a significant association between FHP and neck pain in adults, it remains unknown if FHP could be the cause or a consequence of idiopathic neck pain in adults. So, we need high-quality longitudinal studies to investigate this causality and temporality.
We recommend using a clear definition for the neck pain severity (mild or moderate), duration (acute or chronic), frequency, as well as using valid instruments to determine severity and functional impairment due to neck pain in the future studies, because these simple differences can affect the relation between neck pain and FHP.
Authors should control the possible confounders that may affect neck pain or FHP such as age, sex, general anthropometry (height, weight, BMI), as well as other diseases and disorders. Also, authors should be clear how they controlled these confounders.
Conclusion
Age played an important role as a confounding factor in the relation between FHP and neck pain. Also, the results showed that adults with neck pain show increased FHP when compared to asymptomatic adults, and that FHP is significantly correlated with neck pain measures in adults and older adults. No association was found between FHP and neck pain in adolescents except for lifetime prevalence and number of doctor visits.
Appendix 1
Compliance with Ethical Standards
Conflict of Interest
Nesreen Fawzy, Karima A. Hassan, Salwa F. Abdelmajeed, Ibraheem M Moustafa, and Anabela G. Silva declare that they have no conflict of interest. However, one of them (AGS) is the author of four of the articles referenced here, two of which were included in this systematic review. To avoid conflict of interest, she was blind in the searching and filtering process and she did not contribute to the quality assessment of those two articles.
Human and Animal Rights
All reported studies with human subjects performed by one of the authors (AGS) have been previously published and complied with all applicable ethical standards.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Nesreen Fawzy Mahmoud, Email: dr_noonfawzy@yahoo.com, Email: dr_nesreenfawzy@cu.edu.eg.
Karima A. Hassan, Email: Karima.abdelaty@pt.cu.edu.eg
Salwa F. Abdelmajeed, Email: dr_salwa_fadl@live.com
Ibraheem M. Moustafa, Email: iabuamr@sharjah.ac.ae
Anabela G. Silva, Email: asilva@ua.pt
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Fejer R, Kyvik KO, Hartvigsen J. The prevalence of neck pain in the world population: a systematic critical review of the literature. Eur Spine J. 2006;15(6):834–848. doi: 10.1007/s00586-004-0864-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hoy DG, Protani M, De R, Buchbinder R. The epidemiology of neck pain. Best Pract Res Clin Rheumatol. 2010;24(6):783–792. doi: 10.1016/j.berh.2011.01.019. [DOI] [PubMed] [Google Scholar]
- 3.Genebra CVDS, Maciel NM, Bento TPF, Simeão SFAP, de Vitta A. Prevalence and factors associated with neck pain: a population-based study. Brazilian J Phys Ther. 2017;21(4):274–280. doi: 10.1016/j.bjpt.2017.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guzman J, Frcp C, Hurwitz EL, Carroll LJ, Haldeman S, Co P, et al. A new conceptual model of neck pain linking onset, course, and care: the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. Eur Spine J. United States. 2010;33(4):14–23. doi: 10.1097/BRS.0b013e3181643efb. [DOI] [PubMed] [Google Scholar]
- 5.Mikkelsson M, Salminen JJ, Kautiainen H. Non-specific musculoskeletal pain in preadolescents. Prevalence and 1-year persistence. Pain. 1997;73:29–35. doi: 10.1016/s0304-3959(97)00073-0. [DOI] [PubMed] [Google Scholar]
- 6.Australian Acute Musculoskeletal Pain Guidelines Group. Australian Academic Press; Brisbane. Evidence-based management of acute musculoskeletal pain: a guide clinicians Available from [Google Sch [Ref List. Australia: Australian Academic Press Pty. Ltd.; 2004;35–43.
- 7.McLean SM, May S, Klaber-Moffett J, Sharp DM, Gardiner E. Risk factors for the onset of non-specific neck pain: a systematic review. J Epidemiol Community Health England. 2010;64(7):565–572. doi: 10.1136/jech.2009.090720. [DOI] [PubMed] [Google Scholar]
- 8.Paksaichol A, Janwantanakul P, Purepong N, Pensri P, van der Beek AJ. Office workers’ risk factors for the development of non-specific neck pain: a systematic review of prospective cohort studies. Occup Environ Med England. 2012;69(9):610–618. doi: 10.1136/oemed-2011-100459. [DOI] [PubMed] [Google Scholar]
- 9.Cagnie B, Danneels L, Van Tiggelen D, De Loose V, Cambier D. Individual and work related risk factors for neck pain among office workers: a cross sectional study. Eur Spine J Berlin/Heidelberg: Springer-Verlag. 2007;16(5):679–686. doi: 10.1007/s00586-006-0269-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gustafsson E, Thomee S, Grimby-Ekman A, Hagberg M. Texting on mobile phones and musculoskeletal disorders in young adults: a five-year cohort study. Appl Ergon. 2017;58:208–214. doi: 10.1016/j.apergo.2016.06.012. [DOI] [PubMed] [Google Scholar]
- 11.Kang J-H, Park R-Y, Lee S-J, Kim J-Y, Yoon S-R, Jung K-I. The effect of the forward head posture on postural balance in long time computer based worker. Ann Rehabil Med. 2012;36(1):98–104. doi: 10.5535/arm.2012.36.1.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kendall FP, McCreary EK, Provance PJG, Rodgers MM, Romani RA, et al. Muscles testing and function with posture and pain. Fifth Edition. Lippincott Williams & Wilkins. 2005;49–118.
- 13.Quek J, Pua Y-H, Clark RA, Bryant AL. Effects of thoracic kyphosis and forward head posture on cervical range of motion in older adults. Man Ther. 2013;18(1):65–71. doi: 10.1016/j.math.2012.07.005. [DOI] [PubMed] [Google Scholar]
- 14.De-la-Llave-Rincón AI, Fernández-de-las-Peñas C, Palacios-Ceña D, Cleland JA. Increased forward head posture and restricted cervical range of motion in patients with carpal tunnel syndrome. J Orthop Sport Phys Ther. 2009;39(9):658–664. doi: 10.2519/jospt.2009.3058. [DOI] [PubMed] [Google Scholar]
- 15.J-H LEE. Effects of forward head posture on static and dynamic balance control. J Phys Ther Sci. 2016;28:274–277. doi: 10.1589/jpts.28.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harrison A, Barry-Greb T, Wojtowicz G. Clinical measurement of head and shoulder posture variables. J Orthop Sport Phys Ther. 1996;23(6):353–361. doi: 10.2519/jospt.1996.23.6.353. [DOI] [PubMed] [Google Scholar]
- 17.Visscher CM, Boer WDE, Lobbezoo F, Habets LLMH. Is there a relationship between head posture and craniomandibular pain? 2002;(1992). Available from: file:///C:/Users/ECA/AppData/Local/Mendeley Ltd./Mendeley Desktop/Downloaded/Visscher et al. - 2002 - Is there a relationship between head posture and craniomandibular pain.pdf. [DOI] [PubMed]
- 18.Hanten WP, Olson SL, Russell JL, Lucio RM, Campbell AH. Total head excursion and resting head posture: normal and patient comparisons. Arch Phys Med Rehabil [Internet] 2000;81(1):62–66. doi: 10.1016/s0003-9993(00)90223-5. [DOI] [PubMed] [Google Scholar]
- 19.Falla D, Jull G, Russell T, Vicenzino B, Hodges P. Effect of neck exercise on sitting posture in patients with chronic neck pain. Phys Ther. 2007;87(4):408–417. doi: 10.2522/ptj.20060009. [DOI] [PubMed] [Google Scholar]
- 20.Lau HMC, Chiu TTW, Lam T-H. Clinical measurement of craniovertebral angle by electronic head posture instrument: a test of reliability and validity. Man Ther. 2009;14(4):363–368. doi: 10.1016/j.math.2008.05.004. [DOI] [PubMed] [Google Scholar]
- 21.Yip CHT, Chiu TTW, Poon ATK. The relationship between head posture and severity and disability of patients with neck pain. Man Ther Scotland. 2008;13(2):148–154. doi: 10.1016/j.math.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 22.Silva AG, Sharples P, Johnson MI. Studies comparing surrogate measures for head posture in individuals with and without neck pain. Phys Ther Rev. 2010;15(1):12–22. doi: 10.1179/174328810X12647087218631. [DOI] [Google Scholar]
- 23.Edmondston Stephen SJ. For which patients with neck pain is posture analysis most relevant? Phys Ther Rev. 2010;15(2):112. [Google Scholar]
- 24.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and Meta-analyses: the PRISMA statement. Ann Intern Med Pr. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 25.Thomas B.H., Ciliska D., Dobbins M., Micucci S. A Process for Systematically Reviewing the Literature: Providing the Research Evidence for Public Health Nursing Interventions. Worldviews on Evidence-Based Nursing. 2004;1(3):176–184. doi: 10.1111/j.1524-475X.2004.04006.x. [DOI] [PubMed] [Google Scholar]
- 26.Olivo SA, Bravo J, Magee DJ, Thie NMR, Major PW, Flores-Mir C. The association between head and cervical posture and temporomandibular disorders: a systematic review. J Orofac Pain. 2006;20(November 2016):9–23. [PubMed] [Google Scholar]
- 27.Silva A, Punt TD, Sharples P, Vilas-Boas JP, Johnson MI. Head posture and neck pain of chronic nontraumatic origin: a comparison between patients and pain-free persons. Arch Phys Med Rehabil. 2009;90(4):669–674. doi: 10.1016/j.apmr.2008.10.018. [DOI] [PubMed] [Google Scholar]
- 28.Oliveira AC, Silva AG. Neck muscle endurance and head posture: a comparison between adolescents with and without neck pain. Man Ther J. 2016;22:62–67. doi: 10.1016/j.math.2015.10.002. [DOI] [PubMed] [Google Scholar]
- 29.Dersimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 30.Goh JX, Hall JA, Rosenthal R. Mini meta-analysis of your own studies: some arguments on why and a primer on how. Soc Personal Psychol Compass. 2016;10:535–549. [Google Scholar]
- 31.Cheung CH, Shum ST, Tang SF, Yau PC, Chiu TTW. The correlation between craniovertebral angle, backpack weights, and disability due to neck pain in adolescents. J Back Musculoskelet Rehabil. 2010;23(3):129–136. doi: 10.3233/BMR-2010-0259. [DOI] [PubMed] [Google Scholar]
- 32.Lau KT, Cheung KY, Chan Kwok B, Chan MH, Lo KY, Wing Chiu TT. Relationships between sagittal postures of thoracic and cervical spine, presence of neck pain, neck pain severity and disability. Man Ther. 2010;15(5):457–462. doi: 10.1016/j.math.2010.03.009. [DOI] [PubMed] [Google Scholar]
- 33.Helgadottir H, Kristjansson E, Mottram S, Karduna A, Jonsson HJ. Altered alignment of the shoulder girdle and cervical spine in patients with insidious onset neck pain and whiplash-associated disorder. J Appl Biomech. 2011;27(3):181–191. doi: 10.1123/jab.27.3.181. [DOI] [PubMed] [Google Scholar]
- 34.Nagai T, Abt JP, Sell TC, Clark NC, Smalley BW, Wirt MD, et al. Neck proprioception, strength, flexibility, and posture in pilots with and without neck pain history. Aviat Space Environ Med. 2014;85(5):529–535. doi: 10.3357/asem.3874.2014. [DOI] [PubMed] [Google Scholar]
- 35.Ruivo RM, Pezarat-Correia P, Carita AI. Cervical and shoulder postural assessment of adolescents between 15 and 17 years old and association with upper quadrant pain. Brazilian J Phys Ther. 2014;18(4):364–371. doi: 10.1590/bjpt-rbf.2014.0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nejati P, Lotfian S, Moezy A, Nejati M. The study of correlation between forward head posture and neck pain in iranian office workers. Int J Occup Med Environ Health. 2015;28(2):295–303. doi: 10.13075/ijomeh.1896.00352. [DOI] [PubMed] [Google Scholar]
- 37.Dunleavy K, Neil J, Tallon A, Adamo DE. Reliability and validity of cervical position measurements in individuals with and without chronic neck pain. J Man Manip Ther. 2015;23(4):188–196. doi: 10.1179/2042618614Y.0000000070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mani S, Sharma S, Omar B, Ahmad K, Muniandy Y, Singh DKA. Quantitative measurements of forward head posture in a clinical settings: a technical feasibility study. Eur J Physiother. 2017;19(3):119–123. [Google Scholar]
- 39.Lau HMC, Chiu TTW, Lam T-H. Measurement of craniovertebral angle with electronic head posture instrument: criterion validity. J Rehabil Res Dev. 2010;47(9):911–918. doi: 10.1682/jrrd.2010.01.0001. [DOI] [PubMed] [Google Scholar]
- 40.Dolphens M, Cagnie B, Coorevits P, Vanderstraeten G, Cardon G, D’hooge R, et al. Sagittal standing posture and its association with spinal pain: a school-based epidemiological study of 1196 Flemish adolescents before age at peak height velocity. Spine (Phila Pa 1976) 2012;37(19):1657–1666. doi: 10.1097/BRS.0b013e3182408053. [DOI] [PubMed] [Google Scholar]
- 41.Kim E-K, Kim JS. Correlation between rounded shoulder posture, neck disability indices, and degree of forward head posture. J Phys Ther Sci Japan. 2016;28(10):2929–2932. doi: 10.1589/jpts.28.2929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Subbarayalu Arun V., Ameer Mariam A. Relationships among head posture, pain intensity, disability and deep cervical flexor muscle performance in subjects with postural neck pain. Journal of Taibah University Medical Sciences. 2017;12(6):541–547. doi: 10.1016/j.jtumed.2017.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Richards KV, Beales DJ, Smith AJ, Sullivan PBO, Straker LM. Neck posture clusters and their association with biopsychosocial factors and neck pain in Australian adolescents. Phys Ther. 2016;96(10):1576–1588. doi: 10.2522/ptj.20150660. [DOI] [PubMed] [Google Scholar]
- 44.Andias R, Silva AG. A systematic review with meta-analysis on functional changes associated with neck pain in adolescents. Musculoskeletal Care. 2019;17:23–36. doi: 10.1002/msc.1377. [DOI] [PubMed] [Google Scholar]
- 45.Hsiao L, Cho C. The effect of aging on muscle activation and postural control pattern for young and older computer users. Appl Ergon. 2012;43(5):926–932. doi: 10.1016/j.apergo.2011.12.014. [DOI] [PubMed] [Google Scholar]
- 46.Hansraj KK. Assessment of stresses in the cervical spine caused by posture and position of the head (Abstract, materials and methods) Surg Technol Int. 2014;25:277–279. [PubMed] [Google Scholar]
- 47.Fares J, Fares MY, Fares Y. Musculoskeletal neck pain in children and adolescents: risk factors and complications. Surg Neurol Int. 2017;8:72. doi: 10.4103/sni.sni_445_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mikkelsson LO, Nupponen H, Kaprio J, Kautiainen H, Mikkelsson M. Adolescent flexibility, endurance strength, and physical activity as predictors of adult tension neck, low back pain, and knee injury: a 25 year follow up study. Br J Sport Med. 2006;40:107–113. doi: 10.1136/bjsm.2004.017350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Moreira G, Arthur D, Ferreira S, Alberto L, Nogueira C, José F, et al. Text neck and neck pain in 18–21-year-old young adults. Eur Spine J. 2018;27(6):1249–1254. doi: 10.1007/s00586-017-5444-5. [DOI] [PubMed] [Google Scholar]
- 50.Lee H, Nicholson LL, Adams RD. Neck muscle endurance, self-report, and range of motion data from subjectswith treated and untreated neck pain. J Manip Physiol Ther. 2005;28(1):25–32. doi: 10.1016/j.jmpt.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 51.Shahidi B, Johnson CL, Curran-everett D, Maluf KS. Reliability and group differences in quantitative cervicothoracic measures among individuals with and without chronic neck pain. BMC Musculoskelet Disord. 2012;13:215. doi: 10.1186/1471-2474-13-215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dvorak J, Antinnes JA, Panjabi M, Loustalot D, Bonomo M. Age and gender related normal motion of the cervical spine. Spine (Phila Pa 1976) 1992;17(105):5393–5398. doi: 10.1097/00007632-199210001-00009. [DOI] [PubMed] [Google Scholar]
- 53.Stenneberg MS, Rood M, de Bie R, Schmitt MA, Cattrysse E, Scholten-Peeters GG. To which degree differs active cervical range of motion between patients with neck pain, whiplash and healthy controls? A systematic review and metaanalysis. Arch Phys Med Rehabil. 2017;98(7):1407–1434. doi: 10.1016/j.apmr.2016.10.003. [DOI] [PubMed] [Google Scholar]
- 54.Kaur P, Pattnaik M, Mohanty PP. Relationship of cervicothoracic curvature with muscle strength and endurance in subjects with neck pain. Indian J Physiother Occup Ther. 2013;7(3):156–161. [Google Scholar]
- 55.Cooke MS, Hons B, Orth D, Eng DRCS, Edin FDSRCS. Five-year reproducibility of natural head posture: a longitudinal study. Am J Orthoo Dentofac Orthop. 1990;97:489–494. doi: 10.1016/S0889-5406(05)80029-0. [DOI] [PubMed] [Google Scholar]
- 56.Raine S, Twomey LT. Head and shoulder posture variations women and men. 1997;78(November). Available from: file:///C:/Users/ECA/AppData/Local/Mendeley Ltd./Mendeley Desktop/Downloaded/Raine, Twomey - 1997 - Head and Shoulder Posture Variations Women and Men(2).pdf. [DOI] [PubMed]
- 57.Sun A, Yeo HG, Kim TU, Hyun JK, Kim JY. Radiologic assessment of forward head posture and its relation to myofascial pain syndrome. Ann Rehabil Med. 2014;38(6):821–826. doi: 10.5535/arm.2014.38.6.821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Brink Y, Louw Q, Grimmer K, Jordaan E. The relationship between sitting posture and seated-related upper quadrant musculoskeletal pain in computing South African adolescents: a prospective study. Man Ther. Scotland. 2015;20(6):820–826. doi: 10.1016/j.math.2015.03.015. [DOI] [PubMed] [Google Scholar]
- 59.Salahzadeha Z, Maroufi N, Ahmadi A, Behtashb H, Razmjoo A, Gohari M, Parnianpour M. Assessment of forward head posture in females: observational and photogrammetry methods. J Back Musculoskelet Rehabil. 2014;27:131–139. doi: 10.3233/BMR-130426. [DOI] [PubMed] [Google Scholar]
- 60.Daffin L, Stuelcken M, Sayers M. Internal and external sagittal craniovertebral alignment: a comparison between radiological and photogrammetric approaches in asymptomatic participants. Musculoskelet Sci Pract. 2019;43:12–17. doi: 10.1016/j.msksp.2019.05.003. [DOI] [PubMed] [Google Scholar]