Abstract
Background:
Recent recommendations support more intensive postpartum care for women at risk for complications. Advanced maternal age (AMA) is associated with risk for adverse outcomes, but readmission risk based on maternal age is not well characterized.
Objective:
To evaluate risk for postpartum readmissions and associated severe morbidity by maternal age.
Methods:
This retrospective cohort study used the Nationwide Readmission Database to analyze 60-day all-cause postpartum readmission risk from 2010 to 2014. Risk for severe maternal morbidity (SMM) during readmission was ascertained using criteria from the Centers for Disease Control and Prevention. The primary exposure of interest was maternal age. Outcomes included time to readmission, risk of readmission, and risk for SMM during readmission. Multivariable log linear analyses adjusting for patient, obstetric, and hospital factors were conducted to assess readmission and SMM risk with adjusted risk ratios (aRR) with 95% confidence intervals (CI) as measures of effect.
Results:
Between 2010-2014, we identified 15.7 million deliveries, 15% of which were to women aged 35 or older. The 60-day all-cause readmission rate was 1.7%. Of these, 13% were complicated by SMM. Age-stratification revealed that women 35 and older were at increased risk for readmission and increased risk for SMM. The majority of readmissions occurred within the first 20 days regardless of age, although women 35 and older were more likely to be admitted within the first 10 days of discharge. Patients ages 35-39, 40-44, and >44 years had 9% (95% CI 7-10%), 37% (95% CI 34-39%), and 66% (95% CI 55-79%) significantly higher rates of postapartum readmission when compared to women age 25-29. Women 35-39, 40-44, and >44 years of age had a 15% (95% CI 10-21%), 26% (95% CI 18-34%), and 56% (95% CI 25-94%) higher risk of a readmission with SMM than women 25-29.
Conclusions:
AMA women are at higher risk for both postpartum readmission and severe morbidity during readmission. Women older than 35 years represent the group most likely to experience complications requiring readmission, with the highest risk age 40 and older.
INTRODUCTION
Over the past decade, births to women age 30 and over have risen while the overall birth rate has declined. Assisted reproductive technology and socioeconomic trends have resulted in women having children at later ages. From 2007 to 2016, birth rates rose 2% for women 30 to 34 thirties, 11% for women 35 to 39, and 19% for women 40 to 44.1 The birth rate for women 45 to 49 was 0.9 per 1,000 women in 2016, the highest rate for this age group since 1963.2 The trend of more frequent births among older women is likely to continue as reproductive technologies continue to improve and become more widely available.3
Maternal mortality and severe morbidity in the United States have been increasing over the same period with mortality doubling between 1990 and 2008 despite a global trend of overall decreased maternal mortality.4,5 Both poor neonatal outcomes and risk of maternal morbidity and mortality are directly correlated with increasing maternal age.6–13 Women at extremes of age are at greatest risk, with severe morbidity and mortality more than three times higher for women above 45 years of age compared to those in their mid to late 20s.14
Postpartum outcomes may be of increasing importance with a significant proportion of maternal mortality occurring after delivery.5,15,16 Severe maternal morbidity (SMM) has been increasing with more than 50,000 women annually experiencing severe morbidity an increasing proportion of which is postpartum.17 In the setting of these trends, there is evidence that postpartum care may be underutilized.18 Given that further characterization of postpartum adverse outcomes related to age may be useful in customizing care after delivery discharge, the purpose of this study was to examine risk for postpartum hospitalizations and severe complications by maternal age. The primary objective of this study was to characterize risk for all-cause postpartum readmission within 60 days of discharge from a delivery hospitalization based on the primary exposure of maternal age. The secondary objective of this study was to determine the association of age with risk for severe maternal morbidity during a readmission.
METHODS
Data Source
The 2010 to 2014 Nationwide Readmissions Database (NRD) was utilized for this study. The NRD is one of the largest all-payer databases and is assembled annually by the Healthcare Cost and Utilization Project and is comprised of state-level data with the ability to track patients across hospitalizations within a single state during a single year. The NRD contains a system of weights that allows for the estimation of national estimates representative of nearly 36 million discharges annually. The Columbia University and University of Southern California Institutional Review Boards granted exemptions for this research given that it is deidentified.
Study Population
All delivery hospitalization from 2010 to 2014 were identified using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes of 650 and V27.x. These codes ascertain >95% of delivery hospitalizations.19 Women ages 15 to 54 were included in this analysis. Because the NRD is year-based and cannot be linked across years, delivery hospitalizations occurring between January 1st and October 31st in each year were included. November and December hospitalizations were not included as readmissions during the subsequent 60 days could not be fully ascertained. Per Healthcare Cost and Utilization Project Data User Agreements, cell sizes <10 were not reported. In the case of a patient having multiple postpartum admissions, only the first readmission within 60-days was included in analysis.
Demographic, Clinical, and Hospital Factors
The NRD contains information regarding patient and hospital demographics that were utilized in this analysis. Patient demographic factors included payer information, maternal age, and median income quartile based on ZIP code. Hospital factors included hospital bed size and teaching status. Clinical factors were identified using ICD-9CM codes and included mode of delivery, diabetes status (pre-gestational, gestational, none), hypertensive status (hypertensive disease of pregnancy, chronic hypertension, and no hypertension), postpartum hemorrhage, chronic kidney disease, systemic lupus erythematosus, asthma, and multiple gestation.
Analysis
Demographic analyses were conducted stratified by age (15-17, 18-24, 25-29, 30-34, 35-39, 40-44, and >44 years of age) at time of delivery. Additionally, we stratified readmission delivery hospitalization discharge to readmission time interval by maternal age in 10 day increments (0-10 days, 11-20 days, 21-30 days, 31-40 days, 41-50 days, 51-60 days). For the primary analysis, we analyzed the relationship between maternal age and the risk of all-cause 60-day readmission. Univariable log-linear regression analyses were performed with unadjusted risk rations (RR) and 95% confidence intervals (CI) as measures of effect. Adjusted multivariable log-linear regression analysis was used to determine the effect of maternal age along with patient, hospital, and obstetrical risk factors for the primary outcome of 60-day all-cause readmission with adjusted risk ratios (aRR) and 95% CIs as measures of effect.
We conducted further analysis to assess the risk of delivery hospitalization severe maternal morbidity (SMM) as well as risk of SMM during readmission. We utilized the Centers for Disease Control and Prevention’s SMM composite that includes 17 conditions and 4 procedures ascertained via ICD-9-CM codes including eclampsia, stroke, shock, renal failure, and hysterectomy.20 For delivery SMM, we constructed a log-linear regression model adjusting for patient, hospital, and obstetrical risk factors. For readmission SMM, we constructed an adjusted log linear regression model excluding patients with SMM during their delivery hospitalization. Because there is a strong association between postpartum hemorrhage and transfusion during delivery, we eliminated postpartum hemorrhage from the adjusted model for delivery hospitalization SMM. Adjusted risk ratios were reported with 95% CI as the measures of effect. Population weights were applied to create national estimates. All analyses were performed using SAS 9.4 (SAS Institute, Cary, NC).
RESULTS
From 2010 to 2014, we identified 15.7 million deliveries. Patients >44 years of age comprised 0.2% of all delivery pregnancies, followed by 15-17 year olds (2.7%), 40-44 year olds (4.2%), 35-39 years old (10.6%), 30 to 34 year olds (25.6%), 25 to 29 year olds (28.3%), and 18-24 year olds (28.4%). Risk for medical and obstetric risk factors including pregestational and gestational diabetes, cesarean delivery, chronic hypertension, hypertensive diseases of pregnancy, cesarean delivery, and multiple gestation increased with maternal age (Table 1). Risk for SMM during all delivery hospitalizations was 1.9%. Risk for postpartum readmission within 60 days of a delivery hospitalization was 1.7%. Risk for SMM during all readmissions was 13.4%.
Table 1.
Demographics
| Maternal age (years) | 15-17 | 18-24 | 25-29 | 30-34 | 35-39 | 40-44 | 45-54 |
|---|---|---|---|---|---|---|---|
| Mean length of stay (days) | 2.7 | 2.6 | 2.6 | 2.7 | 2.9 | 3.1 | 3.8 |
| Readmitted within 60 days | 1.9% | 1.9% | 1.6% | 1.5% | 1.7% | 2.2% | 2.6% |
| Severe maternal morbidity (readmission) | 10.3% | 12.2% | 13.5% | 14.2% | 14.4% | 15.6% | 17.4% |
| Severe maternal morbidity (delivery) | 2.2% | 1.9% | 1.6% | 1.7% | 2.1% | 2.8% | 5.0% |
| Time to readmission | % | % | % | % | % | % | % |
| 10 or fewer days | 44.7% | 45.2% | 50.3% | 54.4% | 57.7% | 60.4% | 66.8% |
| 11-20 days | 15.1% | 15.8% | 15.6% | 16.1% | 15.8% | 15.5% | 13.3% |
| 21-30 days | 12.7% | 12.2% | 10.8% | 9.1% | 8.5% | 7.8% | 6.6% |
| 31-40 days | 11.1% | 10.1% | 8.7% | 7.7% | 6.5% | 6.4% | 6.4% |
| 41-50 days | 7.9% | 8.9% | 7.7% | 6.8% | 5.9% | 4.7% | 4.0% |
| 51-60 days | 8.6% | 7.9% | 7.0% | 5.9% | 5.6% | 5.3% | 2.9% |
| Payer | % | % | % | % | % | % | % |
| Medicare | 0.1% | 0.5% | 0.7% | 0.7% | 0.8% | 1.0% | 0.9% |
| Medicaid | 74.6% | 66.5% | 41.2% | 26.1% | 23.7% | 25.0% | 21.4% |
| Private insurance | 21.2% | 27.6% | 52.5% | 68.6% | 71.2% | 69.4% | 72.7% |
| Self-pay | 1.7% | 1.6% | 1.6% | 1.5% | 1.7% | 2.0% | 2.4% |
| No charge | 0.1% | 0.1% | 0.1% | 0.1% | 0.1% | 0.1% | 0.1% |
| Other | 1.9% | 3.5% | 3.7% | 3.0% | 2.5% | 2.4% | 2.3% |
| Median ZIP code income quartile | % | % | % | % | % | % | % |
| Lowest income quartile | 44.6% | 39.1% | 27.3% | 19.8% | 17.9% | 18.1% | 16.8% |
| 2nd lowest quartile | 26.3% | 27.8% | 25.9% | 21.8% | 19.7% | 19.3% | 17.8% |
| 2nd highest quartile | 19.4% | 21.5% | 26.1% | 26.7% | 25.9% | 25.2% | 24.1% |
| Highest income quartile | 8.5% | 10.5% | 19.8% | 30.8% | 35.4% | 36.2% | 39.8% |
| Asthma | 5.3% | 4.4% | 3.5% | 3.2% | 3.4% | 3.5% | 3.6% |
| Systemic lupus | 0.0% | 0.1% | 0.1% | 0.2% | 0.2% | 0.2% | 0.2% |
| Chronic renal disease | 0.3% | 0.3% | 0.3% | 0.3% | 0.3% | 0.3% | 0.4% |
| Multiple gestation | 0.8% | 1.2% | 1.7% | 2.3% | 2.8% | 3.3% | 11.8% |
| Delivery postpartum hemorrhage | 3.5% | 3.0% | 2.8% | 2.9% | 3.1% | 3.3% | 5.2% |
| Cesarean delivery | 19.6% | 27.4% | 31.8% | 36.0% | 41.6% | 47.7% | 61.1% |
| Pregestational diabetes | 0.4% | 0.6% | 0.8% | 1.1% | 1.7% | 2.2% | 2.7% |
| Gestational diabetes | 1.5% | 3.0% | 5.6% | 7.9% | 10.7% | 13.6% | 16.6% |
| Hypertensive diseases or pregnancy | 10.2% | 8.3% | 7.7% | 7.5% | 8.2% | 10.0% | 16.4% |
| Chronic hypertension | 0.3% | 0.8% | 1.5% | 2.1% | 3.0% | 4.6% | 6.2% |
| Hospital bed size | % | % | % | % | % | % | % |
| Small | 10.8% | 11.7% | 11.4% | 11.0% | 10.6% | 9.9% | 9.1% |
| Medium | 26.2% | 27.0% | 26.7% | 25.9% | 25.1% | 24.6% | 22.7% |
| Large | 63.0% | 61.3% | 61.9% | 63.1% | 64.3% | 65.6% | 68.2% |
| Hospital teaching status | % | % | % | % | % | % | % |
| Metropolitan non-teaching | 37.7% | 37.8% | 37.8% | 35.9% | 34.9% | 34.4% | 30.9% |
| Metropolitan teaching | 48.3% | 46.4% | 51.0% | 56.6% | 59.2% | 60.3% | 64.6% |
| Non-metropolitan | 14.0% | 15.8% | 11.2% | 7.5% | 6.0% | 5.4% | 4.5% |
When risk for SMM during delivery hospitalizations was stratified by maternal age risk was highest for women 45 and older (5.0%), followed by women 40 to 44 years of age (2.8%), followed by women 15 to 17 years of age (2.2%) (Table 1). Evaluating risk for readmission within 60 days of a delivery hospitalization, risk was highest among women 45 and older (2.6%), followed by women 40 to 44 (2.2%), followed by women 15 to 17 years of age (1.9%). Evaluating risk for SMM during a readmission hospitalization women 40 to 44 were again at highest risk (17.4%), followed by women 40 to 44 (15.6%), followed by women 35 to 39 years of age (14.4%). Women 15-17 years of age were least likely to experience severe morbidity during a readmission (10.3%). Evaluating the time from discharge to readmission, increasing maternal age was associated with a higher likelihood of being readmitted within 10 days from delivery discharge (Figure 1). 45% of women age 15 to 24 were readmitted within 10 days of discharge compared to 50% of women age 25 to 29, 54% of women age 30 to 34, 58% of women age 35 to 39, 60% of women age 40 to 44, and 67% of women age 45 or older (p<0.01).
Figure 1.
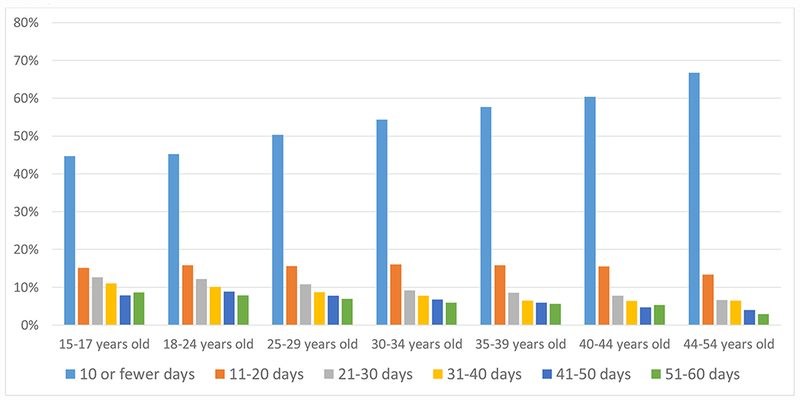
Time to readmission stratified by maternal age
The proportion of patients with each duration of time from delivery hospitalization discharge to readmission is demonstrated stratified by maternal age.
In comparing the unadjusted to adjusted models for readmission, women 45 and older (RR 1.66, 95% 1.55, 1.79), 40 to 44 (RR 1.37, 95% CI 1.34, 1.39), and 15 to 17 (RR 1.22, 95% CI 1.20, 1.25) years of age were at increased risk for readmission within 60 days of delivery discharge compared to women 25 to 29 years age in the unadjusted model (Table 2). In the adjusted model including hospital factors, demographics, and medical and obstetric risk factors, this risk was attenuated; while women 45 and older (aRR 1.28, 95% CI 1.19, 1.38), 40 to 44 (aRR 1.26, 95% CI 1.24, 1.28), and 15 to 17 (aRR 1.11, 95% 1.08, 1.13) remained at increased risk compared to women 25 to 29, the magnitude of the increase risk was lesser for each of these age categories. Other significant factors associated with readmission risk in the adjusted model included lower ZIP code income quartiles compared to the highest, Medicare and Medicaid compared to commercial insurance, and obstetric and medical risk factors including chronic hypertension, hypertensive diseases of pregnancy, chronic kidney disease, asthma, lupus, multiple gestation, postpartum hemorrhage, cesarean delivery, and pregestational diabetes.
Table 2.
Risk for readmission within 60 days of delivery hospitalization discharge
| Unadjusted model | Adjusted model | |||
|---|---|---|---|---|
| RR | 95% CI | aRR | 95% CI | |
| 15-17 years old | 1.22 | 1.20, 1.25 | 1.11 | 1.08, 1.13 |
| 18-24 years old | 1.17 | 1.16, 1.19 | 1.08 | 1.07, 1.09 |
| 25-29 years old | Reference | Reference | ||
| 30-34 years old | 0.96 | 0.95, 0.97 | 1.00 | 0.99, 1.01 |
| 35-39 years old | 1.09 | 1.07, 1.10 | 1.09 | 1.07, 1.10 |
| 40-44 years old | 1.37 | 1.34, 1.39 | 1.26 | 1.24, 1.28 |
| 45-54 years old | 1.66 | 1.55, 1.79 | 1.28 | 1.19, 1.38 |
| Payer | ||||
| Medicare | 3.49 | 3.39, 3.59 | 2.71 | 2.63, 2.79 |
| Medicaid | 1.54 | 1.53, 1.55 | 1.47 | 1.46, 1.49 |
| Private insurance | Reference | Reference | ||
| Self-pay | 1.03 | 1.00, 1.07 | 1.06 | 1.02, 1.09 |
| No charge | 1.15 | 0.98, 1.34 | 1.11 | 0.95, 1.30 |
| Other | 1.11 | 1.09, 1.14 | 1.14 | 1.11, 1.17 |
| Median ZIP code income quartile | ||||
| Lowest income quartile | 1.51 | 1.50, 1.53 | 1.23 | 1.22, 1.25 |
| 2nd lowest quartile | 1.31 | 1.29, 1.32 | 1.17 | 1.15, 1.18 |
| 2nd highest quartile | 1.19 | 1.18, 1.20 | 1.11 | 1.10, 1.13 |
| Highest income quartile | Reference | Reference | ||
| Delivery postpartum hemorrhage | 2.86 | 2.82, 2.90 | 2.75 | 2.71, 2.79 |
| Cesarean delivery | 1.89 | 1.88, 1.91 | 1.76 | 1.75, 1.78 |
| Pregestational diabetes | 2.74 | 2.68, 2.81 | 1.55 | 1.51, 1.58 |
| Gestational diabetes | 0.96 | 0.95, 0.98 | 0.81 | 0.80, 0.83 |
| Systemic lupus | 2.86 | 2.82, 2.90 | 2.37 | 2.24, 2.51 |
| Multiple gestation | 1.79 | 1.76, 1.83 | 1.23 | 1.21, 1.26 |
| Asthma | 1.72 | 1.69, 1.75 | 1.45 | 1.43, 1.47 |
| Chronic renal disease | 3.83 | 3.69, 3.98 | 2.32 | 2.23, 2.41 |
| Hypertensive diseases of pregnacy | 2.77 | 2.74, 2.80 | 2.25 | 2.23, 2.27 |
| Chronic hypertension | 2.72 | 2.67, 2.77 | 2.10 | 2.05, 2.14 |
| Hospital bed size | ||||
| Small | Reference | Reference | ||
| Medium | 1.09 | 1.07, 1.10 | 1.04 | 1.03, 1.06 |
| Large | 1.18 | 1.16, 1.20 | 1.13 | 1.11, 1.14 |
| Hospital teaching status | ||||
| Metropolitan non-teaching | Reference | Reference | ||
| Metropolitan teaching | 1.12 | 1.11, 1.13 | 1.04 | 1.04, 1.05 |
| Non-metropolitan | 1.01 | 1.00, 1.03 | 0.92 | 0.90, 0.93 |
RR, risk ratio. aRR, adjusted risk ratio. CI, confidence interval. Estimates for medical and obstetric conditions are with absence of the condition as the reference
In comparing the unadjusted to adjusted models for SMM during delivery hospitalizations, women 45 and older (RR 3.03, 95% CI 2.87, 31.9), 40 to 44 (RR 1.71, 95% 1.69, 1.74), 35 to 39 (RR 1.29, 95% 1.28, 1.31), and 15 to 17 (RR 1.36, 95% CI 1.33, 1.39) were more likely to experience SMM than women 25 to 29 in unadjusted analysis (Table 3). In adjusted analysis women age 25 to 29 remained the lowest risk group, with risk among women 45 and older (aRR 1.85, 95% CI 1.75, 1.95), 40 to 44 (aRR 1.45, 95% 1.42, 1.47), 35 to 39 (aRR 1.22, 95% CI 1.20, 1.23), and 15 to 17 (aRR 1.35, 95% CI 1.32, 1.38) all at significantly higher risk. Similar to the model for readmission risk, significant factors associated with SMM during the delivery hospitalization in the adjusted model included the lowest ZIP code income quartile compared to the highest, Medicare and Medicaid compared to commercial insurance, and obstetric and medical risk factors including chronic hypertension, hypertensive diseases of pregnancy, chronic kidney disease, asthma, lupus, multiple gestation, postpartum hemorrhage, cesarean delivery, and pregestational diabetes.
Table 3.
Risk for severe maternal morbidity during delivery hospitalizations
| Unadjusted model | Adjusted model | |||
|---|---|---|---|---|
| RR | 95% CI | aRR | 95% CI | |
| 15-17 years old | 1.36 | 1.33, 1.39 | 1.35 | 1.32, 1.38 |
| 18-24 years old | 1.13 | 1.12, 1.14 | 1.07 | 1.06, 1.09 |
| 25-29 years old | Reference | Reference | ||
| 30-34 years old | 1.06 | 1.05, 1.07 | 1.07 | 1.06, 1.08 |
| 35-39 years old | 1.29 | 1.28, 1.31 | 1.22 | 1.20, 1.23 |
| 40-44 years old | 1.71 | 1.69, 1.74 | 1.45 | 1.42, 1.47 |
| 45-54 years old | 3.03 | 2.87, 3.19 | 1.85 | 1.75, 1.95 |
| Payer | ||||
| Medicare | 2.63 | 2.54, 2.71 | 2.01 | 1.95, 2.08 |
| Medicaid | 1.40 | 1.39, 1.41 | 1.40 | 1.39, 1.41 |
| Private insurance | Reference | Reference | ||
| Self-pay | 1.49 | 1.45, 1.53 | 1.61 | 1.56, 1.65 |
| No charge | 1.27 | 1.11, 1.46 | 1.28 | 1.11, 1.48 |
| Other | 1.06 | 1.03, 1.08 | 1.13 | 1.11, 1.16 |
| Median ZIP code income quartile | ||||
| Lowest income quartile | 1.48 | 1.47, 1.50 | 1.27 | 1.26, 1.29 |
| 2nd lowest quartile | 1.16 | 1.15, 1.17 | 1.09 | 1.08, 1.10 |
| 2nd highest quartile | 1.07 | 1.06, 1.08 | 1.04 | 1.03, 1.06 |
| Highest income quartile | Reference | Reference | ||
| Cesarean delivery | 3.31 | 3.29, 3.34 | 2.89 | 2.86, 2.91 |
| Pregestational diabetes | 2.25 | 2.19, 2.30 | 1.06 | 1.03, 1.08 |
| Gestational diabetes | 1.21 | 1.20, 1.23 | 0.93 | 0.92, 0.94 |
| Systemic lupus | 3.78 | 3.59, 3.99 | 1.97 | 1.87, 2.08 |
| Multiple gestation | 3.64 | 3.59, 3.69 | 2.08 | 2.05, 2.11 |
| Asthma | 1.53 | 1.51, 1.56 | 1.27 | 1.25, 1.29 |
| Chronic renal disease | 6.06 | 5.89, 6.23 | 3.93 | 3.81, 4.04 |
| Chronic hypertension | 3.62 | 3.59, 3.65 | 2.76 | 2.74, 2.79 |
| Hypertensive diseases of pregnancy | 2.14 | 2.10, 2.19 | 1.51 | 1.48, 1.55 |
| Hospital bed size | ||||
| Small | Reference | Reference | ||
| Medium | 1.13 | 1.12, 1.15 | 1.06 | 1.05, 1.08 |
| Large | 1.14 | 1.12, 1.15 | 1.04 | 1.03, 1.06 |
| Hospital teaching status | ||||
| Metropolitan non-teaching | Reference | Reference | ||
| Metropolitan teaching | 1.38 | 1.37, 1.39 | 1.28 | 1.27, 1.29 |
| Non-metropolitan | 1.20 | 1.18, 1.21 | 1.11 | 1.10, 1.13 |
RR, risk ratio. aRR, adjusted risk ratio. CI, confidence interval. Estimates for medical and obstetric conditions are with absence of the condition as the reference.
Evaluating SMM during readmissions excluding women with a SMM diagnosis during the delivery hospitalization, in the unadjusted model women 45 and older were at highest risk for SMM (RR 1.56 95% CI 1.25, 1.94), followed by women 40 to 44 (RR 1.26, 95% CI 1.18, 1.34), and women 35 to 39 (RR 1.15, 95% CI 1.10-1.21) (Table 4). Women age 15 to 17 were at lower risk for SMM during postpartum readmissions (RR 0.79, 95% CI 0.72, 0.86). In the adjusted analysis, these factors retained significance. Women age 45 to 54 were at increased risk (aRR 1.31, 95% CI 1.05, 1.64), as were women 40 to 44 (aRR 1.26, 95% 1.19, 1.35), and 35 to 39 (aRR 1.20, 95% CI 1.14, 1.26) compared to women 25 to 29. Women age 15 to 17 remained at lower risk (aRR 0.79, 95% CI 0.72, 0.87). Risk factors at delivery associated with increased for SMM during readmission included postpartum hemorrhage, chronic renal disease, multiple gestation, and pregestational diabetes.
Table 4.
Risk for severe maternal morbidity during postpartum readmissions
| Unadjusted model | Adjusted model | |||
|---|---|---|---|---|
| RR | 95% CI | aRR | 95% CI | |
| 15-17 years old | 0.79 | 0.72, 0.86 | 0.79 | 0.72, 0.87 |
| 18-24 years old | 0.93 | 0.89, 0.96 | 0.92 | 0.88, 0.95 |
| 25-29 years old | Reference | Reference | ||
| 30-34 years old | 1.10 | 1.06, 1.14 | 1.10 | 1.06, 1.15 |
| 35-39 years old | 1.15 | 1.10, 1.21 | 1.20 | 1.14, 1.26 |
| 40-44 years old | 1.26 | 1.18, 1.34 | 1.26 | 1.19, 1.35 |
| 45-54 years old | 1.56 | 1.25, 1.94 | 1.31 | 1.05, 1.64 |
| Payer | ||||
| Medicare | 0.95 | 0.85, 1.07 | 0.92 | 0.82, 1.03 |
| Medicaid | 1.03 | 1.00, 1.06 | 1.10 | 1.06, 1.13 |
| Private insurance | Reference | Reference | ||
| Self-pay | 1.20 | 1.07, 1.34 | 1.18 | 1.05, 1.32 |
| No charge | 1.51 | 0.94, 2.42 | 1.81 | 1.13, 2.90 |
| Other | 0.95 | 0.87, 1.04 | 0.98 | 0.90, 1.07 |
| Median ZIP code income quartile | ||||
| Lowest income quartile | 1.10 | 1.06, 1.15 | 1.20 | 1.15, 1.25 |
| 2nd lowest quartile | 1.03 | 0.99, 1.08 | 1.12 | 1.07, 1.17 |
| 2nd highest quartile | 1.01 | 0.96, 1.05 | 1.07 | 1.02, 1.11 |
| Highest income quartile | Reference | Reference | ||
| Postpartum hemorrhage | 3.89 | 3.76, 4.02 | 4.00 | 3.86, 4.13 |
| Cesarean delivery | 1.20 | 1.17, 1.24 | 1.31 | 1.28, 1.35 |
| Pregestational diabetes | 1.28 | 1.18, 1.38 | 1.21 | 1.12, 1.32 |
| Gestational diabetes | 1.04 | 0.98, 1.10 | 0.99 | 0.93, 1.05 |
| Systemic lupus | 1.47 | 1.23, 1.76 | 1.40 | 1.16, 1.68 |
| Multiple gestation | 1.51 | 1.41, 1.61 | 1.23 | 1.16, 1.32 |
| Asthma | 1.09 | 1.03, 1.15 | 1.12 | 1.06, 1.18 |
| Chronic renal disease | 2.11 | 1.89, 2.36 | 2.18 | 1.95, 2.44 |
| Hypertensive diseases of pregnancy | 0.65 | 0.62, 0.68 | 0.67 | 0.65, 0.70 |
| Chronic hypertension | 1.15 | 1.08, 1.23 | 1.04 | 0.97, 1.12 |
| Hospital bed size | ||||
| Small | Reference | Reference | ||
| Medium | 0.99 | 0.94, 1.05 | 0.98 | 0.93, 1.03 |
| Large | 0.94 | 0.90, 0.98 | 0.91 | 0.87, 0.96 |
| Hospital teaching status | ||||
| Metropolitan non-teaching | Reference | Reference | ||
| Metropolitan teaching | 0.98 | 0.95, 1.01 | 0.94 | 0.91, 0.97 |
| Non-metropolitan | 1.08 | 1.03, 1.13 | 1.07 | 1.01, 1.12 |
RR, risk ratio. aRR, adjusted risk ratio. CI, confidence interval. Estimates for medical and obstetric conditions are with absence of the condition as the reference.
DISCUSSION
In this analysis of postpartum readmission and associated morbidity, women 35 and older were at increased risk for both all-cause readmission and SMM during readmission compared to women in their late twenties. Furthermore, risk for readmission increased with maternal age such that women 45 to 54 were at the highest risk followed by women 40 to 44 and women 35 to 39. This increased risk was retained in adjusted models despite older patients being more likely to have higher median incomes and higher rates of private insurance, factors otherwise associated with lower readmission and SMM risk; this retained risk supports that even controlling for these socioeconomic factors maternal risk remains elevated. These findings align with outcomes research that demonstrates higher risk for maternal morbidity associated with advanced maternal age during the antepartum period and at delivery, as well as increased risk for adverse neonatal outcomes.6–8,14 For both postpartum readmission and risk for severe morbidity during a delivery hospitalization, maternal age-based risk was bimodal with risk higher for women aged 15 to 17 than for women 25 to 29 in addition to risk being higher for older mothers. Risk for younger women was retained in the adjusted models including hospital, demographic, and medial obstetric risk factors. The cause of overall increased risk among the youngest group is unclear; risk may be in part due to social factors and physiology that cannot be accounted for within our study models.
Recent clinical recommendations have increasingly focused on improving care during the postpartum period, the “fourth trimester.” The American College of Obstetricians and Gynecologists (ACOG) has recently updated recommendations regarding postpartum care stating, “To optimize the health of women and infants, postpartum care should become an ongoing process, rather than a single encounter, with services and support tailored to each woman’s individual needs.”21 Traditional approaches to postpartum care with a six-week follow up appointment are being reconsidered in hopes of reducing adverse postpartum maternal outcomes and risk for readmission;22 while a standard six week visit may be appropriate for low risk women to plan health maintenance and follow up, more intensive care may be indicated for at-risk women. An important consideration in optimizing postpartum care is appropriately characterizing maternal risk. Advanced maternal age represents a common, readily recognizable risk factor that, particularly with age 40 or greater and in the presence of other risk factors, may justify closer postpartum surveillance. Future trials are indicated to determine what approaches may be most effective in reducing maternal risk.
There are several important limitations in interpreting the findings of this analysis. While the NRD is a large data set capable of providing national estimates of readmissions it includes limited information on hospital resources and staffing which may be important factors in risk for readmissions and other adverse outcomes. An additional limitation of this analysis is that we are unable to assess outpatient management including prenatal and postnatal care, use of assisted reproductive technology, and consultant and interdisciplinary care for complicated patients in the hospital. We also cannot assess compliance with or efficacy of recommended therapies, such as blood pressure surveillance, antihypertensive medications, or anticoagulation, in the outpatient setting prior to readmission. A further limitation common to administrative data sets is that for secondary diagnoses both under-ascertainment and misclassification may be a concern, particularly if these diagnoses are not tied to billing. That gestational diabetes was “protective” may indicate that it served as a proxy for lower maternal risk not controlled for by other variables in our model. Another related limitation is that diagnosis codes generally do not specify condition severity. Finally, the NRD does not include data on patient race and ethnicity, a factor associated with adverse maternal outcomes.23 Strengths of the NRD include its size, the ability to create nationally representative estimates, and capture of readmissions throughout the year occurring within individual states.
In summary, older women are at higher risk for both postpartum readmission and severe morbidity during readmission. Women older than 35 years are most likely to experience complications requiring readmission with the risk highest at age 40 or older. For women with multiple risk factors including older age, shorter-term or more intensive postpartum follow-up should be investigated to determine if risk for readmissions and associated morbidity can be reduced.
Acknowledgments
Dr. Friedman is supported by a career development award (K08HD082287) from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health
Dr. Attenello is supported by NIH SC CTSI KL2 Clinical and Translational Research Scholar Award.
Footnotes
Conflict of Interest The authors report no conflict of interest
REFERENCES
- 1.Martin JA, Hamilton BE, Osterman MJK. Births in the United States, 2016. NCHS Data Brief. 2017(287):1–8. [PubMed] [Google Scholar]
- 2.Hamilton BE, Martin JA, Osterman MJK, et al. Births: Provisional data for 2016. Vital statistics rapid release; no 2. Hyattsville, MD: National Center for Health Statistics. June 2017. Available from: https://www.cdc/.gov/nchs/data/vsrr/report002.pdf. [Google Scholar]
- 3.Hodes-Wertz B, Druckenmiller S, Smith M, Noyes N. What do reproductive-age women who undergo oocyte cryopreservation think about the process as a means to preserve fertility? Fertil Steril. 2013;100(5):1343–1349. [DOI] [PubMed] [Google Scholar]
- 4.Hogan MC, Foreman KJ, Naghavi M, et al. Maternal mortality for 181 countries, 1980–2008: a systematic analysis of progress towards Millennium Development Goal 5. The Lancet. 2010;375(9726):1609–1623. [DOI] [PubMed] [Google Scholar]
- 5.Creanga AA, Syverson C, Seed K, Callaghan WM. Pregnancy-Related Mortality in the United States, 2011–2013. Obstet Gynecol. 2017;130(2):366–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Delbaere I, Verstraelen H, Goetgeluk S, Martens G, De Backer G, Temmerman M. Pregnancy outcome in primiparae of advanced maternal age. European Journal of Obstetrics Gynecology Reproductive Biology. 2007;135(1):41–46. [DOI] [PubMed] [Google Scholar]
- 7.Ogawa K, Urayama KY, Tanigaki S, et al. Association between very advanced maternal age and adverse pregnancy outcomes: a cross sectional Japanese study. BMC pregnancy childbirth. 2017;17(1):349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Timofeev J, Reddy UM, Huang C-C, Driggers RW, Landy HJ, Laughon SK. Obstetric complications, neonatal morbidity, and indications for cesarean delivery by maternal age. Obstetrics and gynecology. 2013;122(6):1184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lisonkova S, Potts J, Muraca GM, et al. Maternal age and severe maternal morbidity: A population-based retrospective cohort study. PLoS medicine. 2017;14(5):e1002307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jacobsson B, Ladfors L, Milsom I. Advanced maternal age and adverse perinatal outcome. Obstetrics and Gynecology. 2004;104(4):727–733. [DOI] [PubMed] [Google Scholar]
- 11.Booker Wa, Gyamfi-Bannerman C, Sheen J-J, et al. Maternal outcomes by race for women aged 40 years or older. Obstetrics and Gynecology. 2018;132(2):404–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fitzpatrick KE, Tuffnell D, Kurinczuk JJ, Knight M. Pregnancy at very advanced maternal age: a UK population-based cohort study. BJOG. 2017;124(7):1097–1106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhu C, Wang M, Niu G, Yang J, Wang Z. Obstetric outcomes of twin pregnancies at advanced maternal age: A retrospective study. Taiwan J Obstet Gynecol. 2018;57(1):64–67. [DOI] [PubMed] [Google Scholar]
- 14.Sheen J-J, Wright JD, Goffman D, et al. Maternal age and risk for adverse outcomes. American Journal of Obstetrics and Gynecology. 2018;219(4):390.e391–390.e315. [DOI] [PubMed] [Google Scholar]
- 15.Kassebaum NJ, Barber RM, Bhutta ZA, et al. Global, regional, and national levels of maternal mortality, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. The Lancet. 2016;388(10053):1775–1812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pinheiro RL, Areia AL, Mota Pinto A, Donato H. Advanced Maternal Age: Adverse Outcomes of Pregnancy, A Meta-Analysis. Acta Med Port. 2019;32(3):219–226. [DOI] [PubMed] [Google Scholar]
- 17.Callaghan WM, Creanga AA, Kuklina EV. Severe maternal morbidity among delivery and postpartum hospitalizations in the United States. Obstetrics and Gynecology. 2012;120(5):1029–1036. [DOI] [PubMed] [Google Scholar]
- 18.Henderson V, Stumbras K, Caskey R, Haider S, Rankin K, Handler A. Understanding factors associated with postpartum visit attendance and contraception choices: listening to low-income postpartum women and health care providers. Maternal child health journal. 2016;20(1):132–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kuklina E, Whiteman M, Hillis S, Jameieson D, Meikle S, Posner S. An enhanced method for identifying obstetric deliveries: implications for estimating maternal morbidity. Matern Child Health J. 2008;12:469–477. [DOI] [PubMed] [Google Scholar]
- 20.CDC. Severe Maternal Morbidity Indicators and Corresponding ICD Codes during Delivery Hospitalizations. 2018; https://www.cdc.gov/reproductivehealth/maternalinfanthealth/smm/severe-morbidity-ICD.htm.
- 21.ACOG Committee Opinion No. 736: Optimizing Postpartum Care. Obstetrics and gynecology. 2018;131(5):e140–e150. [DOI] [PubMed] [Google Scholar]
- 22.Murray Horwitz ME, Molina RL, Snowden JM. Postpartum Care in the United States - New Policies for a New Paradigm. N Engl J Med. 2018;379(18):1691–1693. [DOI] [PubMed] [Google Scholar]
- 23.Anachebe NF, Sutton MY. Racial disparities in reproductive health outcomes. American Journal of Obstetrics and Gynecology. 2003;188(4):S37–S42. [DOI] [PubMed] [Google Scholar]


