Abstract
Allogeneic blood or marrow transplantation (BMT) is a potentially curative therapy for patients with primary immunodeficiency (PID). Safe and effective reduced-intensity conditioning (RIC) approaches that are associated with low toxicity, utilize alternative donors, and afford good immune reconstitution are needed to advance the field. Twenty PID patients, ranging in age from 4 to 58 years, were treated on a prospective clinical trial of a novel, radiation-free and serotherapy-free RIC, T-cell-replete BMT approach using pentostatin, low-dose cyclophosphamide, and busulfan for conditioning with post-transplantation cyclophosphamide-based graft-versus-host-disease (GVHD) prophylaxis. This was a high-risk cohort with median hematopoietic cell transplantation-comorbidity index of 3. With median follow-up of survivors of 1.9 years, 1-year overall survival was 90% and grade III-IV acute GVHD-free, graft failure-free survival was 80% at day +180. Graft failure incidence was 10%. Split chimerism was frequently observed at early post-BMT timepoints, with a lower percentage of donor T cells which gradually increased by day +60. The cumulative incidences of grade II-IV and grade III-IV acute GVHD (aGVHD) were 15% and 5%, respectively. All aGVHD was steroid-responsive. No patients developed chronic GVHD. Few significant organ toxicities were observed. Evidence of phenotype reversal was observed for all engrafted patients, even those with significantly mixed chimerism (n=2) or with unknown underlying genetic defect (n=3). All six patients with pre-BMT malignancies or lymphoproliferative disorders remain in remission. Most patients have discontinued immunoglobulin replacement. All survivors are off immunosuppression for GVHD prophylaxis or treatment. This novel RIC BMT approach for patients with PID has yielded promising results, even for high-risk patients.
Keywords: Primary immunodeficiency, bone marrow transplantation, reduced intensity conditioning, post-transplantation cyclophosphamide
INTRODUCTION
Allogeneic blood or marrow transplantation (BMT) has long served as a potentially curative therapy for patients with primary immune deficiencies (PID). However, the landscape of PIDs has expanded markedly since the first PID transplants were performed, with >350 PIDs genetically and phenotypically now recognized and many characterized by immune dysregulation rather than solely immune deficiency.1 Increasingly, patients with PIDs of variable natural history, hypomorphic variants or somatic reversion are diagnosed later in life and only considered for BMT after incurring significant co-morbidities or refractory disease sequelae.2–4 Family members may also be affected, limiting donor options.5 Furthermore, in patients without PID-associated malignancy, the benefits of conditioning extend only so far as ensuring engraftment, and graft-versus-host disease (GVHD) is not beneficial. Thus, BMTs for PIDs entail unique challenges regarding the best approaches to achieve engraftment and phenotype reversal with as little short- and long-term toxicity as possible.
We sought to evaluate a novel, reduced-intensity conditioning (RIC) approach to BMT for PIDs, a platform designed with the goals of reducing regimen-related toxicities and complications such as GVHD, utilizing alternative donors, and achieving successful engraftment and robust immune reconstitution. An approach to lymphodepletion-centered RIC developed at the National Institutes of Health (NIH)6,7 was integrated with post-transplantation cyclophosphamide (PTCy) for GVHD prophylaxis, given the low rates of severe acute and chronic GVHD and the comparable outcomes between alternative donors and human leukocyte antigen (HLA)-matched-sibling (MSD) donors observed with PTCy-based platforms.8–13 Pentostatin with low-dose cyclophosphamide was used as the T-cell suppressing backbone of conditioning, based on data demonstrating pentostatin plus cyclophosphamide to result in greater T cell functional impairment compared to fludarabine plus cyclophosphamide, with similar levels of host T cell lymphodepletion.7 Herein, we present the results of a prospective trial of a novel, radiation- and serotherapy-free RIC, PTCy-based, T-cell-replete bone marrow transplantation (BMT) platform for children and adults with PIDs.
METHODS
After institutional review board approval, this single-center prospective clinical trial (, clinicaltrials.gov) was conducted at the NIH Clinical Center. The results of 20 consecutive BMTs performed on the fully-accrued RIC arm, which enrolled patients from November 19, 2015 to October 18, 2017, are presented. Eligible patients were aged 4–75 years with PID of sufficient severity to warrant BMT. The conditioning regimen was an 11-day, reduced-intensity approach consisting of pentostatin, low-dose cyclophosphamide, and 2 days of pharmacokinetically-dosed busulfan with AUC target of 4600 micromol*min/day. GVHD prophylaxis consisted of high-dose, posttransplantation cyclophosphamide (PTCy) on days +3 and +4, followed by sirolimus and mycophenolate mofetil. All grafts were T-cell-replete bone marrow. The BMT platform, including specific drug doses and time, as well as supportive care measures, are outlined in Table 1.
Table 1.
BMT platform and supportive care measures.
| Day | Drug/Intervention | Adult Dosing | Pediatric Dosing |
| Prior to day −11 | Busulfan test dose | 0.8 mg/kg IV to calculate AUC& | 0.8 mg/kg IV to calculate AUC* |
| Day −11 and day −7 | Pentostatin | 4 mg/m2/day IV | |
| Days −11 through −8 | Cyclophosphamide | 3 mg/kg/day orally or IV, dosage cap of 200 mg/day | |
| Days −7 through −4 | Cyclophosphamide | If ALC on day −7 > 100 cells/μL, escalation to 5 mg/kg/day orally$; dosage cap of 400 mg/day | |
| Days −3 and −2 | Busulfan | Pharmacokinetically-dosed, with targeted daily systemic exposure of 4600 uMol-min based on test dose AUC; default dose of 3.2 mg/kg/day if test dose cannot be performed | |
| Day −1 | Day of rest | ||
| Day 0 | Fresh infusion of T-cell replete marrow | Target dose 4.5 × 108 TNC/kg recipient IBW | |
| Days +3 and +4 | Cyclophosphamide@ | 50 mg/kg/day IV% | |
| Mesna | 50 mg/kg/day IV% | ||
| Day +5 | Sirolimus loading dose$ | 6 mg orally | 3 mg/m2 orally#; maximum initial dose 6 mg |
| Days +5 through +35 | MMF | 15 mg/kg orally or IV three times daily; maximum 1000 mg/dose | |
| Starting day +6, continued through day+180 then stopped without taper^ | Sirolimus maintenance dose$ | 2 mg orally goal trough of 5–12 ng/mL | 1 mg/m2 orally#; maximum initial dose 2 mg; goal trough of 5–12 ng/mL |
| Day | Supportive Care Measure | Adult Dosing | Pediatric Dosing |
| Prior to day −11 | Leuprolide for ovarian suppression | Menstruating females | |
| Prior to day −11 | Ivermectin, if from area with endemic Strongyloides | 200 mcg/kg orally daily for 2 consecutive days | |
| −11 through −1 | PJP prophylaxis: trimethoprim-sulfamethoxazole or alternative | ||
| −4 through −1 | Clonazepam for seizure prophylaxis | 0.5 mg orally twice daily | < 10 years old or < 30 kg: 0.005–0.015 mg/kg/dose twice daily, rounded to tablet sizes |
| −4 through −1 | Levetiracetam for seizure prophylaxis | 500 mg orally twice daily | 10 mg/kg orally or IV twice daily, maximum dose 500 mg |
| −11 through +100 | Ursodiol for hepatic protection | < 90 kg: 300 mg orally twice daily ≥ 90 kg: 300 mg each morning and 600 mg each evening, orally |
< 40 kg: 300 mg orally twice daily |
| −11 through +100 or longer | Antifungal prophylaxis | Agent chosen as indicated and tolerated by organ function and drug interactions; end of therapy often chosen to coincide with cessation of sirolimus given drug interactions | |
| −11 through +100 | Weekly whole blood monitoring by quantitative PCR for CMV, EBV, adenovirus, and HHV6; pre-emptive treatment strategy used for CMV (letermovir not approved yet during study period for prophylaxis) | ||
| −11 through +2 years | HSV/VZV prophylaxis: acyclovir | 800 mg orally twice daily | 20 mg/kg orally twice daily, maximum dose 800 mg |
| Upon count recovery through +1 year | PJP prophylaxis: trimethoprim-sulfamethoxazole or alternative | ||
| 0 until PJP prophylaxis resumed | Twice weekly whole blood qualitative PCR for Toxoplasmosis in seropositive individuals | ||
| 0 through ANC recovery | Antibacterial prophylaxis: levofloxacin, or alternative as appropriate | ||
| 0 through +5 | Avoidance of corticosteroids; hydrocortisone permitted for adrenal insufficiency | ||
| +2 through +5 | Normal saline for uroprotection | 90 mL/m2/hr IV | |
| +5 until ANC ≥ 1000/μL for 3 days | Filgrastim | 5 mcg/kg/day SQ or IV | |
| Post-engraftment, as indicated | Immunoglobulin replacement | ||
| +180 onward | Post-BMT immunizations | ||
Abbreviations: IV, intravenous; AUC, area under the curve; ALC, absolute lymphocyte count; IBW, ideal body weight; MMF, mycophenolate mofetil; PJP, Pneumocystis jiroveci pneumonia; PCR, polymerase chain reaction; CMV, cytomegalovirus; EBV, Epstein-Barr virus; HHV6, human herpesvirus 6; HSV, herpes simplex virus; VZV, varicella zoster virus; ANC, absolute neutrophil count; BMT, bone marrow transplantation
Post-transplantation cyclophosphamide infusion on day +3 began 60–72 hours after graft infused (72 hours preferred)
For recipients older than age 16 years, busulfan test dose was based on ideal body weight (IBW) or actual body weight (ABW), whichever is lower, unless recipient was > 120% of IBW, in which case adjusted ideal body weight (IBW+ 25% of difference between IBW and ABW) was used.
For children age 4–16 years, busulfan test dose was based on ABW. Only one patient, P14, could not undergo busulfan pharmacokinetics.
All patients received this dose increase.
Dosed according to IBW, unless recipient weighed less than IBW, in which case ABW was used
Based on ABW
Sirolimus could be stopped sooner for toxicities or mixed chimerism, either with or without an alternative agent depending on the clinical situation
Sirolimus loading and maintenance doses individualized as necessary based on each patient’s concomitant medications and potential drug interactions, particularly the use of azoles, where co-administration was not considered contraindicated, but required significant sirolimus dose reductions.
The primary endpoint was to estimate the grade III-IV acute GVHD-free, graft-failure-free survival (GGFS) at day +180 post-BMT; events were grade III-IV acute GVHD (aGVHD) not responsive to seven days of high-dose steroids, primary or secondary graft failure, or death from any cause.
Acute and chronic GVHD were diagnosed and graded using standard criteria.14,15 T-, B-, and NK-cell subsets were assessed by peripheral blood flow cytometry weekly through day +100 and at study timepoints. Epstein-Barr virus (EBV), cytomegalovirus (CMV), human herpesvirus-6, adenovirus, and BK virus were evaluated weekly in blood and, for BK virus, also urine, by quantitative PCR. CMV monitoring and preemptive treatment were performed as previously published.16
Details regarding study design and definitions, recipient eligibility, donor selection, and monitoring evaluations are listed in Supplemental Methods.
Statistical Analysis
Data were locked for analysis on January 23, 2019. Survival endpoint probabilities were estimated using the Kaplan-Meier method with 95% confidence intervals (CI). Cumulative incidences (CuI) of transplant-related mortality (TRM), GVHD, count recovery, and graft failure were estimated by competing-risk analysis using Gray’s method. Death was a competing risk for all analyses except TRM; relapse of pre-BMT malignancy was a competing risk for TRM. Graft failure was a competing risk for GVHD.
Data were analyzed with R, version 3.3.3 (https://www.R-project.org, R-Foundation for Statistical Computing) and Prism, version 8.0 (GraphPad Software)
RESULTS
Patient and Graft Characteristics
Table 2 shows recipient and graft characteristics. This was a high-risk cohort of children and adults, median Hematopoietic Cell Transplantation-Comorbidity Index (HCT-CI)17 score of 3 (range 0–11), with median follow-up of survivors of 1.9 years (range 1.3–3.1 years). Thirty-five percent of patients received haploidentical donor grafts, 40% matched unrelated, and the rest MSD.
Table 2.
Recipient, donor, and graft characteristics
| Patients (n=20) | |
|---|---|
| Male, n (%) | 13 (65%) |
| Age at BMT, years, median (range) | 18 (4–58) |
| Aged > 18 years, n (%) | 10 (50%) |
| Diagnosis, n | |
| MAGT1 deficiency (XMEN) | 3 |
| PIK3CD gain of function (PASLI) | 3 |
| STAT3 deficiency (Hyper-IgE Syndrome) | 3 |
| Unknown PID | 3 |
| IFNGR1 deficiency, autosomal dominant | 1 |
| IFNGR1 deficiency, autosomal recessive | 1 |
| RAG1 deficiency, hypomorphic | 1 |
| RAG2 deficiency, hypomorphic | 1 |
| Wiskott-Aldrich syndrome, somatic revertant | 1 |
| IL2RG deficiency (X-SCID), somatic revertant | 1 |
| IL10R1 deficiency | 1 |
| NFKB1 haploinsufficiency | 1 |
| Active disease manifestations leading into BMT | |
| Active infection at BMT | 8 (40%) |
| Lymphoma/lymphoproliferative disorder | 6 (30%) |
| Autoimmunity | 8 (40%) |
| Chronic immunosuppression requirement | 7 (35%) |
| HCT-CI, median (range) | 3 (0–11) |
| Donor age, years, median (range) | 27 (15–56) |
| Female donor for male recipient, n (%) | 2 (10%) |
| Donor source, n (%) | |
| HLA-matched-unrelated | 8 (40%) |
| HLA-haploidentical | 7 (35%) |
| HLA-matched-sibling | 5 (25%) |
| ABO, n (%) | |
| Matched | 12 (60%) |
| Minor mismatch | 4 (20%) |
| Major mismatch | 2 (10%) |
| Major and minor mismatch | 2 (10%) |
| Graft dose, cells/kg, median (range) | |
| TNC, × 108 | 4.54 (2.42–9.30) |
| CD3+, × 107 | 5.06 (1.84–10.00) |
| CD34+, × 106 | 5.31 (2.52–14.20) |
| CMV serostatus D/R, n (%) | |
| −/Unknowna | 7 (35%) |
| +/Unknowna | 5 (25%) |
| −/− | 4 (20%) |
| +/+ | 3 (15%) |
| +/− | 1 (5%) |
| EBV serostatus D/R, n (%) | |
| +/+ | 13 (65%) |
| +/Unknowna | 5 (25%) |
| +/− | 2 (10%) |
Abbreviations: BMT, bone marrow transplantation; XMEN, X-linked immunodeficiency with magnesium defect, EBV infection, and neoplasia; PASLI, p110delta-activating mutation causing senescent T cells, lymphadenopathy, and immunodeficiency; HCT-CI, Hematopoietic Cell Transplantation-Comorbidity Index; TNC, total nucleated cell; CMV, human cytomegalovirus; D/R, donor/recipient; EBV, Epstein-Barr virus.
Serostatus for CMV and EBV was unknown for recipients on chronic immunoglobulin replacement therapy who did not have a documented history of the virus detected in blood or tissue to indicate a positive serostatus.
Survival Endpoints
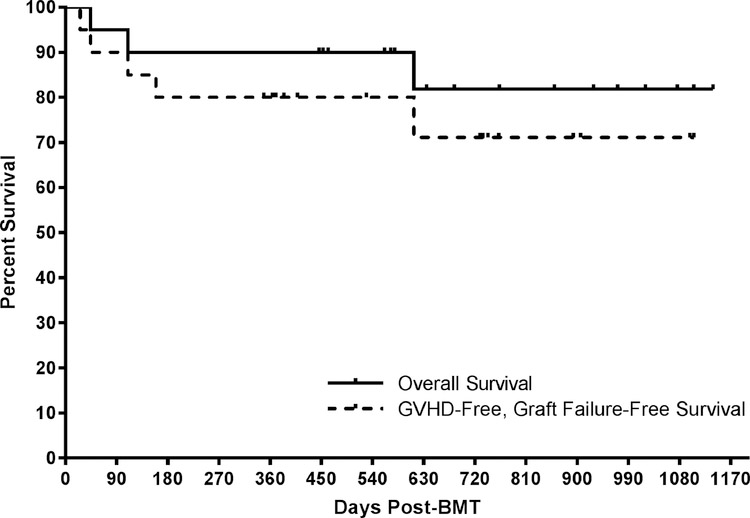
The primary endpoint of GGFS was 80% at day +180 (95% CI 55–92%), with overall survival at 1-year of 90% (95% CI 66–97%), Figure 1. There were 2 early deaths, both infectious, at day +44 (P8) and day +110 (P10). Contributing to P8’s death was severe epistaxis leading to hemorrhagic shock, intubation for airway protection and emergent maxillary artery embolization, now felt to represent a bleeding diathesis previously unappreciated in MAGT1 deficiency.18 An additional patient (P7) had an accidental death on day +613 in the setting of good graft function, complete phenotype reversal including ongoing remission of his EBV+ lymphoma, and no GVHD, organ dysfunction, or infectious issues.
Figure 1.
Kaplan-Meier curves of overall survival and acute grade III-IV GVHD-free, graft-failure-free survival for the cohort, n=20.
Tables 3 and 4 summarize outcomes for the cohort and for individual patients respectively.
Table 3.
Overview of outcomes related to BMT platform.
| Patients (n=20) | |
|---|---|
| Graft failure | 2 (10%) |
| Primary graft failure | 1 (5%) |
| Secondary graft failure | 1 (5%) |
| 1-year transplant-related mortality | 2 (10%) |
| Acute GVHD | |
| Any grade | 4 (20%) |
| Grade II-IV | 3 (15%) |
| Grade III-IV | 1 (5%) |
| Chronic GVHD | 0 |
| Relapse of pre-BMT lymphoproliferative disorder/lymphoma, n=6 | 0 |
| Sinusoidal obstructive syndrome& | 1 (5%) |
| Idiopathic pneumonia syndrome | 1 (5%) |
| Post-BMT donor CD3+ T-lymphocyte infusion, n (%) | 4 (20%) |
| For mixed chimerism or slow engraftment | 3 (15%) |
| For CMV disease | 1 (5%) |
| Second transplant, n (%) | 1 (5%) |
| Freedom from transfusion, n=18 | 18 (100%) |
| Freedom from post-BMT immunosuppression, n=18 | 17 (94%) |
| Freedom from Ig replacement (n=13 survivors on pre-BMT Ig replacement) | 10 (77%) |
| Evidence of phenotype reversal among those with unknown genetic defect, n=3 | 3 (100%) |
| Evidence of phenotype reversal among patients with significantly mixed chimerism, n=2 | 2 (100%) |
Abbreviations: BMT, bone marrow transplantation; GVHD, graft-versus-host disease; CMV, cytomegalovirus; Ig, immunoglobulin
P10 developed sinusoidal obstructive syndrome without reversal of flow on ultrasound or fulfillment of Baltimore criteria, but histologically proven on day +22 liver biopsy performed for hyperbilirubinemia that additionally showed nodular regenerative hyperplasia (presumed to have been present pre-BMT due to prior 6-mercaptopurine treatment), cholestasis of sepsis, and mild hemosiderosis.
Table 4.
Details of individual patient and donor demographics, graft doses, and outcomes.
| Patient | PID | Recipient Age (years) at BMT, Sex | Donor Source, Age (years), Sex | HCT-CI | Bone Marrow Graft Dose | Graft Failure | Subsequent Cell Infusion | Acute GVHD | Chronic GVHD | Most Recent CD3+ Chimerism (% donor) | Most Recent Myeloid Chimerism (% donor) | IgG replacement pre-BMT/post-BMT | Follow-Up | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TNC (×108 cells/kg IBW) | CD3+ (×107 cells/kg IBW) | CD34+ (×106 cells/kg IBW) | |||||||||||||
| P1 | STAT3 deficiency | 7, F | Haplo, 33, F | 1 | 5.2 | 5.1 | 8.7 | No | No | No | No | 98% | 100% | +/+ | A&W, off IS, +3.1 years |
| P2 | PIK3CD GOF | 19, F | MUD, 20, F | 4 | 3.5 | 4.5 | 3.3 | No | No | No | No | 85% | 53% | +/− | A&W, off IS, +3.0 years |
| P3 | Unknown | 52, M | MSD, 56, M | 4 | 4.1 | 1.8 | 3.1 | No | CMV-specific CTLs | No | No | 100% | 100% | +/− | A&W, off IS, +3.0 years |
| P4 | Complete IFNGR1 deficiency | 6, M | MUD, 28, M | 5 | 9.3 | 10.0 | 12.9 | No | No | No | No | 100% | 69% | +/− | A&W, off IS, +2.8 years |
| P5 | STAT3 deficiency | 15, F | MSD, 20, F | 1 | 5.5 | 6.2 | 13.3 | No | No | No | No | 100% | 100% | +/− | A&W, off IS, +2.7 years |
| P6 | Partial IFNGR1 deficiency | 58, F | MSD, 54, F | 3 | 4.5 | 4.0 | 7.7 | No | No | Grade III, gut, steroid responsive | No | 100% | 100% | −/− | A&W, off IS, +2.5 years |
| P7 | Unknown | 29, M | MUD, 26, M | 3 | 3.2 | 2.5 | 2.9 | No | No | Grade I, skin, resolved without treatment | No | 100% | 100% | −/− | Accidental death, no EOD and off IS, day +613 |
| P8 | MAGT1 deficiency | 19, M | Haplo, 17, M | 6 | 4.3 | 5.4 | 4.2 | No | DLI for slow engraftment | No | NE | NE | 97% | +/− | Infectious TRM, day +44 |
| P9 | MAGT1 deficiency | 29, M | MUD, 29, M | 11 | 4.8 | 6.3 | 10.1 | No | No | No | No | 100% | 100% | +/− | A&W, off IS, +2.3 years |
| P10 | IL10R1 deficiency | 28, M | Haplo, 52, F& | 8 | 3.3 | 5.3 | 4.7 | No | Granulocytes during aplasia | Grade II, gut, steroid-responsive | NE | 100% | 100% | +/− | Infectious TRM, day +110 |
| P11 | MAGT1 deficiency | 17, M | MUD, 22, M | 1 | 3.4 | 3.6 | 4.1 | No | No | No | No | 100% | 100% | +/− | A&W, off IS, +2.0 years |
| P12 | NFKB1 haploinsufficiency | 8, F | Haplo, 36, M | 1 | 6.1 | 5.1 | 7.2 | Secondary | DLI × 2 for falling chimerism | No | No | 0% | 3% | +/+ | Alive with improved disease control, off IS, +1.8 years |
| P13 | PIK3CD GOF | 16, F | Haplo, 17, M | 4 | 2.4 | 1.9 | 5.5 | No | DLI for CMV disease | No | No | 100% | 100% | +/sporadic | Alive with complications, on IS for FSGS, +1.7 years |
| P14 | PIK3CD GOF | 4, M | Haplo, 27, M | 0 | 7.2 | 7.3 | 9.2 | Primary | 2nd BMT, followed by DLI for falling chimerism | After 2nd BMT & DLI: Grade III, skin/gut/liver, steroid-refractory | No | 100% | 100% | +/+ | A&W, off IS, +1.5 years |
| P15 | Unknown | 11, F | MUD, 31, F | 0 | 9.3 | 9.5 | 10.7 | No | DLI × 2 for stable, mixed chimerism | No | No | 21% | 65% | +/− | A&W, off IS, +1.5 years |
| P16 | STAT3 deficiency | 12, M | MSD, 15, M | 2 | 5.0 | 5.0 | 8.5 | No | No | No | No | 87% | 100% | −/− | A&W, off IS, +1.5 years |
| P17 | RAG2 deficiency, hypomorphic | 37, M | MUD, 22, M | 1 | 2.8 | 1.9 | 2.5 | No | No | Grade II, gut, steroid responsive | No | 96% | 91% | +/− | A&W, off IS, +1.5 years |
| P18 | Wiskott-Aldrich syndrome | 54, M | MUD, 18, M | 0 | 3.1 | 3.0 | 3.9 | No | No | No | No | 100% | 100% | +/− | A&W, off IS, +1.3 years |
| P19 | RAG1 deficiency, hypomorphic | 4, M | Haplo, 33, M& | 2 | 7.2 | 6.5 | 14.2 | No | No | No | No | 100% | 100% | +/− | A&W, off IS, +1.3 years |
| P20 | IL2RG, revertant | 26, M | MSD, 24, F& | 6 | 4.6 | 2.6 | 4.2 | No | No | No | No | 100% | 100% | −/− | A&W, off IS, +1.2 years |
Abbreviations: PID, primary immune deficiency; BMT, bone marrow transplantation; HCT-CI, Hematopoietic Cell Transplantation-Comorbidity Index; TNC, total nucleated cell; IBW, ideal body weight; GVHD, graft-versus-host disease; GOF, gain of function; F, female; M, male; Haplo, HLA-haploidentical; MUD, 10/10 HLA-matched-unrelated donor; MSD, HLA-matched-sibling donor; CMV, cytomegalovirus; CTL, cytotoxic T lymphocyte; DLI, donor lymphocyte infusion; A&W, alive and well; IS, immunosuppression; EOD, evidence of disease; NE, not evaluable; TRM, transplant-related mortality; FSGS, focal segmental glomerulosclerosis
Donor was a heterozygous carrier. For P20, who had X-linked underlying defect, skewed X-inactivation was confirmed in the donor.
Engraftment and Chimerism
Neutrophil recovery occurred at median day +17 post-BMT (range +14–42) for all patients. The median duration of neutropenia was 9 days (range 6–36). Platelet recovery occurred at median day +30 post-BMT (range +16–45). The CuI of graft failure was 10%. P14 (primary graft failure at day +26) had brisk recovery of autologous, trilineage hematopoiesis (neutrophils on day +14, platelets on day +20), and P12 with secondary graft failure at day +159 had concomitant autologous recovery of trilineage hematopoiesis. Only P12 developed engraftment syndrome, not requiring systemic steroids.
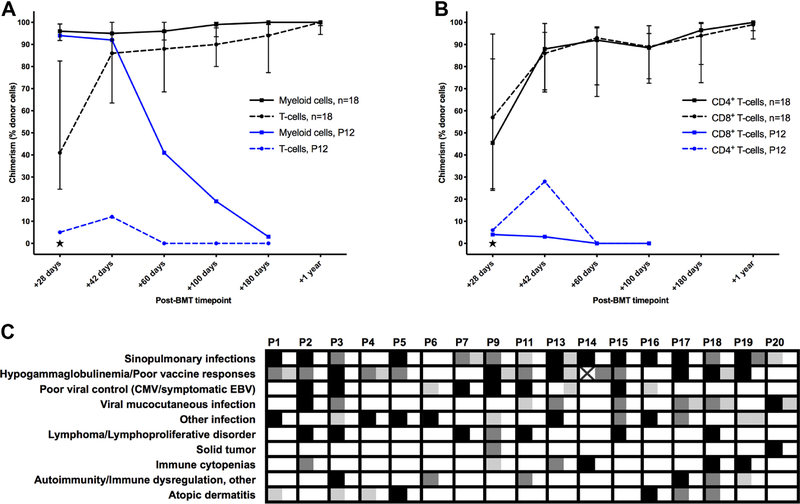
Trends in donor cell engraftment kinetics were observed across all engrafted patients and did not vary by donor type, Figure 2A. Split chimerism, with donor T-cell chimerism markedly lower than myeloid, was observed early post-BMT, with only 5 patients (2 HLA-haploidentical donors, 2 matched unrelated donors, 1 MSD) having predominantly/completely donor cells in both compartments at day +28. At day +28, median donor myeloid chimerism was 96% (range 78–100%, n=19), remaining high on follow-up, while at day +28 median donor T-cell chimerism was 41% (range 9–100%, n=18; P12 5%), rising to median 86% (range 38%−100%, n=18) at day +42. Similar kinetics were observed for CD4+ and CD8+ T-cell chimerism, Figure 2B. Stopping immunosuppression was associated with subsequent conversion to ≥95% donor T-cell chimerism in 7 of 9 cases where T-cell chimerism was <95% donor while on immunosuppression; for 7 patients, T-cell chimerism was ≥95% donor while on immunosuppression, remaining so off immunosuppression. Two patients remain with stable mixed chimerism in both T-cell (85% and 21% donor cells, respectively) and myeloid (53% and 65% donor cells, respectively) subsets, both off immunosuppression for 2.5 years and 1 year, respectively, with phenotype reversal, Figure 2C. Lineage-specific chimerism trends are shown in Supplemental Figure 1.
Figure 2.
Chimerism and phenotype reversal. A) Chimerism in myeloid and CD3+ T-cell subsets, expressed as the percentage of donor cells. Black lines show the median and interquartile range of myeloid (solid line) and CD3+ (dashed line) chimerism for the RIC arm cohort (n=18), excluding the patients with graft failure. Blue lines indicate the percentage of myeloid and CD3+ donor chimerism for P12 with secondary graft failure. P14 with primary graft failure is represented as a single, separate data plot (black star) for myeloid and CD3+ chimerism of 0% on day +28. Most recent chimerism data from patients with follow up beyond 1 year are listed in Table 4. B) Chimerism in CD4+ (solid line) and CD8+ (dashed line) T-cell subsets, shown as subsets shown in panel A for the cohort (n=18, in black), P12 (in blue), and P14 (black star). C) Phenotype reversal in engrafted survivors. For each patient, the left column shows pre-BMT phenotype and the right column post-BMT clinical status. Shading indicates the severity of disease manifestations: black - severe, dark gray - moderate, light gray - mild, white - absent. An X indicates that this disease manifestation could not be assessed, such as due to concomitant immunomodulatory immunoglobulin therapy. The dark gray/”moderate” category also includes historical disease manifestations that were inactive at the time of BMT but represent a significant part of the disease phenotype and indication for transplant, e.g. splenectomy for immune cytopenias (P2, P13), chemotherapy/radiation for lymphoma/lymphoproliferative disorder (P9), Guillain-Barre syndrome (P11). Viral mucocutaneous infections included HPV, HSV, VZV, and molluscum. P13 had significant post-BMT complications, including primary CMV infection resulting in pneumonitis. She also developed focal segmental glomerulosclerosis requiring immunosuppressive therapy. She has 100% donor chimerism across lineages and an underlying PID where full donor chimerism should result in full phenotype reversal. Therefore, the post-BMT grading for phenotype reversal in P13 reflects events likely not related to failure to reverse her disease phenotype, but rather complications in the setting of poor/slow immune reconstitution post-BMT.
Post-BMT donor cell infusions were given to 7 (35%) patients for varied indications and with varied efficacy, detailed in Table 5.
Table 5.
Post-BMT donor cell infusions
| Patient | Donor Cell Infusion Type | DCI Dose | Reason for DCI | Timing of DCI | Chimerism Pre-DCI (% donor) | Chimerism Post-DCI (% donor) | Acute GVHD after DCI | Outcome | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Myeloid | T-cell | Myeloid | T-cell | |||||||
| P3 | Donor-derived tri-virus-specific CTLs | Unknown | CMV infection | +69 | 100% | 100% | 100% | 100% | No | Control of CMV infection |
| P8 | Unconditioned DLI | 5 × 105 CD3+/kg | Slow engraftment | +35 | Whole blood: 50% | 97% | NE | No | Engraftment of neutrophils on day +40, but TRM day +44 | |
| P10 | 3rd party granulocytes | N/A | Planned, during aplasia given active bacterial & fungal infections | +6, +8, +11, +14, +17, +21 | NE | NE | 91% | 98% | Yes, but not related | Unclear benefit - developed cholestasis of sepsis, required abscess drainage, respiratory compromise |
| P12 | Unconditioned DLI Unconditioned DLI |
1 × 106 CD3+/kg 5 × 106 CD3+/kg |
Falling T-cell and myeloid chimerism | +68 +159 |
41% 5% |
0% 0% |
28% 3% |
0% 0% |
No No |
-Brief fevers, abdominal pain – similar but milder to symptoms during initial
engraftment -Very brief fevers, graft loss |
| P13 | Unconditioned DLI | 1 × 105 CD3+/kg | CMV disease – attempt to augment CMV-specific response | +235 | 99% | 98% | 100% | 100% | No | CD8+ T-lymphocytosis with elevated levels of CMV-specific T-cells in the blood. Recovery from CMV pneumonitis. |
| P14 | 2nd BMT& Unconditioned DLI& |
Haplo PBSC graft (same donor) TNC 7.2 × 108/kg CD3+ 7.3 × 107/kg CD34+ 9.2 × 106/kg 5 × 106 CD3+/kg |
Primary graft failure Falling T-cell and myeloid chimerism |
+95 +79 after 2ndBMT |
0% 100% |
0% 40% |
100% 100% |
93% 100% |
No Yes |
Engrafted, but with mixed T-cell chimerism and decreasing blood counts over
time Full donor chimerism, steroid-refractory acute GVHD, grade III, now resolved and off all immunosuppression |
| P15 | Unconditioned DLI Unconditioned DLI |
2 × 106 CD3+/kg 1 × 107 CD3+/kg |
Mixed myeloid and lymphoid chimerism | +227 +304 |
68% 66% |
28% 23% |
69% 63% |
25% 22% |
No No |
Stable chimerism, remained clinically well Stable chimerism, remained clinically well |
Abbreviations: DCI, donor cell infusion; GVHD, graft-versus-host disease; CTL, cytotoxic T-lymphocytes; CMV, cytomegalovirus; DLI, donor lymphocyte infusion; NE, not evaluable (due to insufficient number of cells); TRM, transplant-related mortality; BMT, blood or marrow transplantation; haplo, HLA-haploidentical; PBSC, peripheral blood stem cell
P14 underwent nonemergent second BMT per a published regimen (ref: Klein OR, Chen AR, Gamper C, et al. Alternative-Donor Hematopoietic Stem Cell Transplantation with Post-Transplantation Cyclophosphamide for Nonmalignant Disorders. Biology of blood and marrow transplantation: journal of the American Society for Blood and Marrow Transplantation 2016;22:895–901.) after primary graft failure with autologous recovery. He then had threatened secondary graft failure with declining chimerism and blood counts after the second BMT and received an unconditioned DLI post-second BMT with subsequent aGVHD but also achievement of 100% donor chimerism.
GVHD
The CuI of aGVHD was 20% (95% CI 6–40%), with CuI of grade II-IV aGVHD of 15% (95% CI 4–34%) and grade III-IV aGVHD of 5% (95% CI 0–21%). No patients had steroid-dependent or steroid-refractory aGVHD associated with this BMT platform. P14 underwent second BMT using a different BMT platform and did experience grade III, steroid-refractory aGVHD of the skin, liver, and gut after following that second BMT and DLI.
No patients developed chronic GVHD.
Infectious Complications
Of 9 at-risk patients, 4 (44%) developed CMV reactivation; no patients developed CMV disease following reactivation. Donor-derived CMV-specific cytotoxic T-lymphocytes were administered to P3 on day +69 given intolerance of antiviral agents, with resultant prompt CMV control and no associated toxicity. Primary CMV infections were identified in 4 patients, all children themselves and/or having regular direct contact with young children. Three tolerated the infection with minor or no symptoms at 7 months, 1 year, and 3 years post-BMT while the fourth, P13, developed CMV pneumonitis 7 months post-BMT. Given significant lymphopenia in the setting of CMV pneumonitis, P13 received DLI in hopes of numerically augmenting CMV-specific response although donor remained CMV-seronegative at time of DLI; subsequent studies demonstrated abundant CMV-specific T cells. Severe viral infection occurred in only one other patient (P10), who died of rhinovirus/enterovirus lower respiratory tract-infection (LRTI) and suspected herpes simplex virus encephalitis on day +110.
Clinically significant BK virus-associated hemorrhagic cystitis occurred in 14 (70% of all patients and 82% known at-risk patients) at a median 23 days post-BMT (range 15–74) with median duration of symptoms of 17 days (range 6–124). Therapy with fluoroquinolones or cidofovir was not used. No BK nephropathy occurred.
EBV was frequently detected in whole blood post-BMT, but, of 20 at-risk patients, none required preemptive therapy nor developed post-transplantation lymphoproliferative disorder.
Severe bacterial complications included sepsis and death on day +44 due to health care-associated infection with multi-drug resistant Sphingomonas koreensis (P8), published in detail elsewhere,19 and pneumococcal sepsis at 11 months post-BMT leading to post-infectious cryptogenic organizing pneumonia (P1). Three patients had uncomplicated secondary bacterial pneumonia following viral upper respiratory infection 9–12 months post-BMT, treated as outpatients. Bronchiectasis exacerbations occurred in P7 and P13, both with severe structural abnormalities, in the setting of suboptimal/absent pulmonary hygiene.
Post-BMT fungal infections were infrequent. P1, who had an Aspergillus-colonized pneumatocele pre-BMT, developed an invasive pulmonary aspergillosis at day +28 with associated eosinophilic pneumonia, requiring systemic steroids and tocilizumab along with ongoing posaconazole to prevent Aspergillus resurgence. She had pneumatocele rupture with persistent pneumothorax requiring lobectomy (day +96) and pleurodesis (day +242). P8 was presumed to have disseminated Aspergillosis shortly before his death. Fungal infections requiring oral therapy (n=2) included superficial Trichophyton rubrum and mucocutaneous candidiasis.
Organ Toxicities
This BMT platform has generally not seemed to impact adversely on cardiac or pulmonary function (Supplemental Figure 2). P6 developed idiopathic pneumonia syndrome, which responded to steroids and etanercept, with no clinically significant lung function impairment long-term. Renal injury was infrequent and transient in most cases. Two patients developed ongoing, clinically significant chronic kidney disease. P1 has renal parenchymal echogenicity and requires dual-agent antihypertensive therapy. P13 developed focal segmental glomerulosclerosis (FSGS), collapsing variant, of unclear etiology and is currently maintained on immunosuppression. Interestingly, her otherwise healthy donor has ongoing proteinuria and is of a high-risk race and sex for FSGS, suggesting a previously unappreciated alloimmune/donor-related factor may exist.
One patient (P10) developed histologic evidence of sinusoidal obstructive syndrome (SOS) in the setting of other significant liver pathology.
Endocrine function was evaluated pre- and post-BMT. Three patients developed adrenal insufficiency in the setting of corticosteroid use and posaconazole prophylaxis, now resolved in all but P1. Only one child exhibited suboptimal linear growth post-BMT, also associated with systemic corticosteroids. Post-BMT bone mineral density loss was noted in 6 patients, and two received bisphosphonate therapy. P18 had a previous diagnosis of hypergonadotropic hypogonadism for which he received testosterone replacement pre-BMT. Post-BMT, testosterone remained in the low-normal range, without evidence of bone loss or need for therapy. At 3 years post-BMT, P2 now has regained ovarian function and has return of menstruation. Transient ovarian insufficiency recovered by +1.5 years in P15, aged 11.7 years at time of BMT. Two other adolescent females (P5, P13) have not yet regained ovarian function as of last follow up.
Immune Reconstitution and Phenotype Reversal
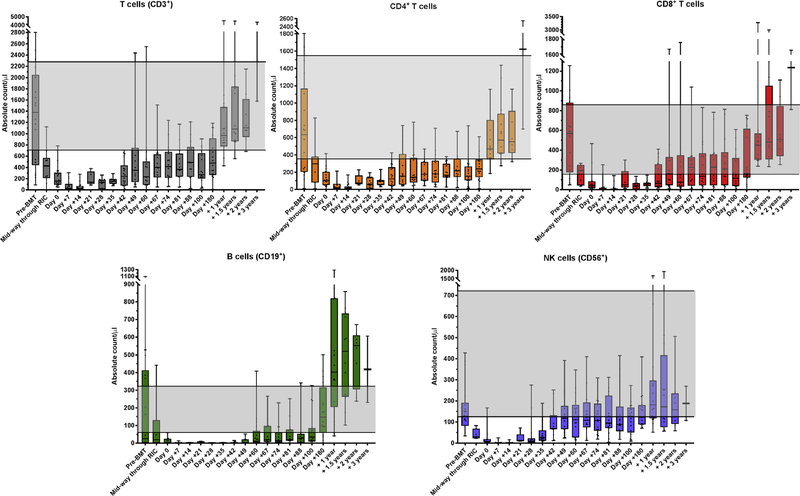
All survivors are off immunosuppression for GVHD prophylaxis or treatment by 6 months post-BMT, although P13 receives immunosuppression for FSGS. Lymphocyte subset reconstitution is shown in Figure 3, with additional details in Supplemental Figures 3 and 4. NK cells recovered first, with median NK-cell numbers within normal range 6–7 weeks post-BMT across age groups. Median total T-cell numbers reached normal age-specific range by day +180 in adults, 1 year in adolescents, and 2 years in younger children, the latter perhaps mediated by CMV-seronegative status of all recipients <12 years old and thus lack of CMV-driven CD8+ T-cell expansion, as has been shown to be a driving factor in CD8+ T-cell recovery previously.20,21 The potential to recover recent thymic emigrants decreased with recipient age, as expected. Total B-cell numbers normalized by day +180 in adolescents and adults and by 1 year in younger children, with memory B cells detectable in varying numbers in all evaluable patients by 1 year post-BMT, comparable to the timing of recovery demonstrated in prior reports of PTCy-based approaches.20
Figure 3.
Post-BMT lymphocyte subset reconstitution, with box-and-whisker plot denoting median and range. Upper and lower limit of institution-specific adult normal range are demarcated for each subset. Patients who experienced graft failure are excluded from this analysis. Of evaluable patients, 47% attained >300 total T cells/ml and 65% attained >50 CD8+ T cells/ml by day +100, while 6% and 44% respectively attained >500 CD4+ T cells/ml by 6 months and 1 year post-BMT; these markers shown to predict survival and graft failure outcomes in young infants and children with severe combined immunodeficiency may not be applicable in an older more heterogeneous population.
All engrafted survivors, even those with mixed chimerism or unknown genetic defect, showed evidence of phenotype reversal (Figure 2C). With median follow up of 1.9 years, humoral recovery in some patients is still in progress, but, in all patients, the PID manifestations that led to BMT referral have either resolved or improved remarkably, even if full phenotype reversal is still evolving.
Post-engraftment inflammatory phenomena were observed in several patients, in response to disseminated mycobacteria (n=3),22 Demodex (n=2), and Aspergillus (n=1), one of whom required systemic steroids to dampen the inflammatory immune response and one of whom had dramatic improvement upon receiving steroids for aGVHD.
Except asplenia prophylaxis, all patients with chronic or recurrent bacterial infections pre-BMT requiring continuous antibiotic use (n=7) have been able to discontinue or, in the case of patients with a high burden of disseminated mycobacterial disease, gradually reduce antimicrobials, without resurgence of infection.
All patients with poor EBV control pre-BMT demonstrated normalization of EBV in the blood (n=12 of 12) and remission from EBV-lymphoproliferative disorder (LPD) or EBV-associated lymphoma (n=6 of 6), with over 1 year of follow-up. No patients experienced relapse after entering BMT with active malignancy (n=2) or in first remission (n=3). All patients with lymphoma who entered BMT in first complete remission received only 2–3 cycles of chemotherapy as a bridge to BMT.
P2, who had a long history of HPV-associated cervical dysplasia, has a normal Pap smear with no detectable HPV 3 years post-BMT, while P20, who presented with extensive full body condylomatous disease and recurrent HPV-associated nasal squamous cell carcinoma, has only a few remaining condylomata with no malignancy recurrence.
Of 13 engrafted survivors who required immunoglobulin replacement pre-BMT, two (P1, P14) continue it at 3 years and 15 months post-BMT respectively, with plans to stop after completion of vaccine series. Another (P13) has maintained normal IgG, IgA, and IgM in the setting of sporadic noncompliance, in contrast to a pattern of low IgG and IgA with high IgM pre-BMT. Hypogammaglobulinemia persists in P4 (suspected to be due to protein-losing enteropathy), P9 and P18, but all demonstrate adequate vaccine responses. All patients with known poor specific antibody titers prior to BMT have either demonstrated adequate response to vaccines received to date or, if too early in vaccine series to evaluate, have normal immunoglobulins, along with class-switched memory B cells.
DISCUSSION
This prospective study demonstrates promising outcomes with a novel RIC-BMT platform, enabling the use of alternative donors and unmanipulated, T-cell-replete grafts across a range of diseases in high-risk PID patients, with partial to complete phenotype reversal in all surviving patients, overall low toxicity, indication that thymic function and gonadal function may be preserved, and markedly low rates of GVHD. The platform and patient population differ from previously published, largely retrospective reports of other promising RIC-BMT approaches for PID23–28 in that our conditioning was radiation-free, there was no in vivo T-cell depletion with serotherapy or ex vivo graft manipulation, and both pediatric and adult patients were included. The rates of graft failure, GVHD, and TRM seen here are lower than other reports of RIC-BMT outcomes for PID where one or more of these complications were more frequent.29–31 The relatively uniform achievement of high myeloid chimerism early post-BMT is notable and we postulate this to be related to a potent and early graft-versus-marrow effect, as the preparative regimen was not myeloablative. The use of DLI was not infrequent in this study, as similarly reported with other RIC-BMT approaches and best captured in a multi-center, phase II trial of RIC-BMT for PID by Allen and colleagues in which 50% of patients had graft failure or required DLI for falling/low donor chimerism and the 1-year probability of being alive with sustained engraftment (>5% donor cells in whole blood) without intervention was 39%, with 61% alive with sustained engraftment with or without intervention.27 Using the same engraftment definitions, our platform compares favorably, with 1-year probability of survival with sustained engraftment without intervention of 75% and with or without intervention of 85%; most patients became full donor chimeras without intervention, often following the cessation of GVHD prophylaxis with sirolimus. The ability of unconditioned DLI to improve mixed chimerism after BMT may ultimately be low, but data presented here and by others suggest that mixed chimerism may not require intervention with DLI, given that it can be stable over time and sufficient for phenotype reversal for some PIDs.23,24,27,32
Although PTCy is known to effectively decrease chronic GVHD incidence including in PID patients,23,25,33–35 the complete absence of chronic GVHD in this study, confirmed on serial, comprehensive evaluations, is one of the most clinically important and promising findings. The low incidence of severe acute and chronic GVHD may be partly related to the gradual increase in donor T cells noted in most patients, allowing for early mixed chimerism, which may be tolerogenic. Even so, our GVHD outcomes stand in contrast to non-PTCy-based approaches to RIC-BMT for PID, even ones that result in potentially-protective mixed chimerism.27,28,36 Notably, the low incidence of GVHD did not compromise control of malignancy and LPD, with all patients with pre-BMT malignancy/LPD remaining in remission, or of pre-BMT immune cytopenias, which also resolved. The immune reconstitution demonstrated herein is in line with previously published immune reconstitution data in the PTCy setting.20 Furthermore, this report provides the first in-depth evaluation of immune reconstitution in patients with PID transplanted using serotherapy-free, PTCy-based approaches and is notably unhindered in this assessment given the low rates of GVHD and freedom from immunosuppression by day +180 after BMT.
However, the mixed T-cell chimerism seen here early after BMT may not be tolerated in all patients, depending on the underlying disease-causing mutation and if host immune cells have a selective advantage over donor cells. As published by others and demonstrated here, the engraftment of patients with GOF mutations, such as in PIK3CD, is variable, and we have deemed the BMT approach herein to require additional modifications to hopefully decrease graft failure rates for these patients.37,38 Sirolimus, a mammalian target of rapamycin (mTOR) inhibitor that can rescue the host T-cell defects in patients with PIK3CD GOF mutations,39 may hinder engraftment of donor T cells when used as GVHD prophylaxis in patients with PIDs where the causative mutation drives hyperactivation of the AKT-mTOR pathway. As a result, we have stopped using mTOR inhibitors as part of GVHD prophylaxis in patients with PIK3CD GOF mutations. As we continue to focus on RIC approaches to transplant but also recognize that this RIC approach may not be optimal for all patients with PID, we have subsequently tailored this approach for patients with PIK3CD GOF mutations or other diseases of T-cell dysregulation and/or proliferation by using peripheral blood stem cell grafts and adding distal serotherapy for augmented host lymphodepletion.
The incidence of graft failure was respectably low for a RIC-BMT approach in non-malignant diseases, and patients with graft failure had immediate autologous reconstitution. Both patients with graft failure did receive HLA-haploidentical grafts, which may represent part of the barrier to engraftment. However, the engraftment kinetics and chimerism for the 5 other recipients of HLA-haploidentical grafts in this study was on par with that of the recipients of HLA-matched grafts. Thus, our assessment is that the graft failure events relate much more to underlying disease features, disease activity in the peri-engraftment period, and, in P14, under-dosing of his busulfan due to the inability to perform pharmacokinetics and use of sirolimus in a PIK3CD GOF patient, although more transplants will need to be performed across donor types using this platform to gain more clarity on the factors contributing to graft failure. At present, there are no published PTCy-based, haplo transplant approaches for patients with PID that similarly avoid serotherapy, radiation, and/or myeloablation for direct comparison to this platform. Approaches that do include one or more of these factors have resulted in high engraftment rates with haplo donors in patients with PID.23,35,40,41 Regardless, further improving engraftment without sacrificing the favorable aspects of this platform is desirable. Across all hard-to-engraft diseases, augmented host lymphodepletion, such as with intermediate-timed serotherapy,42 may improve engraftment without escalating conditioning to myeloablative levels. In this study, marrow grafts were used, although peripheral blood stem cell grafts could be considered as another measure to decrease the risk of graft failure, albeit potentially with a higher risk of GVHD. Myeloablative conditioning (MAC) is another approach to decrease graft failure rates in PIDs, but needs to be considered in view of the guaranteed and potential short- and long-term toxicities. Most patients in this study entered BMT with significant co-morbidities, particularly lung and/or liver dysfunction. Half had HCT-CI scores of ≥3; similar rates of high-risk patients requiring BMT for PID have been published by others.36 In a registry analysis of HCT-CI in non-malignant diseases, HCT-CI scores ≥3 were associated with a significant decrease in survival43 and, because severe combined immunodeficiency represented nearly half of PID patients in that study, the extent of comorbidities seen in older patients with PIDs requiring BMT were almost certainly underrepresented. While reduced-toxicity, treosulfan-containing MAC regimens for PID have yielded very good outcomes, treosulfan is not available worldwide, rates of long-term toxicities such as infertility are not well-defined, and SOS risk is not eliminated.44–50 Additionally, underlying liver pathology may not always be identified pre-BMT, potentially making this patient population more vulnerable to SOS. Thus, MAC-based approaches may not be clinically feasible or desired for many patients with PID referred for BMT.
Serious infectious complications were overall modest for this high-risk cohort, suggesting favorable immune reconstitution and likely due in large part to the freedom from immunosuppression afforded by low GVHD rates. Significant bacterial and fungal complications were largely prevented with standard approaches to prophylaxis and empiric therapy. While detection of respiratory viruses was common, LRTIs were rare. No patients had clinically significant EBV-associated complications, consistent with outcomes previously published with PTCy-based approaches.51 CMV reactivation was controlled with pre-emptive therapy alone in all but one patient, which could in part be associated with the use of sirolimus.16,52 Notably, post-BMT primary CMV infection was not uncommon; all cases occurred after weekly CMV monitoring had stopped, and one case progressed to CMV disease. BK-associated hemorrhagic cystitis did not lead to any long-term sequelae, but it posed significant transient morbidity for patients. The high rates of BK-associated hemorrhagic cystitis are thought to be related to the combination of 1) a high-risk patient population with frequent BK virus detection pre-BMT conferring higher risk of symptomatic cystitis post-BMT, 2) the use of PTCy, and 3) the use of busulfan,53 with busulfan felt to be a significant co-factor given that we have not observed BK-associated hemorrhagic cystitis in our patients with PID who receive a lower-intensity transplant approach that is identical except that it does not contain busulfan. Of note, BK-associated hemorrhagic cystitis incidence did not vary with donor type, as has been shown elsewhere.54
The outcomes presented here, coupled with recently reported impressive BMT outcomes by others,23,36,55 support the safety and efficacy of RIC-BMT for patients across a broad range of PIDs, even those with significant comorbidities, older age, active infection/malignancy, only alternative donor options, and immune-dysregulation phenotypes. The spectrum of PIDs continues to expand, and the present era is one far different than when BMT for PID was used pre-emptively in very young children with diseases uniformly associated with early mortality. The cohort of patients represented here, with no patient younger than 4 years old, is distinctly different from patients with severe combined immunodeficiency who require immediate transplant in infancy and thus the approach, outcomes, and discussion should not be generalized to that patient population.
RIC-BMT approaches for PID will likely remain at the forefront of the field moving forward, as patients will either be referred for BMT when their disease-related comorbidities prohibit MAC, or earlier in their disease course when the risk of MAC-associated morbidity and mortality is difficult to justify. Thus, continued investigation into how to further modify promising RIC-BMT approaches to optimize outcomes, tailoring them as we gain greater understanding of the challenges related to graft failure, organ toxicity, and immune reconstitution that may lie within specific PIDs or disease phenotypes, is essential to further the application of this potentially curative therapy to all who require it.56,57 Investigation into the performance of this novel platform in other non-malignant diseases is also of interest. The worldwide availability of the platform presented here offers an alternative to approaches that use treosulfan, alemtuzumab, or graft manipulation techniques such as alpha/beta T-cell depletion, which are not globally available, are costlier, and/or require specialized technology and expertise.58 Long-term follow-up on the relationship between mixed chimerism and both phenotype reversal and late graft failure, as well as the potential for RIC to afford patients preserved fertility and fewer late toxicities, will be critical to gauge the true, durable success of this approach. Ongoing efforts at NIH include modifications to this platform to help engraftment for PID patients with more difficult-to-engraft diseases and shortening of GVHD prophylaxis to improve immune reconstitution and viral control.
Supplementary Material
Highlights.
We designed a novel reduced intensity radiation- and serotherapy-free BMT platform.
A high-risk cohort of 20 primary immunodeficiency children and adults received BMT.
Acute GVHD rates were low; no chronic GVHD occurred even with alternative donor use.
Low toxicity and mortality were observed.
All engrafted patients show evidence of phenotype reversal.
ACKNOWLEDGMENTS
The authors wish to thank the patients, their families, and the donors who participated in this trial. We thank the providers of the Experimental Transplantation and Immunology Branch and consultants throughout the NIH Clinical Center who cared for the patients, Sharon Adams and staff of the HLA lab, the Department of Transfusion Medicine and Cell Processing Section, Dr. Alina Dulau-Florea and the staff of the Chimerism Lab, Frances T. Hakim and the staff of the Preclinical Development and Clinical Monitoring Facility and the Experimental Transplantation and Immunology Branch Flow Cytometry Core, and the referring doctors who assisted in ongoing post-transplant care of patients upon return home. The authors thankfully acknowledge the generosity of the Mackenzie family in their donation to support the research of transplant for children with primary immunodeficiency diseases. This project has been funded in whole or in part with federal funds from the National Cancer Institute, National Institutes of Health, under contract number HHSN261200800001E. The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does the mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government.
Footnotes
Conflict of interest statement: None of the authors have any conflicts of interest.
CONFLICTS OF INTEREST DISCLOSURE: The authors declare no competing financial interests.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Picard C, Bobby Gaspar H, Al-Herz W, et al. International Union of Immunological Societies: 2017 Primary Immunodeficiency Diseases Committee Report on Inborn Errors of Immunity. J Clin Immunol 2018;38:96–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rosenberg E, Dent PB, Denburg JA. Primary Immune Deficiencies in the Adult: A Previously Underrecognized Common Condition. J Allergy Clin Immunol Pract 2016;4:1101–7. [DOI] [PubMed] [Google Scholar]
- 3.Kobrynski L, Powell RW, Bowen S. Prevalence and morbidity of primary immunodeficiency diseases, United States 2001–2007. J Clin Immunol 2014;34:954–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Connelly JA. Hematopoietic Stem Cell Transplant for a New Primary Immunodeficiency Disorder: A Voyage Where No Transplant Physician Has Gone Before. Biol Blood Marrow Transplant 2017;23:863–4. [DOI] [PubMed] [Google Scholar]
- 5.Acevedo MJ, Wilder JS, Adams S, et al. Outcomes of Related and Unrelated Donor Searches Among Patients with Primary Immunodeficiency Diseases Referred for Allogeneic Hematopoietic Cell Transplantation. Biol Blood Marrow Transplant 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mossoba ME, Halverson DC, Kurlander R, et al. High-Dose Sirolimus and Immune-Selective Pentostatin plus Cyclophosphamide Conditioning Yields Stable Mixed Chimerism and Insufficient Graft-versus-Tumor Responses. Clin Cancer Res 2015;21:4312–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mariotti J, Taylor J, Massey PR, et al. The pentostatin plus cyclophosphamide nonmyeloablative regimen induces durable host T cell functional deficits and prevents murine marrow allograft rejection. Biol Blood Marrow Transplant 2011;17:620–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McCurdy SR, Kasamon YL, Kanakry CG, et al. Comparable composite endpoints after HLA-matched and HLA-haploidentical transplantation with post-transplantation cyclophosphamide. Haematologica 2017;102:391–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.How J, Slade M, Vu K, et al. T Cell-Replete Peripheral Blood Haploidentical Hematopoietic Cell Transplantation with Post-Transplantation Cyclophosphamide Results in Outcomes Similar to Transplantation from Traditionally Matched Donors in Active Disease Acute Myeloid Leukemia. Biol Blood Marrow Transplant 2017;23:648–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ghosh N, Karmali R, Rocha V, et al. Reduced-Intensity Transplantation for Lymphomas Using Haploidentical Related Donors Versus HLA-Matched Sibling Donors: A Center for International Blood and Marrow Transplant Research Analysis. J Clin Oncol 2016;34:3141–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moiseev IS, Pirogova OV, Alyanski AL, et al. Risk-adapted GVHD prophylaxis with post-transplantation cyclophosphamide in adults after related, unrelated, and haploidentical transplantations. Eur J Haematol 2018;100:395–402. [DOI] [PubMed] [Google Scholar]
- 12.Raiola AM, Dominietto A, di Grazia C, et al. Unmanipulated haploidentical transplants compared with other alternative donors and matched sibling grafts. Biol Blood Marrow Transplant 2014;20:1573–9. [DOI] [PubMed] [Google Scholar]
- 13.DeZern AE, Zahurak M, Symons H, Cooke K, Jones RJ, Brodsky RA. Alternative Donor Transplantation with High-Dose Post-Transplantation Cyclophosphamide for Refractory Severe Aplastic Anemia. Biol Blood Marrow Transplant 2017;23:498–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Przepiorka D, Weisdorf D, Martin P, et al. 1994 Consensus Conference on Acute GVHD Grading. Bone Marrow Transplant 1995;15:825–8. [PubMed] [Google Scholar]
- 15.Jagasia MH, Greinix HT, Arora M, et al. National Institutes of Health Consensus Development Project on Criteria for Clinical Trials in Chronic Graft-versus-Host Disease: I. The 2014 Diagnosis and Staging Working Group report. Biology of blood and marrow transplantation : journal of the American Society for Blood and Marrow Transplantation 2015;21:389–401 e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Melendez-Munoz R, Marchalik R, Jerussi T, et al. Cytomegalovirus Infection Incidence and Risk Factors Across Diverse Hematopoietic Cell Transplantation Platforms Using a Standardized Monitoring and Treatment Approach: A Comprehensive Evaluation from a Single Institution. Biol Blood Marrow Transplant 2019;25:577–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sorror M, Storer B, Sandmaier BM, et al. Hematopoietic cell transplantation-comorbidity index and Karnofsky performance status are independent predictors of morbidity and mortality after allogeneic nonmyeloablative hematopoietic cell transplantation. Cancer 2008;112:1992–2001. [DOI] [PubMed] [Google Scholar]
- 18.Dimitrova D, Rose JJ, Uzel G, et al. Successful Bone Marrow Transplantation for XMEN: Hemorrhagic Risk Uncovered. J Clin Immunol 2019;39:1–3. [DOI] [PubMed] [Google Scholar]
- 19.Johnson RC, Deming C, Conlan S, et al. Investigation of a Cluster of Sphingomonas koreensis Infections. N Engl J Med 2018;379:2529–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kanakry CG, Coffey DG, Towlerton AM, et al. Origin and evolution of the T cell repertoire after posttransplantation cyclophosphamide. JCI Insight 2016;1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ogonek J, Varanasi P, Luther S, et al. Possible Impact of Cytomegalovirus -Specific CD8(+) T Cells on Immune Reconstitution and Conversion to Complete Donor Chimerism after Allogeneic Stem Cell Transplantation. Biol Blood Marrow Transplant 2017;23:1046–53. [DOI] [PubMed] [Google Scholar]
- 22.Manion M, Dimitrova D, Pei L, et al. IRIS as a post-transplantation complication in primary immunodeficiency with disseminated M. avium. Clin Infect Dis 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Klein OR, Chen AR, Gamper C, et al. Alternative-Donor Hematopoietic Stem Cell Transplantation with Post-Transplantation Cyclophosphamide for Nonmalignant Disorders. Biol Blood Marrow Transplant 2016;22:895–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Marsh RA, Rao MB, Gefen A, et al. Experience with Alemtuzumab, Fludarabine, and Melphalan Reduced-Intensity Conditioning Hematopoietic Cell Transplantation in Patients with Nonmalignant Diseases Reveals Good Outcomes and That the Risk of Mixed Chimerism Depends on Underlying Disease, Stem Cell Source, and Alemtuzumab Regimen. Biol Blood Marrow Transplant 2015;21:1460–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Thakkar D, Katewa S, Rastogi N, Kohli S, Nivargi S, Yadav SP. Successful Reduced Intensity Conditioning Alternate Donor Stem Cell Transplant for Wiskott-Aldrich Syndrome. J Pediatr Hematol Oncol 2017;39:e493–e6. [DOI] [PubMed] [Google Scholar]
- 26.Ono S, Okano T, Hoshino A, et al. Hematopoietic Stem Cell Transplantation for XIAP Deficiency in Japan. J Clin Immunol 2017;37:85–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Allen CE, Marsh R, Dawson P, et al. Reduced-intensity conditioning for hematopoietic cell transplant for HLH and primary immune deficiencies. Blood 2018;132:1438–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Marsh RA, Vaughn G, Kim MO, et al. Reduced-intensity conditioning significantly improves survival of patients with hemophagocytic lymphohistiocytosis undergoing allogeneic hematopoietic cell transplantation. Blood 2010;116:5824–31. [DOI] [PubMed] [Google Scholar]
- 29.Wehr C, Gennery AR, Lindemans C, et al. Multicenter experience in hematopoietic stem cell transplantation for serious complications of common variable immunodeficiency. J Allergy Clin Immunol 2015;135:988–97 e6. [DOI] [PubMed] [Google Scholar]
- 30.Grossman J, Cuellar-Rodriguez J, Gea-Banacloche J, et al. Nonmyeloablative allogeneic hematopoietic stem cell transplantation for GATA2 deficiency. Biol Blood Marrow Transplant 2014;20:1940–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Horwitz ME, Barrett AJ, Brown MR, et al. Treatment of chronic granulomatous disease with nonmyeloablative conditioning and a T-cell-depleted hematopoietic allograft. N Engl J Med 2001;344:881–8. [DOI] [PubMed] [Google Scholar]
- 32.Cooper N, Rao K, Goulden N, Webb D, Amrolia P, Veys P. The use of reduced-intensity stem cell transplantation in haemophagocytic lymphohistiocytosis and Langerhans cell histiocytosis. Bone Marrow Transpl 2008;42:S47–S50. [DOI] [PubMed] [Google Scholar]
- 33.Shah NN, Freeman AF, Su H, et al. Haploidentical Related Donor Hematopoietic Stem Cell Transplantation for Dedicator-of-Cytokinesis 8 Deficiency Using Post-Transplantation Cyclophosphamide. Biol Blood Marrow Transplant 2017;23:980–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rastogi N, Katewa S, Thakkar D, Kohli S, Nivargi S, Yadav SP. Reduced-toxicity alternate-donor stem cell transplantation with posttransplant cyclophosphamide for primary immunodeficiency disorders. Pediatr Blood Cancer 2018;65. [DOI] [PubMed] [Google Scholar]
- 35.Parta M, Shah NN, Baird K, et al. Allogeneic Hematopoietic Stem Cell Transplantation for GATA2 Deficiency Using a Busulfan-Based Regimen. Biol Blood Marrow Transplant 2018;24:1250–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fox TA, Chakraverty R, Burns S, et al. Successful outcome following allogeneic hematopoietic stem cell transplantation in adults with primary immunodeficiency. Blood 2018;131:917–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nademi Z, Slatter MA, Dvorak CC, et al. Hematopoietic stem cell transplant in patients with activated PI3K delta syndrome. J Allergy Clin Immunol 2017;139:1046–9. [DOI] [PubMed] [Google Scholar]
- 38.Okano T, Imai K, Tsujita Y, et al. Hematopoietic stem cell transplantation for progressive combined immunodeficiency and lymphoproliferation in patients with activated phosphatidylinositol-3-OH kinase delta syndrome type 1. J Allergy Clin Immunol 2018. [DOI] [PubMed] [Google Scholar]
- 39.Lucas CL, Kuehn HS, Zhao F, et al. Dominant-activating germline mutations in the gene encoding the PI(3)K catalytic subunit p110delta result in T cell senescence and human immunodeficiency. Nat Immunol 2014;15:88–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Neven B, Diana JS, Castelle M, et al. Haploidentical Hematopoietic Stem Cell Transplantation with Post-Transplant Cyclophosphamide for Primary Immunodeficiencies and Inherited Disorders in Children. Biol Blood Marrow Transplant 2019. [DOI] [PubMed] [Google Scholar]
- 41.Kurzay M, Hauck F, Schmid I, et al. T-cell replete haploidentical bone marrow transplantation and post-transplant cyclophosphamide for patients with inborn errors. Haematologica 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Marsh RA, Kim MO, Liu CY, et al. An Intermediate Alemtuzumab Schedule Reduces the Incidence of Mixed Chimerism Following Reduced-Intensity Conditioning Hematopoietic Cell Transplantation for Hemophagocytic Lymphohistiocytosis. Biol Blood Marrow Tr 2013;19:1625–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Thakar M, Broglie L, Logan B, et al. The Hematopoietic Cell Transplant Comorbidity Index predicts survival after allogeneic transplant for non-malignant diseases. Blood 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Morillo-Gutierrez B, Beier R, Rao K, et al. Treosulfan-based conditioning for allogeneic HSCT in children with chronic granulomatous disease: a multicenter experience. Blood 2016;128:440–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Slatter MA, Boztug H, Potschger U, et al. Treosulfan-based conditioning regimens for allogeneic haematopoietic stem cell transplantation in children with non-malignant diseases. Bone Marrow Transplant 2015;50:1536–41. [DOI] [PubMed] [Google Scholar]
- 46.Slatter MA, Rao K, Amrolia P, et al. Treosulfan-based conditioning regimens for hematopoietic stem cell transplantation in children with primary immunodeficiency: United Kingdom experience. Blood 2011;117:4367–75. [DOI] [PubMed] [Google Scholar]
- 47.Aydin SE, Freeman AF, Al-Herz W, et al. Hematopoietic Stem Cell Transplantation as Treatment for Patients with DOCK8 Deficiency. J Allergy Clin Immunol Pract 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Haskologlu S, Kostel Bal S, Islamoglu C, et al. Outcome of treosulfan-based reduced-toxicity conditioning regimens for HSCT in high-risk patients with primary immune deficiencies. Pediatr Transplant 2018;22:e13266. [DOI] [PubMed] [Google Scholar]
- 49.Faraci M, Diesch T, Labopin M, et al. Gonadal Function after Busulfan Compared with Treosulfan in Children and Adolescents Undergoing Allogeneic Hematopoietic Stem Cell Transplant. Biol Blood Marrow Transplant 2019. [DOI] [PubMed] [Google Scholar]
- 50.Faraci M, Bertaina A, Luksch R, et al. Sinusoidal Obstruction Syndrome/Veno-Occlusive Disease after Autologous or Allogeneic Hematopoietic Stem Cell Transplantation in Children: a retrospective study of the Italian Hematology-Oncology Association-Hematopoietic Stem Cell Transplantation Group. Biol Blood Marrow Transplant 2019;25:313–20. [DOI] [PubMed] [Google Scholar]
- 51.Kanakry JA, Kasamon YL, Bolanos-Meade J, et al. Absence of post-transplantation lymphoproliferative disorder after allogeneic blood or marrow transplantation using post-transplantation cyclophosphamide as graft-versus-host disease prophylaxis. Biol Blood Marrow Transplant 2013;19:1514–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Guglieri-Lopez B, Perez-Pitarch A, Garcia-Cadenas I, et al. Effect of Sirolimus Exposure on the Need for Preemptive Antiviral Therapy for Cytomeglovirus Infection after Allogeneic Hematopoietic Stem Cell Transplantation. Biol Blood Marrow Transplant 2019;25:1022–30. [DOI] [PubMed] [Google Scholar]
- 53.Gilis L, Morisset S, Billaud G, et al. High burden of BK virus-associated hemorrhagic cystitis in patients undergoing allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant 2014;49:664–70. [DOI] [PubMed] [Google Scholar]
- 54.Copelan OR, Sanikommu SR, Trivedi JS, et al. Higher Incidence of Hemorrhagic Cystitis Following Haploidentical Related Donor Transplantation Compared with Matched Related Donor Transplantation. Biol Blood Marrow Transplant 2019;25:785–90. [DOI] [PubMed] [Google Scholar]
- 55.Gungor T, Teira P, Slatter M, et al. Reduced-intensity conditioning and HLA-matched haemopoietic stem-cell transplantation in patients with chronic granulomatous disease: a prospective multicentre study. Lancet 2014;383:436–48. [DOI] [PubMed] [Google Scholar]
- 56.Duarte RF, Labopin M, Bader P, et al. Indications for haematopoietic stem cell transplantation for haematological diseases, solid tumours and immune disorders: current practice in Europe, 2019. Bone Marrow Transplant 2019. [DOI] [PubMed] [Google Scholar]
- 57.Dvorak CC, Long-Boyle J, Dara J, et al. Low Exposure Busulfan Conditioning to Achieve Sufficient Multilineage Chimerism in Patients with Severe Combined Immunodeficiency. Biol Blood Marrow Transplant 2019;25:1355–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Weisdorf D, Ruiz-Arguelles GJ, Srivastava A, Gomez-Almaguer D, Szer J. Economic Challenges in Hematopoietic Cell Transplantation: How Will New and Established Programs Face the Growing Costs? Biol Blood Marrow Transplant 2017;23:1815–6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.