Abstract
Driving under the influence of cannabis (DUIC) is a public health concern, and data are needed to develop screening and prevention tools. Measuring the level of intoxication that cannabis users perceive as safe for driving could help stratify DUIC risk. This study tested whether intoxication levels perceived as safe for driving predicted past-month DUIC frequency. Online survey data were collected in 2017 from a national sample of n=3,010 past-month cannabis users with lifetime DUIC (age 18+). Respondents indicated past-month DUIC frequency, typical cannabis intoxication level (1–10 scale), and cannabis intoxication level perceived as safe for driving (0–10 scale). Approximately 24%, 38%, 13%, and 24% of respondents engaged in DUIC on 0, 1–9, 10–19, and 20–30 days respectively in the past month. Among these four DUIC frequency groups, median typical intoxication varied little (5–6), but median intoxication perceived as safe for driving varied widely (3–8). Higher intoxication levels perceived as safe for driving corresponded to frequent DUIC (Spearman’s rho: 0.46). For each unit increase in intoxication level perceived as safe for driving, the odds of past-month DUIC increased 18% to 68% (multinomial logistic regression odds ratio - MOR1–9 days: 1.18, 95% CI: 1.13–1.23; MOR10–19 days: 1.40, 95% CI: 1.30–1.50; MOR20–30 days: 1.68, 95% CI: 1.57–1.80). In this targeted sample of past-month cannabis users, DUIC frequency varied widely, but daily/near-daily DUIC was common (24%). Measuring intoxication levels perceived as safe for driving permits delineation of past-month DUIC frequency. This metric has potential as a component of public health prevention tools.
Keywords: Cannabis, Marijuana, Driving under the influence, Intoxication, Risk perception
Introduction
As U.S. states continue to legalize medical and recreational cannabis, the prevalence of adult cannabis use in the general population is increasing,1,2 as is the prevalence of driving under the influence of cannabis (DUIC).3 Increases in DUIC pose a serious public health problem given that the acute effects of tetrahydrocannabinol (THC) administration include psychomotor impairments that elevate the risk of motor vehicle accidents.4–9 Despite this knowledge, actionable data that can be used to prevent DUIC on a population-level scale are limited – creating a need to examine DUIC and related factors to inform empirically-based screening practices and prevention efforts.
From a public safety perspective, the days, hours, and minutes preceding the decision to drive under the influence of cannabis represent critical intervention points. As such, research efforts might focus specifically on identifying those factors that precede, predict, and modify DUIC behavior. One of these potential factors is risk perception – a psychological construct noted for its utility in predicting DUIC.10–12 However, at present, data concerning the functional relationship between DUIC risk perception and DUIC behaviors are lacking,12 and there appear to be idiosyncrasies that warrant further scrutiny. For example, data from driving simulation studies indicate that unlike individuals who are under the influence of alcohol, those under the influence of THC drive more slowly and reduce risky driving behaviors – suggesting that these drivers are aware of their intoxication-induced deficits and may be attempting to compensate for those deficits.13,14 Perhaps unsurprisingly, multiple self-report and focus-group studies suggest that cannabis consumers perceive DUIC as less dangerous than alcohol-impaired driving.15–18
DUIC risk-perceptions appear to be comprised (at least in part) of several distinct beliefs concerning the safety of DUIC. Some individuals believe they can drive safely under the influence of cannabis by engaging in compensatory driving behaviors that mitigate risk; others believe that cannabis does not impair their driving ability at all; and still others believe that using cannabis improves their driving ability.15–18 Each of these beliefs is unique in its own right, but in many respects, each is a derivative of one overarching construct: the perception of cannabis intoxication’s impact on one’s ability to drive safely.
In the alcohol literature, the perceived safety of driving at a given level of intoxication is a known subcomponent of the overall perceived risk of drunk driving,19,20 and enables identification and stratification of impaired-driving risk profiles.21,22 For example, simply asking individuals if they believe it is safe to drive after consuming alcohol fails to make critical distinctions between those who believe it is safe to drive after consuming one alcoholic beverage, and those who believe it is safe to drive after consuming four. Analogous considerations are largely absent from analyses of cannabis-impaired driving. Ideally, the perceived risk of DUIC could be examined in relation to beliefs about the effects of consuming specific quantities of THC. However, such metrics are currently unavailable.23 Self-reported intoxication could potentially serve as a useful proxy that may help us make critical distinctions in DUIC risk.
The present study uses data from a large, demographically- and behaviorally-heterogeneous sample to address the following question: Do self-reported measures of the level of cannabis intoxication that one perceives as safe for driving predict the frequency of DUIC in the past month among current cannabis users with a lifetime history of DUIC?
Methods
Recruitment Strategy
We used a social media-based data collection strategy24 to recruit cannabis users to participate in an anonymous online survey. Between 08/14/2017 to 10/01/2017, a URL link to a Qualtrics25 survey was distributed to individuals age 18–65 living in the U.S. via Facebook advertisements. Potential participants who clicked the advertisement were directed to the survey consent page. We used two recruitment strategies to obtain data from frequent and less frequent cannabis users. In the first strategy, cannabis-specific advertisements were directed to the Facebook accounts of frequent cannabis users. No incentives were used in the first strategy because frequent cannabis users willingly respond to online surveys and provide valid data without requiring incentives.24,26–28 In the second strategy, we directed generic advertisements to the Facebook accounts of less-frequent cannabis users and incentivized survey completion with an online raffle for a $10 Amazon gift code. The Dartmouth Committee for the Protection of Human Subjects approved the study protocol.
Survey Design and Participants
The survey assessed demographics (e.g., age, state residence), patterns of cannabis use (e.g., frequency of use, route of administration) and perceptions and patterns of DUIC. Respondents were reminded repeatedly throughout the survey that responses were anonymous. Survey items used a forced-choice format. Respondents were required to provide consent and report their current age before beginning the survey. Those under the age of 18 were automatically disqualified.
Multiple data quality assurance features were used. To avoid false responses from internet bots, we used the “captcha verification” data quality feature. To prevent individuals from completing the survey more than once, we used the “Prevent Ballot Box Stuffing” data quality feature. Data cleaning involved checking for logical consistency and reliability across questions (e.g., current age ≥ age of cannabis initiation, reported date of birth matches reported age, similar responses to different versions of the same question). After removing respondents who did not provide logical or consistent answers, the resulting dataset consisted of n=9,258 participants. Of these individuals, n=4,308 (47%) reported using cannabis at least once within the past month. We considered past-month users with no lifetime DUIC (and therefore no past-month DUIC) as being substantively different from, and at a distinctly lower risk than, past-month users with lifetime DUIC but no past-month DUIC. For this reason, we further limited the sample to those who had engaged in DUIC at least once in their life (sensitivity analyses of past-month users with no lifetime DUIC are presented in the supplemental material). Of the n=4,308 past-month users, n=4,107 (95%) responded to the lifetime DUIC question. Among these participants, n=3,039 (74%) reported lifetime DUIC and n=1,068 (26%) reported no lifetime DUIC. Of those who reported lifetime DUIC, n=3,010 (99%) reported their past-month frequency of DUIC. This paper presents an analysis of these n=3,010 respondents.
Measures
DUIC Frequency (Past Month)
We assessed the frequency of past-month DUIC by asking participants the following question: ―Think about how high you typically get when you use cannabis. In the past 30 days, how many days have you driven a car within 2 hours after getting that high?” The response options were: 0 days, 1–2 days, 3–5 days, 6–9 days, 10–19 days, 20–25 days, 26–29 days, all 30 days. For analyses, this variable was collapsed into four groups: (1) 0 days of DUIC in the past month (2) 1–9 days of DUIC in the past month, (3) 10–19 days of DUIC in the past month, and (4) 20–30 days of DUIC in the past month. This was done to make the DUIC frequency groups comparable (i.e., equal range of days of DUIC for each group) and ensure sample sizes that would provide stable estimates.
Cannabis Use Frequency (Past Month)
We assessed the frequency of cannabis use in the past-month by asking participants the following question: ―How many days have you used cannabis (marijuana) in the past 30 days?” The response options were: 1–2 days, 3–5 days, 6–9 days, 10–19 days, 20–25 days, 26–29 days, all 30 days. For analyses, this variable was collapsed into three groups: (1) use on 1–9 days, (2) use on 10–19 days, and (3) use on 20–30 days. This was done to ensure the groups were comparable with each other (i.e., equal range of days of use) and with the DUIC frequency groups above.
Cannabis Intoxication Ratings (Typical Intoxication and DUIC Intoxication)
We measured two types of self-reported intoxication. The first was typical intoxication level, which served as the “control” intoxication measure. The second was the intoxication level perceived as safe for driving (i.e., “DUIC intoxication”). To assess typical intoxication, respondents were asked: “When you use cannabis, how high do you typically get?” To assess DUIC intoxication, respondents were asked: “Currently, how high could you get and still drive safely?” For both questions, respondents gave their answer using an 11-point (range 0–10) rating scale.10,29–31 On this rating scale, the phrase (i.e., anchor) “Sober/Need to be Sober” was placed next to the response option of 0, the phrase “Light Buzz” was placed next to the response option of 1, and the phrase “So high that you throw up/vomit”32–34 was placed next to the response option of 10. Of note, the phrase “0 = Sober/Need to be Sober” was displayed as an anchor in both scales, but 0 was not a response option in the typical intoxication scale.
Analyses
We used Spearman’s rank-order correlation to examine bivariate relationships among three variables: (1) past-month frequency of cannabis use, (2) intoxication scale ratings, and (3) past-month frequency of DUIC. We then used adjusted logistic and multinomial logistic regression models to examine these same relationships. All models were estimated using cluster-robust standard errors to account for intrastate correlation and were adjusted for age, race, gender, education, employment, years living in one’s current state, lifetime number of days of cannabis use, lifetime number of methods of administration used, and the number of days used cannabis in the past 30 days. Additionally, because we tracked which advertisement was used to collect each survey response, we also adjusted for differences in sampling strategies. Because almost all pvalues were statistically significant, our interpretation of the results is based primarily on the effect sizes (e.g., odds ratios, correlation coefficients) and confidence intervals. All analyses were conducted using Stata 14.35
Results
Demographics and Patterns of Cannabis Use (Table 1)
Table 1.
Demographic and cannabis use characteristics (n=3,010)a
| Demographic characteristics | %b |
| Race | |
| African American | 3 |
| Caucasian | 81 |
| Hispanic | 7 |
| Other | 10 |
| Gender | |
| Male | 56 |
| Female | 43 |
| Other | 1 |
| Education | |
| High school or less | 36 |
| Some college / Associate | 48 |
| Bachelor’s or more | 16 |
| Employment | |
| Full time (35+ hrs/wk) | 41 |
| Part time | 16 |
| Student | 26 |
| Other (retired, disabled, unemployed) | 18 |
| Age | |
| 18–24 | 59 |
| 25–34 | 16 |
| 35–44 | 10 |
| 45+ | 16 |
| Cannabis use characteristics | |
| Number of days used cannabis in life | |
| 1 – 99 days | 7 |
| 100 – 499 days | 23 |
| 500 – 999 days | 22 |
| 1000 or more days | 49 |
| Number of days used cannabis in past 30 days | |
| 1 – 9 days | 17 |
| 10 – 19 days | 11 |
| 20 – 30 days | 72 |
| Lifetime (yes/no) use of different methods of administration | |
| Smoke | 99 |
| Vape Concentrates | 74 |
| Vape Plant Material | 66 |
| Use Edible | 90 |
| Use Dab Rig | 65 |
| Use Other | 6 |
| Lifetime number of methods of administration used | |
| 1 method | 5 |
| 2 methods | 13 |
| 3 methods | 15 |
| 4 methods | 19 |
| 5 methods | 46 |
| 6 methods | 3 |
Limited to past-month cannabis users who reported driving under the influence of cannabis at least once in their life.
Percents may not add exactly to 100 due to rounding. Additionally, lifetime use of different method of administration was not forced to a single response option and thus percents do not add to 100.
Table 1 displays demographic and cannabis use characteristics of the sample. The majority of the sample was male (56%), between the ages of 18–24 (59%), Caucasian (81%) and working at least part-time (57%). Over half reported using cannabis 500 times or more in their life, and 72% reported using at least 20 days in the past month. The correlation between estimates of the percent of the total U.S. population living within each state (U.S. Census 2017), and the percent of survey respondents living in each state indicated that U.S. states were proportionally represented in the study (Spearman’s rho: 0.94; not in table).
Cannabis Use Frequency and Intoxication Ratings
Typical intoxication ratings were positively but weakly related to the frequency of cannabis use (Spearman’s rho: 0.04). In contrast, DUIC intoxication ratings were strongly related to the frequency of cannabis use — higher DUIC intoxication ratings corresponded to more frequent cannabis use (Spearman’s rho: 0.30). Finally, those who provided higher DUIC intoxication ratings also tended to provide higher typical intoxication ratings (Spearman’s rho: 0.30) (not shown in tables).
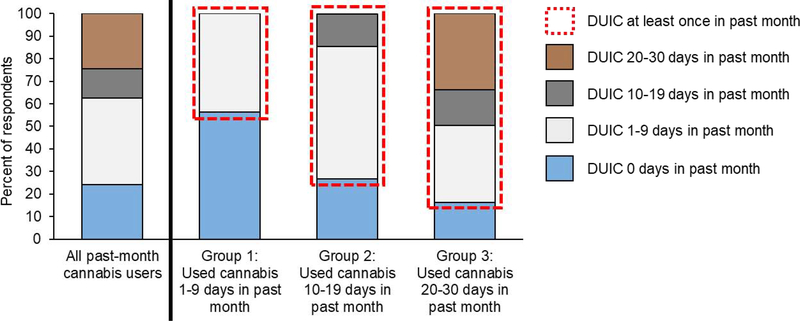
Cannabis Use Frequency and DUIC Frequency (Figure 1)
Figure 1. Number of days drove under the influence of cannabis (DUIC) in the past month across cannabis use frequency groupsa.
aLimited to past-month cannabis users who reported driving under the influence of cannabis at least once in their life.
Figure 1 displays the number of days of DUIC in the past month (i.e., DUIC frequency) among those with different patterns of past-month cannabis use. Note that these data have logically forced zero counts (e.g., those who only used cannabis once in the past month could not have driven under the influence of cannabis on 20 days). Nonetheless, Figure 1 suggests that those who had used cannabis more frequently in the past month were more likely to have driven under the influence at least once in the past month. For example, 56% of those who had used cannabis on 1–9 days reported zero days of DUIC in the past month, compared with only 16% of those who had used cannabis on 20–30 days reporting zero days. An adjusted logistic regression model indicated those who had used cannabis on 10–19 and 20–30 days were 3.1 (95% CI: 2.4, 4.0) and 5.0 (95% CI: 4.0, 6.1) times as likely, respectively, to report DUIC at least once in the past month, as those who had only used cannabis on 1–9 days. This binary comparison is represented by the blue sections and red outline sections in Figure 1.
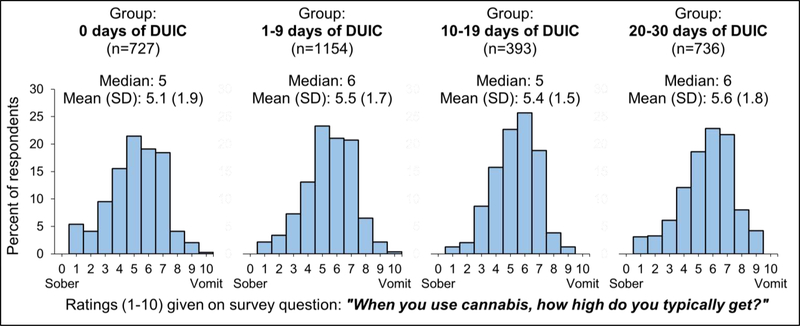
DUIC Frequency and Typical Intoxication Ratings (Figure 2)
Figure 2. Distribution of typical intoxication scale ratings among respondents with different frequencies of DUIC in the past 30 daysa.
aLimited to past-month cannabis users who reported driving under the influence of cannabis at least once in their life.
Figure 2 examines how typical intoxication level varies in relation to the frequency of DUIC. Figure 2 divides the sample into four groups: (1) no DUIC in the past month; (2) 1–9 days of DUIC in the past month; (3) 10–19 days of DUIC in the past month, and (4) 20–30 days of DUIC in the past month. The distributions of typical intoxication ratings were highly similar across the four DUIC groups. For example, the median typical intoxication rating among those with no past-month DUIC was five. Similarly, the median rating among those with 20–30 days of DUIC was six. Although typical intoxication ratings were positively correlated with past-month DUIC frequency, the effect was small (Spearman’s rho: 0.09).
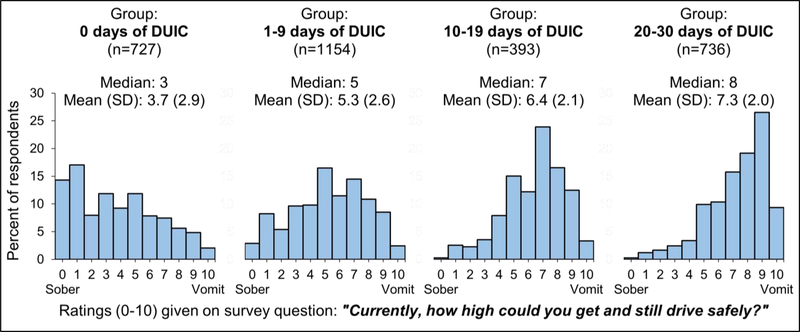
DUIC Frequency and DUIC Intoxication Ratings (Figure 3)
Figure 3. Distribution of DUIC intoxication scale ratings among respondents with different frequencies of DUIC in the past 30 daysa.
aLimited to past-month cannabis users who reported driving under the influence of cannabis at least once in their life.
Figure 3 examines how the intoxication level perceived to be safe for driving varies in relation to the frequency of DUIC. Figure 3 divides the sample into four groups: (1) no DUIC in the past month; (2) 1–9 days of DUIC in the past month; (3) 10–19 days of DUIC in the past month, and (4) 20–30 days of DUIC in the past month. In contrast to the typical intoxication ratings (Figure 2), the distributions of DUIC intoxication ratings varied substantially across DUIC frequency groups (Figure 3). For example, the median intoxication rating perceived as safe for driving among those who did not drive under the influence in the past month was three, whereas the median rating increased to eight among those who drove 20–30 days in the past month. Overall, greater DUIC intoxication ratings perceived as safe for driving corresponded to more frequent DUIC (Spearman’s rho: 0.46).
Using Intoxication Ratings to Predict DUIC Frequency (Table 2 and Figure 4)
Table 2.
Adjusted multinomial logistic regression model using intoxication ratings to predict the number of days an individual drove under the influence of cannabis (DUIC) in the past 30 daysa
| Dependent variable: Number of days drove under the influence of cannabis (DUIC) within the past 30 days | ||||||
|---|---|---|---|---|---|---|
| Comparison 1 | Comparison 2 | Comparison 3 | ||||
| DUIC 1–9 days vs. DUIC 0 days (Ref) | DUIC 10–19 days vs. DUIC 0 days (Ref) | DUIC 20–30 days vs. DUIC 0 days (Ref) | ||||
| MOR | (95% CI) | MOR | (95% CI) | MOR | (95% CI) | |
| Model 1: Typical intoxication rating | 1.05 | (0.97, 1.13) | 1.01 | (0.93, 1.09) | 1.12 | (1.03, 1.23) |
| Model 2: DUIC intoxication rating | 1.18 | (1.13, 1.23) | 1.40 | (1.30, 1.50) | 1.68 | (1.57, 1.80) |
Both models adjusted for number of days used cannabis in past 30 days, lifetime number of days used cannabis, years living in current U.S. state, age, gender, race, education, employment, sampling strategy and number of methods of administration used in ones lifetime. Models estimated using cluster-robust standard errors to account for intrastate correlation. Both models limited to respondents who had used cannabis once or more the past 30 days and had driven under the influence of cannabis at least once in their life.
MOR = multinomial logistic odds ratio.
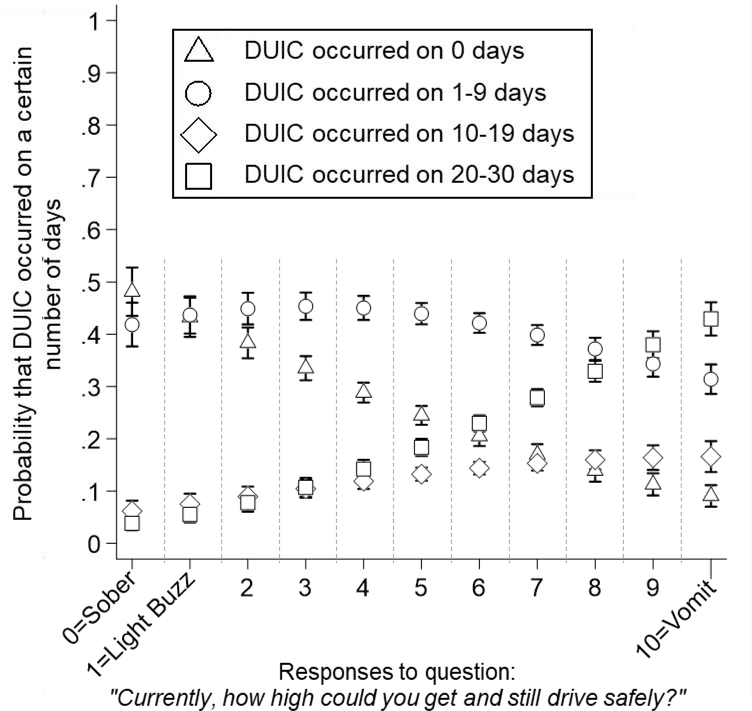
Figure 4. Adjusted probabilities of having driven under the influence of cannabis (DUIC) on a certain number of days among those who gave a particular rating on the driving intoxication scalea.
aModel adjusted for number of days used cannabis in past 30 days, lifetime number of days used cannabis, years living in current U.S. state, age, gender, race, education, employment, sampling strategy and number of methods of administration used in one’s lifetime. Models estimated using cluster-robust standard errors to account for intrastate correlation. Limited to respondents who had used cannabis once or more the past 30 days and had driven under the influence of cannabis at least once in their life.
Table 2 displays two multinomial logistic regression models testing the relationship between intoxication ratings and the frequency of DUIC while adjusting for covariates (including past-month frequency of cannabis use). The results indicate that the likelihood of high-frequency DUIC in the past month increases for each unit increase in the level of intoxication perceived as safe for driving. More specifically, a one unit increase in the level of intoxication perceived as safe for driving is associated with an increase in likelihood of DUIC on 1–9 days, 10–19 days, and 20–30 days in the past month, by approximately 18%, 40%, and 68% respectively. The effect sizes for typical intoxication ratings were much smaller. Sensitivity analyses demonstrated that including past-month cannabis users with no lifetime DUIC in the reference (i.e., 0 days of DUIC) group had little effect on the typical intoxication regression coefficients. However, adding this group increased the predictive strength of DUIC intoxication ratings for each comparison (supplemental material).
Finally, Figure 4 displays adjusted predictions from the multinomial logistic regression model for the DUIC intoxication scale presented in Table 2. Specifically, Figure 4 illustrates that on average, providing a low rating on the DUIC intoxication scale is associated with a lower probability of having engaged in frequent DUIC (i.e., higher probability of no past-month DUIC). For example, among those who responded 0 (“Sober”) on the DUIC intoxication scale (X-axis), there was an approximately 48% chance of 0 days of DUIC, a 42% chance of 1–9 days of DUIC, a 6% chance of 10–19 days of DUIC, and a 4% chance of 20–30 days of DUIC. Conversely, on average, providing a high rating on the DUIC intoxication scale is associated with a higher probability of having engaged in frequent DUIC in the past month.
Discussion
The purpose of this study was to examine the relationship between the level of cannabis intoxication perceived as safe for driving and the frequency of past-month DUIC among current cannabis users. Results suggest that the frequency of past-month DUIC varies substantially among current cannabis users and that the intoxication level perceived as safe for driving, not one’s typical level of intoxication, can be used to predict this frequency. These findings highlight the possibility of stratifying DUIC risk among current cannabis users. Items with this discriminatory ability could prove useful for informing future research and public health efforts concerning epidemiological surveillance, preventive messaging, or screening.
These results are congruent with prior studies. For example, other studies have demonstrated that perceived safety and perceived dangerousness, as well as greater frequency of cannabis use, predict DUIC behaviors and help identify high-risk groups.11,16,36–38 Importantly, however, the utility of self-reported measures of intoxication should be understood with caution and within the context of the broader scientific literature. A recent study by Boggs and colleagues demonstrated that individuals with significantly different blood levels of THC will report equal ratings of subjective intoxication on visual analog scales.39 Additionally, blood THC concentration, not subjective intoxication, predicted motor skill impairment.39 Thus, while the measures of subjective intoxication used in the present study may help us determine who is most likely to drive under the influence of cannabis, they may not reliably inform us about how impaired those individuals are when they do drive. Additionally, when interpreting the intoxication scale results, it is important to consider potential item ordering effects. During the survey, respondents reported their typical level of intoxication immediately before reporting DUIC intoxication. Juxtaposing these two items and ordering the typical intoxication item before the DUIC intoxication item may have altered response patterns via anchoring-like effects.
In theory, lower ratings on the DUIC intoxication scale should correspond to a lower probability of having driven under the influence in the past month. Conversely, higher ratings should correspond to a higher probability of having driven under the influence on a greater number of days. Our results reflected this pattern to a large extent. However, an interesting caveat warrants mention. As expected, among participants who reported needing to be sober to drive safely (i.e., rating of 0 on DUIC intoxication scale), the order of the most likely to least likely behaviors was zero days of DUIC in the past month, followed by 1–9, 10–19, and 20–30 days. One would expect this ordered relationship to be exactly reversed among those who reported the highest rating (10) on the scale (i.e., DUIC on 20–30 days as the most likely, followed by 10–19, 1–9, and 0 days). We observed that at a DUIC intoxication rating of 10, DUIC on 20–30 days was indeed the most likely, and 0 days of DUIC was the least likely, but DUIC on 1–9 days remained more likely than DUIC on 10–19 days. We offer several possible interpretations for this result. From a survey methods standpoint, response options within the range of 10–19 days may be too cognitively demanding on recall and memory. Alternatively, there may be one or several confounding variables that, if controlled, would have altered the model. Finally, the targeted sampling method used in this study may have over-sampled specific types of cannabis consumers with specific types of driving behaviors.
There are two crucial “ceiling”-related limitations to consider when interpreting the results. First, frequent cannabis use is a prerequisite for frequent DUIC; it is impossible to use cannabis on two days in the past month, but drive under the influence of cannabis on twenty days. This logic induces a correlation between the two variables. Thus, we collapsed DUIC frequency into a binary variable (DUIC at least once vs. no DUIC) and compared the odds of DUIC across the three cannabis-use-frequency groups (1–9 days vs. 10–19 days vs. 20–30 days). A reasonable argument could still be made that even this comparison is flawed because the probability of engaging in DUIC at least once is still greater for those who had more opportunities (i.e., more use days) to engage in DUIC. Regardless, we believe our results help rule out the possibility that individuals with lower frequencies of use (e.g., used 1–9 days) have an abnormally high percent of DUIC on the days that they use. We were unable to examine this possibility in more detail because our data were categorical.
Second, overall or typical driving frequency creates an upper limit on DUIC frequency. A strong limitation of this study is that we did not assess non-intoxicated driving frequency. Had we done so, it would have been possible to make further distinctions among subgroups of participants by calculating the ratio of intoxicated to non-intoxicated driving frequencies. For example, one individual may typically drive only five total days per month and is intoxicated while driving on all five of these days. Conversely, a different person may drive on thirty days per month but only drive under the influence on five of those thirty days. Both of these individuals would be classified as having driven under the influence on five days in the past month, but they likely represent two distinct risk profiles. A similar issue may affect the composition of the DUIC frequency reference (i.e., 0 days of DUIC) group. Because we did not assess whether participants had access to a car or owned a driver’s license, we do not know if some respondents were inadvertently classified as having 0 days of DUIC simply because they did not have a car or license. This group is likely distinct in multiple ways from current cannabis users who had the opportunity to drive under the influence (i.e., owned a car and had a driver’s license), but chose not to.
Several additional limitations warrant discussion. First, this study did not assess the quantity (e.g., grams) or potency (e.g., %THC) of the cannabis products used by respondents. These aspects of cannabis use patterns may be related to DUIC risk perception.40 Furthermore, they may also affect patterns of responding on both the typical intoxication and DUIC intoxication scales if they function either as causes or proxy indicators of different levels of tolerance to the effects of THC. Additionally, a study by Allen and colleagues demonstrated that being under the influence of cannabis while taking a survey about intoxicated driving predicts agreement with the statement “I can safely drive under the influence of marijuana”.41 Participants in the present study may have been intoxicated at the time of the survey which could have affected the results. However, the lack of empirical literature on this topic makes it difficult to fully articulate the potential effects that this may have had on the results. Given that those who use cannabis more frequently are also more likely to believe they can drive safely under the influence, the correlation between current intoxication and perceptions of DUIC safety could be a manifestation of underlying pathology (i.e., cannabis use disorder). Future survey studies of cannabis use behaviors should consider examining this issue further. Finally, these data were not collected with probability-based methods. Although all U.S. states are proportionally represented, the generalizability of our data is limited due to our use of a targeted sampling strategy which resulted in oversampling of Caucasians and young adults.
The perceptions, use, and legal status of cannabis continue to evolve in the U.S., spurring the need for evidence-based interventions. To this end, constructs such as perceived risk could serve as useful components of such interventions. However, risk perception is complex and comprised of multiple subcomponents (e.g., perceived probability of consequences) that may all have implications for understanding DUIC behaviors.11,18,36,42 Additionally, risk perception is just one of several components that will likely need to be incorporated into new intervention strategies; being young and male, starting cannabis use at an early age, peer cannabis use, and perceived peer norms concerning intoxicated driving also predict DUIC behaviors.37,38,43–46 Overall, effectively addressing cannabis-related public safety issues such DUIC will require multilevel and multicomponent interventions (e.g., state and municipal level policy-based, social norms, massmedia campaigns, cannabis-related beliefs, and education).47
In sum, the present study demonstrates the variability of DUIC patterns among current cannabis users and the potential utility of measuring intoxication levels perceived as safe for driving to understand these patterns. In the age of legal cannabis, epidemiological investigations that consider non-traditional nuances of cannabis perceptions and behaviors can provide meaningful insights relevant to public health.
Supplementary Material
Highlights.
Online survey of driving under the influence of cannabis (DUIC)
Sample of 3,010 past-month cannabis users endorsing lifetime DUIC
DUIC in past month: 0 days: 24%, 1–9 days: 38%, 10–19 days: 13%, 20–30 days: 25%
Intoxication level (0–10) perceived as safe for driving predicts DUIC frequency
Acknowledgements
We would like to thank Brian Goodness for his contributions to this project.
Financial support for this study and preparation of the manuscript was provided by the National Institute on Drug Abuse (NIDA): T32-DA037202, P30-DA029926, R01-DA040411 and the National Institute on Alcohol Abuse and Alcoholism (NIAAA): F32-AA027941. The funding sources were not involved in the study design; collection, analysis, and interpretation of data; writing of the report; or in the decision to submit the article for publication.
Footnotes
Conflict of Interest Statement: The authors have no conflicts of interest to declare
The data presented in this manuscript were collected as part of the first author’s dissertation research while he completed his Ph.D. at The Dartmouth Institute for Health Policy and Clinical Practice and the Center for Technology and Behavioral Health within the Dartmouth Geisel School of Medicine. The analysis and writing for this manuscript were conducted at Dartmouth as well as at the Washington University School of Medicine, in St. Louis (first author’s current affiliation).
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Compton WM, Han B, Jones CM, Blanco C, Hughes A. Marijuana use and use disorders in adults in the USA, 2002–14: analysis of annual cross-sectional surveys. The Lancet Psychiatry. 2016;3(10):954–964. [DOI] [PubMed] [Google Scholar]
- 2.Hasin DS, Saha TD, Kerridge BT, et al. Prevalence of Marijuana Use Disorders in the United States Between 2001–2002 and 2012–2013. JAMA Psychiatry. 2015;72(12):1235–1242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fink DS, Stohl M, Sarvet AL, et al. Medical Marijuana Laws and Driving Under the Influence of Marijuana and Alcohol. Under Review. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rogeberg O, Elvik R. The effects of cannabis intoxication on motor vehicle collision revisited and revised. Addiction. 2016;111(8):1348–1359. [DOI] [PubMed] [Google Scholar]
- 5.Asbridge M, Hayden JA, Cartwright JL. Acute cannabis consumption and motor vehicle collision risk: systematic review of observational studies and meta-analysis. BMJ. 2012;344:e536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li MC, Brady JE, DiMaggio CJ, Lusardi AR, Tzong KY, Li GH. Marijuana Use and Motor Vehicle Crashes. Epidemiologic Reviews. 2012;34(1):65–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hall W What has research over the past two decades revealed about the adverse health effects of recreational cannabis use? Addiction. 2015;110(1):19–35. [DOI] [PubMed] [Google Scholar]
- 8.Ramaekers JG, Berghaus G, van Laar M, Drummer OH. Dose related risk of motor vehicle crashes after cannabis use. Drug Alcohol Depend. 2004;73(2):109–119. [DOI] [PubMed] [Google Scholar]
- 9.Ronen A, Gershon P, Drobiner H, et al. Effects of THC on driving performance, physiological state and subjective feelings relative to alcohol. Accid Anal Prev. 2008;40(3):926–934. [DOI] [PubMed] [Google Scholar]
- 10.Aston ER, Merrill JE, McCarthy DM, Metrik J. Risk Factors for Driving After and During Marijuana Use. J Stud Alcohol Drugs. 2016;77(2):309–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Arterberry BJ, Treloar H, McCarthy DM. Empirical Profiles of Alcohol and Marijuana Use, Drugged Driving, and Risk Perceptions. J Stud Alcohol Drugs. 2017;78(6):889–898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davis KC, Allen J, Duke J, et al. Correlates of Marijuana Drugged Driving and Openness to Driving While High: Evidence from Colorado and Washington. PLoS One. 2016;11(1):e0146853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hartman RL, Brown TL, Milavetz G, et al. Cannabis effects on driving longitudinal control with and without alcohol. J Appl Toxicol. 2016;36(11):1418–1429. [DOI] [PubMed] [Google Scholar]
- 14.Hartman RL, Huestis MA. Cannabis effects on driving skills. Clinical chemistry. 2013;59(3):478–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Greene KM. Perceptions of driving after marijuana use compared to alcohol use among rural American young adults. Drug Alcohol Rev. 2018;37(5):637–644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fischer B, Rodopoulos J, Rehm J, Ivsins A. Toking and driving: Characteristics of Canadian university students who drive after cannabis use—an exploratory pilot study. Drugs: Education, Prevention and Policy. 2009;13(2):179–187. [Google Scholar]
- 17.Swift W, Jones C, Donnelly N. Cannabis use while driving: A descriptive study of Australian cannabis users. Drug-Educ Prev Polic. 2010;17(5):573–586. [Google Scholar]
- 18.McCarthy DM, Lynch AM, Pederson SL. Driving after use of alcohol and marijuana in college students. Psychol Addict Behav. 2007;21(3):425–430. [DOI] [PubMed] [Google Scholar]
- 19.Kypri K, Stephenson S. Drink-driving and perceptions of legally permissible alcohol use. Traffic Inj Prev. 2005;6(3):219–224. [DOI] [PubMed] [Google Scholar]
- 20.Greenfield TK, Rogers JD. Alcoholic beverage choice, risk perception and self-reported drunk driving: effects of measurement on risk analysis. Addiction. 1999;94(11):1735–1743. [DOI] [PubMed] [Google Scholar]
- 21.Jaccard J, Turrisi R. Cognitive processes and individual differences in judgments relevant to drunk driving. Journal of personality and social psychology. 1987;53(1):133–145. [PubMed] [Google Scholar]
- 22.Turrisi R, Wiersma K. Examination of judgments of drunkenness, binge drinking, and drunk-driving tendencies in teens with and without a family history of alcohol abuse. Alcoholism-Clinical and Experimental Research. 1999;23(7):1191–1198. [PubMed] [Google Scholar]
- 23.Solowij N, Lorenzetti V, Yucel M. Effects of Cannabis Use on Human Behavior: A Call for Standardization of Cannabis Use Metrics. JAMA Psychiatry. 2016;73(9):995–996. [DOI] [PubMed] [Google Scholar]
- 24.Borodovsky JT, Marsch LA, Budney AJ. Studying Cannabis Use Behaviors With Facebook and Web Surveys: Methods and Insights. JMIR Public Health Surveill. 2018;4(2):e48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Qualtrics Survey Software [computer program]. Provo, Utah, USA: 2019. [Google Scholar]
- 26.Borodovsky JT, Lee DC, Crosier BS, Gabrielli JL, Sargent JD, Budney AJ. U.S. cannabis legalization and use of vaping and edible products among youth. Drug Alcohol Depend. 2017;177:299–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Borodovsky JT, Budney AJ. Legal cannabis laws, home cultivation, and use of edible cannabis products: A growing relationship? Int J Drug Policy. 2017;50:102–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ramo DE, Prochaska JJ. Broad Reach and Targeted Recruitment Using Facebook for an Online Survey of Young Adult Substance Use. Journal of Medical Internet Research. 2012;14(1):e28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hughes JR, Fingar JR, Budney AJ, Naud S, Helzer JE, Callas PW. Marijuana use and intoxication among daily users: an intensive longitudinal study. Addict Behav. 2014;39(10):1464–1470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.van der Pol P, Liebregts N, Brunt T, et al. Cross-sectional and prospective relation of cannabis potency, dosing and smoking behaviour with cannabis dependence: an ecological study. Addiction. 2014;109(7):1101–1109. [DOI] [PubMed] [Google Scholar]
- 31.Leung SO. A Comparison of Psychometric Properties and Normality in 4-, 5-, 6-, and 11-Point Likert Scales. J Soc Serv Res. 2011;37(4):412–421. [Google Scholar]
- 32.Whiting PF, Wolff RF, Deshpande S, et al. Cannabinoids for Medical Use: A Systematic Review and Metaanalysis. JAMA. 2015;313(24):2456–2473. [DOI] [PubMed] [Google Scholar]
- 33.Vandrey R, Herrmann ES, Mitchell JM, et al. Pharmacokinetic Profile of Oral Cannabis in Humans: Blood and Oral Fluid Disposition and Relation to Pharmacodynamic Outcomes. J Anal Toxicol. 2017;41(2):83–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Spindle TR, Cone EJ, Schlienz NJ, et al. Acute Effects of Smoked and Vaporized Cannabis in Healthy Adults Who Infrequently Use Cannabis: A Crossover Trial. JAMA Netw Open. 2018;1(7):e184841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.StataCorp. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP; 2015. [Google Scholar]
- 36.Arterberry BJ, Treloar HR, Smith AE, Martens MP, Pedersen SL, McCarthy DM. Marijuana use, driving, and related cognitions. Psychol Addict Behav. 2013;27(3):854–860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Berg CJ, Daniel CN, Vu M, Li J, Martin K, Le L. Marijuana Use and Driving Under the Influence among Young Adults: A Socioecological Perspective on Risk Factors. Subst Use Misuse. 2018;53(3):370–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cuttler C, Sexton M, Mischley L. Driving Under the Influence of Cannabis: An Examination of Driving Beliefs and Practices of Medical and Recreational Cannabis Users across the United States. Cannabis. 2018;1(2):1–13. [Google Scholar]
- 39.Boggs DL, Cortes-Briones JA, Surti T, et al. The dose-dependent psychomotor effects of intravenous delta-9-tetrahydrocannabinol (Delta(9)-THC) in humans. J Psychopharmacol. 2018;32(12):1308–1318. [DOI] [PubMed] [Google Scholar]
- 40.Cavazos-Rehg PA, Krauss MJ, Sowles SJ, Zewdie K, Bierut L. Operating a motor vehicle after marijuana use: Perspectives from people who use high-potency marijuana. Subst Abus. 2018;39(1):21–26. [DOI] [PubMed] [Google Scholar]
- 41.Allen JA, Davis KC, Duke JC, et al. Association between self-reports of being high and perceptions about the safety of drugged and drunk driving. Health Educ Res. 2016;31(4):535–541. [DOI] [PubMed] [Google Scholar]
- 42.Jones C, Donnelly N, Swift W, Weatherburn D. Preventing cannabis users from driving under the influence of cannabis. Accid Anal Prev. 2006;38(5):854–861. [DOI] [PubMed] [Google Scholar]
- 43.Whitehill JM, Rodriguez-Monguio R, Doucette M, Flom E. Driving and riding under the influence of recent marijuana use: Risk factors among a racially diverse sample of young adults. J Ethn Subst Abuse. 2018:1–19. [DOI] [PubMed] [Google Scholar]
- 44.Kohn C, Saleheen H, Borrup K, Rogers S, Lapidus G. Correlates of drug use and driving among undergraduate college students. Traffic Inj Prev. 2014;15(2):119–124. [DOI] [PubMed] [Google Scholar]
- 45.Whitehill JM, Rivara FP, Moreno MA. Marijuana-using drivers, alcohol-using drivers, and their passengers: prevalence and risk factors among underage college students. JAMA Pediatr. 2014;168(7):618–624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Le Strat Y, Dubertret C, Le Foll B. Impact of age at onset of cannabis use on cannabis dependence and driving under the influence in the United States. Accid Anal Prev. 2015;76:1–5. [DOI] [PubMed] [Google Scholar]
- 47.Berg CJ. A Socioecological Perspective Regarding Risk Factors for Driving Under the Influence of Marijuana Among Young Adults. Subst Abuse. 2018;12:1178221818805084. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.