Abstract
The Ironman is one of the most popular triathlon events in the world. Such a race involves a great number of tactical decisions for a healthy finish and best performance. Dehydration is widely postulated to decrease performance and is known as a cause of dropouts in Ironman. Despite the importance of hydration status after an Ironman triathlon, there is a clear lack of review and especially meta-analysis studies on this topic. Therefore, the objective was to systematically review the literature and carry out a meta-analysis investigating the hydration status after an Ironman triathlon. We conducted a systematic review of the literature up to June 2016 that included the following databases: PubMed, SCOPUS, Science Direct and Web of Science. From the initial 995 references, we included 6 studies in the qualitative analysis and in the meta-analysis. All trials had two measures of hydration status after a full Ironman race. Total body water, blood and urine osmolality, urine specific gravity and sodium plasma concentration were considered as hydration markers. Three investigators independently abstracted data on the study design, sample size, participants’ and race characteristics, outcomes, and quantitative data for the meta-analysis. In the pooled analysis, it seems that the Ironman event led to a moderate state of dehydration in comparison to baseline values (SMD 0.494; 95% CI 0.220 to 0.767; p = 0.001). Some evidence of heterogeneity and consistency was also observed: Q = 19.6; I2 = 28.5%; τ2 = 2.39. The results suggest that after the race athletes seem to be hypo-hydrated in comparison to baseline values.
Key words: endurance, dehydration, swimming, cycling, running
Introduction
The Ironman is a multi-stage endurance event covering 3.8 km swimming, 180 km cycling and 42.195 km running (Knechtle et al., 2016). Every year, more than 50,000 participants in more than 20 countries try to qualify for the World Championship in Kona, Hawaii (Stiefel et al., 2013), one of the toughest endurance races in the world (Bentley et al., 2002; Lepers, 2008). In addition, most participants are unprofessional triathletes aged between 35 and 45 years old and even though amateurs, they must have a very controlled dietary and training routine to decrease health risks and achieve the best personal performance in each event (Bentley et al., 2002; Buell et al., 2013).
During an Ironman race, energy expenditure ranges from 8,500 to 11,000 kcal (Kreider, 1991), with a body mass loss from 4 to 8% (Speedy et al., 2001) and total body water (TBW) turnover may be around 16 L or 1.33 L.hour-1 (Cuddy et al., 2010). Medical volunteers attending Kona’s (World Championship) physicians’ tents reported that dehydration and hyperthermia were the main concerns in Ironman® finishers, greater than other risks such as corneal abrasions, simple exhaustion, burns caused by jellyfish with rare anaphylaxis or bike accidents (Laird and Johnson, 2012).
With regard to performance, although muscle glycogen and blood glucose were the most important substrates for contracting muscles (Coyle, 1995; Holloszy and Kohrt, 1996; Ivy, 1999), Noakes (2000) pointed that it was unlikely that only muscle glycogen depletion limited prolonged exercise. Thus, it has been suggested that dehydration could also impair performance (Coyle, 2004). In the need to dissipate the heat generated during exercise, sweat losses occur (Sawka, 1992). This body water reduction may result in an increased heart rate, a reduction in plasma volume (PV), stroke volume and a skin blood flow, leading to an inability to maintain thermal homeostasis (Sawka, 1992; Sawka and Montain, 2000; Sawka and Pandolf, 1990). Furthermore, water loss by sweating is accompanied by the loss of important minerals, such as potassium, which has been postulated as one of the possible causes of fatigue (Fitts, 1994). Severe dehydration could also reduce the rate of gastric emptying while increasing the likelihood of gastrointestinal problems (Rehrer et al., 1990).
All these factors, alone or together, seem to be responsible for the impairment of performance in prolonged exercise. Walsh et al. (1994) reported that reductions in body mass of 12% resulted in a 44% reduction in performance, while 3% dehydration caused by diuretics induced a 3-5% reduction in 1,500-10,000m running times (Armstrong et al., 1985). Additionally, in a triathlon, the inability to consume fluids during the swim portion and inappropriate water intake during cycling had a great influence on the subsequent running performance (Kreider et al., 1988), being the stage (running) of the Ironman® with most dropouts compared to swimming and cycling (Laird and Johnson, 2012). These potential harms are possibly increased by elevated temperature and relative humidity (Latzka and Montain, 1999; Sawka and Montain, 2000).
Although there exist medical (Dallam et al., 2005) and nutritional (Jeukendrup et al., 2005) recommendations highlighting the importance of hydration during prolonged exercise such as an Ironman triathlon, this issue remains of critical importance, especially considering different dietary and hydration strategies applied during the race that might be very individual. The same way hypohydration may lead to the aforementioned physiological limitations, overhydration leads to electrolyte imbalance that may result in hyponatremia (low plasma sodium) (Hiller et al., 1987; Speedy et al., 2000a, 2000b), which affects negatively performance and besides, could also result in mental confusion, weakness, fainting and death (Hew-Butler et al., 2015; Jeukendrup et al., 2005).
Despite the importance of hydration status after an Ironman triathlon, there is a clear lack of review and especially meta-analysis studies on this topic. Such studies would have great practical implications for athletes and coaches as they would provide information on optimal hydration strategies. Therefore, the purpose of this article was to critically review the literature on hydration status after an Ironman triathlon. A quantitative analysis was also performed to achieve objective results. To the best of our knowledge, this is the first review with a meta-analysis on this topic. Our hypothesis was that athletes participating in an Ironman triathlon would finish the race with high levels of dehydration.
Methods
A systematic review of the literature was conducted up to June 2016, including the following databases: PubMed, Web of Science, Science Direct and SCOPUS. Our search included papers published from 2006 as it is the year of the first report (Laursen et al., 2006) related to hydration status after an Ironman race or distance matched to an endurance triathlon (Figure 1).
Figure 1.
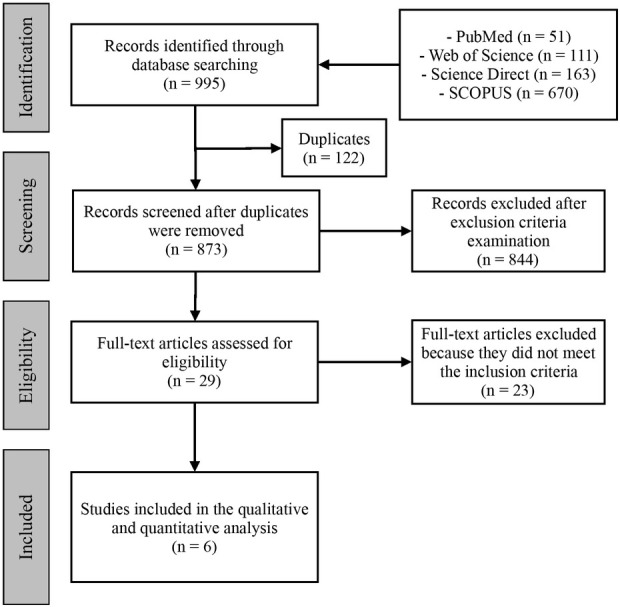
PRISM flow diagram for the search strategy.
We included studies fulfilling the following criteria: (a) full report of an original investigation published in a peer-reviewed journal; (b) publications in English, Spanish or Portuguese; (c) hydration status assessed before and at least one hour after the race (Ironman distance); triathlon distance matching to Ironman distance (3.8 km swim; 180 km cycling; 42 km run). Articles were excluded if: (a) a full-text article was unavailable; (b) the study used drug administration or nutritional supplementation before and/or during the race.
All relevant data from each included study were extracted: characteristics of the sample (n, sex and age); characteristics of the race (weather, hydration and feeding, and finish time); body composition and hydration outcomes. Hydration variables were extracted as mean and standard deviation (SD) values at baseline and post-race for the quantitative analysis. The characteristics of included studies are summarized in Table 1 and are presented by order of publication.
Table 1.
Hydration/dehydration outcomes studied in full Ironman races.
| Study | Sample [n; age (mean ± SD; sex] | Race characteristics | Body composition | Hydration/dehydration outcome | ||||
|---|---|---|---|---|---|---|---|---|
| Temperature [mean (range)] | Hydration / Feeding | Mean race time | Body mass (Δ%) | Free fat mass (Δ%) | Variable | Relative variation (Δ%) | ||
| Laursen et al. (2006) | 10; 34.7 ± 4.8; male | 20.5°C (19 – 26°C) | NR | 10h11min | -2.93% | NR | USG (g/ml) | 0.59 % * |
| Hew-Butler et al. (2007) | 181; 34.2 ± 8.2; male | 20.5°C (17–23.9°C) | ad libitum | 12h39min | -4.87% | NR | Plasma Na (mmol/l) | 0.64 % |
| Knechtle et al. (2010) | 16; 36.6 ± 7.0; female | NR (17–23°C) | NR | 12h11min | -1.00% | -1.8% | USG (g/ml) Plasma Na (mmol/l) | 1.29 % * -1.66 % * |
| Knechtle et al. (2010) | 27; 39.3 ± 9.2; male | NR (17–25°C) | NR | 11h36min | -2.3% | -2.3% | USG (g/ml) Plasma Na (mmol/l) | 1.19 % * - 0.43 % |
| Total Body Water (l) | - 1.18 % | |||||||
| Meyer et al. (2012) | 15; 40.1 ± 6.8; male | NR (14–23.2°C) | ad libitum | 11h09min | -3.2% | -2.9% | USG (g/ml) Plasma [Na+] (mmol/l) | 1.28 % * 0.79 % |
| Urine osmolality (mosmol/kgH2O) | 57.3 % * | |||||||
| Serum osmolality (mosmol/kgH2O) | 2.70 % * | |||||||
| Mueller et al. (2013) | 8; 43.5 ± 5.5; male | NR (14–23.2°C) | ad libitum | 11h27min | -2.5% | -2.35% | USG (g/ml) Plasma [Na+] (mmol/l) | 1.48 % * 1.15 % * |
| Urine osmolality (mosmol/kgH2O) | 68.3 % * | |||||||
| Plasma osmolality (mosmol/kgH2O) | 3.2 % * | |||||||
Hydration/dehydration outcomes studied in full Ironman races. NR: non-reported; USG: urine specific gravity (g/ml); Na: plasmatic sodium (mmol/l); TBW: total body water (l); UO: urine osmolality (mosmol/kgH2O); PO: plasma osmolality (mosmol/kgH2O); PO: plasma osmolality (mosmol/kgH2O); *: statistical difference from baseline to post-race values (p < 0.05)
We performed the meta-analysis by computing the standardized mean difference (SMD; Hedges’ g) using the random-effects model, and carried out quantitative analyses on the confined data derived from the baseline measure (before race) and post-race values of each study. If any hydration variable had a negative effect pointing to dehydration, it was inversely plotted for the pooled analysis to calculate the SMD. As previously suggested (Borenstein et al., 2009), we combined the outcomes for trials with more than one hydration variable. We assessed heterogeneity with the Cochran’s Q test and tau-squared (τ2) and measured inconsistency (the percentage of total variation across studies due to heterogeneity) of effects across exercise interventions using the I2 statistic proposed by Higgins et al. (2003). The risk of publication bias was objectively assessed with the Egger et al.’s test (1997). The level of significance was set at p = 0.05 for all analyses, except for Egger’s regression to assess funnel plot asymmetry, which was set at p = 0.1, as previously suggested (Egger et al., 1997). We used the software Comprehensive Meta-Analysis (CMA 3.0, Englewood, USA) and GraphPad Prism (v.6.0, California, USA) to carry out all procedures.
Results
The search of PubMed, Web of Science, Science Direct and SCOPUS provided a total of 995 citations. After adjusting for duplicates, 873 articles were included for further analysis, yet, 844 were discarded for not meeting inclusion criteria after the abstract review. We examined the full text of the remaining 29 articles in more detail; 23 appeared not to meet the inclusion criteria as described and were also discarded. Finally, six studies met all the criteria and were therefore included in the systematic review and quantitative analysis (Figure 1).
All studies selected for this review were observational cross-sectional trials published in English. They referred to different official full Ironman races (3.8 km swim; 180 km cycling; 42.195 km run) and measured at least one hydration variable before and after the event (1-h maximum). A more thorough description of each race, sampling and outcomes is available in Table 1. The studies used five different hydration variables: plasma osmolality (PO), urine osmolality (UO), plasma sodium (Na), urine specific gravity (USG) and total body water (TBW).
Summary and individual effects of each study are presented in the forest plot (Figure 2). In the pooled analysis, it was found that the Ironman race led to a moderate state of dehydration in comparison to baseline values (SMD 0.494; 95 % CI 0.220 to 0.767; p = 0.001). Some evidence of heterogeneity and consistency was also observed: Q = 19.6; I2 = 28.5%; τ2 = 2.39 (Higgins et al., 2003).
Figure 2.
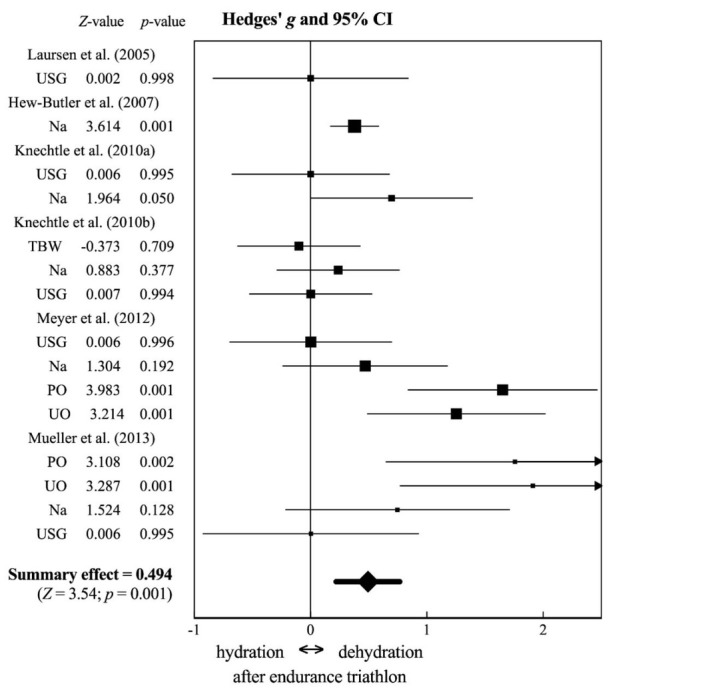
Forest plot: standardized mean difference (Hedges’ g) and 95% confidence interval of each analysis from each study and summary effect. The square size of each study expresses its respective weight. CI: confidence interval; USG: urine specific gravity; Na: sodium plasma concentration; TBW: total body water; PO: plasma osmolality; UO: urine osmolality.
Discussion
The present study aimed to systematically review the literature and carry out a meta-analysis investigating the hydration status after an Ironman triathlon. Current evidence was almost unanimous pointing to a hypo-hydration state after this endurance triathlon; such an outcome was also confirmed in the meta-analysis performed with available data.
The main causes of dehydration during endurance exercise were sweat losses and fluid restriction/unavailability (Cheuvront and Kenefick, 2014). For that matter, it has been suggested that body mass losses greater than 2% represent intracellular or osmotic dehydration (ICD) (Cheuvront and Kenefick, 2014; Costill et al., 1976; Darrow and Yannet, 1935). Although ICD depends on a number of factors, it may indicate an approximately 1.4 L of TBW loss, decreasing PV and increasing PO, activating osmoreceptors and secondary baroreceptors for a neuro-endocrine reflex for water balance, including compensatory renal water conservation and water acquisition (thirst) (Dunn et al., 1973; Robertson and Athar, 1976; Sawka et al., 2015). Furthermore, hyper osmolality is a possible consequence of dehydration that can help to mediate body core temperature (Sawka, 1992) and cardiovascular strain (Montain and Coyle, 1992; Wingo et al., 2012). These factors, together with increased thirst sensation (Rolls et al., 1980) may elevate effort perception and produce subjective feelings of fatigue that might limit performance in endurance exercise (Noakes, 2007), such as an Ironman triathlon.
On the other hand, some evidence reported a positive relationship between dehydration and endurance performance (Dugas et al., 2009; Kay and Marino, 2003; Knechtle et al., 2012; Zouhal et al., 2011); however, the physiological mechanisms that may occur were not yet elucidated (Goulet, 2012). TBW loss may be a fine line between performance improvement and a metabolic overcharge, increasing the risk of the dropout in endurance races. It seems that some weight loss during endurance exercise is needed to maintain euhydration. However, reaching consensus about whether dehydration improves or decreases performance, and in which conditions, is far beyond the scope of this study. This issue has been previously reviewed by Goulet (Goulet, 2011; Goulet, 2012).
Considering the present results, although there was a positive and significant effect indicating a dehydrated status after the Ironman triathlon, it should be noted that from a clinical perspective none of the studies reported mean values below or over normal variables (Chernecky and Berger, 2007; Rose, 1987; Williamson and Snyder, 2014). The explanation is possibly a combination of pre-race overhydration and adequate fluid intake during the race. Food and fluid intake during the race was ad libitum, since the race organizers or athletes themselves provided it, allowing a satisfactory nutrition replacement. Kimber et al. (2002) described the dietary consumption of 18 triathletes (10 males) during an Ironman triathlon and reported a fluid intake of 127 ml⋅kg-1 for women and 123 ml⋅kg-1 for men.
Furthermore, studies included in the present analysis were performed in day temperature ranging from 17 to 26 °C, which represents a pleasant weather to race for most athletes. This could possibly influence hydration status. Several studies have demonstrated the exercise-heat stress effect on endurance performance (Kenefick et al., 2010; Rowell, 1983; Sawka et al., 1992, 2011). Kenefick et al. (2010) reported a performance decrease of approximately 6% for each 4°C temperature increase during a time trial cycling effort. Heat stress when combined with physical effort may push the cardiovascular system close to its limits while competing simultaneously to thermoregulatory and metabolic demands for the skin blood flow and contracting skeletal muscles, respectively (Rowell, 1983), favoring the installation of fatigue. Thus, during exercise-heat stress, sweat output may exceed fluid intake and lead to dehydration, which often increases heat storage and reduces the ability to tolerate exercise-heat strain (Sawka et al., 1992, 2011). Furthermore, it is worth mentioning that hypohydration represents a continuum from both athletic and clinical perspective, whereas clinical dehydration considering body mass deficit is referred to as mild (1-5%), moderate (2-5%) and severe (>10%), and from an athletic perspective is mild to moderate (2-5%) and severe (>5%) (McDermott et al., 2017).
Although there is a general body of evidence regarding hydration status after endurance exercise in the heat, it seems to be a gap in the literature regarding Ironman triathlons, which could represent interesting data, in the way that almost 30% of Ironman races are performed in tropical locations, including the World Championship in Kona, Hawaii, with weather temperate reaching 38°C (Bentley et al., 2002; Lepers, 2008).
Moreover, all studies only included Ironman finishers, and possible cases of unfinished races due to dehydration might have been excluded. The evaluation of clinical variables of dropouts may provide fundamental information for coaches and athletes. It is also noteworthy that there is some variability in data affecting body hydration, such as: fluid overloading (as a consequence of excessive drinking) and serious dehydration in Ironman triathlons. Furthermore, the present study has some limitations, such as the small number of studies included in the analysis, the small sample size used in some of these studies and the heterogeneity of variables used to determine hydration status.
In conclusion, analysis of the current body of evidence regarding hydration status after Ironman events demonstrated that after the race athletes seemed to be hypo-hydrated in comparison to baseline values, but not sufficiently to be diagnosed as clinically dehydrated. On the other hand, given the importance of hydration to performance, the results suggest that athletes' performance could have been better if they were properly hydrated. Thus, it is also suggested that athletes, coaches, nutritionists and physiologists should be concerned to better evaluate this condition, favoring the achievement of better performance.
References
- Armstrong LE, Costill DL, Fink WJ. Influence of diuretic-induced dehydration on competitive running performance. Med Sci Sports Exerc. 1985;17:456–461. doi: 10.1249/00005768-198508000-00009. [DOI] [PubMed] [Google Scholar]
- Bentley DJ, Millet GP, Vleck VE, McNaughton LR. Specific aspects of contemporary triathlon. Sports Med. 2002;32:345–359. doi: 10.2165/00007256-200232060-00001. [DOI] [PubMed] [Google Scholar]
- Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to Meta-analysis. Wiley; 2009. [Google Scholar]
- Buell JL, Franks R, Ransone J, Powers ME, Laquale KM, Carlson-Phillips A. National Athletic Trainers A. National Athletic Trainers' Association position statement: evaluation of dietary supplements for performance nutrition. J Athl Train. 2013;48:124–136. doi: 10.4085/1062-6050-48.1.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chernecky CC, Berger BJ. Laboratory tests and diagnostic procedures. Elsevier Health Sciences; 2007. [Google Scholar]
- Cheuvront SN, Kenefick RW. Dehydration: physiology, assessment, and performance effects. Compr Physiol. 2014. [DOI] [PubMed]
- Costill D, Cote R, Fink W. Muscle water and electrolytes following varied levels of dehydration in man. J Appl Physiol. 1976;40:6–11. doi: 10.1152/jappl.1976.40.1.6. [DOI] [PubMed] [Google Scholar]
- Coyle EF. Substrate utilization during exercise in active people. Am J Clin Nutr. 1995;61:968S–979S. doi: 10.1093/ajcn/61.4.968S. [DOI] [PubMed] [Google Scholar]
- Coyle EF. Fluid and fuel intake during exercise. J Sports Sci. 2004;22:39–55. doi: 10.1080/0264041031000140545. [DOI] [PubMed] [Google Scholar]
- Cuddy JS, Slivka DR, Hailes WS, Dumke CL, Ruby BC. Metabolic profile of the Ironman World Championships: a case study. Int J Sports Physiol Perform. 2010;5:570–576. doi: 10.1123/ijspp.5.4.570. [DOI] [PubMed] [Google Scholar]
- Dallam GM, Jonas S, Miller TK. Medical considerations in triathlon competition: recommendations for triathlon organisers, competitors and coaches. Sports Med. 2005;35:143–161. doi: 10.2165/00007256-200535020-00004. [DOI] [PubMed] [Google Scholar]
- Darrow DC, Yannet H. The changes in the distribution of body water accompanying increase and decrease in extracellular electrolyte. J Clin Invest. 1935;14:266. doi: 10.1172/JCI100674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dugas J, Oosthuizen U, Tucker R, Noakes T. Rates of fluid ingestion alter pacing but not thermoregulatory responses during prolonged exercise in hot and humid conditions with appropriate convective cooling. Eur J Appl Physiol. 2009;105:69–80. doi: 10.1007/s00421-008-0876-6. [DOI] [PubMed] [Google Scholar]
- Dunn FL, Brennan TJ, Nelson AE, Robertson GL. The role of blood osmolality and volume in regulating vasopressin secretion in the rat. J Clin Invest. 1973;52:3212. doi: 10.1172/JCI107521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitts RH. Cellular mechanisms of muscle fatigue. Physiol Rev. 1994;74:49–94. doi: 10.1152/physrev.1994.74.1.49. [DOI] [PubMed] [Google Scholar]
- Goulet ED. Effect of exercise-induced dehydration on time-trial exercise performance: a meta-analysis. Br J Sports Med. 2011;45(14):1149–56. doi: 10.1136/bjsm.2010.077966. [DOI] [PubMed] [Google Scholar]
- Goulet ED. Dehydration and endurance performance in competitive athletes. Nutr Rev. 2012;70:S132–S136. doi: 10.1111/j.1753-4887.2012.00530.x. [DOI] [PubMed] [Google Scholar]
- Hew-Butler T, Collins M, Bosch A, Sharwood K, Wilson G, Armstrong M, Jennings C, Swart J, Noakes T. Maintenance of plasma volume and serum sodium concentration despite body weight loss in ironman triathletes. Clin J Sport Med. 2007;17:116–122. doi: 10.1097/JSM.0b013e3180326836. [DOI] [PubMed] [Google Scholar]
- Hew-Butler T, Rosner MH, Fowkes-Godek S, Dugas JP, Hoffman MD, Lewis DP, Maughan RJ, Miller KC, Montain SJ, Rehrer NJ, Roberts WO, Rogers IR, Siegel AJ, Stuempfle KJ, Winger JM, Verbalis JG. Statement of the Third International Exercise-Associated Hyponatremia Consensus Development Conference, Carlsbad, California, 2015. Clin J Sport Med. 2015;25:303–320. doi: 10.1097/JSM.0000000000000221. [DOI] [PubMed] [Google Scholar]
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hiller WDB, O'Toole ML, Fortess EE, Laird RH, Imbert PC, Sisk TD. Medical and physiological considerations in triathlons. Am J Sports Med. 1987;15:164–167. doi: 10.1177/036354658701500212. [DOI] [PubMed] [Google Scholar]
- Holloszy JO, Kohrt WM. Regulation of carbohydrate and fat metabolism during and after exercise. Annu Rev Nutr. 1996;16:121–138. doi: 10.1146/annurev.nu.16.070196.001005. [DOI] [PubMed] [Google Scholar]
- Ivy JL. Role of carbohydrate in physical activity. Clin Sports Med. 1999;18:469–484. doi: 10.1016/s0278-5919(05)70162-9. [DOI] [PubMed] [Google Scholar]
- Jeukendrup AE, Jentjens RL, Moseley L. Nutritional considerations in triathlon. Sports Med. 2005;35:163–181. doi: 10.2165/00007256-200535020-00005. [DOI] [PubMed] [Google Scholar]
- Kay D, Marino FE. Failure of fluid ingestion to improve self-paced exercise performance in moderate-to-warm humid environments. J Thermal Biol. 2003;28:29–34. [Google Scholar]
- Kenefick RW, Cheuvront SN, Palombo LJ, Ely BR, Sawka MN. Skin temperature modifies the impact of hypohydration on aerobic performance. J Appl Physiol. 2010;109:79–86. doi: 10.1152/japplphysiol.00135.2010. [DOI] [PubMed] [Google Scholar]
- Kimber NE, Ross JJ, Mason SL, Speedy DB. Energy balance during an ironman triathlon in male and female triathletes. Int J Sport Nutr Exerc Metab. 2002;12:47–62. doi: 10.1123/ijsnem.12.1.47. [DOI] [PubMed] [Google Scholar]
- Knechtle B, Baumann B, Wirth A, Knechtle P, Rosemann T. Male ironman triathletes lose skeletal muscle mass. Asia Pac J Clin Nutr. 2010;19:91–97. [PubMed] [Google Scholar]
- Knechtle B, Knechtle P, Wirth A, Alexander Rust C, Rosemann T. A faster running speed is associated with a greater body weight loss in 100-km ultra-marathoners. J Sports Sci. 2012;30:1131–1140. doi: 10.1080/02640414.2012.692479. [DOI] [PubMed] [Google Scholar]
- Knechtle B, Nikolaidis PT, Rosemann T, Rust CA. [Ironman Triathlon] Praxis (Bern 1994) 2016;105:761–773. doi: 10.1024/1661-8157/a002369. [DOI] [PubMed] [Google Scholar]
- Knechtle B, Wirth A, Baumann B, Knechtle P, Kohler G, Rosemann T, Senn O. An ironman triathlon does not lead to a change in body mass in female triathletes. Res Sports Med. 2010;18:115–126. doi: 10.1080/15438621003627059. [DOI] [PubMed] [Google Scholar]
- Kreider RB. Physiological considerations of ultraendurance performance. Int J Sport Nutr. 1991;1:3–27. doi: 10.1123/ijsn.1.1.3. [DOI] [PubMed] [Google Scholar]
- Kreider RB, Boone T, Thompson WR, Burkes S, Cortes CW. Cardiovascular and thermal responses of triathlon performance. Med Sci Sports Exerc. 1988;20:385–390. doi: 10.1249/00005768-198808000-00010. [DOI] [PubMed] [Google Scholar]
- Laird RH, Johnson D. The medical perspective of the Kona Ironman Triathlon. Sports Med Arthrosc. 2012;20:239. doi: 10.1097/JSA.0b013e3182736e8e. [DOI] [PubMed] [Google Scholar]
- Latzka WA, Montain SJ. Water and electrolyte requirements for exercise. Clin Sports Med. 1999;18:513–524. doi: 10.1016/s0278-5919(05)70165-4. [DOI] [PubMed] [Google Scholar]
- Laursen PB, Suriano R, Quod MJ, Lee H, Abbiss CR, Nosaka K, Martin DT, Bishop D. Core temperature and hydration status during an Ironman triathlon. Br J Sports Med. 2006;40:320–325. doi: 10.1136/bjsm.2005.022426. discussion 325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lepers R. Analysis of Hawaii ironman performances in elite triathletes from 1981 to 2007. Med Sci Sports Exerc. 2008;40:1828–1834. doi: 10.1249/MSS.0b013e31817e91a4. [DOI] [PubMed] [Google Scholar]
- McDermott BP, Anderson SA, Armstrong LE, Casa DJ, Cheuvront SN, Cooper L, Kenney WL, O'Connor FG, Roberts WO. National Athletic Trainers' Association Position Statement: Fluid Replacement for the Physically Active. J Athl Train. 2017;52:877–895. doi: 10.4085/1062-6050-52.9.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer M, Knechtle B, Bürge J, Knechtle P, Mrazek C, Wirth A, Ellenrieder B, Rüst CA, Rosemann T. Ad libitum fluid intake leads to no leg swelling in male Ironman triathletes–an observational field study. J Int Soc Sports Nutr. 2012;9:1. doi: 10.1186/1550-2783-9-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montain SJ, Coyle EF. Influence of graded dehydration on hyperthermia and cardiovascular drift during exercise. J Appl Physiol. 1992;73:1340–1350. doi: 10.1152/jappl.1992.73.4.1340. [DOI] [PubMed] [Google Scholar]
- Mueller SM, Anliker E, Knechtle P, Knechtle B, Toigo M. Changes in body composition in triathletes during an Ironman race. Eur J Appl Physiol. 2013;113:2343–2352. doi: 10.1007/s00421-013-2670-3. [DOI] [PubMed] [Google Scholar]
- Noakes TD. Physiological models to understand exercise fatigue and the adaptations that predict or enhance athletic performance. Scand J Med Sci Sports. 2000;10:123–145. doi: 10.1034/j.1600-0838.2000.010003123.x. [DOI] [PubMed] [Google Scholar]
- Noakes TD. Does dehydration impair exercise performance? Med Sci Sports Exerc. 2007;39:1209–1217. doi: 10.1249/mss.0b013e318124a664. [DOI] [PubMed] [Google Scholar]
- Rehrer N, Beckers E, Brouns F, Ten Hoor F, Saris W. Effects of dehydration on gastric emptying and gastrointestinal distress while running. Med Sci Sports Exerc. 1990;22:790–795. doi: 10.1249/00005768-199012000-00010. [DOI] [PubMed] [Google Scholar]
- Robertson GL, Athar S. The interaction of blood osmolality and blood volume in regulating plasma vasopressin in man. J Clin Endocrinol Metab. 1976;42:613–620. doi: 10.1210/jcem-42-4-613. [DOI] [PubMed] [Google Scholar]
- Rolls BJ, Wood R, Rolls ET, Lind H, Lind W, Ledingham JG. Thirst following water deprivation in humans. Am J Physiol. 1980;239:R476–R482. doi: 10.1152/ajpregu.1980.239.5.R476. [DOI] [PubMed] [Google Scholar]
- Rose BD. Pathophysiology of renal disease. McGraw-Hill Professional Publishing; 1987. [Google Scholar]
- Rowell LB. Cardiovascular adjustments to thermal stress. Compr Physiol. 1983.
- Sawka MN. Physiological consequences of hypohydration: exercise performance and thermoregulation. Med Sci Sports Exerc. 1992;24:657–670. [PubMed] [Google Scholar]
- Sawka MN, Cheuvront SN, Kenefick RW. Hypohydration and Human Performance: Impact of Environment and Physiological Mechanisms. Sports Med. 2015;1:S51–60. doi: 10.1007/s40279-015-0395-7. 45 Suppl. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawka MN, Leon LR, Montain SJ, Sonna LA. Integrated physiological mechanisms of exercise performance, adaptation, and maladaptation to heat stress. Compr Physiol. 2011 doi: 10.1002/cphy.c100082. [DOI] [PubMed] [Google Scholar]
- Sawka MN, Montain SJ. Fluid and electrolyte supplementation for exercise heat stress. Am J Clin Nutr. 2000;72:564S–572S. doi: 10.1093/ajcn/72.2.564S. [DOI] [PubMed] [Google Scholar]
- Sawka MN, Pandolf KB. Effects of body water loss on physiological function and exercise performance. Perspectives in Exercise Science and Sports Medicine. 1990;3:1–38. [Google Scholar]
- Sawka MN, Young AJ, Latzka WA, Neufer PD, Quigley MD, Pandolf KB. Human tolerance to heat strain during exercise: influence of hydration. J Appl Physiol. 1992;73:368–375. doi: 10.1152/jappl.1992.73.1.368. [DOI] [PubMed] [Google Scholar]
- Speedy DB, Noakes TD, Kimber NE, Rogers IR, Thompson JM, Boswell DR, Ross JJ, Campbell RG, Gallagher PG, Kuttner JA. Fluid balance during and after an ironman triathlon. Clin J Sport Med. 2001;11:44–50. doi: 10.1097/00042752-200101000-00008. [DOI] [PubMed] [Google Scholar]
- Speedy DB, Rogers IR, Noakes TD, Thompson JM, Guirey J, Safih S, Boswell DR. Diagnosis and prevention of hyponatremia at an ultradistance triathlon. Clin J Sport Med. 2000a;10:52–58. doi: 10.1097/00042752-200001000-00010. [DOI] [PubMed] [Google Scholar]
- Speedy DB, Rogers IR, Noakes TD, Wright S, Thompson JM, Campbell R, Hellemans I, Kimber NE, Boswell DR, Kuttner JA. Exercise-induced hyponatremia in ultradistance triathletes is caused by inappropriate fluid retention. Clin J Sport Med. 2000b;10:272–278. doi: 10.1097/00042752-200010000-00009. [DOI] [PubMed] [Google Scholar]
- Stiefel M, Rust CA, Rosemann T, Knechtle B. A comparison of participation and performance in age-group finishers competing in and qualifying for Ironman Hawaii. Int J Gen Med. 2013;6:67–77. doi: 10.2147/IJGM.S40202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh R, Noakes T, Hawley J, Dennis S. Impaired high-intensity cycling performance time at low levels of dehydration. Int J Sports Med. 1994;15:392–398. doi: 10.1055/s-2007-1021076. [DOI] [PubMed] [Google Scholar]
- Williamson MA, Snyder LM. Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis. Lippincott Williams & Wilkins; 2014. [Google Scholar]
- Wingo JE, Ganio MS, Cureton KJ. Cardiovascular drift during heat stress: implications for exercise prescription. Exerc Sport Sci Rev. 2012;40:88–94. doi: 10.1097/JES.0b013e31824c43af. [DOI] [PubMed] [Google Scholar]
- Zouhal H, Groussard C, Minter G, Vincent S, Cretual A, Gratas-Delamarche A, Delamarche P, Noakes TD. Inverse relationship between percentage body weight change and finishing time in 643 forty-two-kilometer marathon runners. Br J Sports Med. 2011;45:1101–1105. doi: 10.1136/bjsm.2010.074641. [DOI] [PubMed] [Google Scholar]


