Abstract
Leiomyosarcomas are known to typically originate from smooth muscle cell. Primary adrenal leiomyosarcoma is an extremely rare mesenchymal tumor associated with delayed diagnosis and poor prognosis. We report a rare case of leiomyosarcoma arising from the left adrenal gland in a 27-year-old male who presented with left side back ache. It was a solid mass of cms situated superior to the left kidney. Left adrenalectomy was done and microscopic examination revealed a primary adrenal leiomyosarcoma.
Keywords: Primary adrenal leiomyosarcoma, Adrenalectomy, Immunohistochemistry
Introduction
Primary adrenal leiomyosarcoma is a very rare tumor and represents 0.1–0.2% of all intra-abdominal soft tissue malignancies in adults [1]. The diagnosis is based on the findings of both histological and immuno-histochemical examinations, which are indispensable not only for determining the type of the tumor, but also for predicting its biological behavior. Leiomyosarcomas are known to arise from smooth muscle within the various organs such as the uterus, alimentary canal, and blood vessels. Primary adrenal leiomyosarcoma is extremely rare and only around 30 cases have been reported in the English literature [1, 2]. It presents typically as a retroperitoneal mass with symptoms of pain, mass, and pressure effect on the surrounding organs. It is difficult to make a pre-operative diagnosis as there are no specific radiologic features available, although imaging studies including CT and MRI are important for assessing the resectability of the tumor as well as assessing the possibility of metastasis. We herein report a rare case of leiomyosarcoma potentially arising from the left adrenal gland in a 27-year-old male who presented with left side back ache.
Case report
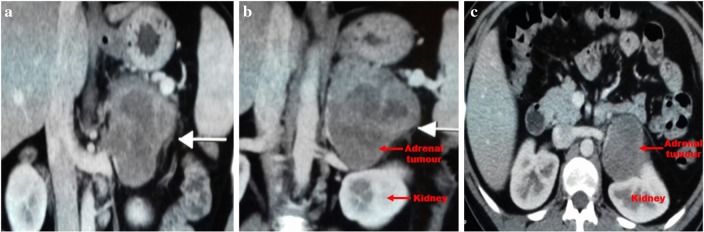
A 27-year-old male presented to the Uro-oncological services of the hospital with complaints of left loin pain which had gradually increased in severity since the past 2 months. The patient was moderately built and nourished with his blood pressure within normal ranges. Routine blood and urine biochemical tests were all within normal ranges. Abdominal ultrasonography (USG) revealed a huge mass in the region of left suprarenal area. Computed tomography (CT) revealed a well-defined soft tissue density in the left suprarenal region measuring 9 6.5 7 cms (Fig. 1). Post contrast study showed moderate enhancement with irregular non-enhancing necrotic areas within. Perilesional fat stranding was seen with thickening of the left anterior renal fascia, medially the lesion was not seen separately from the body and the lateral limb of the left adrenal gland. The tumor displaced the left kidney postero-inferiorly and showed minimal vascularity with feeders from the superior adrenal artery. Few enlarged para aortic lymph nodes were seen at the level of renal hilum, largest measuring 1.9 1.4 cms.
Fig. 1.
Computed tomography (CT) showing a well-defined soft tissue density in the left suprarenal region measuring 9 × 6.5 × 7 cms
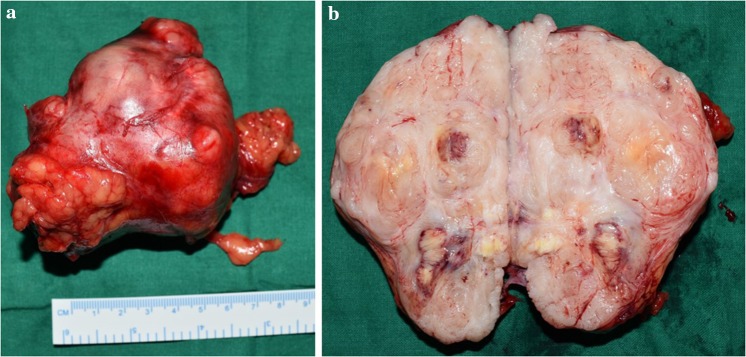
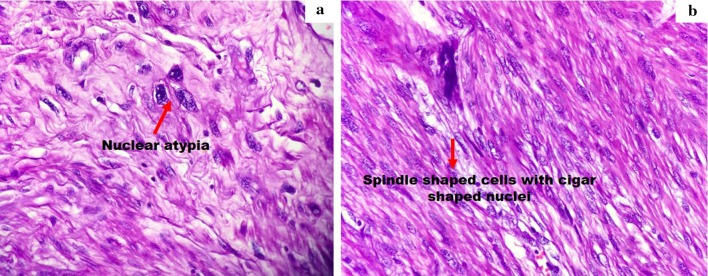
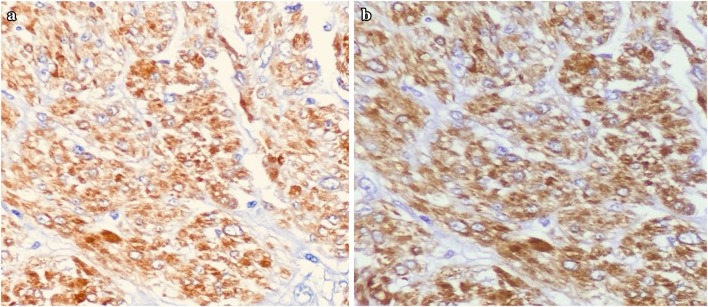
Twenty-four hours urinary excretion of vanillyl mandelic acid (VMA) was 6.30 mg/24 h and serum cortisol was 8.32 g/dl. Similarly 24 h excretion of urinary catecholamines was within normal range. In view of the CT and biochemical findings an open left adrenalectomy was performed and the excised specimen sent for histo-pathological examination (Fig. 2a, b). Gross examination of the specimen showed a nodular, firm, well encapsulated tumor (Fig. 3a, b). Microscopic examination showed a well encapsulated tumor with tumor cells that were spindle shaped with prominent, eosinophilic cytoplasm resembling smooth muscle fibers. Most of the nuclei were elongated, enlarged, hyperchromatic and vesicular with coarse chromatin. Nuclear mitosis was prominently increased. A diagnosis of primary adrenal leiomyosarcoma was made. Immuno-histochemistry studies showed a Desmin positive, H-Caldesmon positive and C-kit negative tumour (Fig. 4a, b). The MIB-1/Ki-67 proliferative index is approximately 18–20% in the proliferative area of the tumour.
Fig. 2.
Gross specimen of left adrenalectomy showing nodular, firm, well encapsulated tumour
Fig. 3.
Microscopic examination showing well encapsulated tumour with tumour cells that were spindle shaped with prominent, eosinophilic cytoplasm resembling smooth muscle fibers. There is moderate nuclear atypia with few bizarre atypical nuclear forms. The mitotic activity is in the range of 8–9 mitosis/50 high power fields. There is characteristic mast cell and eosinophil infiltration within the tumour
Fig. 4.
Immuno-histochemistry of the mass shows Desmin positive, H-Caldesmon positive and C-kit negative tumour
Discussion
Primary adrenal leiomyosarcoma (PML) was first reported by Choi and Liu [3]. It is believed to originate from the smooth muscle wall of the central adrenal vein and its branches [4]. The tumors are most commonly seen in the elderly patients, with abdominal or flank pain being the most common presenting features. Other symptoms include lower extremity edema, spider angiomata whenever the tumor invades the inferior vena cava. The incidence is approximately same both in the females and males, and equally located on the right and left side. Only two cases of bilateral tumors have been reported as of now [5, 6]. Histologically most of the reported cases are of conventional type and only five cases are of pleomorphic variety [2]. Four of the reported patients were immune-deficient due to HIV (Human immunodeficiency virus) or Epstein-Barr virus infection [2, 5]. Probably these tumors arise in an immunosuppressive situation however, it is not certain whether these viruses are known to be pathogenetic.
PML are known not to produce any adrenal hormones and there are no known tumor markers that are applicable for diagnosis. Similarly there are no imaging characteristics that one can associate with these lesions. Histopathological and immunohistochemical evaluation helps in determining the type of tumor and also helps in differential diagnosis. Conventional leiomyosarcomas show a strong immunoreactivity for smooth muscle markers such as smooth muscle actin and/or muscle specific actin in 90–95% of cases, and desmin in 70–90% of cases [2, 7].
The low incidence of adrenal leiomyosarcoma makes it difficult to draw a consistent treatment recommendation. Surgery remains the primary option in the management of these lesions. Complete resection with negative margins represents the most useful therapeutic option. Laparoscopic approach in malignant adrenal diseases remains a controversial issue, however, several reports regarding its feasibility have appeared in literature in the last few years [8, 9]. Sergio et al. [10] reported on the successful laparoscopic resection of an adrenal leiomyosarcoma. Prognosis remains unpredictable, however patients with invasive disease, venous thrombosis, adjacent organ invasion, and distant metastases carry a poor prognosis [11]. Adjuvant therapy combined with surgery has often been used especially in patients with poor prognosis.
Funding
None.
Compliance with ethical standards
Conflict of interest
The author declare that there is no competing interest.
Informed consent
Informed consent from the patient was taken prior to the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
R. B. Nerli, Email: rbnerli@gmail.com
Shridhar Ghagane, Email: shridhar.kleskf@gmail.com.
Neeraj S. Dixit, Email: neerajdixit08@yahoo.co.in
Murigendra B. Hiremath, Email: murigendra@gmail.com
References
- 1.Onishi T, Yanagihara Y, Kikugawa T, Miura N, Noda T, Kakuda T, et al. Primary adrenal leiomyosarcoma with lymph node metastasis: a case report. World J Surg Oncol. 2016;14:176. doi: 10.1186/s12957-016-0936-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou Y, Tang Y, Tang J, Deng F, Gong G, Dai Y. Primary adrenal leiomyosarcoma: a case report and review of literature. Int J Clin Exp Pathol. 2015;8:4258–4263. [PMC free article] [PubMed] [Google Scholar]
- 3.Choi SH, Liu K. Leiomyosarcoma of the adrenal gland and its angiographic features: a case report. J Surg Oncol. 1981;16:145–148. doi: 10.1002/jso.2930160205. [DOI] [PubMed] [Google Scholar]
- 4.Lack EE, Graham CW, Azumi N, Bitterman P, Runsnock EJ, O’brien W, Lynch JH. Primary leiomyosarcoma of adrenal gland Case report with immune-histochemical and ultrastructural study. Am J Surg Pathol. 1991;15:899–905. doi: 10.1097/00000478-199109000-00011. [DOI] [PubMed] [Google Scholar]
- 5.Linos D, Kiriakopoulos AC, Tsakayannis DE, Theodoridou M, Chrousos G. Laparoscopic excision of bilateral primary adrenal leiomyosarcoma in a 14-year old girl with acquired immuno-deficiency syndrome (AIDS) Surgery. 2004;136:1098–1100. doi: 10.1016/j.surg.2003.07.007. [DOI] [PubMed] [Google Scholar]
- 6.Hamada S, Ito K, Tobe M, Otsuki H, Hama Y, Kato Y, Suqiura Y, Kaji T, Asano T, Hayakawa M. Bilateral adrenal leiomyosarcoma treated with multiple local therapies. Int J Clin Oncol. 2009;14:356–360. doi: 10.1007/s10147-008-0844-5. [DOI] [PubMed] [Google Scholar]
- 7.Mohanty SK, Balani JP, Parwani AV. Pleomorphic leiomyosarcoma of the adrenal gland: case report and review of the literature. Urology. 2007;70:591. doi: 10.1016/j.urology.2007.07.029. [DOI] [PubMed] [Google Scholar]
- 8.Nerli RB, Reddy MN, Guntaka A, Patil S, Hiremath MB. Laparoscopic adrenalectomy for adrenal masses in children. J Paed Urol. 2011;7:182–186. doi: 10.1016/j.jpurol.2010.04.006. [DOI] [PubMed] [Google Scholar]
- 9.Ravish IR, Nerli RB, Reddy MN, Suresh SN, Thakkar R. Laparoscopic adrenalectomy for large pheochromocytoma. BJU Int. 2007;100:1126–1129. doi: 10.1111/j.1464-410X.2007.07179.x. [DOI] [PubMed] [Google Scholar]
- 10.Sergio Q, Califano I, Carrizo F, Daffinoti A, Calónico N. Primary adrenal leiomyosarcoma treated by laparoscopic adrenalectomy. Endocrinol Nutr. 2015;62:472–473. doi: 10.1016/j.endonu.2015.05.008. [DOI] [PubMed] [Google Scholar]
- 11.Matsui Y, Fujikawa K, Oka H, Fukuzawa S, Takeuchi H. Adrenal leiomyosarcoma extending into the right atrium. Int J Urol. 2002;9:54–56. doi: 10.1046/j.1442-2042.2002.00413.x. [DOI] [PubMed] [Google Scholar]