Abstract
Introduction: Low quality of life is one of the most common symptoms of Multiple Sclerosis (MS) which can reduce satisfaction with life, as well as increase death ratio and neuro-mental problems. The present study aimed to determine the effect of Mindfulness-Based Stress Reduction (MBSR) therapy on the quality of life in women with Multiple sclerosis in the city of Ahvaz.
Methods: Forty eight patients who had referred to neurologists were selected by convenient sampling and were assigned into two groups (MBSR and control) randomly. The participants of the two groups answered the 36-item quality of life questionnaire. The experimental group was under treatment for 8 sessions while the control group did not receive any psychological treatment. Data were analyzed, using SPSSver.13 software by repeated measures analysis of variance.
Results: In the MBSR group, the mean subscales of QOL had more significant reduction compare to control group. Also the improvement of all subscales of mental and physical QOL continued after two months later in follow up stage.
Conclusion: The findings suggest that MBSR is useful for improving the quality of life in patients with MS.
Keywords: Multiple sclerosis, Mindfulness, Quality of life
Introduction
Multiple sclerosis (MS) is the most common chronic neurological disease that affects adults between 20 to 50 years .1 MS prevalence ranges from 54 to 223 per 100,000 people in the world, and about two and a half million people worldwide suffer from multiple sclerosis.2 World Health Organization estimated the prevalence of MS 51.54 per 100,000 in Iran.1 According to the latest report from Khuzestan province to the MS Society until 2012, the number of people diagnosed with MS disease was 1130 people, 600 of whom are living in the city of Ahvaz.3
In general, MS is classified into four main types: relapsing–remitting, secondary progressive type, primary progressive type, and relapsing–progressive.4 about 5% of MS patients have quick changes with repetitive relapse and progress of disability. In contrast, 10-20 percent of MS patients have benign disease which remains over a long time. However, it can be associated with rare recurrence.5
Physical performances, social relationships and job opportunities are all impaired in patients with MS. These factors often have adverse effects on the quality of life (QOL) and life satisfaction level.6,7 the quality of life is the people's perception of their position in life in terms of culture, value system of where they live, goals, expectations, standards and priorities. It is quite individual in nature, and cannot normally be observed by others and is based on people's perception of various aspects of their lives.8
Previous studies have shown that patients with MS experience a lower QOL than the control group.9,10 in recent years, there have been a lot of studies focusing on the relationship between symptoms and low QOL among MS patients. Overall, the studies have shown that fatigue and psychological symptoms were significantly related to the QOL.9-12
In recent years a variety of psychological treatments that are known as complementary treatment have been used to reduce the number of attacks in these diseases. One way to complement the medication treatment is mindfulness-based stress reduction therapy (MBSR) it is a complementary and alternative medicine based on the mind-body intervention, which has been identified as a potential treatment for insomnia13 and it has been shown, especially in mindfulness training, to reduce anxiety and improve the quality of life.14-17 MBSR effects on well- being and QOL of patients with chronic illness by mechanisms such as relaxation, meta-cognitive insight, preservative thinking, and contact with reality compassion, empathy, exposure and cognitive reappraisal.18
Some of these mechanisms are unique to MBSR compared to other therapies. In a recent study, MBSR and consciousness Yoga program have been shown to improve QOL in MS patients, but there has been no follow-ups stage to evaluate the effects in the long run.19 Due to the increasing frequency of MS in Iran1 and its detrimental Effects on the patient’s quality of life, the use of new therapies that have proved to be effective in other parts of the world seems to be necessary. Therefore in this study has been evaluated the effect of MBSR on quality of life in women with MS and followed the therapeutic achievements. Also, a larger sample size has been selected from another city of Iran.
Materials and methods
This randomized controlled clinical trial was performed in 2014 in Ahvaz MS Society (IRCT201507087227N5). The study population included all female patients aged 20 - 50 years with MS referring to Ahvaz MS society from January to June 2014.
The sample size was calculated based on a previous study in which Grossman et al., investigated the impact of mindfulness training on QOL, depression and fatigue in patients with MS and reported that the mean and standard deviation of depression before the intervention was 16.33 (10.46) and changed to 5.29 (7.07) after the intervention.20
According to a 95% confidence level and test power of 0.9% using Cohen’s formula, 15 participants were estimated to be needed in each group. However, we recruited 24 patients in each group to achieve more reliable results.
After the sample size calculation and reviewing the files of patients with MS in Ahvaz MS society, 48 patients meeting the inclusion criteria were selected by convenient sampling. Then patients were called on and invited to participate in the study. If a patient agreed to participate, he or she was invited to attend the study briefing session and if not, another patient was selected in a similar fashion. Then, using a random number table, they were assigned into experimental (MBSR) and control groups. The inclusion criteria were having a medical diagnosis of MS, having a minimum literacy of intermediate school level, not having a psychotic disorder (according to the structural clinical interview for DSM disorders for Axis I; SCID-I administered by a clinical psychologist) and receiving no regular psychotherapy during the last 6 months. The exclusion criteria were having a relapsing MS and absence of more than two therapeutic sessions.
In addition to the usual treatments for MS, the experimental group received eight weeks of MBSR training weekly, according to the protocol developed by Kabat-Zinn.21 the outline of the protocol is shown in (Table 1)However, the control group only received treatments as usual (TAU). The quality of life questionnaire was administered to the experimental group at pre-test (before the intervention), post-test (at the end of intervention) and two months after the end of intervention (follow-up).
Table 1. The content of the sessions .
| 1st Session | Introducing the concept of automatic pilot Promoting raisin-eating, body-inspection |
| 2nd Session | Facing obstacle Practicing yoga |
| 3rd Session | Perform mindfulness while breathing Doing meditation while sitting |
| 4th Session | Staying in present Ticking off pleasant thoughts Mastering STOP technique |
| 5th Session | Identifying and accepting unpleasant experiences Discussing insights and communication |
| 6th Session | Moving from the intrapersonal to the interpersonal world Discovering conflict management Managing outrage or conscious anger |
| 7th Session | Planning for personal care Alleviating pain Seeking the right refuge for pain |
| 8th Session | Recapitulating the acquired techniques during the treatment Writing an autobiography in 5 chapters |
Patients in the TAU group were also invited to Ahvaz MS society to respond to the quality of life questionnaire simultaneously with the MBSR group. Patients in both groups completed the demographic questionnaire at baseline. Both groups also received their routine drug treatments. All the MBRS sessions were held in Ahvaz MS Society and held by a trained psychologist. Each session lasted for 120 minutes from 10 to 12 o’clock on Tuesdays. For participants who had missed one or two sessions, additional sessions were held. After finishing the study, all patients in the control group were also contacted and invited to voluntarily attend MBSR sessions similar to those the experimental group had passed.
Quality of Life scale has proved its applications in clinical practice, health policy, as well as studies to evaluate its effectiveness in the general population. Concepts that are measured by this questionnaire are not assigned to age and a specific disease. The questionnaire is designed to assess the health of both physical and mental status, formed by the combination of eight health domains scores. The questionnaire contains 36 questions that evaluate the eight domains of health.22
In addition to measuring 8 aspects of quality, two combined scales which are formed by the integration of scales are achieved, too.
-
Physical Component Summary (PCS)
Physical functioning + physical problems + bodily pain + general health
-
Mental Component Summary (MCS)
Social functioning + mental health + vitality + mental problems
The reliability and validity of the questionnaire were confirmed in a study in Persian.23 the score of each of the areas was calculated independently in accordance with the instructions. Scoring ranged from zero (worst) to 100 (best condition). In the present study the alpha coefficient of 0.90 was obtained.
The study flow chart is brought in (Figure 1). The data quality of life of the 36 questions were statistically analyzed, using SPSS (version 13.0, Chicago, IL, USA), and mean and standard deviation were used in descriptive statistics, and inferential statistics was provided using the repeated measures analysis of variance (RM-ANOVA).
Figure 1.
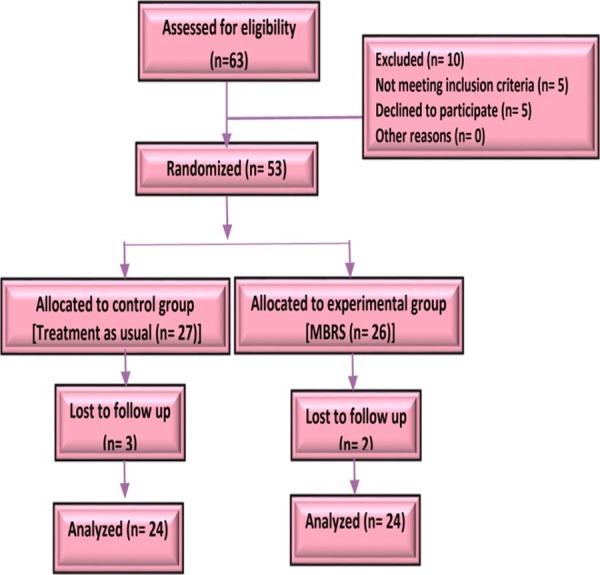
The study design
Results
The sample containing demographic characteristics, including age, marital status and education level with t- test and chi-square test is given in (Table 2). In addition,
Table 2. Demographic characteristics of patients with MS in MBSR and control groups .
| Variable | MBSR | Control | P |
| Age | 5.77 ( 25.70) | 2.39 ( 24.85) | 0.54a |
| Education level | 0.88b | ||
| High school | 10 (25) | 11 (27.5) | |
| Bachelor | 10 (25) | 9 (22.5) | |
| Marital status | 0.99c | ||
| Married | 10 (25) | 10 (25) | |
| Single | 10 (25) | 10 (25) |
Abbreviations: MBSR, mindfulness-based stress reduction, aData are presented as mean ( SD) or No. (%),bt-test,c Chi-square test.
marital status and educational level and frequency are shown in parentheses.
In the table above, the mean and the standard deviation of the age for experimental and control groups has been provided. There was no significant difference between the two groups in the demographic characteristics such as age, marital status and education level. Mauchly’s test of sphericity showed the null hypothesis that the error covariance matrix of the orthonormalized transformed dependent variables is proportional to an identity matrix was confirmed (Mauchly’s W=398, P<0.01). Hotelling’s trace test showed there were significant differences between the two groups in sleep quality scores in 3 phases (F= 18.789, P< 0.001).
Table 3 shows the mean scores and standard deviation of the scores in the subscales of the quality of life in the experimental and control groups, according to the pre-test, post-test and follow-up. The table shows that the mean quality of life subscales scores in MBSR group were improved in 2 phases (posttest and follow- up) compared to prates
Table 3. Mean and standard deviation of scores in the subscales of the quality of life in the experimental and control groups, according to the pre-test, post-test and follow-up .
| Outcome measure | Pre-test Mean (SD) |
Post-test Mean (SD) | Follow-up Mean (SD) | Mean Square | df | F | Time P |
Time ×Group P |
| General health | 2332.00 | 1 | 16.79 | < 0.001 | < 0.001 | |||
| MBSR | 46.05(8.30) | 46.30(7.27) | 46.20(7.92) | |||||
| TAU | 45.60(7.84) | 59.35(5.33) | 60.05(5.40) | |||||
| Physical functioning | 2033.63 | 1 | 17.28 | <0 .001 | <0 .001 | |||
| MBSR | 46.90(7.01) | 47.30(6.99) | 47.20(7.25) | |||||
| TAU | 46(7.43) | 59.80(5.57) | 60.30(5.20) | |||||
| Limitation in roles due to physical problems | 2000.83 | 1 | 15.60 | <0 .001 | < 0.001 | |||
| MBSR | 46.5(6.64) | 47.45(6.51) | 47.25(7.22) | |||||
| TAU | 45.85(7.59) | 59.5(6.35) | 60.35(6.63) | |||||
| Limitation in roles due to emotional problem | 2314.40 | 1 | 18.09 | <0 .001 | <0 .001 | |||
| MBSR | 46.35(7.78) | 46.40(7.59) | 46.25(7.36) | |||||
| TAU | 45.90))7.17 | 59.15(5.51 ) | 60.30(5.63) | |||||
| bodily pain | 1888.13 | 1 | 16.25 | < 0.001 | <0 .001 | |||
| MBSR | 46.65(6.57) | 47.65(6.56) | 47.40(6.56) | |||||
| TAU | 45.85(7.88) | 59.55(5.81) | 60.10(5.55) | |||||
| Social functioning | 1840.83 | 1 | 15.74 | <0 .001 | <0 .001 | |||
| MBSR | 46.90(7.01) | 47.25(6.93) | 47.40(6.90) | |||||
| TAU | 45.55(7.77) | 59.30(5.19) | 60(5.04) | |||||
| Vitality | 1904.03 | 1 | 18.69 | < 0.001 | < 0.001 | |||
| MBSR | 46.70(6.38) | 47.75(6.52) | 48.10(6.48) | |||||
| TAU | 45.70(7.39) | 60.30(5.57) | 60.45(5.42) | |||||
| Mental health | 1778.70 | 1 | 15.20 | <0 .001 | < 0.001 | |||
| MBSR | 46.95(6.95) | 47.65(6.56) | 47.80(6.97) | |||||
| TAU | 45.65(7.84) | 59.40(5.32) | 60.45(5.29) |
Discussion
The aim of this study was to investigate the effect of MBSR on the QOL in female patients with multipl sclerosis in city of Ahvaz, Iran. The findings indicate that this therapy is effective in improving quality of life. So MBSR improves QOL in the experimental group compared with the control group at post-test and follow-up during two months. The results of this study are consistent with findings from other studies.23,25
Given that the QOL has various dimensions (including physical, psychological, social and spiritual), mindfulness exercise is designed to have an impact on all these dimensions.
Regular mindfulness exercises lead to increased self-acceptance, reduced sensitivity to transient thoughts and emotions and improve the ability to respond to different situations. By developing the non-judgmental awareness of thoughts, emotions and life events, it can provide the preliminaries for health, happiness in life and consequently, improve the QOL in mental areas.
It seems all practices of MBSR can improve mental health area of QOL. The formal practices of MBSR (such as mindful breathing, body scan, mindful yoga and sitting meditation) can increase awareness to here and now and improve mental states. Also people with informal practices of MBSR (doing all activities in daily life such as walking, dish washing, taking a shower, with awareness and nonjudgmental attention) can get more satisfaction and vitality. On the other hand, MBSR learns patients to pay attention and to writ the pleasant events in daily life. It can improve their mood and emotions.
One mental health component of QOL is social functioning. People were trained with Mindfulness practices to pay attention to their interpersonal relationships. The STOP technique learns the patients to not get stuck in habitual patterns about activities of daily life and interpersonal relationships especially under stress. The STOP (that is an acronym word) learns you to Stop and pause momentarily whatever you’re doing (S), Take a breath (T), Observe and notice what is happening inside you, and outside of you (O) and Proceed and continue doing what you were doing, or don’t (P).21 With doing the STOP, people can get rid of reactive responses to individual and interpersonal stimuluses and show suitable responses. Other techniques about anger management and conflict management help people improve their communication with others.
Planning for personal care is another practice of MBSR that it can improve QOL in both area (mental and physical). MBSR practices and techniques reconcile people with their values such as interpersonal effectiveness and self- care 26 that they disturb in MS.
Our knowledge about the body. In MBSR, attention is given to the body and breathing exercises and we become aware of having the feeling that we experienced in the body and even our breathing. Moreover, when we realize we are in a state of anger, the body is heated while in a state of fear, the heart rate increases, and breathing becomes short and sharp. By doing yoga, we experience our body more and this knowledge provides more Control.16
In fact, it seems that the practice of awareness of the Present moment is effective through techniques such as focusing on the breath and body awareness and focus on the here and now, as well as on the cognitive and information processing.16 Also MBSR improved QOL in physical areas especially physical pain. Continuous mindfulness training increases
MBSR can improve perception about the pain through acceptance and nonjudgmental attitude that it is flourished in the process of the therapy. A review demonstrated that while expert meditators report the same pain intensity as non-meditators, they experience reduced unpleasantness. Also people with lower-back pain found limited evidence that MBSR can improve pain acceptance.26 so while the pain is still there, the patient is less involved with it and he/she can deal with the values in the life and QOL was promoted.
Overall, we might conclude that mindfulness is a way of thinking and living which, in addition to the mental discipline of mindfulness, is followed by discipline and physical and physiological consequences. This type of system that leads to the well-being and physical and mental health can be preferred in the lives of people with chronic pain who are looking for better compatibility with the problems.
It is noteworthy, therapists who use the MBSR techniques should be aware of the continuing training programs in patients. One study has shown that usually the subjects' scores in the follow-up period tend to return to pre-test scores.26 However, the continuing effects of therapy are also reported in the follow-up of our study.
This study had some limitations. It was carried out only with patients with low MS severity. Also this study investigated only the females suffering from MS who had visited MS Clinic in Ahwaz
Conclusion
Mindfulness based stress reduction is an effective therapy on the quality of life in female patients with MS. It can decrease patients’ problems in physical functioning and bodily pain. Also practices of MBSR can increase Social functioning and vitality and overall physical and mental health in patients with MS.
Acknowledgments
Authors are grateful to staff of Ahvaz MS Society and participants.
Ethical issues
None to be declared.
Conflict of interest
The authors declare no conflict of interest in this study
Citation: Kolahkaj B, Zargar F, Majdinasab N. The effect of mindfulness-based stress reduction (MBSR) therapy on quality of life in women with multiple sclerosis, Ahvaz, Iran. J Caring Sci 2019; 8 (4): 213-7. doi:10.15171/jcs.2019.030.
References
- 1.Etemadifar M, Izadi S, Nikseresht A, Sharifian M, Sahraian MA, Nasr Z. Estimated prevalence and incidence of multiple sclerosis in Iran. Eur Neurol. 2014;72(5-6):370–4. doi: 10.1159/000365846. [DOI] [PubMed] [Google Scholar]
- 2.Julian LJ, Vella L, Vollmer T, Hadjimichael O, Mohr DC. Employment in multiple sclerosis. J Neurol. 2008;255(9):1354–60. doi: 10.1007/s00415-008-0910-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Latimer-Cheung AE, Pilutti LA, Hicks AL, Ginis KAM, Fenuta AM, MacKibbon KA. et al. Effects of exercise training on fitness, mobility, fatigue, and health-related quality of life among adults with multiple sclerosis: a systematic review to inform guideline development. Arch Phys Med Rehabil. 2013;94(9):1800–28. doi: 10.1016/j.apmr.2013.04.020. [DOI] [PubMed] [Google Scholar]
- 4.Janardhan V, Bakshi R. Quality of life in patients with multiple sclerosis: the impact of fatigue and depression. J Neurol Sci. 2002;205(1):51–8. doi: 10.1016/s0022-510x(02)00312-x. [DOI] [PubMed] [Google Scholar]
- 5.Cohen JA, Rae-Grant A. Handbook of multiple sclerosis. 1 st ed : Springer; 2010. New York: Springer; 2010. [Google Scholar]
- 6.Schiavolin S, Leonardi M, Giovannetti AM, Antozzi C, Brambilla L, Confalonieri P. et al. Factors related to difficulties with employment in patients with multiple sclerosis: a review of 2002–2011 literature. Int J Rehabil Res. 2013;36(2):105–11. doi: 10.1097/MRR.0b013e32835c79ea. [DOI] [PubMed] [Google Scholar]
- 7.Nejati S, Rajezi Esfahani S, Rahmani S, Afrookhteh G, Hoveida S. The effect of group mindfulness-based stress reduction and consciousness yoga program on quality of life and fatigue severity in patients with ms. J Caring Sci. 2016;5(4):325–35. doi: 10.15171/jcs.2016.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reid KJ, Baron KG, Lu B, Naylor E, Wolfe L, Zee PC. Aerobic exercise improves self-reported sleep and quality of life in older adults with insomnia. Sleep Med. 2010;11(9):934–40. doi: 10.1016/j.sleep.2010.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Papuć E, Stelmasiak Z. Factors predicting quality of life in a group of Polish subjects with multiple sclerosis: Accounting for functional state, socio-demographic and clinical factors. Clin Neurol Neurosurg. 2012;114(4):341–6. doi: 10.1016/j.clineuro.2011.11.012. [DOI] [PubMed] [Google Scholar]
- 10.Rainone N, Chiodi A, Lanzillo R, Magri V, Napolitano A, Morra VB. et al. Affective disorders and health-related quality of life (HRQOL) in adolescents and young adults with multiple sclerosis (MS): the moderating role of resilience. Qual Life Res. 2017;26(3):727–36. doi: 10.1007/s11136-016-1466-4. [DOI] [PubMed] [Google Scholar]
- 11.Newland PK, Lunsford V, Flach A. The interaction of fatigue, physical activity, and health-related quality of life in adults with multiple sclerosis (MS) and cardiovascular disease (CVD) Appl Nurs Res. 2017;33:49–53. doi: 10.1016/j.apnr.2016.09.001. [DOI] [PubMed] [Google Scholar]
- 12.Benedict RH, Wahlig E, Bakshi R, Fishman I, Munschauer F, Zivadinov R. et al. Predicting quality of life in multiple sclerosis: accounting for physical disability, fatigue, cognition, mood disorder, personality, and behavior change. J Neurol Sci. 2005;231(1):29–34. doi: 10.1016/j.jns.2004.12.009. [DOI] [PubMed] [Google Scholar]
- 13.Gong H, Ni CX, Liu YZ, Zhang Y, Su WJ, Lian YJ. et al. Mindfulness meditation for insomnia: A meta-analysis of randomized controlled trials. J Psychosom Res. 2016;89:1–6. doi: 10.1016/j.jpsychores.2016.07.016. [DOI] [PubMed] [Google Scholar]
- 14.Tanay G, Lotan G, Bernstein A. Salutary proximal processes and distal mood and anxiety vulnerability outcomes of mindfulness training: A pilot preventive intervention. Behav Ther. 2012;43(3):492–505. doi: 10.1016/j.beth.2011.06.003. [DOI] [PubMed] [Google Scholar]
- 15.Sedaghat M, Mohammadi R, Alizadeh K, Imani AH. The effect of mindfulness-based stress reduction on mindfulness, stress level, psychological and emotional well-being in Iranian sample. Procedia Soc Behav Sci. 2011;30:929–34. doi: 10.1016/j.sbspro.2011.10.180. [DOI] [Google Scholar]
- 16.Vøllestad J, Sivertsen B, Nielsen GH. Mindfulness-based stress reduction for patients with anxiety disorders: evaluation in a randomized controlled trial. Behav Res Ther. 2011;49(4):281–8. doi: 10.1016/j.brat.2011.01.007. [DOI] [PubMed] [Google Scholar]
- 17.Lovas DA, Barsky AJ. Mindfulness-based cognitive therapy for hypochondriasis, or severe health anxiety: a pilot study. J Anxiety Disord. 2010;24(8):931–5. doi: 10.1016/j.janxdis.2010.06.019. [DOI] [PubMed] [Google Scholar]
- 18.Bogosian A, Hughes A, Norton S, Silber E, Moss-Morris R. Potential treatment mechanisms in a mindfulness-based intervention for people with progressive multiple sclerosis. Br J Health Psychol. 2016;21(4):859–80. doi: 10.1111/bjhp.12201. [DOI] [PubMed] [Google Scholar]
- 19.Nejati S, Esfahani SR, Rahmani S, Afrookhteh G, Hoveida S. The effect of group mindfulness-based stress reduction and consciousness yoga program on quality of life and fatigue severity in patients with ms. J Caring Sci. 2016;5(4):325. doi: 10.15171/jcs.2016.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grossman P, Kappos L, Gensicke H, D'souza M, Mohr D, Penner I. et al. MS quality of life, depression, and fatigue improve after mindfulness training a randomized trial. Neurology. 2010;75(13):1141–9. doi: 10.1212/WNL.0b013e3181f4d80d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Matchim Y, Armer JM, Stewart BR, editors editors. Mindfulness-based stress reduction among breast cancer survivors: a literature review and discussion. Oncol Nurs Forum. 2011;38(2):E61–71. doi: 10.1188/11.ONF.E61-E71. [DOI] [PubMed] [Google Scholar]
- 22.Fjorback L, Arendt M, Ørnbøl E, Fink P, Walach H. Mindfulness‐based stress reduction and mindfulness‐based cognitive therapy–a systematic review of randomized controlled trials. Acta Psychiatr Scand. 2011;124(2):102–19. doi: 10.1111/j.1600-0447.2011.01704.x. [DOI] [PubMed] [Google Scholar]
- 23.Smith B, Metzker K, Waite R, Gerrity P. Short-Form mindfulness-based stress reduction reduces anxiety and improves health-related quality of life in an inner-city population. Holist Nurs Pract. 2015;29(2):70–7. doi: 10.1097/HNP.0000000000000075. [DOI] [PubMed] [Google Scholar]
- 24.Berard JA, Bowman M, Atkins HL, Freedman MS, Walker LA. Cognitive fatigue in individuals with multiple sclerosis undergoing immunoablative therapy and hematopoietic stem cell transplantation. J Neurol Sci. 2014;336(1):132–7. doi: 10.1016/j.jns.2013.10.023. [DOI] [PubMed] [Google Scholar]
- 25.Niazi AK, Niazi SK. Mindfulness-based stress reduction: a non-pharmacological approach for chronic illnesses. N Am J Med Sci. 2011;3(1):20. doi: 10.4297/najms.2011.320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Khanipour H, Borj ali A, Mohanmmad khani P. Effect of Mindfulness-based cognitive therapy on general symptoms of patients with a history of major depression disorder. Clinical Psychology Studies. 2012;7(2):31–50. [Google Scholar]


