Abstract
Background:
The creation of a single patient-reported outcome (PRO) platform validated across hip preservation, osteoarthritis (OA), and total hip arthroplasty (THA) populations may reduce barriers and streamline routine collection of PROs in clinical practice. As such, the purpose of this study was to determine if augmenting the Hip dysfunction and Osteoarthritis Outcome Score, Joint Replacement (HOOS,JR) with addistional HOOS questions would result in a PRO platform that could be used across a wider spectrum of hip patient populations.
Hypothesis:
The HOOS,JR would demonstrate a notable ceiling effect, but that augmenting the HOOS,JR with additional HOOS questions, a responsive PRO platform could be created.
Study Design:
Case series. Level of Evidence: Diagnostic, Level II.
Methods:
Using pre- and postoperative responses to the HOOS questionnaires from a sample of 304 peri-acetabular osteotomy patients, additional items were identified to augment the HOOS,JR. Psychometric properties of newly-created PRO tool (HOOSglobal) were then compared to the HOOS,JR and other PRO instruments developed for hip OA and/or THA patients.
Results:
By augmenting the HOOS,JR with two additional questions, the HOOSglobal was more responsive than all other included PRO tools and had significantly fewer maximum postoperative scores than the HOOS,JR (p<0.0001), HOOS-PS (p<0.0001), WOMAC (p=0.02), UCLA (p=0.0002), and mHHS scores (p=0.04). The postoperative threshold HOOSglobal score associated with patients achieving an acceptable symptom state was 62.5 points.
Conclusion:
The HOOSglobal offers a valid and responsive PRO tool following PAO and may potentially provide the orthopedic community a PRO platform to be used across hip-related subspecialties. For patients undergoing peri-acetabular osteotomy, a postoperative HOOSglobal score ≥ 62.5 was associated with patients achieving an acceptable symptom state.
Keywords: hip, outcome, periacetabular osteotomy, responsiveness, patient-acceptable symptom state
Introduction:
The Hip dysfunction and Osteoarthritis Outcome Score (HOOS) is a 40-item patient-reported outcome (PRO) tool that has provided invaluable information related to subjective pain and function for hip osteoarthritis (OA) and arthroplasty patients.22 However, while the full version of the HOOS allows for the specific domains of Pain, Symptoms, Activities of Daily Living (ADL), Sports and Recreation (Sport), and Quality of Life (QOL), the length of the tool has been a barrier to incorporating routine use into clinical practice. With the impending mandatory physician quality reporting for arthroplasty surgeons, Lyman et al. recently validated the HOOS Joint Replacement, or HOOS, JR.15 Consisting of six items from the full HOOS, the HOOS, JR is an efficient and responsive tool to that provides clinicians with a global score to assess postoperative hip arthroplasty outcomes.15 However, since the HOOS,JR was developed using a cohort of hip arthroplasty patients with an average age of 64 years, it is unlikely that the HOOS,JR would demonstrate similar psychometric properties if administered to younger, more active hip preservation patients.
There are clear advantages of having an efficient, valid and responsive global PRO measure, as meaningful clinical data can be generated with less burden to the patient, surgeon, and clinical staff. Furthermore, efficient global PRO scores may be more easily incorporated into the patient’s electronic health record. Despite these advantages, to date there is no single PRO tool validated for use across hip-related subspecialties. PRO tools originally developed for the total hip arthroplasty (THA) community such as the Harris Hip Score have demonstrated large ceiling effects when administered to hip preservation patients. On the contrary, PRO tools such as the International Hip Outcome Tool (iHOT) and Hip Outcome Score (HOS) have been validated in the hip preservation population but not in the OA or THA population.16, 18 The creation of a single PRO platform validated across hip preservation, OA, and THA populations may reduce barriers and streamline routine collection of PROs in clinical practice. As such, the purpose of this study was to develop a PRO platform by augmenting the HOOS, JR with additional questions from the full version of the HOOS, and to assess the validity and responsiveness of this tool in a hip preservation patient population. We hypothesized that when administered to a hip preservation patient population, the augmented HOOS, JR (termed the HOOSglobal) would demonstrate superior psychometric properties when compared to the HOOS, JR and other PRO tools that were originally developed for the OA and/or THA communities.
Methods:
Patients
From an IRB-approved, multicenter prospective cohort (Academic Network of Conservational Hip Outcomes Research (ANCHOR), Washington University IRB protocol #201107167), we identified 304 consecutive peri-acetabular osteotomy (PAO) patients (283 females, 61 males, age = 24.7 ± 9.4 years) with minimum 1-year follow-up and complete pre- and postoperative PRO data. All patients underwent PAO for hip dysplasia, with a subset having concomitant procedures to address cam (n = 16), pincer (n = 2), or combined deformity (n = 3). We included all PAO patients that had consented to participate in the study protocol, and patients were not excluded based on age, sex, race, or the presence of concomitant injury. In addition to the HOOS, patients routinely completed UCLA Activity Scale32 and modified Harris Hip Score (mHHS)25 questionnaires both prior to and following surgery. From the full version of the HOOS, the HOOS, JR,15 HOOS-Physical Function Shortform (HOOS-PS),6 and Western Ontario and MacMaster Universities Arthritis Index (WOMAC)3 were calculated.
Item selection
To develop the HOOSglobal, we first identified individual items from the HOOS that were not included in the HOOS, JR for which a percentage of patients reported persistent postoperative difficulty. Items with <33% of patients with postoperative responses of “none” were selected for possible inclusion in the HOOSglobal meaning that at least two-thirds of patients continue to report pain or difficulty with that item at a minimum of one year after PAO. This was done to ensure the face and content validity of the HOOSglobal. We included only those items for possible inclusion for which a relatively high percentage of patients reported continued pain or difficulty one year after PAO. Items that relatively few patients reported pain or difficulty would not discriminate between patients with a poor or good outcome and by eliminating such items, the face and content validity of the HOOSglobal would be maintained. Once potential additional items were identified, we applied a Rasch measurement model to the stacked dataset using both the HOOS, JR and HOOSglobal.24, 28, 29 Because each item has its own distinct set of category descriptors, the analysis was conducted using the Rasch Partial Credit model available in Winsteps Rasch Measurement Software version 3.81.0 (Winsteps, Beaverton, OR).17, 30 Details regarding the methods used in the Rasch analysis, item inclusion and exclusion, and comparative results of the HOOS,JR and HOOSglobal can be found in the accompanying electronic Supplemental files.
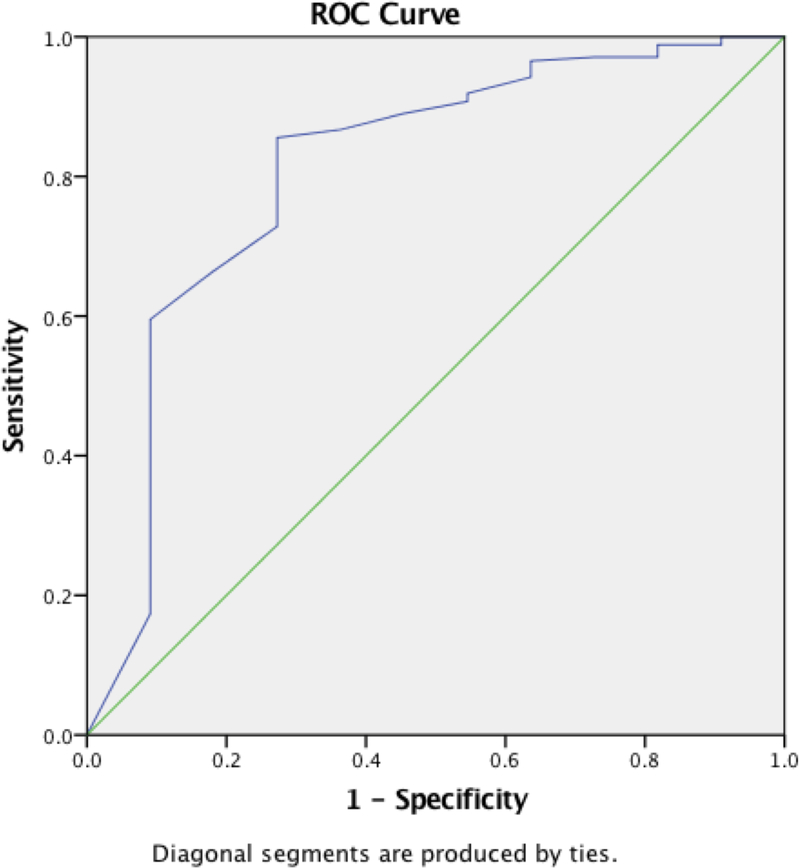
We then calculated the HOOSglobal score associated with a Patient-Acceptable Symptom State (PASS). The PASS represents the postoperative threshold value of a given PRO instrument that is associated with the majority of patients with postoperative scores above the PASS threshold are satisfied with their surgical procedure.9 To do so, we employed methods similar to those recently used to calculate the PASS for the International Knee Documentation Committee (IKDC) subjective knee form and Knee injury and Osteoarthritis Outcome Score (KOOS) after anterior cruciate ligament reconstruction.19 At the most recent postoperative follow-up visit, patients were asked if they were satisfied with their hip surgery with the options of either “Yes” or “No.” We then utilized a Receiver Operator Characteristic (ROC) curve to determine if a PASS threshold for the HOOSglobal could be identified. The PASS threshold was determined by calculating the Youden index,31 which is product of the sensitivity and specificity for a given outcome score, and the PASS threshold was the combination of sensitivity and specificity with the greatest Youden index.
Comparison of the HOOSglobal, HOOS,JR, and other hip PRO instruments
The responsiveness and the presence of floor and ceiling effects with the HOOSglobal in comparison to the HOOS, JR and other PRO tools were then evaluated using the previously described methods.10 The responsiveness of the HOOSglobal was also assessed by determining if the HOOSglobal was able to detect expected differences between patients’ pre- and postoperative scores. Responsiveness has been defined as a PRO tool’s ability to detect meaningful or clinically important changes.11 Responsiveness was assessed using three commonly used methods: effect size (ES), standardized response mean (SRM), and relative efficiency (RE).10, 12, 23 ES is the mean pre- to postoperative change divided by the standard deviation of the preoperative scores, and ES > 0.8 are considered large.5, 10 SRM is the pre- to postoperative change divided by the standard deviation of the change scores for that particular PRO tool,11, 12 and SRM is interpreted similarly to ES, with values > 0.8 considered large. The RE represents a ratio of the pre- to postoperative t-statistics of the HOOSglobal and each of the other PRO tools [RE = (tKOOSglobal/tother PROs)2].11, 12 RE values > 1 are indicative of the HOOSglobal being more responsive than the other PRO tools. The presence of a floor or ceiling effect was defined using the threshold of 15% of patients reporting either the worst possible or best possible scores, respectively.13 A ceiling effect is present when more than 15% of the sampled patients report the best possible score, and conversely, a floor effect is present when more than 15% of the sampled patients demonstrate the worst possible score. Neither floor and ceiling effects are ideal as both are indicative of a scoring system that can either not discriminate between an extremely poor result and a poor result (floor effect) or between an excellent and good result (ceiling effect). We have previously observed marked postoperative ceiling effects with OA and/or THA-based PRO tools in this patient population, and one-tailed chi-square tests were used to determine if the prevalence of maximum possible HOOSglobal postoperative scores differed from the other PRO tools included in this study (HOOS, JR, HOOS-PS, WOMAC, UCLA, and mHHS).
Results:
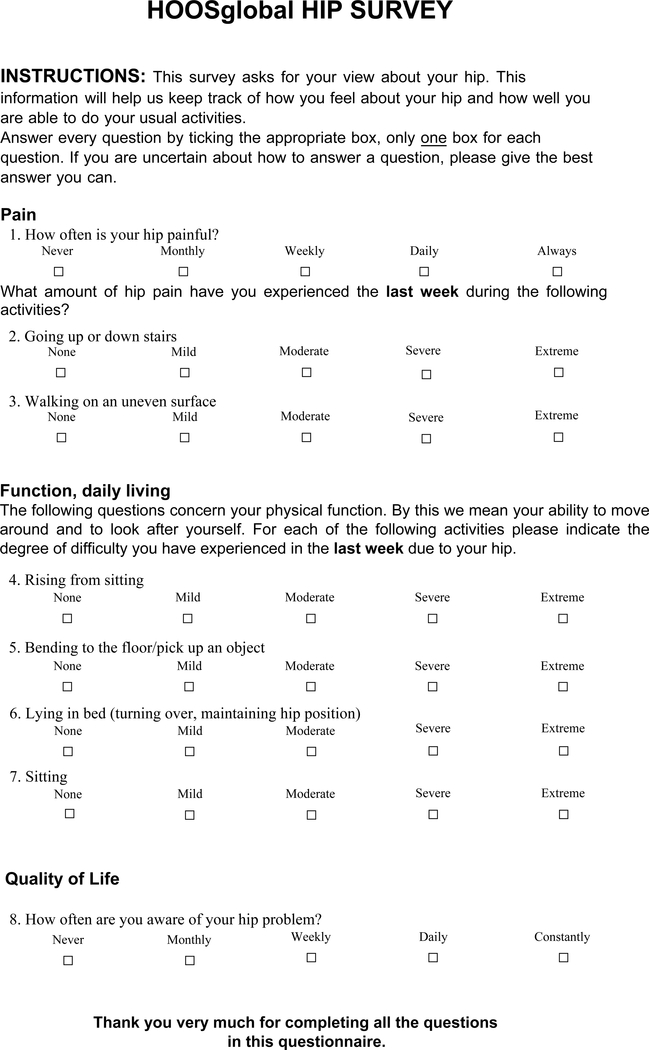
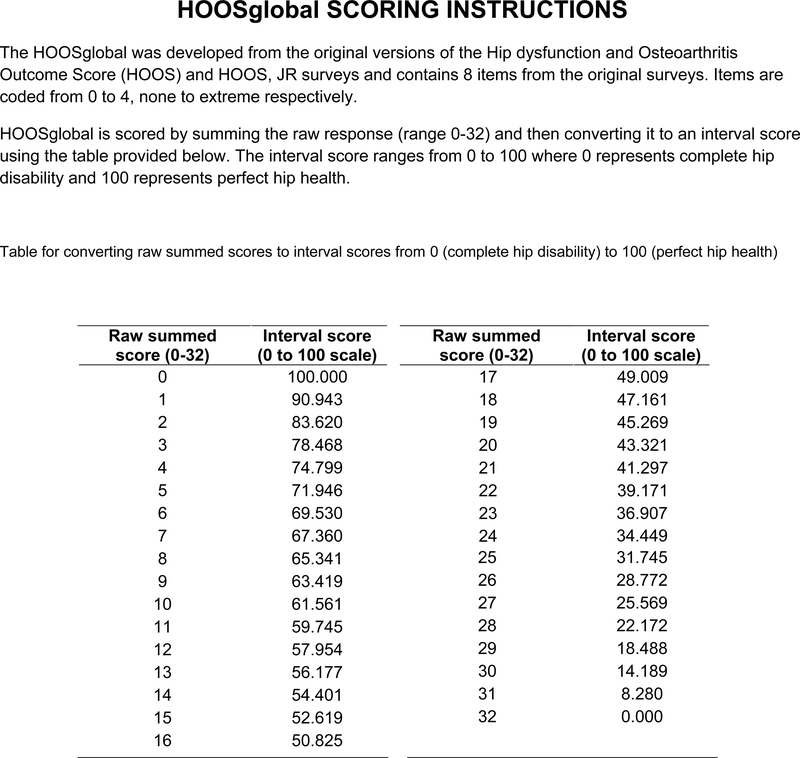
Based on the item selection methods and Rasch anslysis results, two additional items were identified from the full version of the HOOS that met the criteria for inclusion in the HOOSglobal: question P1: “How often is your hip painful?”, and question Q1: “How often are you aware of your hip?” The raw HOOSglobal score was then determined by summing the responses to the original six HOOS, JR items and questions P1 and Q1. The scaled HOOSglobal score was determined using the logit conversion table and detailed results of the Rasch analyses, HOOSglobal questionnaire, and scoring instructions can be found in the Supplemental Files available on the journal’s website.
At mean follow-up of 4.0 ± 1.5 years, HOOSglobal and all other PROs significantly improved from the preoperative visit (Tables 1, 2). While all PRO tools including the HOOSglobal exceeded the 15% threshold for ceiling effects (HOOSglobal had a 16% prevalence of maximum scores), the HOOSglobal had significantly fewer maximum postoperative scores than the HOOS, JR (p < 0.0001), HOOS-PS (p < 0.0001), WOMAC (p = 0.02), UCLA (p = 0.0002), and mHHS scores (p = 0.04, Table 1). A subset of 184 patients completed the postoperative satisfaction question, with 173 (94%) reported being satisfied with their procedure and 11 were not satisfied (6%). The PASS threshold score for HOOSglobal was 62.5 (ROC curve Area Under Curve (AUC) = 0.81 [95% CI: 0.66, 0.96], p = 0.001), with sensitivity = 0.86 and specificity = 0.73 (Figure 1).
Table 1.
Comparison of pre- and postoperative patient-reported outcome tools
| Instrument | Preoperative | Postoperative | Preoperative Floor Effect (n, %)* |
Postoperative Ceiling Effect (n, %)* |
Pre/post t statistic† |
Pre/post p value |
Effect size |
Standardized Response Mean |
Relative Efficiency‡ |
|---|---|---|---|---|---|---|---|---|---|
| HOOSglobal | 52.1 ± 14.6 | 74.5 ± 17.8 | 2 (<1%) | 49 (16%) | 20.96 | 1.5 | 1.2 | - | |
| HOOS, JR | 62.3 ± 18.6 | 84.2 ± 17.0 | 2 (<1%) | 110 (36%) | 19.5 | 1.2 | 1.1 | 1.16 | |
| HOOS-PS | 68.1 ± 19.3 | 87.3 ± 14.4 | 2 (<1%) | 90 (30%) | 16.8 | 1.0 | 1.0 | 1.56 | |
| WOMAC | 66.3 ± 21.0 | 88.1 ± 15.9 | 1 (<1%) | 70 (23%) | 18.76 | 1.0 | 1.0 | 1.25 | |
| UCLA | 6.9 ± 2.5 | 7.4 ± 2.3 | 1 (<1%) | 86 (28%) | 3.19 | 0.2 | 0.2 | 43.17 | |
| mHHS | 61.7 ± 16.3 | 84.7 ± 15.7 | 1 (<1%) | 66 (22%) | 20.05 | 1.4 | 1.0 | 1.09 | |
All outcome tools exceeded the 15% ceiling effect threshold postoperatively; however, the HOOSglobal had significantly fewer maximum scores postoperatively than the other PRO tools (p < 0.04 for all paired comparisons)
All outcome score significantly improved from the pre- to postoperative period (p < 0.01)
Relative to the HOOSglobal, and Relative Efficiency values > 1 indicated greater responsiveness of the HOOSglobal
Table 2.
Pre- and postoperative results of the five HOOS subscale scores (Symptom, Pain, Activities of Daily Living (ADL), Sports, and Quality of Life (QOL))
| Instrument | Preoperative | Postoperative | Preoperative Floor Effect (n, %)* |
Postoperative Ceiling Effect (n, %)* |
Pre/post t statistic† |
Effect size |
Standardized Response Mean |
|---|---|---|---|---|---|---|---|
| Symptom | 59.2 ± 19.2 | 78.4 ± 18.2 | 0 (0%) | 56 (18%) | 16.02 | 1.0 | 1.0 |
| Pain | 56.6 ± 20.5 | 83.7 ± 18.3 | 2 (<1%) | 65 (21%) | 21.68 | 1.3 | 1.2 |
| ADL | 68.4 ± 22.1 | 89.4 ± 15.8 | 2 (<1%) | 101 (33%) | 17.26 | 1.0 | 1.0 |
| Sport | 47.1 ± 25.5 | 76.5 ± 23.7 | 10 (3%) | 86 (28%) | 17.63 | 1.2 | 1.0 |
| QOL | 35.9 ± 22.4 | 70.9 ± 25.7 | 21 (7%) | 61 (20%) | 21.99 | 1.6 | 1.3 |
All HOOS subscales exceeded the 15% ceiling effect threshold postoperatively
All HOOS subscale scores significantly improved from the pre- to postoperative period (p < 0.001)
Figure 1.
HOOSglobal hip survey.
Discussion:
The purpose of this study was to develop a PRO platform by augmenting the HOOS, JR with additional questions from the full version of the HOOS, and to compare the validity and responsiveness of this tool to other PRO tools in a hip preservation patient population. The results by and large supported our hypothesis that the HOOSglobal would demonstrate superior psychometric properties when compared to the HOOS, JR and other PRO tools that were originally developed for the OA and/or THA communities. By adding two additional items related to how often the patient has pain in the involved hip and how often the patient is aware of the hip significantly lessened the prevalence of patients with perfect postoperative scores. The HOOS, JR provides surgeons with a valid and efficient method to quantify postoperative outcomes following hip arthroplasty15; however, the HOOS, JR does not appear to be appropriate for use with hip preservation patient populations who have undergone periacetabular osteotomy surgery as a large ceilings effect was noted. This finding was not unique to the HOOS, JR as large ceiling effects were also present for the HOOS-PS, WOMAC, UCLA, mHHS and the five HOOS subscales after PAO. Not only did the HOOSglobal alleviate some of the psychometric limitations of other OA-based PRO instruments, interpretation of HOOSglobal results can be put in clinical context with postoperative scores ≥ 62.5 were associated with patients achieving an acceptable symptom state.
These tools were initially created and validated largely in hip OA and THA patients1, 3, 7, 22 and have proven to be effective measurement options for their target patient populations. Our results are similar to other previous reports that have also questioned the use of OA-related PRO instruments in populations of hip preservation patients. In a systematic review, Lodhia et al. reported notable ceiling effects with the WOMAC when used with femoroacetabular impingement and labral pathology.14 Similarly, Aprato et al. reported that 14% of patients with good to excellent modified Harris Hip Scores one year after hip arthroscopy were dissatisfied with their outcome,2 which could have been the result of a ceiling effect in this younger, more active patient population.
The goal of this work was not to supplant the HOOS, JR but rather to build upon it to reduce barriers to routine PRO collection in the clinical setting. The principal advantage of using the HOOSglobal as a PRO platform is the versatility to be used across a variety of hip patient populations, thus reducing some of the burden to the orthopedic practice associated with routine PRO collection. The eight HOOSglobal questions can be scored differently for different patient subsets. All eight questions can be used to generate a HOOSglobal for hip preservation patients while the original six HOOS, JR questions can be scored for late stage OA and/or THA patients. Unlike the current available methods of using multiple PRO tools for hip preservation and arthroplasty subsets of patients, front office staff would not need to differentiate which hip PRO questionnaire to give an individual patient. For example, the front office staff for a clinician that normally sees both preservation and OA patients during the course of a clinic day would not have to determine which PROM tool to give each patient, but rather, could use the HOOSglobal for adult hip patients. Similarly, being able to use the HOOSglobal could alleviate the complexities of collecting hip-related PROs in multi-subspecialty practices. Perhaps most importantly, the eight questions of the HOOSglobal take less than five minutes to complete, thereby minimizing the burden to the patient as well as reducing the likelihood that PRO collection will dramatically alter patient flow during the course of an average clinic day.
While the HOOSglobal may offer a single platform to reduce barriers to routine clinical PRO collection, we are not suggesting that this tool is a “silver bullet.” The HOOSglobal significantly reduced the prevalence of perfect postoperative scores when compared to OA/THA PRO tools, the 16% prevalence of perfect scores was above the 15% ceiling effect threshold. As such, future studies are necessary to determine if the HOOSglobal is an acceptable alternative to hip preservation-specific instruments, especially in athletic hip arthroscopy patients. Recommended PRO tools are available through the AAOS website; however, while the HOOS and HOOS, JR have been recommended for use with hip OA patients,26 the AAOS has not given guidance as to what tool(s) are best suited for the assessment of patients prior to and following hip preservation procedures. Multiple tools exist, including the International Hip Outcome Tool (iHOT),18 the Hip Outcome Score (HOS),20 Nonarthritic Hip Score (NAHS),4 the Hip Sports Activity Scale (HSAS),21 and the Copenhagen Hip and Groin Outcome Score (HAGOS),27 Core Outcome Measures Index – Hip (COMI-Hip),8 among others. While these have been utilized in the hip preservation literature, there is limited head-to-head comparative information related to the clinimetric and psychometric properties of these instruments. Also, it remains unclear if these hip preservation-specific tools could be utilized as patients transition from hip preservation to OA to arthroplasty, as they have not been validated in the OA or arthroplasty populations.
This study was not without limitation. First, an a priori power analysis was not performed as part of this study. Rather, we used liberal inclusion and exclusion criteria to ensure that the development of the HOOSglobal could be generalized to the broad PAO patient population. There is potential for a selection bias in that the study was performed with patients that elected to participate in a research study; however, because of the liberal inclusion/exclusion criteria there was little opportunity for selection bias on behalf of the researchers. Second, hip preservation-specific PRO instruments were not included as part of this multicenter prospective cohort. As such, we were unable to directly compare the responsiveness between OA- and hip preservation-specific PRO instruments. At the time that the multicenter registry was initiated, the psychometric properties of hip preservation-specific PRO tools had not yet been fully vetted, and since one of the primary goals of the registry is to evaluate long-term outcomes and the progression to OA, OA-based PRO tools were utilized. Third, the HOOSglobal was used in a PAO population in the current study and the HOOS, JR has been validated in the THA population. While these two patient populations represent the “anchors” on the continuum of post-traumatic osteoarthritis, the validity of the HOOSglobal platform has not been evaluated in either those with mild to moderate hip osteoarthritis or potentially younger and more active hip arthroscopy and/or FAI patient populations. Future studies are necessary to assess the test-retest reliability of the HOOSglobal and to determine if the current results are generalizable to additional patient groups.
In conclusion, the HOOS, JR and other OA-based PRO instruments demonstrated large ceiling effects in a hip preservation population following PAO. While we can conclude that OA-based PRO tools may not be the most appropriate method to quantify outcomes after hip preservation procedures due to the large ceiling effects that were observed, by including two additional HOOS questions, the HOOSglobal offers a valid and responsive PRO tool following PAO and may potentially provide the orthopedic community a PRO platform to be used across hip-related subspecialties. Finally, postoperative HOOSglobal scores ≥ 62.5 were associated with patients achieving an acceptable symptom state.
Supplementary Material
Figure 2.
HOOSglobal scoring instructions.
Figure 3.
Receiver Operator Characteristic (ROC) curve used to determine the postoperative HOOSglobal score threshold associated with postoperative patient satisfaction
What is known about the subject:
The HOOS, JR offers an efficient method to evaluate postoperative outcomes following THA; however, the ability to utilize this PROM tool in younger, more active hip preservation patient population has not been determined.
What this study adds to the existing knowledge:
The HOOS, JR is not a valid or responsive tool to assess patient-reported outcomes following peri-acetabular osteotomy; however, an aggregate score combining HOOS, JR with the 2 additional HOOS questions, was valid and responsive in this patient population.
Acknowledgments
Disclosure: This work was supported in part by Award UL1RR024992 from the National Center for Research Resources (J.C.C.). It was also supported in part by the Curing Hip Disease Fund (J.C.C.), the ANCHOR Research Fund, Smith & Nephew (J.C.C.), and the NFL Charities (J.C.C.)
Footnotes
ANCHOR Study Group Members who contributed to this article
Paul E. Beaulé, MD, FRCSC, Young-Jo Kim, MD, PhD, Michael B. Millis, MD, David A. Podeszwa, MD, Perry L. Schoenecker, MD, Rafael J. Sierra, MD, Ernest L. Sink, MD, Daniel J. Sucato, MD, Robert T. Trousdale, MD, and Ira Zaltz, MD
This study was performed at the University of Kentucky
References
- 1.Amstutz HC, Thomas BJ, Jinnah R, Kim W, Grogan T, Yale C. Treatment of primary osteoarthritis of the hip: a comparison of total joint and surface replacement arthroplasty. J Bone Joint Surg (Am). 1984;66:228–241. [PubMed] [Google Scholar]
- 2.Aprato A, Jayasekera N, Villar RN. Does the modified Harris hip score reflect patient satisfaction after hip arthroscopy? Am J Sports Med. 2012;40(11):2557–2560. [DOI] [PubMed] [Google Scholar]
- 3.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: A health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapies in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 4.Christensen CP, Althausen PL, Mittleman MA, Lee JA, McCarthy JC. The nonarthritic hip score: reliable and validated. Clin Orthop Related Res. 2003;406:75–83. [DOI] [PubMed] [Google Scholar]
- 5.Cohen J Statistical power analysis for the behavioral sciences. Vol 2nd Hillsdale, NJ: Lawrence Earlbaum Associates; 1988. [Google Scholar]
- 6.Davis AM, Perruccio AV, Canizares M, et al. The development of a short measure of physical function for hip OA HOOS-Physical Function Shortform (HOOS-PS): an OARSI/OMERACT initiative. Osteoarthritis Cartilage. 2008;16(5):551–559. [DOI] [PubMed] [Google Scholar]
- 7.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg (Am). 1969;51:737–755. [PubMed] [Google Scholar]
- 8.Impellizzeri FM, Mannion AF, Naal FD, Leunig M. Validation of the Core Outcome Measures Index in patients with femoroacetabular impingement. Arthroscopy. 2015;31(7):1238–1246. [DOI] [PubMed] [Google Scholar]
- 9.Kvien TK, Heiberg T, Hagen KB. Minimal clincally important improvement/difference (MCII/MCID) and the patient acceptable symptom state (PASS): what do these concepts mean? Ann Rheum Dis. 2007;66(suppl 3):iii40–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lam ETP, Lam CLK, Fong DYT, Huang WW. Is the SF-12 version 2 health survey a valid and equivalent substitute for the SF-36 version 2 health survey for the Chinese? J Eval Clin Pract. 2013;19:200–208. [DOI] [PubMed] [Google Scholar]
- 11.Liang MH. Longitudinal construct validity: establishment of clinical meaning in patient evaluative instruments. Medical Care. 2000;38:1184–1190. [PubMed] [Google Scholar]
- 12.Liang MH, Larson MG, Cullen KE, Schwartz JA. Comparative measurement efficiency and sensitivity of five health status instruments for arthritis research. Arthritis Rheum. 1985;28(5):542–547. [DOI] [PubMed] [Google Scholar]
- 13.Lim CR, Harris K, Dawson J, Beard D, Fitzpatrick R, Price AJ. Floor and ceiling effects in the OHS: an analysis of the NHS PROMs data set. BMJ Open. 2015;5:e007765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lodhia P, Slobogean GP, Noonan VK, Gilbart MK. Patient-reported outcome instruments for femoroacetabular impingement and hip labral pathology: a systematic review of the clinimetric evidence. Arthroscopy. 2011;27(2):279–286. [DOI] [PubMed] [Google Scholar]
- 15.Lyman S, Lee Y-Y, Franklin PD, Li W, Mayman DJ, Padgett DE. Validation of the HOOS, JR: A short-form hip replacement survey. Clin Orthop Related Res. 2016;474:1472–1482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Martin RL, Kelly BT, Philippon MJ. Evidence of validity for the hip outcome score. Arthroscopy. 2006;22(12):1304–1311. [DOI] [PubMed] [Google Scholar]
- 17.Masters GN. A Rasch Model for partial credit scoring. Psychometrika. 1982;47(2):149–174. [Google Scholar]
- 18.Mohtadi NG, Griffin DR, Pedersen ME, et al. The development and validation of a self-administered quality-of-life outcome measure for young, active patients with symptomatic hip disease: the International Hip Outcome Tool (iHOT-33). Arthroscopy. 2012;28(5):595–605. [DOI] [PubMed] [Google Scholar]
- 19.Muller B, Yabroudi MA, Lynch A, et al. Defining thresholds for the patient acceptable symptom state for the IKDC subjective knee form and KOOS for patients who underwent ACL reconstruction. Am J Sports Med. 2016;44(11):2820–2826. [DOI] [PubMed] [Google Scholar]
- 20.Naal FD, Impellizzeri FM, Miozzari HH, Mannion AF, Leunig M. The German Hip Outcome Score: validation in patients undergoing surgical treatment for femoroacetabular impingement. Arthroscopy. 2011;27(3):339–345. [DOI] [PubMed] [Google Scholar]
- 21.Naal FD, Miozzari HH, Kelly BT, Magennis EM, Leunig M, Noetzli HP. The Hip Sports Activity Scale (HSAS) for patients with femoroacetabular impingement. Hip Int. 2013;23(2):204–211. [DOI] [PubMed] [Google Scholar]
- 22.Nilsdotter A-K, Lohmander LS, Klassbo M, Roos EM. Hip disability and osteoarthritis outcome score (HOOS)--validity and responsiveness in total hip replacement. BMC Musculoskeletal Disorders. 2003;4:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nilsdotter A-K, Roos EM, Westerlund JP, Roos HP, Lohmander LS. Comparative responsiveness of measures of pain and function after total hip replacement. Arthritis Care & Research. 2001;45:258–262. [DOI] [PubMed] [Google Scholar]
- 24.Rasch G Probabilistic Models for Some Intelligence and Attainment Tests. Copenhagen, Denmark: Danish Institute for Educational Research; 1960. [Google Scholar]
- 25.Shamra S, Shah R, Draviraj KP, Bhamra MS. Use of telephone interviews to follow up patients after total hip replacement. J Telemedicine and Telecare. 2005;11:211–214. [DOI] [PubMed] [Google Scholar]
- 26.Surgeons AAoO. Patient Reported Outcome Measures. Accessed 12/7/2016.
- 27.Thorborg K, Holmich P, Christensen R, Petersen J, Roos EM. The Copenhagen Hip and Groin Outcome Score (HAGOS): development and validation according to the COSMIN checklist. Br J Sports Med. 2011;45(6):478–491. [DOI] [PubMed] [Google Scholar]
- 28.Wright BD. Time 1 to Time 2 (Pre-test to Post-test) comparison: Racking and Stacking. Rasch Measurement Transactions. 1996;10(1):478. [Google Scholar]
- 29.Wright BD. Rack and Stack: Time 1 vs. Time 2 or Pre-Test vs. Post-Test. Rasch Measurement Transactions. 2003;17(1):905–906. [Google Scholar]
- 30.Wright BD, Masters GN. Rating Scale Analysis. Chicago, IL: MESA Press; 1982. [Google Scholar]
- 31.Youden WJ. Index for rating diagnostic tests. Cancer. 1950;3(1):32–35. [DOI] [PubMed] [Google Scholar]
- 32.Zahiri CA, Schmalzried TP, Szuszczewicz ES, Amstutz HC. Assessing activity in joint replacement patients. J Arthroplasty. 1998;13(8):890–895. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.