Abstract
Introduction
Cone-beam computed tomography (CBCT) is considered to be the most informative radiographic method for pre- and postoperative analysis of the maxillary anatomy and for avoiding further complication. Canalis sinuosus is one of such structures that damage can go along with bleeding and neurological symptomatology. The aim of the study was to investigate radiological and morphometric features of the canalis sinuosus in Russian population using CBCT technique.
Materials and Methods
150 CBCT scans of 61 males and 89 females aged from 24 to 80 years were retrospectively studied with different slice thickness and evaluated with regards to prevalence and diameter among age and gender groups in Russia.
Results
CS prevalence in this study was 67%, and CS was most frequently presented in the lateral incisor region (33.5%). Women showed statistically higher CS prevalence (p < 0.01) than the male group, and there was no statistically significant difference observed between occurrence and localization of CS and age groups.
Conclusion
CBCT examination demonstrated good diagnostic efficiency in CS visualization, and the CS may have variations on its location and prevalence with statistically significant differences between the gender group and without significant differences among age groups and can depend on the population.
1. Introduction
Dental implant placement in the anterior maxilla is a medium or high complexity challenge and requires careful preoperative planning [1]. Two-dimensional radiographic techniques have multiple limitations for such cases that is why cone-beam computed tomography (CBCT) is considered to be the most informative radiographic method for performing comprehensive pre- and postoperative analysis of the maxillary anatomy and, consequently, for avoiding further complication [2–5].
The significant variability in maxillary neovascularization and high trabecular anterior maxilla density emphasizes the importance of three-dimensional diagnostics and avoiding this method poses a risk for bleeding and neurological symptomatology [6, 7].
One of such structures, that damage can go along with these complications, is canalis sinuosus (CS) [8]. CS is an intrabony structure that carries the anterior superior alveolar nerve and vessels. For example, Machado et al. [9] presented two case reports where patients suffered from pain and it immediately relieved after implant extractions that were placed with CS damaging.
The recent systematic literature review of CS [6] studies showed that the terminal portion of CS is more prevalent in the anterior region of the maxilla, more specifically in the incisor and canine region near the palate [10–14], and that locations can be favourable positions for better dental implant anchoring and esthetic outcomes in the anterior maxilla [1]. However, as the literature review showed there is no CBCT or other studies of CS in Russia where dental practitioners still use the data obtained from foreign authors.
The aim of this study was to investigate radiological and morphometric features of the canalis sinuosus in Russian population using CBCT technique.
2. Materials and Methods
150 CBCT scans of 61 males and 89 females aged from 24 to 80 years (mean age is 63.27 ± 6.8) with 10 × 8.5 field of view were retrospectively studied, who attended the radiologic diagnostic center for three-dimensional radiological scanning for different diagnostic purposes. Written consent was signed by all individuals before taking the procedure. The CBCT device had the following characteristics: 0.2 mm/0.3 mm voxel size; 0.5 mm focal spot; 18 sec scanning time; and 55–99 kB/4–16 mA tube voltage.
The following exclusion criteria were used: the presence of a supernumerary or retained tooth in the anterior maxilla, the presence of a pathological or traumatic lesion in this region, patients who had previously undergone a surgical procedure in the maxilla, and the presence of technical artefacts.
Firstly, the scans were analyzed in Ez3D Plus (Vatech Co., Korea, 2009), software on panoramic and cross-sectional views with 0.5 mm, 1 mm, 3 mm, and 10 mm slice thicknesses. CS was identified according to its description in the literature [9].
Secondly, mesiodistal location according to the Oliveira-Santos et al. classification [15] and facial-palatal location were determined. The prevalence and location were analyzed with regards to age: young group (24–44 years), middle age (45–59 years), and elderly (60 years and more) and gender groups using one-way ANOVA test with StatPlus 6 (AnalystSoft).
3. Results
The slice thickness of CBCT scans was sequentially changed from 0.5 mm to 1 mm to 3 mm and to 10 mm. CS on images with different slice thicknesses was evaluated separately (Figure 1).
Figure 1.
CS with different slice thicknesses in the same patient: (a) 0.5 mm, (b) 1 mm, (c) 3 mm, and (d) 10 mm. Note that CS is almost visualized with 3 mm and 10 mm slice thicknesses.
Then, CS visualization was graded with the four-point rating scale. This method was precisely and comprehensively described by Jacobs et al. [16] while evaluating the mandibular incisive canal with CBCT. This method showed that the optimal visualization of CS was reached with 0.5 mm/1 mm slice thickness (Figure 2).
Figure 2.
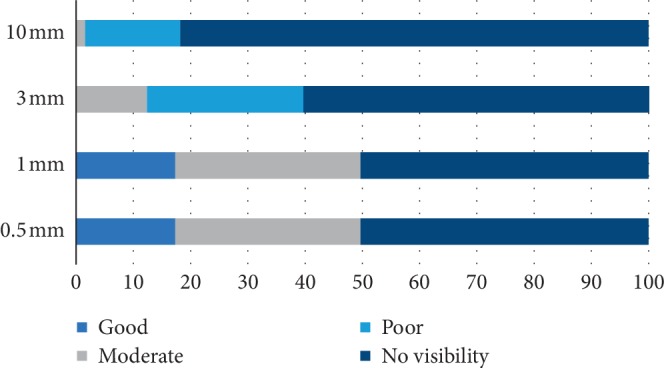
CS visualization with the four-point rating scale: no visibility—important structures are not visualized; poor—important structures are not diagnostic; moderate—important structures are diagnostic but could be improved; good—important structures are optimally visualized.
Evaluating CBCT scans with 1 mm slice thickness, the alveolar process part of CS was evident in 101 of 150 patients (67% of total patients). 22 of these 101 patients (21.7%) presented with CS only on the right side, 33 (32.6%) patients only on the left side, and 47 (45.7%) patients on both sides. In total, 149 CS were identified on both sides with 0.5 mm slice thickness and CS was presented in 46% on the right side (22 + 47 of total 149 canals) and 54% on the left side (32 + 47 of total 149 canals) and this difference was not statistical (p=0.6).
Data on CS localization according to Oliveira-Santos et al. and facial-palatal localization are shown in Tables 1 and 2 consequently. Most often CS was located in the lateral incisor region and palatally. In addition, statistically more (p < 0.01) female persons presented CS compared to the male group. However, there was no statistically significant difference between age groups (p=0.8).
Table 1.
CS localization according to Oliveira-Santos et al.
| No | Region | Total % (n) | Gender % (n) | Age % (n) | |||
|---|---|---|---|---|---|---|---|
| Male | Female | 24–44 | 45–60 | 60 and more | |||
| 1 | Central incisor | 24.2 (36) | 8.7 (13) | 15.4 (23) | 7.3 (11) | 6.7 (10) | (15) |
| 2 | Between central and lateral incisors | 10.7 (16) | 5.3 (8) | 5.3 (8) | 4 (6) | 2 (3) | (7) |
| 3 | Lateral incisor | 33.5 (50) | 13.4 (20) | 20.1 (30) | 10.7 (16) | 10 (15) | (19) |
| 4 | Canine | 21.5 (32) | 9.3 (14) | 12 (18) | 11.4 (17) | 4.6 (7) | (8) |
| 5 | First premolar | 9.4 (14) | 2.6 (4) | 6.7 (10) | 6 (9) | 2 (3) | 1.3 (2) |
| 6 | Lateral to incisive foramen | 0.7 (1) | 0.7 (1) | 0 | 0.7 (1) | 0 | 0 |
| 7 | Posterior to incisive foramen | 0 (0) | 0 | 0 | 0 | 0 | 0 |
| 40.2 (60) | 59.8 (89) | 40.2 (60) | 25.5 (38) | 34.3 (51) | |||
Table 2.
CS localization regarding to facial-palatal position.
| No | Position | Total % (n) | Gender % (n) | Age % (n) | |||
|---|---|---|---|---|---|---|---|
| Male | Female | 24–44 | 45–60 | 60 and more | |||
| 1 | Facial | 12 (18) | 4 (6) | 8 (12) | 0.7 (1) | 5.3 (8) | 6.1 (9) |
| 2 | Central | 12 (18) | 6.7 (9) | 5.3 (9) | 7.3 (11) | 4.1 (6) | 0 |
| 3 | Palatal | 76 (113) | 30 (45) | 46 (68) | 32 (48) | 16.7 (25) | 26.8 (40) |
4. Discussion
It is extremely important that the professional has knowledge about the trajectory and caliber of the CS, aiming at the prevention of injury during dental procedures that surround it [6]. Several studies and clinical cases showed that CBCT is the best radiographic technique for CS visualization [6]. CBCT application is recommended to identify CS and understand its location, diameter, length, and variation, avoiding possible iatrogenic complications in the implant site or other surgical procedures involving the anterior maxilla [17].
However, several studies demonstrated different conclusions on the dependence of the slice thickness of CBCT scans and the detection of the anatomical and other structures, as well as the way that reduces artefacts [18–24]. Our choice of slice thickness was 1 mm for good and moderate detection of CS without missing it and with high reduction of artefacts in this case.
Ferlin et al. [6] showed that the prevalence of CS in different populations using different study methods ranged from 52.1% to 100% of samples. Our study of Russian population revealed 67% of CS prevalence. This prevalence was close to a German study (67.6%) by Ghandourah et al. [13] and Turkish study (70.8%) by Orhan et al. [14].
Similar to other studies, this study of Russian population showed that there was no statistically significant difference with regards to the side. In addition, CS was most frequently presented in the lateral incisor region (33.5%), central incisor region (24.2%), and canine region (21.5%) and near the palate that makes its localization regarding to different directions close to other populations [6].
Gurler et al. [10] and von Arx et al. [11] noted that men showed a higher prevalence in relation to CS, but without statistically significant differences, as well as Machado et al. [9] who found an increased prevalence of males over females, but in our Russian population the study women showed statistically higher CS prevalence (p < 0.01) than the male group with the same tendency of CS localization described above.
There was no statistically significant difference observed between occurrence and localization of CS and age groups. Orhan et al. [14] in the Turkish group and Ghandourah et al. [13] in the German population observed higher prevalence of CS in older age groups in comparison with young adults, and our study showed higher prevalence in the young group (32%).
5. Conclusion
CBCT examination demonstrated good diagnostic efficiency in CS visualization (67%). In addition, this study showed the importance of slice thickness choice for CS visualization. The best visualization was reached with 0.5 mm and 1 mm slice thicknesses. The results of the Russian population study allow us to conclude that the CS may have variations on its location and prevalence with statistically significant differences between the gender group and without significant differences among age groups and can depend on the particular population.
Acknowledgments
The publication has been prepared with the support of the “RUDN University Program 5–100.”
Data Availability
The data used to support the findings of this study are included within the article.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
References
- 1.Belser U., Martin W. ITI Treatment Guide: Implant Therapy in the Esthetic Zone: Single-Tooth Replacement. Vol. 1. Berlin, Germany: Quintessence Publishing; 2010. [Google Scholar]
- 2.Maestre-Ferrín L., Galán-Gil S., Carrillo-García C., Peñarrocha-Diago M. Radiographic findings in the maxillary sinus: comparison of panoramic radiography with computed tomography. The International Journal of Oral & Maxillofacial Implants. 2011;26(2):341–346. [PubMed] [Google Scholar]
- 3.Baciut M., Hedesiu M., Bran S., Jacobs R., Nackaerts O., Baciut G. Pre- and postoperative assessment of sinus grafting procedures using cone-beam computed tomography compared with panoramic radiographs. Clinical Oral Implants Research. 2013;24(5):512–516. doi: 10.1111/j.1600-0501.2011.02408.x. [DOI] [PubMed] [Google Scholar]
- 4.Yildirm T. T., Kaya F. A., Yokus B., et al. Clinical and radiographic comparison by analyzed cone beam CT between one stage and two stage dental implants. Journal of International Dental and Medical Research. 2017;10(2):368–373. [Google Scholar]
- 5.Noorani T. Y., Shahid F., Ghani N. R. N. A., Saad N. R., Nowrin S. A. Effective use of cone beam computed tomography to detect a lateral root perforation: a case report. Journal of International Dental and Medical Research. 2018;11(2):520–526. [Google Scholar]
- 6.Ferlin R., Pagin B. S. C., Yaedú R. Y. F. Canalis sinuosus: a systematic review of the literature. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology. 2019;127(6):545–551. doi: 10.1016/j.oooo.2018.12.017. [DOI] [PubMed] [Google Scholar]
- 7.Azhari F. O., Fariska I. Normal value of cortical and mandibular trabecular bone density using cone beam computed tomography (CBCT) Journal of International Dental and Medical Research. 2019;12(1):160–164. [Google Scholar]
- 8.Tolstunov L. Horizontal Alveolar Ridge Augmentation in Implant Dentistry: A Surgical Manual. Hoboken, NJ, USA: Wiley-Blackwell; 2016. [DOI] [PubMed] [Google Scholar]
- 9.Machado V. D. C., Chrcanovic B. R., Felippe M. B., Manhães Júnior L. R. C., de Carvalho P. S. P. Assessment of accessory canals of the canalis sinuosus: a study of 1000 cone beam computed tomography examinations. International Journal of Oral and Maxillofacial Surgery. 2016;45(12):1586–1591. doi: 10.1016/j.ijom.2016.09.007. [DOI] [PubMed] [Google Scholar]
- 10.Gurler G., Delilbasi C., Ogut E. E., Aydin K., Sakul U. Evaluation of the morphology of the canalis sinuosus using cone-beam computed tomography in patients with maxillary impacted canines. Imaging Science in Dentistry. 2017;47(2):69–74. doi: 10.5624/isd.2017.47.2.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.von Arx T., Lozanoff S., Sendi P., Bornstein M. M. Assessment of bone channels other than the nasopalatine canal in the anterior maxilla using limited cone beam computed tomography. Surgical and Radiologic Anatomy. 2013;35(9):783–790. doi: 10.1007/s00276-013-1110-8. [DOI] [PubMed] [Google Scholar]
- 12.Manhães Júnior L. R. C., Villaça-carvalho M. F. L., Moraes M. E. L., Lopes S. L. P. d. C., Silva M. B. F., Junqueira J. L. C. Location and classification of Canalis sinuosus for cone beam computed tomography: avoiding misdiagnosis. Brazilian Oral Research. 2016;30(1):p. e49. doi: 10.1590/1807-3107bor-2016.vol30.0049. [DOI] [PubMed] [Google Scholar]
- 13.Ghandourah A. O., Rashad A., Heiland M., Hamzi B. M., Friedrich R. E. Cone-beam tomographic analysis of canalis sinuosus accessory intraosseous canals in the maxilla. German Medical Science. 2017;15 doi: 10.3205/000261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Orhan K., Gorurgoz C., Akyol M., Ozarslanturk S., Avsever H. An anatomical variant: evaluation of accessory canals of the canalis sinuosus using computed tomography. Folia Morphologica. 2018;77(3):551–557. doi: 10.5603/fm.a2018.0003. [DOI] [PubMed] [Google Scholar]
- 15.Oliveira-Santos C., Rubira-Bullen I. R. F., Monteiro S. A. C., León J. E., Jacobs R. Neurovascular anatomical variations in the anterior palate observed on CBCT images. Clinical Oral Implants Research. 2012;24(9):1044–1048. doi: 10.1111/j.1600-0501.2012.02497.x. [DOI] [PubMed] [Google Scholar]
- 16.Jacobs R., Mraiwa N., vanSteenberghe D., Gijbels F., Quirynen M. Appearance, location, course, and morphology of the mandibular incisive canal: an assessment on spiral CT scan. Dentomaxillofacial Radiology. 2002;31(5):322–327. doi: 10.1038/sj.dmfr.4600719. [DOI] [PubMed] [Google Scholar]
- 17.Arruda J. A., Pedro S., Silva L., et al. Dental implant in the canalis sinuosus: a case report and review of the literature. Case Reports in Dentistry. 2017;2017:5. doi: 10.1155/2017/4810123.4810123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jasa G. R., Shimizu M., Okamura K., et al. Effects of exposure parameters and slice thickness on detecting clear and unclear mandibular canals using cone beam CT. Dentomaxillofacial Radiology. 2017;46(4) doi: 10.1259/dmfr.20160315.20160315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pour D., Arzi B., Shamshiri A. Assessment of slice thickness effect on visibility of inferior alveolar canal in cone beam computed tomography images. Dental Research Journal. 2016;13(6):p. 527. doi: 10.4103/1735-3327.197041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sezgin Ö. S., Kayıpmaz S., Sahin B. The effect of slice thickness on the assessment of bone defect volumes by the cavalieri principle using cone beam computed tomography. Journal of Digital Imaging. 2013;26(1):115–118. doi: 10.1007/s10278-012-9480-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jia M. X., Zhang X., Li N., Han C. B. Impact of different CBCT imaging monitor units, reconstruction slice thicknesses, and planning CT slice thicknesses on the positioning accuracy of a MV-CBCT system in head-and-neck patients. Journal of Applied Clinical Medical Physics. 2012;13(5):117–125. doi: 10.1120/jacmp.v13i5.3766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mühler M., Schulz R., Schmidt S., Schmeling A., Reisinger W. The influence of slice thickness on assessment of clavicle ossification in forensic age diagnostics. International Journal of Legal Medicine. 2006;120(1):15–17. doi: 10.1007/s00414-005-0010-9. [DOI] [PubMed] [Google Scholar]
- 23.Doğan H., Veldkamp W. J., Dibbets‐Schneider P., et al. Effects of heart rate, filling and slice thickness on the accuracy of left ventricular volume measurements in a dynamic cardiac phantom using ECG-gated MDCT. The British Journal of Radiology. 2008;81(967):577–582. doi: 10.1259/bjr/92798700. [DOI] [PubMed] [Google Scholar]
- 24.Mordanov O., Khabadze Z., Daurova F., et al. Second mesiobuccal canal evaluation features with cone-beam computed tomography. International Journal of Dentistry. 2019;2019:4. doi: 10.1155/2019/5856405.5856405 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support the findings of this study are included within the article.



