Abstract
AIM
To evaluate the safety and efficacy of transepithelial photorefractive keratectomy (t-PRK) with adjuvant mitomycin C (MMC) versus femtosecond laser assisted keratomileusis (Femto-LASIK) in correction of high myopia.
METHODS
Prospective randomized comparative study including 156 eyes of 156 patients with high myopia and a spherical equivalent refraction (SER) <-6.00 D. They were divided randomly into two groups: Group A included 72 eyes treated with t-PRK with adjuvant MMC and Group B included 84 eyes treated with Femto-LASIK. Visual acuity, SER, corneal topography, pachymetry and keratometry were assessed for 12mo postoperatively.
RESULTS
The preoperative mean SER was -8.86±1.81 and -9.25±1.70 D in t-PRK MMC group and Femto-LASIK respectively (P=0.99) which improved to -0.65±0.43 D and -0.69±0.50 D at 12mo follow up. Mean SER remained stable during the 12mo of follow-up, with no statistically significant difference between the two groups (P=0.64). In t-PRK MMC group, only six eyes needed retreatment after six months of follow up. And two eyes showed haze (one reversible haze grade 2, while the other had dense irreversible haze grade 4).
CONCLUSION
t-PRK MMC provides safe and satisfactory visual outcomes and acceptable risk as Femto-LASIK in patients with high myopia.
Keywords: transepithelial photorefractive keratectomy, femtosecond laser assisted keratomileusis, high myopia, corneal haze, Egypt
INTRODUCTION
Photorefractive keratectomy (PRK) was first introduced 30 years ago[1]. Transepithelial photorefractive keratectomy (t-PRK) was proposed in the late 1990s as an alternative to conventional PRK. t-PRK removes the epithelium by laser phototherapeutic keratectomy followed by laser ablation of the stroma[2]–[3].
Although PRK is an established procedure for refractive correction of myopia, its popularity was downsized in favor for laser-assisted in situ keratomileusis (LASIK). Yet PRK is still needed in conditions where LASIK is not possible. However, postoperative haze following PRK is not uncommon in eyes undergoing higher degrees of correction making it the main limiting factor for using laser correction of vision in this group. Subsequent development of LASIK offered more rapid visual recovery with less pain and less haze. However, LASIK treatment in eyes with high myopia results in considerably deeper intrusion into the stroma, with concerns regarding biomechanical stability and an increased risk of ectasia. Further, many reports have regarded application of a suction ring during LASIK to be a potential risk factor for rhegmatogenous retinal detachment, especially in high myopes, because the procedure might induce vitreous traction and detachment resulting from sudden decompression of the eye[4]–[7].
Corneal haze, epithelial healing abnormalities, and pain are known adverse effects of PRK[8]–[9]. Development of adjuvant mitomycin C (MMC) therapy as prophylaxis for haze has demonstrated benefits in the refractive correction of high myopia and resulted in reappraisal of the role of PRK vs LASIK in this group[10]. Although postoperative discomfort is greater and visual recovery is slower compared to LASIK, surface ablation techniques avoid LASIK flap complications, thus substantially decreasing the risk of postoperative ectasia[11]. However, there have been few studies of clinical outcomes of t-PRK in high myopia[12]–[13].
The femtosecond laser has been used in a wide variety of ophthalmological procedures, allowing customization of the corneal flap parameters, such as diameter, thickness, and hinge position, which are the main advantages of using the femtosecond laser which lessen the risk of flap related complications such as buttonholed or incomplete flaps[14]–[15].
The aim of this study was to evaluate the safety and efficacy of t-PRK versus femtosecond laser assisted keratomileusis (Femto-LASIK) in the correction of high myopia in Egypt. This region is dry and sunny with high levels of ultraviolet (UV) light, which may increase the risk of postoperative haze after PRK[16].
SUBJECTS AND METHODS
Ethical Approval
The study was approved by the medical Ethics Committee at the Faculty of Medicine, Sohag University, and adhered to the Tenets of the Declaration of Helsinki. Written informed consent was obtained before surgery from all patients. Clinical Trial Registry Number: PACTR201906529708454.
This prospective comparative interventional study enrolled patients with high myopia who sought laser vision correction between April 2016 and May 2017 at Sohag Center for LASIK and Corneal Surgeries, Sohag, Egypt.
The inclusion criteria were high myopia [spherical equivalent refraction (SER) <-6.00 D][17]. Age 20-45y, LASIK is not possible for full correction due to thin cornea with residual stromal bed ≥280 µm[18]. Emmetropia was the target with full correction of the refractive error. Exclusion criteria were based on preoperative assessment of ocular topography, and included corneal dystrophy with topographic irregularity, pellucid marginal degeneration, forme fruste keratoconus, severe dry eye syndrome, previous corneal or intraocular surgery, history of current eyelid disease, or any form of keratitis in addition to patients with a history of keloid formation. Patients with incomplete 12mo follow up were excluded as well.
The 156 eyes with high myopia were classified randomly into two groups according to which eye involved right or left. They were divided randomly into two groups. Group A included 72 eyes treated with t-PRK with adjuvant MMC and group B included 84 eyes treated with Femto-LASIK.
All patients were evaluated pre and postoperatively for the following: manifest uncorrected distant visual acuity (UCVA), best corrected distant visual acuity (BCVA). Decimal notation was used to describe the visual acuity, SER, slit-lamp biomicroscopy, intraocular pressure, and fundus examination. Corneal topography was evaluated using Sirius Scheimpflug Placido topography (CSO, Florence, Italy).
Preparation for the surgery included application of prophylactic topical antibiotic eye drops (gatifloxacin 0.3% 5 times per day) in the 24h preoperatively followed by topical anaesthesia (benoxinate hydrochloride 0.4%) applied 2min before surgery).
After application of povidone iodine 10% surgical scrub on the lashes and eyelids, a closed-loop lid speculum was applied. In all cases, stromal ablation was carried out by an excimer laser [VISX S4IR: Abbott Medical Optics (AMO), Santa Ana, CA, USA]. In the t-PRK: 50 µm of epithelium was removed followed by stromal ablation of the exact depth needed. The stromal bed was washed with cold balanced salt solution[19] to lessen the thermal effect of laser ablation. After laser ablation, MMC 0.02% was applied for 40s in all cases.
Femto-LASIK was done after application of topical anesthesia, a 90-µm thickness flap was created using by the IntraLase (iFS, Abbott). Femtosecond laser parameters for the corneal flap creation included bed energy level of 0.85 µJ, a side-cut energy level of 0.95 µJ with superior hinge orientation, flap diameter 9.00 mm, side cut angle 90 degree and hinge angle 90 degree. After lifting the flap, ablation was performed using the same excimer laser device.
A silicone hydrogel bandage contact lens was applied after laser ablation until complete epithelial healing was confirmed in t-PRK MMC group. The postoperative medications included topical antibiotic eye drops (gatifloxacin 0.3% 5 times daily for 1wk), topical steroid eye drops (prednisolone acetate 1% 5 times daily for 1wk), lubricant eye drops, and systemic non-steroidal anti-inflammatory drugs. UV protection was advised and 1000 mg of vitamin C were prescribed for at least 1mo. Gradual tapering of topical steroids over one month was performed to decrease the risk of corneal scarring.
Postoperative visits were scheduled for the first postoperative day, and then at 1wk and 1, 3, 6, and 12mo after surgery. Each follow-up visit included slit-lamp examination in group A to detect haze, which was graded according to the method proposed by Fantes et al[20] as 0 (no haze), 0.5 (trace haze on oblique illumination), 1 (corneal cloudiness not interfering with visibility of the fine details of the iris), 2 (mild effacement of the fine details of the iris), 3 (moderate obscuration of the fine details of the iris), or 4 (details of the lens and iris not discernible).
Statistical Analysis
The data were analyzed using SPSS for Windows version 18.0 software (SPSS Inc., Chicago, IL, USA). It was used to compare both groups. A P-value <0.05 was considered to be statistically significant. Independent sample t-test was used to compare means of preoperative variables of the 2 groups. Correlation coefficients including Pearson or Spearman assess the correlation between different variables under normal conditions.
RESULTS
A total of 156 eyes of 156 patients were enrolled for this prospective study, 60 were males (38.5%) and 96 females (61.5%). The mean of age of group A was 29.76±5.01y and 27.94±6.69y in group B. Demographic data for both groups are shown in Table 1. The target refraction in all patients was emmetropia.
Table 1. Demographic data for both groups.
| Parameters | Group A (t-PRK) | Group B (Femto-LASIK) | P |
| Eyes | 72 | 84 | 0.86 |
| Age (y) | 29.76±5.01 | 27.94±6.69 | 0.731 |
| Gender (M:F) | 32:40 | 28:56 |
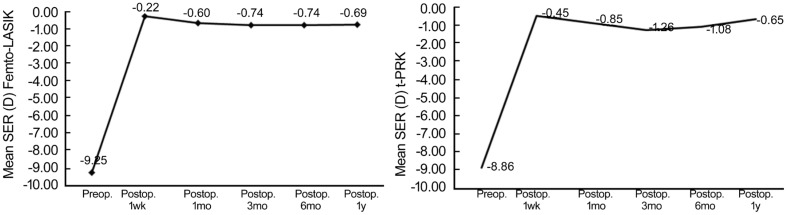
In group A, the preoperative mean SER was -8.86±1.81 D and -9.25±1.70 D in group B with (P=0.99) which improved to -0.65±0.43 D and -0.69±0.51 D respectively at 12mo follow up (P=0.64; Figure 1).
Figure 1. Changes in mean SER in both groups all over a period of one year follow up.
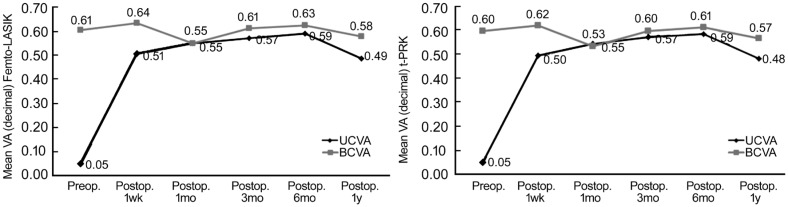
As regards the visual outcomes; in group A, the preoperative mean UCVA was 0.05±0.02 and 0.05±0.01 in group B with (P=0.96) which improved to 0.48±0.17 and 0.49±0.18 at 12mo follow up (P=0.53; Figure 2).
Figure 2. Changes in mean UCVA versus BCVA in both groups all over a period of one year follow up.
Twelve-month changes in vision and refraction indices between the two groups are compared in Table 2, comparison of baseline parameters showed no significant difference between the two groups preoperatively (all P>0.05).
Table 2. Twelve-month changes in vision and refraction indices between the two groups.
| Parameters | Preop. | P | 1wk | P | 1mo | P | 3mo | P | 6mo | P | 1y | P | |
| UCVA | Femto | 0.05±0.01 | 0.96 | 0.51±0.17 | 0.47 | 0.55±0.17 | 0.49 | 0.57±0.18 | 0.57 | 0.59±0.17 | 0.48 | 0.49±0.18 | 0.53 |
| t-PRK | 0.05±0.02 | 0.50±0.15 | 0.54±0.16 | 0.56±0.17 | 0.58±0.16 | 0.48±0.17 | |||||||
| BCVA | Femto | 0.61±0.17 | 0.47 | 0.64±0.17 | 0.41 | 0.55±0.18 | 0.51 | 0.61±0.16 | 0.41 | 0.63±0.16 | 0.45 | 0.58±0.17 | 0.45 |
| t-PRK | 0.60±0.15 | 0.63±0.15 | 0.54±0.16 | 0.60±0.15 | 0.62±0.15 | 0.57±0.15 | |||||||
| SER | Femto | -9.25±1.70 | 0.99 | -0.22±0.67 | 0.2 | -0.60±0.59 | 0.005 | -0.74±0.49 | 0.01 | -0.74±0.48 | 0.001 | -0.69±0.51 | 0.64 |
| t-PRK | -8.86±1.81 | -0.45±0.98 | -0.85±0.95 | -1.26±0.96 | -1.08±0.92 | -0.65±0.43 | |||||||
| Sphere | Femto | -7.88 | 0.79 | -0.15 | 0.23 | -0.39 | 0.004 | -0.49 | 0.001 | -0.55 | 0.001 | -0.46 | 0.156 |
| t-PRK | -7.50 | -0.36 | -0.64 | -1.01 | -0.88 | -0.45 | |||||||
| Cylinder | Femto | -2.73 | 0.01 | -0.14 | 0.51 | -0.42 | 0.27 | -0.50 | 0.30 | -0.39 | 0.20 | -0.48 | 0.07 |
| t-PRK | -2.72 | -0.18 | -0.42 | -0.50 | -0.40 | -0.41 | |||||||
P-value for comparison of postoperative value all over 12mo of follow-up with the preoperative value; UCVA: Uncorrected distant visual acuity; BCVA: Best corrected distant visual acuity; SER: Spherical equivalent refraction.
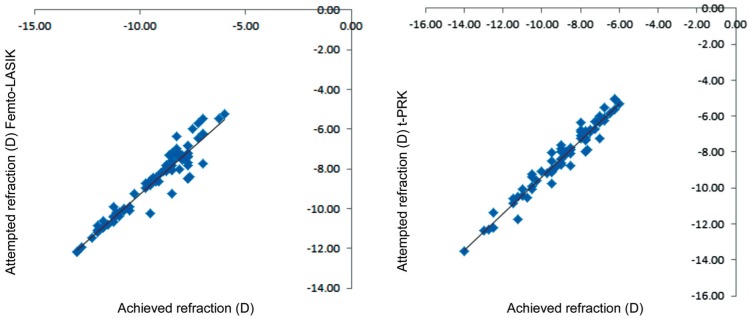
Scattergram of attempted versus achieved mean SER for Femto-LASIK group and t-PRK at 12mo postoperatively was shown in Figure 3.
Figure 3. Scattergram of attempted versus achieved mean SER for both groups at 12mo postoperatively.
The safety indices (ratio of the mean BCVA at 12mo postoperatively to the mean preoperative BCVA), the efficacy indices (the ratio of the mean postoperative UCVA to the mean preoperative BCVA at 12mo) and predictability of both groups were summarized in Table 3.
Table 3. Safety, efficacy and predictability of both groups at 12mo.
| Parameters | Group A (t-PRK) | Group B (Femto-LASIK) |
| Safety (%) | 95.0 | 95.1 |
| Efficacy (%) | 80.0 | 80.3 |
| Predictability (%) | ||
| SER within 1.00 (D) | 71.43 | 85.71 |
| SER within 1.50 (D) | 84.52 | 95.24 |
Regarding stability at 12mo postoperatively, both procedures were stable with no statistically significant differences among the measured SER.
Six eyes needed retreatment due to marked regression <-1.00 D at six months of follow up. After patient consultation with the surgeon and checking the availability of enough corneal thickness, another t-PRK retreatment was done to reach the desired refraction. Patients were satisfied with UCVA of 0.3±0.10 at the end of the 12mo follow up period.
Five eyes in the study population developed complications, comprising delayed epithelial healing in two eyes and complete healing occurred only after cessation of topical steroids. Corneal haze developed in two eyes of two patients (one eye with grade 2 haze at 3mo that improved with topical steroids and the other eye with dense irreversible grade 4 haze at 2mo and necessitated lamellar keratoplasty). One eye suffered from toxic epitheliopathy (an unhealthy thickened irregular epithelial surface with punctate epithelial erosions and opacification extending from the epithelial surface down to the subepithelial and superficial stromal regions) which was controlled by switch from preserved to preservative-free eye drops with UCVA of 0.3±0.12 at the end of the 12mo follow up period (Figure 4).
Figure 4. Postoperative complications of t-PRK in the studied population.
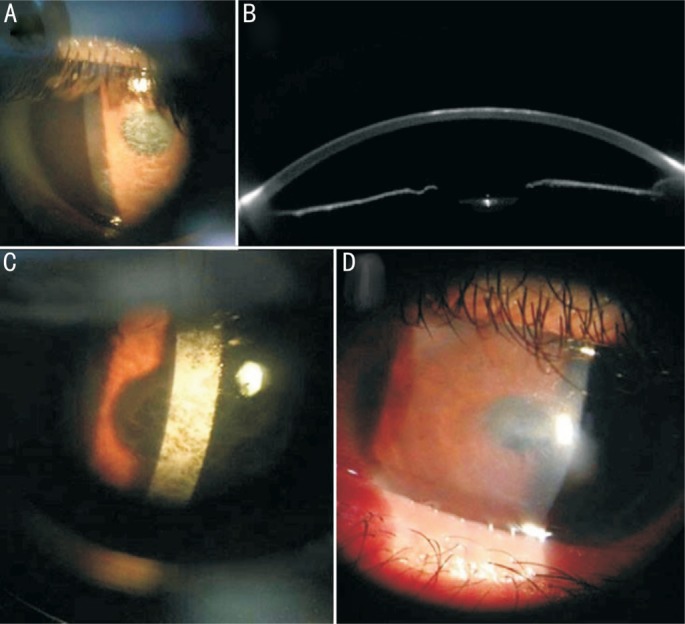
A: Haze grade 2; B: Scheimpflug imaging of the same eye; C: Haze grade 4; D: Toxic epitheliopathy.
Complications in the Femto-LASIK group included two eyes with released suction ring and two eyes with microstriae which were corrected by re-floating the flap.
DISCUSSION
PRK is a safe and effective technique for correction of low and moderate myopia[19]. However, its clinical outcomes in highly myopic eyes need to be evaluated in more detail especially in dry and sunny environments. High levels of UV exposure may increase the risk of corneal haze.
In our study, epithelium was removed using the excimer laser which we preferred due to the homogeneous and uniform epithelial removal. Epithelial removal using laser has superior impact on postoperative pain and on subepithelial opacification[21]–[22].
In a study that compared the visual outcomes and safety of t-PRK and conventional PRK in eyes with low to moderate myopia, Naderi et al[2] found that t-PRK was superior to conventional PRK in terms of improving safety and efficacy indices and visual acuity. Our findings showed significant improvement in UCVA (P<0.0001) with a high safety index (0.95). This is particularly significant because our subjects were high myopes in a high UV environment and were followed for at least 1y.
Our results agreed with those of Adib-Moghaddam et al[23] who reported a high degree of safety and visual improvement after t-PRK in patients with myopia up to -8.75 D during 18mo of follow-up.
In the current study, postoperative refraction was stable, with no statistically significant regression observed recorded during 12mo of follow-up. This finding is in agreement with that of Kaluzny et al[13] who compared t-PRK and alcohol-assisted PRK in eyes with moderate myopia and compound myopic astigmatism correction and reported that the mean refractive spherical equivalent was stable during 3mo of follow-up.
However, not all studies coincide with our results. A study by Buratto et al[24], found that 29 of 40 eyes treated by PRK showed regression of myopia by 6mo after surgery.
Our results confirm that the use of MMC in a concentration of 0.02% for 40s yielded better visual results and less haze which was most feared. The efficacy of MMC was investigated in different studies with different concentrations and different application time[25]–[28].
The predictability of t-PRK group demonstrates good refractive predictability at 1y (84.52%) but less than Femto-LASIK group. These results are consistent with those of Dausch et al[29] who investigated the clinical outcomes of PRK for myopia exceeding -8.00 D using a standard or aspherical optimized profile in 100 eyes and demonstrated high predictability for both techniques over a follow-up duration of 1y.
Also, in a study of Hashemi et al[30] who compared the results of Femto-LASIK and PRK with MMC for the correction of myopia more than 7.0 D, they found that differences between both groups in baseline indices were not statistically significant at 6mo after surgery which coincides with our results.
Hashmani et al[31] studied visual outcomes and satisfaction among patients of PRK and femtosecond LASIK. They found the efficacy indexes of the femto-Lasik and PRK groups were 1.00 and 0.82, respectively. The predictability of the procedures was 92.1% and 64.9% which is lower than our results.
The low incidence of haze in our study can be explained by application of MMC 0.02% for 40s, as in a study by Kremer et al[32] who reported a decreased risk of haze following PRK with application of MMC in 1520 eyes, even in eyes with delayed epithelial healing.
Cooling the corneal bed with cold balanced salt solution as a routine step in our excimer laser treatment is also beneficial because it lessens the thermal effect of laser ablation, which in turn decreases formation of corneal haze. The beneficial effect of this technique was seen in a study by Niizuma et al[19] who investigated the ability of cold balanced salt solution to reduce the risk of subepithelial haze. Stein et al[33] also investigated the effect of cooling the cornea during PRK to reduce postoperative corneal haze and found that haze was significantly reduced in eyes that were irrigated with cold balanced salt solution.
In conclusion, the results of t-PRK in patients with high myopia in Egypt with hot sunny weather is was shown to be safe with high efficacy in decreasing refractive error and acceptable risk through 1y of follow-up. Further studies are warranted to investigate if similar techniques can produce acceptable results in extreme myopia (SE<-10.00).
Acknowledgments
Conflicts of Interest: Mounir A, None; Mostafa EM, None; Ammar H, None; Mohammed OA, None; Alsmman AH, None; Farouk MM, None; Elghobaier MG, None.
REFERENCES
- 1.Munnerlyn CR, Koons SJ, Marshall J. Photorefractive keratectomy: a technique for laser refractive surgery. J Cataract Refract Surg. 1988;14(1):46–52. doi: 10.1016/s0886-3350(88)80063-4. [DOI] [PubMed] [Google Scholar]
- 2.Naderi M, Jadidi K, Mosavi SA, Daneshi SA. Transepithelial photorefractive keratectomy for low to moderate myopia in comparison with conventional photorefractive keratectomy. J Ophthalmic Vis Res. 2016;11(4):358–362. doi: 10.4103/2008-322X.194070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Clinch TE, Moshirfar M, Weis JR, Ahn CS, Hutchinson CB, Jeffrey JH. Comparison of mechanical and transepithelial debridement during photorefractive keratectomy. Ophthalmology. 1999;106(3):483–489. doi: 10.1016/S0161-6420(99)90135-5. [DOI] [PubMed] [Google Scholar]
- 4.Sia RK, Ryan DS, Edwards JD, Stutzman RD, Bower KS. The US Army Surface Ablation Study: comparison of PRK, MMC-PRK, and LASEK in moderate to high myopia. J Refract Surg. 2014;30(4):256–264. doi: 10.3928/1081597X-20140320-04. [DOI] [PubMed] [Google Scholar]
- 5.Hashemi H, Salimi Y, Pir P, Asgari S. Photorefractive keratectomy with mitomycin-C for high myopia: three year follow-up results. Acta Med Iran. 2017;55(1):42–48. [PubMed] [Google Scholar]
- 6.Al-Rashaed S, Al-Halafi AM. Retinal detachment after laser in situ keratomileusis. Middle East Afr J Ophthalmol. 2011;18(3):224–227. doi: 10.4103/0974-9233.84052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yumusak E, Ornek K, Ozkal F. Bilateral simultaneous rhegmatogenous retinal detachment following laser in situ keratomileusis. Case Rep Ophthalmol. 2016;7(2):341–345. doi: 10.1159/000446602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Margo JA, Munir WM. Corneal haze following refractive surgery: a review of pathophysiology, incidence, prevention, and treatment. Int Ophthalmol Clin. 2016;56(2):111–125. doi: 10.1097/IIO.0000000000000112. [DOI] [PubMed] [Google Scholar]
- 9.McCarty CA, Garrett SK, Aldred GF, Taylor HR. Assessment of subjective pain following photorefractive keratectomy. Melbourne Excimer Laser Group. J Refract Surg. 1996;12(3):365–369. doi: 10.3928/1081-597X-19960301-11. [DOI] [PubMed] [Google Scholar]
- 10.Talamo JH, Gollamudi S, Green WR, De La Cruz Z, Filatov V, Stark WJ. Modulation of corneal wound healing after excimer laser keratomileusis using topical mitomycin C and steroids. Arch Ophthalmol. 1991;109(8):1141–1146. doi: 10.1001/archopht.1991.01080080101040. [DOI] [PubMed] [Google Scholar]
- 11.Broderick KM, Sia RK, Ryan DS, Stutzman RD, Mines MJ, Frazier TC, Torres MF, Bower KS. Wavefront-optimized surface retreatments of refractive error following previous laser refractive surgery: a retrospective study. Eye Vis (Lond) 2016;3:3. doi: 10.1186/s40662-016-0034-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bakhsh AM, Elwan SAM, Chaudhry AA, El-Atris TM, Al-Howish TM. Comparison between transepithelial photorefractive keratectomy versus alcohol-assisted photorefractive keratectomy in correction of myopia and myopic astigmatism. J Ophthalmol. 2018;2018:5376235. doi: 10.1155/2018/5376235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kaluzny BJ, Cieslinska I, Mosquera SA, Verma S. Single-step transepithelial PRK vs alcohol-assisted PRK in myopia and compound myopic astigmatism correction. Medicine (Baltimore) 2016;95(6):e1993. doi: 10.1097/MD.0000000000001993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marino GK, Santhiago MR, Wilson SE. Femtosecond lasers and corneal surgical procedures. Asia Pac J Ophthalmol (Phila) 2017;6(5):456–464. doi: 10.22608/APO.2017163. [DOI] [PubMed] [Google Scholar]
- 15.Ye MJ, Liu CY, Liao RF, Gu ZY, Zhao BY, Liao Y. SMILE and wavefront-guided LASIK out-compete other refractive surgeries in ameliorating the induction of high-order aberrations in anterior corneal surface. J Ophthalmol. 2016;2016:8702162. doi: 10.1155/2016/8702162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stojanovic A, Nitter TA. Correlation between ultraviolet radiation level and the incidence of late-onset corneal haze after photorefractive keratectomy. J Cataract Refract Surg. 2001;27(3):404–410. doi: 10.1016/s0886-3350(00)00742-2. [DOI] [PubMed] [Google Scholar]
- 17.Bar Dayan Y, Levin A, Morad Y, Grotto I, Ben-David R, Goldberg A, Onn E, Avni I, Levi Y, Benyamini OG. The changing prevalence of myopia in young adults: a 13-year series of population-based prevalence surveys. Invest Ophthalmol Vis Sci. 2005;46(8):2760–2765. doi: 10.1167/iovs.04-0260. [DOI] [PubMed] [Google Scholar]
- 18.Zhang J, Yu KM. Femtosecond laser corneal refractive surgery for the correction of high myopic anisometropic amblyopia in juveniles. Int J Ophthalmol. 2017;10(11):1678–1685. doi: 10.18240/ijo.2017.11.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Niizuma T, Ito S, Hayashi M, Futemma M, Utsumi T, Ohashi K. Cooling the Cornea to prevent side effects of photorefractive keratectomy. J Refract Corneal Surg. 1994;10(2 Suppl):S262–S266. [PubMed] [Google Scholar]
- 20.Fantes FE, Hanna KD, Waring GO, 3rd, Pouliquen Y, Thompson KP, Savoldelli M. Wound healing after excimer laser keratomileusis (photorefractive keratectomy) in monkeys. Arch Ophthalmol. 1990;108(5):665–675. doi: 10.1001/archopht.1990.01070070051034. [DOI] [PubMed] [Google Scholar]
- 21.Durrie DS, Lesher MP, Cavanaugh TB. Classification of variable clinical response after photorefractive keratectomy for myopia. J Refract Surg. 1995;11(5):341–347. doi: 10.3928/1081-597X-19950901-10. [DOI] [PubMed] [Google Scholar]
- 22.Lee HK, Lee KS, Kim JK, Kim HC, Seo KR, Kim EK. Epithelial healing and clinical outcomes in excimer laser photorefractive surgery following three epithelial removal techniques: mechanical, alcohol, and excimer laser. Am J Ophthalmol. 2005;139(1):56–63. doi: 10.1016/j.ajo.2004.08.049. [DOI] [PubMed] [Google Scholar]
- 23.Adib-Moghaddam S, Soleyman-Jahi S, Salmanian B, Omidvari AH, Adili-Aghdam F, Noorizadeh F, Eslani M. Single-step transepithelial photorefractive keratectomy in myopia and astigmatism: 18-month follow-up. J Cataract Refract Surg. 2016;42(11):1570–1578. doi: 10.1016/j.jcrs.2016.08.029. [DOI] [PubMed] [Google Scholar]
- 24.Buratto L, Ferrari M. Photorefractive keratectomy or keratomileusis with excimer laser in surgical correction of severe myopia: which technique is better? Eur J Implant Refract Surg. 1993;5(3):183–186. [Google Scholar]
- 25.Majmudar PA, Schallhorn SC, Cason JB, Donaldson KE, Kymionis GD, Shtein RM, Verity SM, Farjo AA. Mitomycin-C in corneal surface excimer laser ablation techniques: a report by the American Academy of Ophthalmology. Ophthalmology. 2015;122(6):1085–1095. doi: 10.1016/j.ophtha.2015.01.019. [DOI] [PubMed] [Google Scholar]
- 26.Kaiserman I, Sadi N, Mimouni M, Sela T, Munzer G, Levartovsky S. Corneal breakthrough haze after photorefractive keratectomy with mitomycin C: incidence and risk factors. Cornea. 2017;36(8):961–966. doi: 10.1097/ICO.0000000000001231. [DOI] [PubMed] [Google Scholar]
- 27.Arranz-Marquez E, Katsanos A, Kozobolis VP, Konstas AGP, Teus MA. A critical overview of the biological effects of mitomycin C application on the Cornea following refractive surgery. Adv Ther. 2019;36(4):786–797. doi: 10.1007/s12325-019-00905-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Garcia-Gonzalez M, Drake Rodriguez-Casanova P, Rodriguez-Perez I, Rodero A, Teus MA. Long-term follow-up of LASEK with mitomycin C performed to correct myopia in thin corneas. J Refract Surg. 2017;33(12):813–819. doi: 10.3928/1081597X-20171004-06. [DOI] [PubMed] [Google Scholar]
- 29.Dausch D, Dausch B, Wottke M, Sluyterman van Langeweyde G. Comparison of clinical outcomes in PRK with a standard and aspherical optimized profile: a full case analysis of 100 eyes with 1-year follow-up. Clin Ophthalmol. 2014;8:2251–2260. doi: 10.2147/OPTH.S66608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hashemi H, Miraftab M, Ghaffari R, Asgari S. Femtosecond-assisted LASIK versus PRK: comparison of 6-month visual acuity and quality outcome for high myopia. Eye Contact Lens. 2016;42(6):354–357. doi: 10.1097/ICL.0000000000000216. [DOI] [PubMed] [Google Scholar]
- 31.Hashmani N, Hashmani S, Ramesh P, Rajani H, Ahmed J, Kumar J, Kumar A, Jamali M. A comparison of visual outcomes and patient satisfaction between photorefractive keratectomy and femtosecond laser-assisted in situ keratomileusis. Cureus. 2017;9(9):e1641. doi: 10.7759/cureus.1641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kremer I, Ehrenberg M, Levinger S. Delayed epithelial healing following photorefractive keratectomy with mitomycin C treatment. Acta Ophthalmol. 2012;90(3):271–276. doi: 10.1111/j.1755-3768.2010.01894.x. [DOI] [PubMed] [Google Scholar]
- 33.Stein HA, Salim AG, Stein RM, Cheskes A. Corneal cooling and rehydration during photorefractive keratectomy to reduce postoperative corneal haze. J Refract Surg. 1999;15(2 Suppl):S232–S233. doi: 10.3928/1081-597X-19990302-18. [DOI] [PubMed] [Google Scholar]