It has been well documented that acute osteoporotic vertebral fractures (OVF) can have no visible deformation of vertebral body, and these OVFs are commonly termed as radiographically ‘occult’ (1-4). Magnetic resonance imaging (MRI) can help the diagnosis of these occult OVFs. However, some of these ‘occult’ OVF are actually radiographically evidential if we look carefully.
Though vertebral endplate depression and anterior cortex buckling have been noted as signs of OVF (5-11), their significance may not have been well recognized by all spine radiograph readers (radiologists, orthopedic surgeons, rheumatologists, etc.). OVF is generally considered to be associated with vertebral body height loss; however, it is not always the case, particularly at the early phase. In our recent analysis of radiological reports for spine radiograph referred due to back pain, it was noted that osteoporotic ECF (endplate and/or cortex fracture) without vertebral body height loss was commonly missed (12). On the other hand, no singular moderate/severe OVF (one OVF in one patient) was missed; though OVFs at multiple levels were often under-reported, i.e., not all OVFs were precisely reported (12).
Hereby we present a few cases of OVFs in the literatures (Figures 1-3), which were originally considered to be ‘occult’ OVF. Thus, the prevalence of ‘occult’ OVF may have been over-estimated. These cases illustrate the importance of recognizing ECF. Note the relevance of ECF has been emphasized in Genant’s original paper on OVF semi-quantitative grading (5), as well as many following articles (6-11,13,14). In some cases, acute ECF with minimal vertebral deformity can quickly progress to vertebral collapse (Figure 4). For radiograph of elderly female patients with a history of acute back pain in a setting of possible osteoporosis, close attention should be paid to look at vertebral endplate depression and anterior cortex buckling, particularly for vertebral levels with OVF high risk (10,11,15,16). With adequate training, radiologists can play a unique role in correctly interpreting the fine details of spine radiograph, and contribute to the clinical care for patients with OVF (17).
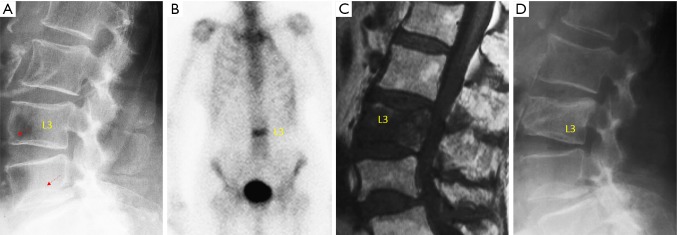
Figure 1.
An 88-year-old woman with acute lower back pain after a fall of her own height. (A) Radiograph performed 2 days after the fall shows a previously known L4 lower endplate fracture (dotted arrow, an indicator of osteoporosis). L3 has an anterior cortex buckling (dotted arrow), which was missed in the initial reporting; (B) bone scintigraphy shows a band-like pattern of L3; (C) T1-weighted magnetic resonance imaging performed 3 weeks after initial radiograph. Normal signal in L4 confirms the chronic nature of its fracture. L3 has a reduced signal in most of the body; (D) radiograph taken 4 months after the onset of pain shows L3 deformity. [modified with permission from (2)].
Figure 2.

A 71-year-old woman with osteoporosis and no history of falls/injuries. Plain lumbar radiograph (left) shows L2 and L4 lower endplate depressions (dotted arrows). T1-weighted magnetic resonance imaging (right) shows L2 endplate fracture and associated lower marrow signal, suggesting acute nature of this fracture. Bone marrow signal is normal at L4 level, suggesting L4 fracture is likely old. This case was referred as radiographically ‘occult’ osteoporotic vertebral fracture in the initial reporting. [modified with permission from (3)].
Figure 3.
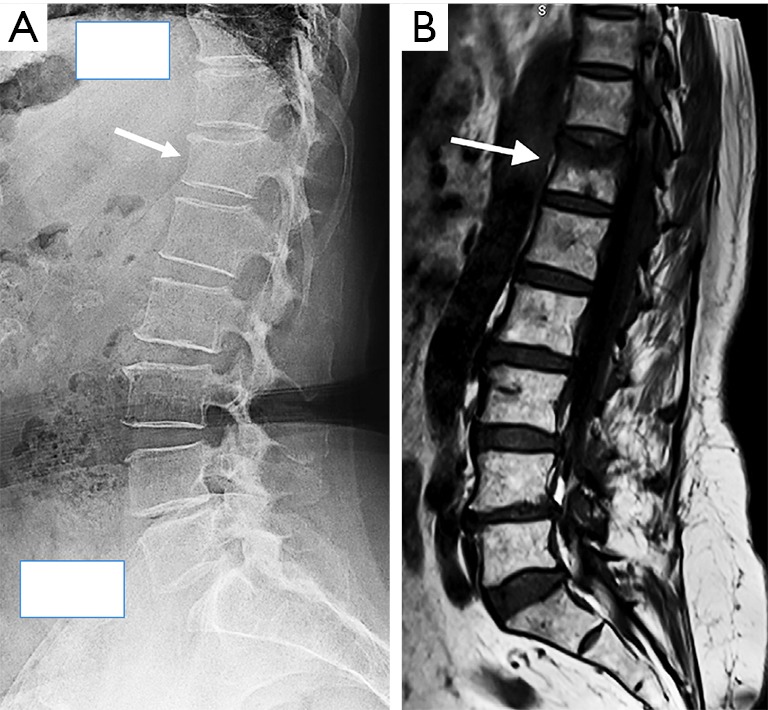
A 68-year-old woman with osteoporotic vertebral fracture. (A) Radiograph shows T12 vertebra mild wedging and upper endplate depression (fracture) which was missed in the initial reporting; (B) T1-weighted magnetic resonance imaging shows acute fracture of upper part of T12 vertebra. [modified with permission from (4)].
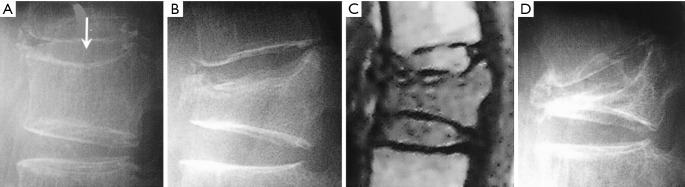
Figure 4.
A 71-year-old woman with osteoporotic vertebral fracture. (A) Radiograph taken two days after the onset of acute pain, arrow indicates an upper endplate fracture; (B) radiograph and (C) magnetic resonance imaging, were taken 3 weeks after the incident, showing severe vertebral deformity; (D) radiograph taken 5 months after the incident, the vertebral deformity progressed to collapse. [reproduced with permission from (5)].
Acknowledgments
None.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Kanchiku T, Taguchi T, Kawai S. Magnetic resonance imaging diagnosis and new classification of the osteoporotic vertebral fracture. J Orthop Sci 2003;8:463-6. 10.1007/s00776-003-0665-3 [DOI] [PubMed] [Google Scholar]
- 2.Pham T, Azulay-Parrado J, Champsaur P, Chagnaud C, Legré V, Lafforgue P. "Occult" osteoporotic vertebral fractures: vertebral body fractures without radiologic collapse. Spine (Phila Pa 1976) 2005;30:2430-5. 10.1097/01.brs.0000184303.86932.77 [DOI] [PubMed] [Google Scholar]
- 3.Terakado A, Orita S, Inage K, Kubota G, Kanzaki T, Mori H, Shinohara Y, Nakamura J, Matsuura Y, Aoki Y, Furuya T, Koda M, Ohtori S. A Clinical Prospective Observational Cohort Study on the Prevalence and Primary Diagnostic Accuracy of Occult Vertebral Fractures in Aged Women with Acute Lower Back Pain Using Magnetic Resonance Imaging. Pain Res Manag 2017;2017:9265259. [DOI] [PMC free article] [PubMed]
- 4.Marongiu G, Congia S, Verona M, Lombardo M, Podda D, Capone A. The impact of magnetic resonance imaging in the diagnostic and classification process of osteoporotic vertebral fractures. Injury 2018;49 Suppl 3:S26-31. 10.1016/j.injury.2018.10.006 [DOI] [PubMed] [Google Scholar]
- 5.Genant HK, Wu CY, van Kuijk C, Nevitt MC. Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 1993;8:1137-48. 10.1002/jbmr.5650080915 [DOI] [PubMed] [Google Scholar]
- 6.Yoshida T, Nanba H, Mimatsu K, Kasai T. Treatment of osteoporotic spinal compression fractures. Conservative therapy and its limitation. Clin Calcium 2000;10:53-8. [Google Scholar]
- 7.Jiang G, Eastell R, Barrington NA, Ferrar L. Comparison of methods for the visual identification of prevalent vertebral fracture in osteoporosis. Osteoporos Int 2004;15:887-96. 10.1007/s00198-004-1626-1 [DOI] [PubMed] [Google Scholar]
- 8.Ito Z, Harada A, Matsui Y, Takemura M, Wakao N, Suzuki T, Nihashi T, Kawatsu S, Shimokata H, Ishiguro N. Can you diagnose for vertebral fracture correctly by plain X-ray? Osteoporos Int 2006;17:1584-91. 10.1007/s00198-006-0123-0 [DOI] [PubMed] [Google Scholar]
- 9.Wáng YXJ, Che-Nordin N. Informed communication with study subjects of radiographically detected osteoporotic vertebral deformity. Quant Imaging Med Surg 2018;8:876-80. 10.21037/qims.2018.09.06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wáng YXJ, Santiago RF, Deng M, Nogueira-Barbosa MH. Identifying osteoporotic vertebral endplate and cortex fractures. Quant Imaging Med Surg 2017;7:555-91. 10.21037/qims.2017.10.05 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wáng YXJ, Deng M, He LC, Che-Nordin MN, Santiago RF. Osteoporotic vertebral endplate and cortex fractures: a pictorial review. J Orthop Translat 2018;15:35-49. 10.1016/j.jot.2018.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Du MM, Che-Nordin N, Ye PP, Qiu SW, Yan ZH, Wang YX. Underreporting characteristics of osteoporotic vertebral compressive fracture in back pain clinic patients of a tertiary hospital in China. J Orthop Translat 2020. doi: 10.1016/j.jot.2019.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lentle BC, Berger C, Probyn L, Brown JP, Langsetmo L, Fine B, Lian K, Shergill AK, Trollip J, Jackson S, Leslie WD, Prior JC, Kaiser SM, Hanley DA, Adachi JD, Towheed T, Davison KS, Cheung AM, Goltzman D; CaMos Research Group. Comparative Analysis of the radiology of osteoporotic vertebral fractures in women and men: cross-sectional and longitudinal observations from the Canadian Multicentre Osteoporosis Study (CaMos). J Bone Miner Res 2018;33:569-79. 10.1002/jbmr.3222 [DOI] [PubMed] [Google Scholar]
- 14.Wáng YXJ, Che-Nordin N, Deng M, Leung JCS, Kwok AWL, He LC, Griffith JF, Kwok TCY, Leung PC. Osteoporotic vertebral deformity with endplate/cortex fracture is associated with higher further vertebral fracture risk: the Ms. OS (Hong Kong) study results. Osteoporos Int 2019;30:897-905. 10.1007/s00198-019-04856-4 [DOI] [PubMed] [Google Scholar]
- 15.Lentle B, Trollip J, Lian K. The radiology of osteoporotic vertebral fractures redux. J Clin Densitom 2016;19:40-7. 10.1016/j.jocd.2015.08.009 [DOI] [PubMed] [Google Scholar]
- 16.Che-Nordin N, Deng M, Griffith JF, Leung JCS, Kwok AWL, Zhu YQ, So RHY, Kwok TCY, Leung PC, Wáng YX. Prevalent osteoporotic vertebral fractures more likely involve the upper endplate than the lower endplate and even more so in males. Ann Transl Med 2018;6:442. 10.21037/atm.2018.10.61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guglielmi G, Balzano RF, Cheng X. What is changed in the diagnosis of osteoporosis: the role of radiologists. Quant Imaging Med Surg 2018;8:1-4. 10.21037/qims.2018.02.04 [DOI] [PMC free article] [PubMed] [Google Scholar]