Abstract
The major histocompatibility complex class II (MHC II)–CD4 immunologic synapse is classically described between the T-cell receptor of CD4-positive lymphocytes and MHC II on antigen-presenting cells. This interaction and others between surrounding costimulatory and checkpoint molecules promote differentiation of naïve CD4 T lymphocytes into helper T cells subtypes, including types 1, 2, and 17 helper T cells, that have more tailored immunologic responses. Although MHC II is mainly produced by professional antigen-presenting cells, it can be aberrantly produced by other cell types, including hepatocytes in various liver pathologies, such as autoimmune hepatitis and alcoholic hepatitis. This can lead to direct targeting of hepatocytes by CD4-positive lymphocytes, which form an immunologic synapse with the hepatocyte. The lymphocytes internalize the MHC II–CD4 complexes in a phagocytosis-like mechanism and in the process eat the hepatocyte piece by piece. We review the evidence for this mechanism and the role of these autoimmune responses in various liver diseases, including alcoholic hepatitis, autoimmune hepatitis, and primary biliary cirrhosis. The role of aberrant MHC II in malignancy, including hepatocellular carcinoma, is also reviewed. Further understanding of this mechanism can lead to better understanding of the immune mechanisms involved in these liver pathologies, with potential diagnostic and therapeutic applications.
Historical Context and Current Understanding of the Immunologic Synapse
Initially, it was recognized that the major histocompatibility complex (MHC) is required for specific recognition of antigen by T cells.1 Solving the crystal structure of major histocompatibility complex shed further light on this mechanism as it demonstrated how a foreign peptide antigen fit into the MHC complex.2 Other molecules required for T-cell activation were also discovered; however, it was unclear how these various signals could cause T-cell activation as activating them alone was not sufficient for T-cell activation.3
The first description of the immunologic synapse in 1995 furthered our understanding in 1995.4 Using digital imaging to analyze antigen-specific interactions between individual T cells and antigen-presenting cells, the authors showed that rather than even distribution of key molecules involved in T-cell activation, there were segregated, concentrated three-dimensional clusters of molecules. Subsequent studies further characterized the immunologic synapse. The classic description is a bull's eye with a central major histocompatibility (MHC)–T-cell receptor structure surrounded by a ring of lymphocyte function-associated antigen-1 and intercellular adhesion molecule 1 adhesion molecules.5 Further outside is a ring that includes CD45.6 In T cells, there are two main types of immunologic synapses, depending on the type of MHC complex and T-cell coreceptor: MHC II–CD4 and MHC I–CD8. CD8 T cells have cytotoxic function toward MHC I loaded with proteasome-degraded peptide. Our focus is on the MHC II–CD4 immunologic synapse.
The MHC II–CD4 immunologic synapse results in helper T-cell activation due to presentation of endocytosed antigen on the MHC II complex.7 Specialized antigen-presenting cells, such as dendritic cells and macrophages, endocytose antigens and load them onto MHC II, where they are recognized by naïve CD4-positive T lymphocytes. First, adhesion molecules pull the T cell and the target cell together.8 Then, the T-cell receptor binds to the MHC II–peptide complex, with CD4 functioning as a coreceptor. The MHC II–CD4 immunologic synapse is 15 nm across.9 Positive costimulatory molecules CD40, CD40 ligand, CD80/86, and CD28 aid the interaction,10 whereas negative costimulators programmed death ligand 1 (PDL1), program cell death protein 1 (PD-1), CD80, and CTLA-4 attenuate the interaction.11,12 Successful activation of CD4 T cells leads to differentiation into helper T cell subtypes, including types 1, 2, and 17 helper T cells (Th1, Th2, and Th17, respectively), that have more tailored immune responses.
Aberrant MHC II Production in Hepatocytes and Other Nonantigen-Presenting Cells
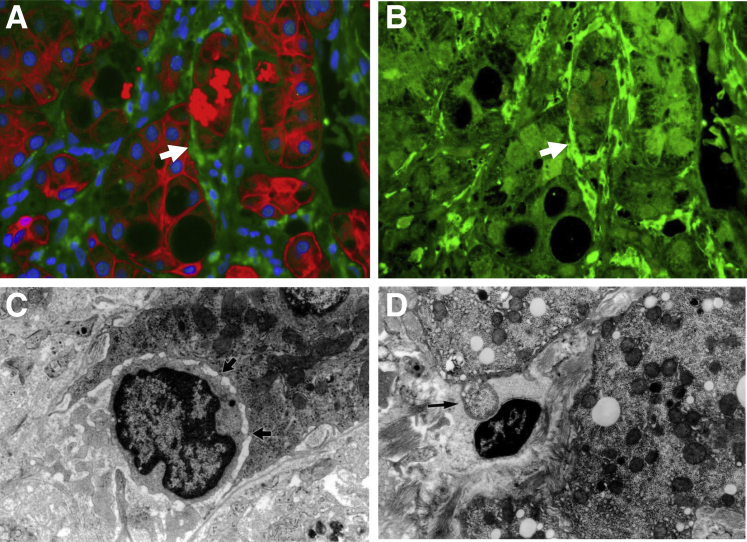
Although MHC II is classically thought to be found on antigen-presenting cells, it can also be present on other cell types. In skin, breast, lung, and kidney tissues, MHC II is normally present.13 MHC II can also be aberrantly present in various liver pathologies. In viral hepatitis and autoimmune hepatitis, hepatocytes aberrantly have higher levels of MHC II.14,15 In a series of pediatric liver biopsies, MHC II was aberrantly present on hepatocytes in 3 of 10 cases of autoimmune hepatitis and 5 of 9 cases of primary sclerosing cholangitis, but not in biliary atresia, α-1 antitrypsin deficiency, idiopathic neonatal hepatitis, or normal liver.16 Interestingly, the cases that showed aberrant hepatocyte MHC II were untreated patients. Also, hepatocytes in human biopsies of alcoholic hepatitis have increased levels of MHC II but not those in nonalcoholic steatohepatitis17,18 (Figure 1). In our study, the biopsies of alcoholic hepatitis also showed higher levels of interferon-γ and IL-1α compared with those of nonalcoholic steatohepatitis and normal controls.
Figure 1.
A: Aberrant major histocompatibility complex class II (MHC II) production (green) in a liver biopsy with alcoholic hepatitis. Note the Mallory body (arrow), which stains positively for CAM5.2 (red) in the hepatocyte coated with MHC II. Nuclei are stained with DAPI (blue). B: Same biopsy with only MHC II shown (green); note the pericellular distribution of MHC II in the hepatocyte with Mallory body (arrow). C: Electron micrograph of a lymphocyte indenting a hepatocyte and forming multiple immunologic synapses (arrows) with the hepatocyte. D: Electron micrograph from a case of autoimmune hepatitis with a lymphocyte surrounding a bleb (arrow) from a hepatocyte. C and D: Adapted from Wang et al18 with permission from Experimental and Molecular Pathology. Original magnification: ×780 (A and B); ×700 (C); ×24,000 (D).
The aberrant production of MHC II is triggered by interferon-γ.15 Once hepatocytes produce MHC II, they can express costimulatory molecules and activate CD4-positive lymphocytes, toward either a Th1 or a Th2 phenotype.19 By itself, aberrant MHC II production is not sufficient to cause autoimmune hepatitis,19 but it may enhance an already existing autoimmune response. It may also help bypass the normally immunotolerant microenvironment of the liver.20 Interestingly, MHC II production is also present on bile duct epithelium in primary biliary cirrhosis and primary sclerosing cholangitis.21
Aberrant MHC II production is also seen in other organs, usually in the autoimmune setting, with the level of expression tending to correlate with disease severity. In autoimmune thyroiditis, aberrant MHC II production is seen in thyrocytes and is associated with a slight increase in the severity of the autoimmune response compared with cases with no MHC II expression in thyrocytes.22 Similar to autoimmune hepatitis, MHC II production by itself was not sufficient to trigger autoimmune thyroiditis. Aberrant MHC II production is also seen in diabetic insulitis,23 autoimmune uveitis,24 adrenal atrophy,25 autoimmune gastritis,26 and rheumatoid arthritis–like joint disease.27 Misfolded cellular proteins are transported to the cell surface by MHC II molecules, a possible mechanism for autoimmune response.28 In the case of rheumatoid arthritis–like joint disease, transgenic mice that aberrantly produce MHC II did not spontaneously develop autoimmune joint disease, but they were highly susceptible to immunization with low doses of foreign protein (bovine collagen), whereas negative control mice did not respond to this stimulus. The aberrantly MHC II–producing mice developed joint disease phenotypically and histologically akin to rheumatoid arthritis.27
Aberrant MHC II production can also be seen in the neoplastic setting. Melanoma cells often aberrantly produce MHC II, which leads to a dampening of CD8 T-cell antitumor activity.29 In papillary thyroid carcinoma, higher levels of MHC II are inversely correlated with recurrence of carcinoma.30 In a study of triple-negative breast cancer, the presence of MHC II components is associated with progression-free survival.31 Among the genes with significantly higher expression in no relapse patients were CIITA, the activator of MHC II; CD74, the chaperone for MHC II; and various human leukocyte antigen (HLA) genes that express the components of MHC II. Histologically, this was correlated with tumor cells staining for CD74 and HLA-DPB1 protein and lymphocytic infiltrate. In addition to the aforementioned examples, MHC II production can be seen in tumor cells in colorectal carcinoma,32 squamous cell carcinoma,33 and osteosarcoma.34
The MHC II–CD4 Immunologic Synapse and Piecemeal Necrosis
To further understand the role of aberrant MHC II in liver pathology, it is necessary to understand piecemeal necrosis, which is the historical term for interface hepatitis.35 Normally, there is a sharp demarcation between the portal tract and surrounding cords of hepatocytes, which is termed the limiting plate. In interface hepatitis, this demarcation is disrupted and a predominantly mononuclear inflammatory cell infiltrate involves the hepatic sinusoids in the periportal regions.36 The hepatocytes in this area are gradually destroyed. This phenomenon is seen in various conditions, including autoimmune hepatitis, viral hepatitis, primary biliary cirrhosis, and liver transplant rejection.37 It is also observed in alcoholic hepatitis.38
The mechanism of hepatocyte damage varies by disease. However, there is a mixture of CD4- and CD8-positive T-lymphocyte infiltrate, of which CD4 lymphocytes are usually predominant.36 B cells are uncommon in these lymphocytic infiltrates.39 More important, when CD4-positive lymphocytes are activated through the MHC II–CD4 immunologic synapse, they can absorb molecules from the antigen-presenting cell, including MHC and the costimulatory molecule B7.40 This process is dependent on the actin cytoskeleton.41 It is also dependent on TC21 and RhoG, a GTPase involved in phagocytosis.42 Normally, CD4 T lymphocytes interact with antigen-presenting cells, but if hepatocytes can aberrantly express MHC II, this raises the question of whether CD4 lymphocytes can directly attack and phagocytose hepatocytes. Indeed, with their T-cell receptors, T cells can phagocytose beads 1 to 6 μm in diameter.42 For comparison, a hepatocyte is 20 to 30 μm in width; thus, the size and scale of this mechanism seem plausible.
To further investigate, we previously performed electron microscopy studies for piecemeal necrosis in viral hepatitis, autoimmune hepatitis, primary biliary cirrhosis, and steatohepatitis.18,43 Piecemeal necrosis requires formation of an immunologic synapse between the lymphocyte and hepatocyte as they closely associate with each other. The hepatocyte indents at the interface with the lymphocyte, and the lymphocytes eat hepatocytes piece by piece and digest them in their lysosomes. Microscopically one sees loss of liver cell volume and irregular pieces (nubbins) of hepatocytes dispersed through the sinusoidal area devoid of nuclear material. By electron microscopy, one sees lymphocytes indenting the cytoplasm and approaching the nucleus of hepatocytes. Other images show attachments between the plasma membranes of lymphocyte and hepatocyte, strongly suggestive of immunologic synapse formation. Furthermore, lymphocytes are seen surrounding blebs of neighboring hepatocytes, as though in the process of phagocytosing them, and phagosomes are seen within the cytoplasm of activated lymphocyte. This phenomenon was named troxis necrosis, deriving from the Greek verb trogo, meaning to eat, chew, gnaw, to reflect direct phagocytosis of hepatocytes by lymphocytes.18
MHC II is aberrantly produced in various hepatitis pathologies, and CD4 lymphocytes are the predominant lymphocytic infiltrate; the process of piecemeal necrosis is likely due to CD4 lymphocytes directly attacking and eating hepatocytes. For instance, CD4-positive lymphocytes closely associate with hepatocytes in alcoholic hepatitis, and electron microscopy showed them forming immunologic synapses with hepatocytes.17
Interestingly, a subset of CD4 lymphocytes has been shown to have direct cytotoxic activity.44,45 The CD4-positive cytotoxic T cells can derive from any subset of T-helper cells but usually arise from Th1 cells, which secrete interferon-γ and promote a cell-mediated response.46 The presence of CD4 cytotoxic lymphocytes may be protective in nature as some viruses can cause their host cells to underexpress MHC class I, thus evading CD8 cytotoxic T-lymphocyte response.47
Immunologic Synapse Formation in Autoimmune Hepatitis
Autoimmune hepatitis is diagnosed by a combination of clinical and pathologic features. The typical biopsy findings include a heavy portal inflammatory infiltrate and interface hepatitis, with plasma cells and eosinophils accompanying lymphocytes.48 Lobular hepatitis may also be seen. Drug-induced hepatitis has varying appearance, depending on the medication, but can show similar histologic features to autoimmune hepatitis.
The inflammatory infiltrate of autoimmune hepatitis typically shows CD4-positive lymphocytes in the portal tracts. The lymphocytic infiltrate at the area of interface hepatitis varies in immunophenotype. In one study, CD8-positive lymphocytes were predominant in the areas of interface hepatitis in contrast to the CD4-rich portal tracts.20 In another study, an analysis of 189 T-cell clones from four autoimmune hepatitis liver biopsies showed predominantly CD4+/CD8- clones, with a CD4/CD8 ratio of 2.0 to 3.8.48 Interestingly, some of the CD4-positive T-cell clones showed cytolytic activity, lending further support to the concept of cytotoxic T cells.49 An additional study of 12 pediatric liver biopsies for patients with autoimmune hepatitis also showed predominantly CD4-positive lymphocytes in the portal tract compared with CD8-positive lymphocytes.50 Interestingly, the autoimmune reaction occurs in spite of increased checkpoint inhibitor PD-1 expression on Kupffer cells.51
Immunologic synapse formation has been shown in autoimmune hepatitis with CD4-positive lymphocytes.43 In addition, in a case of drug-induced hepatitis secondary to immunomodulatory medications, CD4 lymphocytes were seen forming immunologic synapses with hepatocytes.52 This phenomenon was also seen in cases of hepatotoxicity due to black cohosh53 and from taking Herbalife weight loss supplements.54 Immunologic synapse formation from CD4-positive lymphocytes and MHC II–producing hepatocytes may be an important mechanism in autoimmune hepatitis that leads to direct phagocytosis of hepatocytes.
Autoimmune Mechanisms in Alcoholic Hepatitis
Alcoholic hepatitis is characterized histologically by steatosis, Mallory body formation, pericellular and perivenular fibrosis, and hepatocyte ballooning.48 In addition, it is associated with an immune response that is multifactorial in nature. Previously characterized mechanisms include lipopolysaccharide-induced acute inflammation due to increased gut epithelial membrane permeability,55 direct response to free fatty acids,56 and reactive oxygen species formation.57 In addition, the response is partly antibody mediated. Autoantibodies can be formed against cytochrome proteins CYP2E1 and CYPEA4,58,59 hydroxyethyl radical protein adducts,60 and acetaldehyde binding to cellular proteins.61
Overall, these mechanisms trigger a primarily acute inflammatory response with neutrophils and macrophages. Lymphocyte response in alcoholic hepatitis is less well described.62 However, increased levels of MHC II have recently been shown on hepatocellular membranes in biopsies of alcoholic hepatitis (Figure 1). Immunologic synapse formation has also been observed between CD4-positive lymphocytes and hepatocytes in these biopsies. Combined with previous findings regarding piecemeal necrosis in steatohepatitis, direct eating of hepatocytes by CD4-positive lymphocytes may be an important autoimmune mechanism seen in alcoholic hepatitis.18
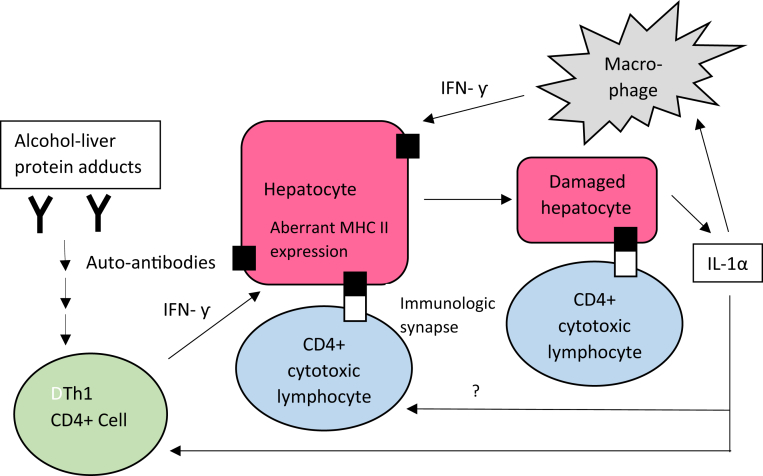
A proposed model for this autoimmunity can be seen in Figure 2. Exposure to alcohol leads to development of autoantibodies, which activate Th1 helper T cells in the traditional antigen-presenting cell pathway. Th1 cells secrete interferon-γ, leading to increased levels of MHC II in hepatocytes, which allows direct targeting of hepatocytes by CD4-positive cells. As hepatocytes are eaten and degraded, inflammatory cytokines, such as IL-1α, are released, which further activate CD4 lymphocytes, leading to a positive feedback loop. In addition, IL-1α recruits macrophages, which themselves secrete interferon-γ, leading to further MHC II expression on hepatocytes and additional positive feedback.
Figure 2.
Model for autoimmune mechanisms in alcoholic hepatitis. Autoantibodies to alcohol-liver protein adducts lead to a type 1 helper T-cell (Th1) response, leading to secretion of interferon-γ (IFN-γ). IFN-γ causes aberrant major histocompatibility complex class II (MHC II) production on hepatocytes, leading to targeting by CD4-positive cytotoxic lymphocytes. As hepatocytes are destroyed, they release IL-1α, which, among other effects, further enhances antigen-activated CD4+ T-cell response, generating a positive feedback loop.
Autoimmune Mechanisms in Primary Biliary Cirrhosis
Primary biliary cirrhosis is characterized pathologically by initial heavy portal inflammation with bile duct damage, followed by ductular proliferation, scarring with bridging fibrosis, and cirrhosis.54 Granulomas are sometimes seen. The inflammatory infiltrate is predominantly lymphocytic, with mostly CD4-positive T cells, and the overall appearance may mimic other forms of chronic hepatitis.
One study of 15 liver biopsies from patients with primary biliary cirrhosis showed expression of MHC II subregion genes (HLA-DP, HLA-DR, and HLA-DQ) on bile duct epithelial cells in early-stage disease.63 In advanced-stage disease, this expression decreased. In addition, four biopsies showed hepatocytes staining for HLA-DR. Another study found increased levels of MHC class I molecules in addition to aberrant HLA-DR expression.64 Furthermore, certain alleles of HLA-DR and HLA-DQ are associated with increased risk for primary biliary cirrhosis, whereas other alleles are considered protective.65 Thus, it appears that aberrant MHC II on bile duct epithelium plays a role in the early-stage pathology of this disease.
Summary and Diagnostic and Clinical Applications
Aberrant MHC II on hepatocytes or bile duct epithelium is a mechanism to amplify autoimmune response by CD4-positive lymphocytes and even lead to direct targeting and destruction by cytotoxic CD4 T lymphocytes. The lymphocytes form MHC II–CD4 immunologic synapses with hepatocytes and, in the process of internalizing these complexes, phagocytose the hepatocytes piece by piece. This is an additional autoimmune mechanism that appears to be involved in various pathologies, including autoimmune hepatitis, alcoholic hepatitis, and primary biliary cirrhosis.
There are several follow-up investigations. One is whether MHC II immunohistochemistry can be used for diagnostic purposes. As there is considerable overlap in the histologic appearance of viral hepatitis, autoimmune hepatitis, primary biliary cirrhosis, and primary sclerosing cholangitis, the presence of aberrant MHC II could be used to help differentiate between these conditions. In particular, viral hepatitis and autoimmune hepatitis would show aberrant MHC II on hepatocytes, whereas primary biliary cirrhosis and primary sclerosing cholangitis would show MHC II on bile duct epithelium. Given data from previous studies, this marker would likely have lower sensitivity but high specificity; it may have higher sensitivity in untreated patients.16
Second, we can investigate whether MHC II is aberrantly produced in hepatocellular carcinoma. One study investigated whether differential expression of individual genes and signaling pathway components correlated with recurrence-free survival for hepatocellular carcinoma.66 The authors found that MHC II–related antigen-presenting pathways significantly correlated with longer recurrence-free survival time. They note that MHC II molecules were found on CD68-positive (macrophage) and CD45-positive (lymphocyte) cells. Whether MHC II is present on tumor cells remains to be investigated, in addition to whether lymphocytes can be seen on electron microscopy, directly forming immunologic synapses with tumor cells.
Recent clinical trials have investigated use of pembrolizumab in advanced hepatocellular carcinoma. Pembrolizumab is an inhibitor of PD-1, a receptor that is expressed in lymphocytes and attenuates T-cell activation via the immunologic synapse. A nonrandomized, open-label, phase 2 trial of pembrolizumab for patients with hepatocellular carcinoma previously treated with sorafenib found that 17% of 104 treated patients had partial or complete response to the medication.67 This finding prompted a fast-track approval of pembrolizumab for this indication by the Food and Drug Administration. The phase 3 trial of pembrolizumab showed a trend toward improved overall survival and progression-free survival, although these findings were not statistically significant.68 Why do only some patients respond to pembrolizumab? One hypothesis is that some patients had higher levels of tumor MHC II; even if the inhibitory signal from PD-L1 is diminished by the medication, lymphocytes may not adequately target tumor cells if there is insufficient tumor MHC II. As pembrolizumab is an expensive medication, stratification of potential therapeutic response by a marker such as MHC II may lead to more cost-effective management.
Finally, in the setting of autoimmune liver pathologies, one wonders what mechanisms can attenuate MHC II–CD4 immunologic synapse formation and piecemeal necrosis. The adverse effects of CTLA-4 and PD-1 checkpoint inhibitors include reactions resembling autoimmune disease, including pruritis, rash, colitis, inflammation pneumonitis, and interstitial nephritis.69 These medications can also worsen already existing autoimmune disease,70 such as psoriasis.71 Type 1 diabetes has even been induced in the context of this medication.72 It stands to reason that the opposite action, enhancing checkpoint inhibitor CTLA-4 and PD-1 activity, would have the opposite effect of reducing autoimmunity. In addition, one can consider blocking the costimulatory molecule activity of CD28 and CD80, which theoretically would have a similar effect as enhancing checkpoint inhibitor activity. Further studies are needed to evaluate the feasibility and efficacy of such targeted therapies.
Footnotes
Supported by NIH/National Institute on Alcohol Abuse and Alcoholism grant UO-21898-05 (S.W.F.).
Disclosures: None declared.
References
- 1.Blanden R.V., Doherty P.C., Dunlop M.B., Gardner I.D., Zinkernagel R.M., David C.S. Genes required for cytotoxicity against virus-infected target cells in K and D regions of H-2 complex. Nature. 1975;254:269–270. doi: 10.1038/254269a0. [DOI] [PubMed] [Google Scholar]
- 2.Bjorkman P.J., Saper M.A., Samraoui B., Bennett W.S., Strominger J.L., Wiley D.C. Structure of the human class I histocompatibility antigen, HLA-A2. Nature. 1987;329:506–512. doi: 10.1038/329506a0. [DOI] [PubMed] [Google Scholar]
- 3.Monks C.R., Kupfer H., Tamir I., Barlow A., Kupfer A. Selective modulation of protein kinase C-theta during T-cell activation. Nature. 1997;385:83–86. doi: 10.1038/385083a0. [DOI] [PubMed] [Google Scholar]
- 4.Monks C.R., Freiberg B.A., Kupfer H., Sciaky N., Kupfer A. Three-dimensional segregation of supramolecular activation clusters in T cells. Nature. 1998;396:82–86. doi: 10.1038/25764. [DOI] [PubMed] [Google Scholar]
- 5.Dustin M.L., Springer T.A. Lymphocyte function-associated antigen-1 (LFA-1) interaction with intercellular adhesion molecule-1 (ICAM-1) is one of at least three mechanisms for lymphocyte adhesion to cultured endothelial cells. J Cell Biol. 1988;107:321–331. doi: 10.1083/jcb.107.1.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Johnson K.G., Bromley S.K., Dustin M.L., Thomas M.L. A supramolecular basis for CD45 tyrosine phosphatase regulation in sustained T cell activation. Proc Natl Acad Sci U S A. 2000;97:10138–10143. doi: 10.1073/pnas.97.18.10138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dustin M.L. The immunological synapse. Cancer Immunol Res. 2015;11:1023–1033. doi: 10.1158/2326-6066.CIR-14-0161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Springer T.A. Adhesion receptors of the immune system. Nature. 1990;346:425–434. doi: 10.1038/346425a0. [DOI] [PubMed] [Google Scholar]
- 9.Garcia K.C., Degano M., Stanfield R.L., Brunmark A., Jackson M.R., Peterson P.A., Teyton L., Wilson I.A. An alphabeta T cell receptor structure at 2.5 A and its orientation in the TCR-MHC complex. Science. 1996;274:209–219. doi: 10.1126/science.274.5285.209. [DOI] [PubMed] [Google Scholar]
- 10.Bromley S.K., Iaboni A., Davis S.J., Whitty A., Green J.M., Shaw A.S., Weiss A., Dustin M.L. The immunological synapse and CD28-CD80 interactions. Nat Immunol. 2001;2:1159–1166. doi: 10.1038/ni737. [DOI] [PubMed] [Google Scholar]
- 11.Krummel M.F., Allison J.P. CTLA-4 engagement inhibits IL-2 accumulation and cell cycle progression upon activation of resting T cells. J Exp Med. 1996;183:2533–2540. doi: 10.1084/jem.183.6.2533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ishida Y., Agata Y., Shibahara K., Honjo T. Induced expression of PD-1, a novel member of the immunoglobulin gene superfamily, upon programmed cell death. EMBO J. 1992;11:3887–3895. doi: 10.1002/j.1460-2075.1992.tb05481.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Drozina G., Kohoutek J., Jabrane-Ferrat N., Peterlin B.M. Expression of MHC II genes. Curr Top Microbiol Immunol. 2005;290:147–170. doi: 10.1007/3-540-26363-2_7. [DOI] [PubMed] [Google Scholar]
- 14.Dienes H.P., Hutteroth T., Hess G., Meuer S.C. Immunoelectron microscopic observations on the inflammatory infiltrates and HLA antigens in hepatitis B and non-A, non-B. Hepatology. 1987;7:1317–1325. doi: 10.1002/hep.1840070623. [DOI] [PubMed] [Google Scholar]
- 15.Franco A., Barnaba V., Natali P., Balsano C., Musca A., Balsano F. Expression of class I and class II major histocompatibility complex antigens on human hepatocytes. Hepatology. 1988;8:449–454. doi: 10.1002/hep.1840080302. [DOI] [PubMed] [Google Scholar]
- 16.Lobo-Yeo A., Senaldi G., Portmann B., Mowat A.P., Mieli-Vergani G., Vergani D. Class I and class II major histocompatibility antigen expression on hepatocytes: a study in children with liver disease. Hepatology. 1990;12:224–232. doi: 10.1002/hep.1840120208. [DOI] [PubMed] [Google Scholar]
- 17.Lu J.G., Iyasu A., French B., Tillman B., French S.W. Overexpression of MHCII by hepatocytes in alcoholic hepatitis (AH) compared to non-alcoholic steatohepatitis (NASH) and normal controls. Alcohol. 2019 doi: 10.1016/j.alcohol.2019.08.008. [Epub ahead of print] doi: 10.1016/j.alcohol.2019.08.008. [DOI] [PubMed] [Google Scholar]
- 18.Wang M.Y., Morgan T., Lungo W., Wang L., Sze G.Z., French S.W. “Piecemeal” necrosis: renamed troxis necrosis. Exp Mol Pathol. 2001;71:137–146. doi: 10.1006/exmp.2001.2397. [DOI] [PubMed] [Google Scholar]
- 19.Herkel J., Jagemann B., Wiegard C., Garcia Lazaro J.F., Lueth S., Kanzler S., Blessing M., Schmitt E., Lohse A.W. MHC class-II expressing hepatocytes function as antigen-presenting cells and activate specific CD4 T lymphocytes. Hepatology. 2003;37:1079–1085. doi: 10.1053/jhep.2003.50191. [DOI] [PubMed] [Google Scholar]
- 20.Horst A.K., Neumann K., Diehl L., Tiegs G. Modulation of liver tolerance by conventional and nonconventional antigen-presenting cells and regulatory immune cells. Cell Mol Immunol. 2016;13:277–292. doi: 10.1038/cmi.2015.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hashimoto E., Lindor K.D., Homburger H.A., Dickson E.R., Czaja A.J., Wiesner R.H., Ludwig J. Immunohistochemical characterization of hepatic lymphocytes in primary biliary cirrhosis in comparison with primary sclerosing cholangitis and autoimmune chronic active hepatitis. Mayo Clin Proc. 1993;68:1049–1055. doi: 10.1016/s0025-6196(12)60897-0. [DOI] [PubMed] [Google Scholar]
- 22.Kimura H., Kimura M., Tzou S.C., Chen Y.C., Suzuki K., Rose N.R., Caturegli P. Expression of class II major histocompatability complex molecules on thyrocytes does not cause spontaneous thyroiditis but mildly increases its severity after immunization. Endocrinology. 2005;146:1154–1162. doi: 10.1210/en.2004-1165. [DOI] [PubMed] [Google Scholar]
- 23.Londei M., Lamb J.R., Bottazzo G.F., Feldmann M. Epithelial cells expressing aberrant MHC class II determinants can present antigen to cloned human T cells. Nature. 1984;312:639–641. doi: 10.1038/312639a0. [DOI] [PubMed] [Google Scholar]
- 24.Lipski D.A., Dewispelaere R., Foucart V., Caspers L.E., Defrance M., Bruyns C., WIllermain F. MHC class II expression and potential antigen-presenting cells in the retinal during experimental autoimmune uveitis. J Neuroinflammation. 2017;14:136. doi: 10.1186/s12974-017-0915-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jackson R., McNicol A.M., Farquharson M., Foulis A.K. Class II MHC expression in normal adrenal cortex and cortical cells in autoimmune Addison's disease. J Pathol. 1988;155:113–120. doi: 10.1002/path.1711550207. [DOI] [PubMed] [Google Scholar]
- 26.Bockerstett K.A., Wong C.F., Koehm S., Ford E.L., DiPaolo R.J. Molecular characterization of gastric epithelial cells using flow cytometry. Int J Mol Sci. 2018;19:1096. doi: 10.3390/ijms19041096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kanazawa S., Ota S., Sekine C., Tada T., Otsuka T., Okamoto T., Sonderstrup G., Peterlin B.M. Aberrant MHC class II expression in mouse joints leads to arthritis with extraarticular manifestations similar to rheumatoid arthritis. Proc Natl Acad Sci U S A. 2006;103:14465–14470. doi: 10.1073/pnas.0606450103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Arase H., Jin H., Tanimura K., Suenaga T., Arase N., Lanier L.L. Cellular misfolded proteins transported to the cell surface by aberrantly expressed MHC class II molecules are major autoantibody targets in autoimmune diseases. J Immunol. 2017;198 Suppl 1 156.20. [Google Scholar]
- 29.Donia M., Andersen R., Kjeldsen J.W., Fagone P., Munir S., NIcoletti F., Andersen M.H., Thor Straten P., Svane I.M. Aberrant expression of MHC class II in melanoma attracts inflammatory tumor-specific CD4+ T-cells, which dampen CD8+ T cell antitumor reactivity. Cancer Res. 2015;75:3747–3759. doi: 10.1158/0008-5472.CAN-14-2956. [DOI] [PubMed] [Google Scholar]
- 30.Jo Y.S., Lee J.C., Li S., Choi Y.S. Significance of the expression of major histocompatibility complex class II antigen, HLA-DR and -DQ, with recurrence of papillary thyroid cancer. Int J Cancer. 2008;122:785–790. doi: 10.1002/ijc.23167. [DOI] [PubMed] [Google Scholar]
- 31.Forero A., Li Y., Chen D., Grizzle W.E., Updike K.L., Merz N.D., Downs-Kelly E., Burwell T.C., Vaklavas C., Buchsbaum D.J., Myers R.M., LoBuglio A.F., Varley K.E. Expression of the MHC class II pathway in triple-negative breast cancer tumor cells is associated with a good prognosis and infiltrating lymphocytes. Cancer Immunol Res. 2016;4:390–399. doi: 10.1158/2326-6066.CIR-15-0243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Degener T., Momburg F., Moller P. Differential expression of HLA-DR, HLA-DP, HLA-DQ and associated invariant chain (Ii) in normal colorectal mucosa, adenoma and carcinoma. Virchows Arch A Pathol Anat Histopathol. 1988;412:315–322. doi: 10.1007/BF00750257. [DOI] [PubMed] [Google Scholar]
- 33.Nasman A., Andersson E., Marklund L., Tertipis N., Hammarstedt-Nordenvall L., Attner P., Nyberg T., Masucci G.V., Munck-Wikland E., Ramqvist T., Dalianis T. HLA class I and II expression in oropharyngeal squamous cell carcinoma in relation to tumor HPV status and clinical outcome. PLoS One. 2013;8:e77025. doi: 10.1371/journal.pone.0077025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhou Q., Xu J., Zhao J., Zhang S., Pan W. Downregulation of CD99 and upregulation of human leukocyte antigen class II promote tumor aggravation and poor survival in patients with osteosarcomas. Onco Targets Ther. 2014;7:477–484. doi: 10.2147/OTT.S54765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Popper H. Mechanism of cell and tissue damage produced by immune reactions. In: Miescher G.P., editor. Second International Symposium on Immunopathology. Grune and Stratton; New York, NY: 1962. p. 303. [Google Scholar]
- 36.Czaja A.J., Carpenter H.A. Histologic findings in chronic hepatitis C with autoimmune features. Hepatology. 1997;26:459–466. doi: 10.1002/hep.510260229. [DOI] [PubMed] [Google Scholar]
- 37.Si L., Whiteside T.L., VanThiel D.H., Rabin B.S. Lymphocytic subpopulations at the site of “piecemeal” necrosis in the end state chronic liver diseases and rejecting liver allografts in the cyclosporin-treated patients. Lab Invest. 1984;50:341. [PubMed] [Google Scholar]
- 38.French S.W., Nash S., Shitabata P., Kachi K., Hara C., Chedid A., Mendenhall C.L. Pathology of alcoholic liver disease. Semin Liver Dis. 1993;13:154–169. doi: 10.1055/s-2007-1007346. [DOI] [PubMed] [Google Scholar]
- 39.Alexander G., Williams R. Characterization of the mononuclear cell infiltrate in piecemeal necrosis. Lab Invest. 1984;50:247. [PubMed] [Google Scholar]
- 40.Huang J.F., Yang Y., Sepulveda H., Shi W., Hwang I., Peterson P.A., Jackson M.R., Sprent J., Cai Z. TCR-mediated internalization of peptide-MHC complexes acquired by T cells. Science. 1999;286:952. doi: 10.1126/science.286.5441.952. [DOI] [PubMed] [Google Scholar]
- 41.Hwang I., Sprent J. Role of the actin cytoskeleton in T cell absorption and internalization of ligands from APC. J Immunol. 2001;166:5099–5107. doi: 10.4049/jimmunol.166.8.5099. [DOI] [PubMed] [Google Scholar]
- 42.Martinez-Martin N., Fernandez-Areans E., Cemerski S., Delgado P., Turner M., Heuser J., Irvine D.J., Huang B., Bustelo X.R., Shaw A., Alarcon B. T cell receptor internalization from the immunological synapse is mediated by TC21 and RhoG GTPase-dependent phagocytosis. Immunity. 2011;35:208–222. doi: 10.1016/j.immuni.2011.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.French S.W., Lu J.G. Piecemeal necrosis is due to the immunologic synapse formation and internalization of intact TCR-MHCII complexes by CD4 T cells. Exp Mol Pathol. 2018;105:150–152. doi: 10.1016/j.yexmp.2018.07.004. [DOI] [PubMed] [Google Scholar]
- 44.Takeuchi A., Saito T. CD4 CTL, a cytotoxic subset of CD4+ T cells, their differentiation and function. Front Immunol. 2017;8:194. doi: 10.3389/fimmu.2017.00194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Aslan N., Yurdaydin C., Wiegand J., Greten T., Ciner A., Meyer M.F., Heiken H., Kuhlmann B., Kaiser T., Bozkaya H., Tillman H.L., Bozdayi A.M., Manns M.P., Wedemeyer H. Cytotoxic CD4 T cells in viral hepatitis. J Viral Hepat. 2006;13:505–514. doi: 10.1111/j.1365-2893.2006.00723.x. [DOI] [PubMed] [Google Scholar]
- 46.Appay V., Zaunders J.J., Papagno L., Sutton J., Jaramillo A., Waters A., Easterbrook P., Grey P., Smith D., McMichael A.J., Cooper D.A., Rowland-Jones S.L., Kelleher A.D. Characterization of CD4(+) CTLs ex vivo. J Immunol. 2002;168:5954–5958. doi: 10.4049/jimmunol.168.11.5954. [DOI] [PubMed] [Google Scholar]
- 47.Juno J.A., van Bockel D., Kent S.J., Kelleher A.D., Zaunders J.J., Munier C.M. Cytotoxic CD4 T cells: friend or foe during viral infection? Front Immunol. 2017;8:19. doi: 10.3389/fimmu.2017.00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Geller S.A., Petrovic L.M. Lippincott Williams & Wilkins; Philadelphia, PA: 2009. Biopsy Interpretation of the Liver; pp. 163–170. [Google Scholar]
- 49.Lohr H., Manns M., Kyriatsoulis A., Lohse A.W., Trautwein C., Meyer zum Buschenfelde K.H., Fleischer B. Clonal analysis of liver-infiltrating T cells in patients with LKLM-1 antibody-positive autoimmune chronic active hepatitis. Clin Exp Immunol. 1991;84:297–302. doi: 10.1111/j.1365-2249.1991.tb08164.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Senaldi G., Portmann B., Mowat A.P., Wieli-Vergani G., Vergani D. Immunohistochemical features of the portal tract mononuclear cell infiltrate in chronic aggressive hepatitis. Arch Dis Child. 1992;67:1447–1453. doi: 10.1136/adc.67.12.1447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Oikawa T., Takahashi H., Ishikawa T., Hokari A., Otsuki N., Azuma M., Zeniya M., Tajiri H. Intrahepatic expression of the co-stimulatory molecules programmed death-1, and its ligands in autoimmune liver disease. Pathol Int. 2007;57:485–492. doi: 10.1111/j.1440-1827.2007.02129.x. [DOI] [PubMed] [Google Scholar]
- 52.Wei C.H., Penunun A., Karpouzas G., Fleishman W., Datta A., French S.W. Troxis necrosis, a novel mechanism for drug-induced hepatitis secondary to immunomodulatory therapy. Exp Mol Pathol. 2016;99:341–343. doi: 10.1016/j.yexmp.2015.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Enbom T.E., Le M.D., Oesterich L., Rutgers J., French S.W. Mechanism of hepatotoxicity due to black cohosh and electron microscopy analysis of two liver biopsies with clinical correlation. Exp Mol Pathol. 2014;96:279–283. doi: 10.1016/j.yexmp.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 54.Chen G.C., Ramanthan Y.S., Law D., Funchain P., Chen G.C., French S., Shlopov B., Eysselein V., Chung D., Reicher S., Pham B.V. Acute liver injury induced by weight-loss herbal supplements. World J Hepatol. 2010;12:410–415. doi: 10.4254/wjh.v2.i11.410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rao R. Endotoxemia and gut barrier dysfunction in alcoholic liver disease. Hepatology. 2009;50:638–644. doi: 10.1002/hep.23009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mavrelis P.G., Ammon H.V., Gleysteen J.J., Komorowski R.A., Charaf U.K. Hepatic free fatty acids in alcoholic liver disease and morbid obesity. Hepatology. 1983;3:226–231. doi: 10.1002/hep.1840030215. [DOI] [PubMed] [Google Scholar]
- 57.Lakshminarayanan V., Beno D.W., Costa R.H., Roebuck K.A. Differential regulation of interleukin-8 and intercellular adhesion molecule-1 by H2O2 and tumor necrosis factor-alpha in endothelial and epithelial cells. J Biol Chem. 1997;272:32910–32918. doi: 10.1074/jbc.272.52.32910. [DOI] [PubMed] [Google Scholar]
- 58.Lytton S.D., Helander A., Zhang-Gouillon Z.Z., Stokkeland K., Bordone R., Arico S., Albano E., French S.W., Ingelman-Sundberg M. Autoantibodies against cytochromes P-4502E1 and P-4503A in alcoholics. Mol Pharmacol. 1999;55:223–233. doi: 10.1124/mol.55.2.223. [DOI] [PubMed] [Google Scholar]
- 59.Albano E., French S.W., Ingelman-Sundberg M. Cytochrome P4502E1, hydroxyethyl free radicals, and immune reactions associate with alcoholic liver disease. Alcohol Clin Exp Res. 1998;22:739–742. [Google Scholar]
- 60.Albano E., French S.W., Ingelman-Sundberg M. Hydroxyethyl radicals in ethanol hepatotoxicity. Front Bio Sci. 1999;4:dA533–dA540. doi: 10.2741/albano. [DOI] [PubMed] [Google Scholar]
- 61.Worrall S., De Jersey J., Shanley B.C., Wilce P.A. Ethanol induces the production of antibodies to acetaldehyde-modified epitopes in rats. Alcohol. 1989;24:217–223. [PubMed] [Google Scholar]
- 62.Wang H.J., Gao B., Zakhari S., Nagy L.E. Inflammation in alcoholic liver disease. Annu Rev Nutr. 2012;32:343–368. doi: 10.1146/annurev-nutr-072610-145138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Spengler U., Pape G.R., Hoffman R.M., Johnson J.P., Eisenburg J., Paumgartner G., Riethmuller G. Differential expression of MHC class II subregion products on bile duct epithelial cells and hepatocytes in patients with primary biliary cirrhosis. Hepatology. 1988;8:459–462. doi: 10.1002/hep.1840080304. [DOI] [PubMed] [Google Scholar]
- 64.Van der Ord J.J., Sciot R., Desmet V.J. Expression of MHC products by normal and abnormal bile duct epithelium. J Hepatol. 1986;3:310–317. doi: 10.1016/s0168-8278(86)80483-4. [DOI] [PubMed] [Google Scholar]
- 65.Webb G.J., Siminovitch K.A., Hirschfield G.M. The immunogenetics of primary biliary cirrhosis: a comprehensive review. J Autoimmun. 2015;64:42–52. doi: 10.1016/j.jaut.2015.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Xie X.W., Mei M.H., Liao W.J., Qian L.H., Yu X., Fei R., Qin L.L., Zhang H.H., Peng J.R., Shen D.H., Wei L., Chen S. Expression of CIITA-related MHCII molecules in tumors linked to prognosis in hepatocellular carcinoma. Int J Oncol. 2009;34:681–688. doi: 10.3892/ijo_00000194. [DOI] [PubMed] [Google Scholar]
- 67.Zhu A.X., Finn R.S., Edeline J., Cattan S., Ogasawara S., Palmer D., Verslype C., Zagonel V., Fartoux L., Vogel A., Sarker D., Verset G., Chan S.L., Knox J., Daniele B., Webber A.L., Ebbinghaus S.W., Ma J., Siegal A.B., Cheng A.L., Kudo M., KEYNOTE-224 investigators Pembrolizumab in patients with advanced hepatocellular carcinoma previously treated with sorafenib (KEYNOTE-224): a non-randomised, open-label phase 2 trial. Lancet Oncol. 2018;19:940–952. doi: 10.1016/S1470-2045(18)30351-6. [DOI] [PubMed] [Google Scholar]
- 68.Finn S.R., Baek-Yeol R., Philippe M., Kudo M., Bouattour M., Lim H.Y., Vladimirovich Breder V., Edeline J., Chao Y., Ogasawara S., Yau T., Garrido M., Chan S.L., Knox J.J., Daniele B., Ebbinghaus S., Chen E., Siegel A.B., Zhu A.X., Cheng A.L. Results of KEYNOTE-240: phase 3 study of pembrolizumab (Pembro) vs best supportive care (BSC) for second line therapy in advanced hepatocellular carcinoma (HCC) J Clin Oncol. 2019;37:4004. [Google Scholar]
- 69.Larkin J., Chiarion-Sileni V., Gonzalez R., Grob J.J., Cowey L., Lao C.D., Schadendorf D., Dummer R., Smylie M., Rutkowski P., Ferrucci P.F., Hill A., Wagstaff J., Carlino M.S., Haanen J.B., Maio M., Marquez-Rodas I., McArther G.A., Ascierto P.A., Long G.V., Callahan M.K., Postow M.A., Grossman K., Sznol M., Dreno B., Bastholt L., Yang A., Rollin L.M., Horak C., Hodi F.S., Wolchok J.D. Combined nivolumab and ipilimumab or monotherapy in untreated melanoma. N Engl J Med. 2015;373:23–34. doi: 10.1056/NEJMoa1504030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Johnson D.B., Beckermann K.E., Wang D.Y. Immune checkpoint inhibitor therapy in patients with autoimmune disease. Oncology (Williston Park) 2018;32:190–194. [PubMed] [Google Scholar]
- 71.Kato Y., Otsuka A., Miyachi Y., Kabashima K. Exacerbation of psoriasis vulgaris during nivolumab for oral mucosal melanoma. J Eur Acad Dermatol Venereol. 2016;30:e89–e91. doi: 10.1111/jdv.13336. [DOI] [PubMed] [Google Scholar]
- 72.Chae Y.K., Chiec L., Mohindra N., Gentzler R., Patel J., Giles F. A case of pembrolizumab-induced type-1 diabetes mellitus and discussion of immune checkpoint inhibitor-induced type 1 diabetes. Cancer Immunol Immunother. 2017;66:25–32. doi: 10.1007/s00262-016-1913-7. [DOI] [PMC free article] [PubMed] [Google Scholar]