Abstract
Introduction
Individuals with chronic kidney disease (CKD) generally have poor participation in self-care. We hypothesized that greater kidney disease knowledge and health literacy would associate with better self-care.
Methods
We enrolled 401 participants with non–dialysis-dependent CKD from one academic center in this cross-sectional study. Validated surveys were used to assess health literacy level (inadequate vs. adequate; Rapid Estimate of Adult Literacy in Medicine), perceived kidney disease knowledge (Perceived Kidney Disease Knowledge Survey [PiKS]), objective kidney disease knowledge (Kidney Disease Knowledge Survey [KiKS]), and a CKD self-care measure was constructed as the sum of self-reported self-care behaviors using the adapted Summary of Diabetes Self-Care Activities Assessment. The association between health literacy level, PiKS scores, KiKS scores, and the CKD self-care measure was assessed with multivariable adjusted linear regression models.
Results
Participants had a mean age of 57 years and 17.7% had inadequate health literacy. PiKS scores were positively associated with the CKD self-care measure (β = 1.05, 95% confidence interval [CI] 0.50–1.63), and a positive trend was observed for KiKS scores and the CKD self-care measure (β = 0.30, 95% CI: −0.12 to 0.72). Health literacy was not associated with CKD self-care measure.
Conclusion
Objective kidney disease knowledge is likely necessary, but not sufficient for self-care and may depend on the level of health literacy. Perceived kidney knowledge may offer a novel target to assess patients at risk for poor self-care, and be used in targeted educational interventions.
Keywords: health literacy, kidney disease knowledge, perceived kidney disease knowledge, self-care, self-efficacy, self-management
CKD affects approximately 26 million people in the United States.1 Many of the strategies aimed to optimize kidney disease management rely heavily on patient self-care behaviors, including adhering to medications and making lifestyle modifications.2 Self-care among individuals with dialysis-dependent kidney disease has been linked to overall improved physical functioning and well-being.3,4 In a recent meta-analysis, self-management interventions among individuals with nondialysis CKD were observed to be beneficial for urine protein decline, blood pressure level, and exercise capacity.5 Yet, individuals with CKD generally have poor participation in self-care behaviors, for reasons that have not yet been well described.6
In chronic disease populations outside of CKD, such as diabetes and heart failure, health literacy and disease-specific knowledge have been reported to be integral to self-care practices.7 Health literacy is defined as the ability “to obtain, process, and understand the basic health information and services needed to make appropriate health decisions.”8 Over the past 2 decades, health literacy has been increasingly recognized to influence the ability of patients to take action and navigate within their social networks and health systems. Health literacy may be particularly important for patients with kidney disease because of the complexity of self-care required to improve cardiovascular, metabolic, hematologic, and other complications they face. Inadequate health literacy is quite common (∼23%)9 in CKD, and low health literacy has been cross-sectionally associated with lower estimated glomerular filtration rate10 and poorer cardiovascular risk profiles10 among patients with non–dialysis-dependent CKD. Among those with end-stage kidney disease, lower health literacy has been associated longitudinally with higher rates of hospitalization11 and mortality.12 Unfortunately, many patients with kidney disease, even those under the care of nephrologists, also lack knowledge on basic concepts about how the kidneys function, and kidney disease in general. Low patient kidney disease knowledge has been associated with worse clinical outcomes, including less use of permanent dialysis access.13 Despite the proposed influence of health literacy and kidney disease knowledge on self-care behaviors, little is known about how either relates to self-care practices in patients with CKD.
In this study, we examined the association of 2 types of kidney disease knowledge (perceived and objective), health literacy, and self-care behaviors among adults with non–dialysis-dependent CKD. We hypothesized that greater kidney disease knowledge and adequate health literacy would be associated with higher levels of self-care behavior participation.
Methods
This cross-sectional study used surveys to assess the level of health literacy, perception of kidney disease knowledge, objective kidney disease knowledge, and self-care behaviors among adults with established non–dialysis-dependent CKD recruited from nephrology clinics, both attending (9) and fellow-led (16) clinics, within 1 large academic nephrology center from April 2009 through October 2010 (n = 401). Patients were screened within 1 week of an upcoming follow-up nephrology visit for eligibility criteria, which included a diagnosis of CKD stages 1 to 5, the ability to speak and read English, and at least 1 encounter with a nephrologist in the clinic. To determine CKD stage, the most recent serum creatinine level and urine protein measurement were extracted from the medical record. The serum creatinine was used to estimate GFR with the 4-variable Modification of Diet in Renal Disease equation,14 and CKD stage was determined using the National Kidney Foundation Kidney Disease Outcomes Quality Initiative guidelines.15 Patients were ineligible if they had a preexisting cognitive or vision impairment, a kidney transplant, or were currently receiving dialysis, as it was felt their disease-specific knowledge might include topics outside the scope of general CKD knowledge. Patients were sequentially recruited if they met inclusion criteria, their nephrologist agreed, and they were amenable to be consented. Several patients were excluded by the nephrologists on the basis of severe illness or cognitive dysfunction. Please see Supplementary Figure S1 for the flow diagram. The sample size was guided by the validation of the KiKS and the PiKS.16,17 After the clinic visit and not in the presence of the nephrologist, patients completed surveys in a private area, with a trained research assistant available nearby for assistance. The Vanderbilt University Institutional Review Board approved the study and written informed consent was obtained from all participants and is in accordance with the Declaration of Helsinki.
Health Literacy, Kidney Disease Knowledge, and Covariate Measures
Health literacy was assessed using the Rapid Estimate of Adult Literacy in Medicine, which was delivered by trained research personnel.18 The Rapid Estimate of Adult Literacy in Medicine score (range 0 to 66) was calculated by awarding 1 point for each correctly pronounced word, and 0 for each mispronounced or skipped word. A score of 59 or less defined low health literacy, whereas a score of 60 or more indicated adequate health literacy.18 If patients screened for low health literacy, they were then offered to have the survey read to them. Objective knowledge of kidney disease was assessed with the validated 28-item KiKS, which measured knowledge about many topics integral to self-care practices and prevention of CKD progression. The KiKS score was determined as the percentage of correct responses (0–1).16 The perception of kidney disease knowledge was assessed with the PiKS in which participants rated their knowledge on a 9-item scale from 1 (“I don’t know anything”) to 4 (“I know a lot”) about areas relevant to CKD management.17 The PiKS score was determined as an average of the 9 ratings (range 0 to 4). The remaining survey questions were related to sociodemographic factors (age, sex, race, ethnicity, education, income level), and medical history and health status (body mass index, diabetes, hypertension, awareness of CKD diagnosis, urine protein-to-creatinine ratio, number of times seen by a nephrologist in 1 year).
Self-Care Behavior Measures
Nine self-care behavior measures (general “healthful” diet consumption, fruits/vegetables intake, high-fat diet intake, physical activity participation, smoking, medication adherence, nephrotoxin avoidance, blood glucose testing, and foot care) were collected with survey questions adapted for CKD and guided by the validated Summary of Diabetes Self-Care Activities Assessment, as well as its scoring system, with a higher score indicative of better self-care.19 The self-care behaviors were scored as number of days of the past 7 the participant reported engaging in the behavior (range 0–7 days), and reverse scoring was implemented in a manner similar to the Summary of Diabetes Self-Care Activities Assessment for poor self-care behavior responses (Table 1). The dichotomous self-care behavior of smoking was scored 0 for current smoking and 7 for nonsmoking.
Table 1.
Assessment and scoring of individual and composite self-care behaviors
| Individual self-care behaviors | Corresponding survey assessment | Composite self-care behavior scores |
|---|---|---|
| Diet behavior scorea | “Followed a healthful eating plan” “Eat 5 or more servings of fruits and vegetables” “Eat high-fat foods, such as red meat or full-fat dairy products”b |
General CKD self-care score |
| Exercise behaviorsa | “Daily physical activity of at least 30 minutes” “Participated in a specific exercise session (e.g., swimming, walking, biking) outside of work” |
General CKD self-care score |
| Smoking behaviorc | “Have you smoked a cigarette, even one puff, during the past 7 days?” | General CKD self-care score |
| Medication adherence behaviora | “Taking medications exactly as prescribed” “Taking medication differently from prescribed”b “Not taking a prescribed medication”b |
General CKD self-care score |
| Nephrotoxin avoidance behaviora | “Taking over-the-counter or prescribed nonsteroidal anti-inflammatory medications or herbs”b “Taking nonprescribed vitamins or other natural remedies”b |
General CKD self-care score |
| Blood glucose testing behaviord | “Tested your blood sugar” “Testing the recommended times per day” |
Diabetes-related self-care score |
| Foot care behaviord | “Checked your feet” | Diabetes-related self-care score |
Scored as the mean of reported days (0–7) in the previous week participated in each behavior.
Reported days (0–7) scored in reverse.
If “yes,” scored as “0,” and if “no,” scored as “7.”
Scored as reported days (0–7); participants with diabetes (n = 145).
To create a summary measure of self-care behaviors, we combined the individual self-care behavior scores to create a 5-item general CKD self-care summary score, which included the following: the mean of 3 diet behaviors, physical activity participation, nonsmoking, medication adherence, and nephrotoxin avoidance (range 0–35) (Table 1). If the participant reported having diabetes, a diabetes-related CKD self-care summary score was constructed with the 5-item general CKD self-care score and incorporating glucose testing, foot care, and including diabetes medication adherence into the medication adherence score, range 0 to 49 (Table 1). We decided to give equal weight to each component of the self-care score because there has not been conclusive evidence on the prioritization of behaviors for the management of CKD.
Statistical Analyses
The study population was described using means, SDs, medians, interquartile ranges (IQRs), and percentages (%), with differences across key characteristics assessed using Pearson’s χ2 and Kruskal-Wallis tests as appropriate.
Differences in median summary scores were tested with the Mann-Whitney test for subgroups with adequate (vs. inadequate) health literacy and diabetes (vs. without diabetes). Unadjusted linear regression models and models adjusted for covariates thought to influence self-care behaviors (sex, age, race, education, income, estimated glomerular filtration rate, urine protein-to-creatinine ratio, hypertension, diabetes, body mass index, CKD awareness, and times seen by a nephrologist in past year) were used to examine the association of health literacy, KiKS and PiKS scores with self-care behaviors, and then further adjusted for health literacy, and KiKS and PiKS scores.
In addition, we evaluated health literacy (adequate vs. inadequate) as a potential effect modifier of the association between KiKS and PiKS, and the general and diabetes-related CKD self-care summary scores because health knowledge has been linked with level of health literacy.20 We also evaluated if the stage of CKD (stage 1–2 vs. stage 3 vs. stage 4–5) was a potential effect modifier of the relationship between health literacy and PiKS and KiKS with CKD self-care summary scores, because self-care behaviors may not be constant across the stages of CKD. In addition, we assessed if the associations among KiKS, PiKS, and healthy literacy were differentially related based on race (white vs. nonwhite) or socioeconomic level (income ≤$55,000 vs. >$55,000 per year). Another secondary analysis assessed for the association of health literacy, PiKS, and KiKS with the individual self-care behaviors. A sensitivity analysis was performed using a general CKD self-care summary score that included individual diet behaviors instead of a mean of the diet behaviors to assess the consistency with the primary results. All analyses were performed using STATA, version 11.2 (StataCorp, College Station, TX).
Results
The baseline characteristics of the 401 participants overall and those with diabetes (n = 145) are reported in Table 2. Overall, nearly one-quarter (22.9%) had CKD stage 1 to 2 and 38.2% had diabetes. There was complete data except for proteinuria (14.2%), body mass index (9.5%), smoking status and income (5.2% missing), hypertension and education (1.7% missing), and awareness of CKD diagnosis (0.5%).
Table 2.
Baseline characteristics of the study population overall and participants with diabetes
| Baseline characteristics | Overall (n = 401) | With diabetes (n = 145) |
|---|---|---|
| Age, yr, mean (SD) | 56.7 (15.8) | 59.7 (12.7) |
| Female, % | 46.9 | 45.5 |
| Race, % | ||
| White | 83.0 | 80.7 |
| Nonwhite | 17.0 | 19.3 |
| Annual income, % | ||
| ≤$25,000 | 18.7 | 18.8 |
| >$25,000 to ≤$55,000 | 33.7 | 37.7 |
| >$55,000 | 47.6 | 43.5 |
| Education level, % | ||
| Less than high school | 6.5 | 4.8 |
| High school and higher | 93.5 | 95.2 |
| CKD status, % | ||
| Stages 1–2 | 22.9 | 12.5 |
| Stage 3 | 48.9 | 53.1 |
| Stages 4–5 | 28.2 | 34.5 |
| Baseline eGFR, ml/min per 1.732, mean (SD) | 46.2 (25.5) | 39.8 (18.6) |
| Urine protein-to-creatinine ratio, mean (SD) | 0.78 (1.85) | 0.83 (1.45) |
| Aware of CKD diagnosis, % | 95.5 | 94.4 |
| Times seen nephrologist in past year, % | ||
| 0–1 | 17.5 | 13.8 |
| 2 | 22.9 | 21.4 |
| 3 | 23.9 | 26.2 |
| 4 | 33.9 | 35.9 |
| Diabetes, % | 38.2 | 100 |
| Hypertension, % | 85.8 | 89.5 |
| Body mass index, kg/m2, mean (SD) | 31.1 (7.8) | 33.9 (8.3) |
| Current smoker, % | 9.0 | 5.5 |
| Perceived knowledge score, median (IQR) | 2.6 (2.1–3.0) | 2.6 (2.1–3.0) |
| Objective knowledge score, median (IQR) | 0.68 (0.57–0.75) | 0.68 (0.57–0.79) |
| Inadequate health literacy, % | 17.7 | 17.9 |
CKD, chronic kidney disease; eGFR, estimated glomerular filtration rate.
Perceived knowledge score range (0–4); objective knowledge score range (0–1).
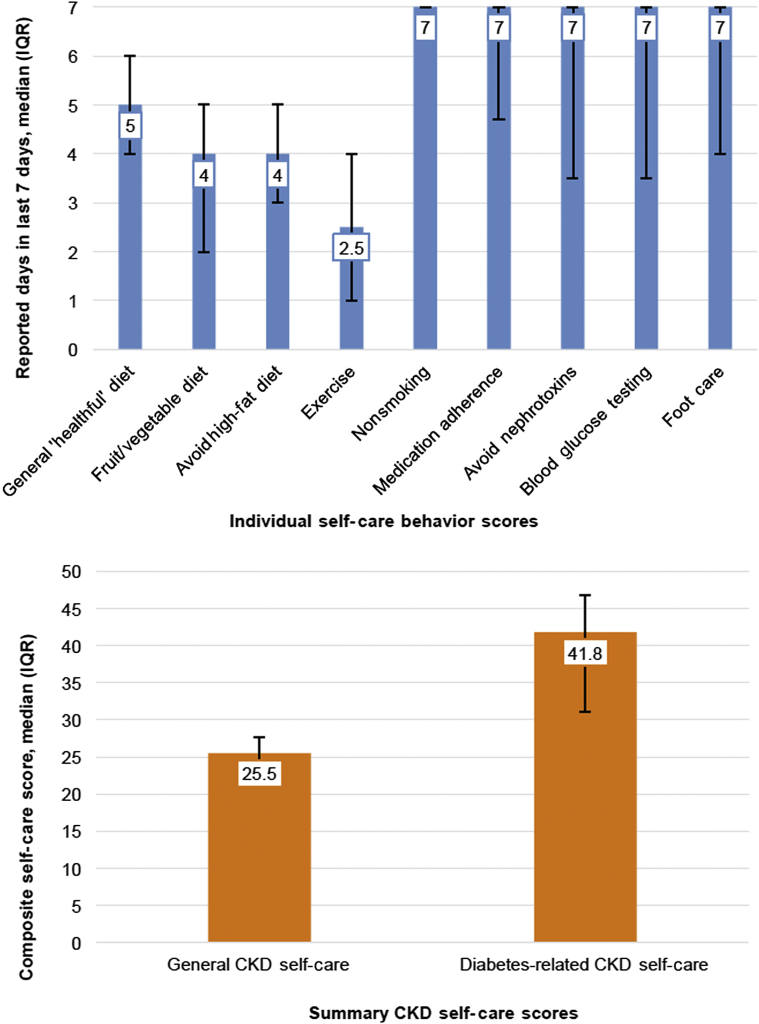
In the previous week, participants reported a median of 5 days consuming a general “healthful” diet (IQR 4–6 days) and 4 days of eating ≥5 servings of fruits and vegetables (IQR 2–5 days), as well as fewer than 3 days of physical activity (median 2.5 [IQR 1–4] days) (Figure 1; Supplementary Table S1). Participants reported median daily medication adherence and avoidance of nephrotoxins (7 [IQR 4.7–7] and 7 [IQR 3.5–7] days, respectively) in the previous week. Among those with diabetes, more than 50% reported checking their blood sugar and feet daily basis (7 [IQR 3.5–7] and 7 [IQR 4–7] days, respectively) in the past week.
Figure 1.
Scores of individual self-care behavior (upper panel) and summary chronic kidney disease (CKD) self-care behavior measures (lower panel), reported as median, and error bars indicate interquartile range (IQR).
For all participants, the median general CKD self-care summary score was 25.5 (IQR 22.5–27.7) (Figure 1). Participants with diabetes reported a lower median CKD self-care summary score than those without diabetes, but this was not statistically significant (25.3 [IQR 22.7–27.8] vs. 25.7 [IQR 22.5–27.8]; P = 0.69). Median CKD self-care summary scores did not differ significantly between those with inadequate and adequate health literacy (24.7 [21.3–26.8] vs. 25.7 [22.7–27.8], respectively; P = 0.11). The median diabetes-related CKD self-care summary score was 41.8 (IQR 31.0–46.8) (Figure 1), and scores did not differ depending on health literacy (P = 0.46).
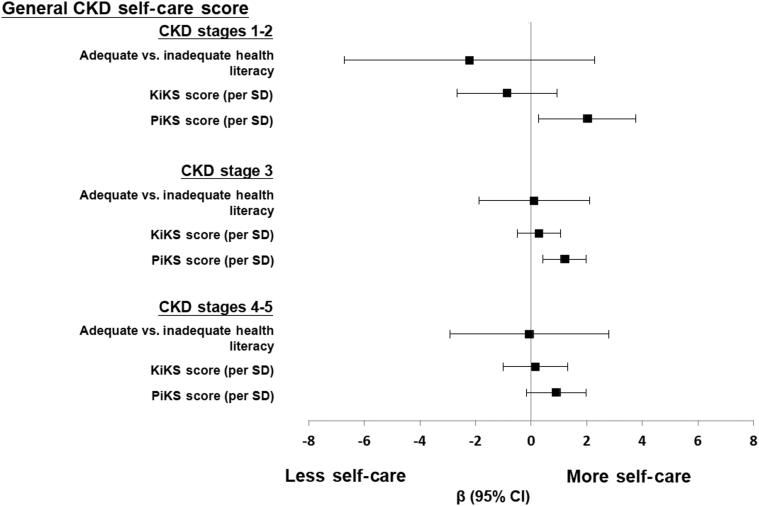
When modeled continuously (per SD) in unadjusted analyses, perceived kidney disease knowledge, as determined by PiKS scores, were positively associated with general CKD self-care summary scores (β = 0.71, 95% CI: 0.29–1.12). In the final multivariable adjusted model, higher PiKS scores remained associated with higher general CKD self-care scores (β = 1.07, 95% CI: 0.50–1.63) (Table 3). In unadjusted models, greater objective kidney disease knowledge, as determined by KiKS scores, had a positive trend with general CKD self-care scores (β = 0.30, 95% CI: −0.12 to 0.72). The association between KiKS scores and self-care behaviors was attenuated after adjustment for health literacy and PiKS scores, but the association between PiKS scores and self-care behaviors did not attenuate after similar adjustment for health literacy and knowledge. Health literacy was not observed to be associated with the CKD self-care summary scores. There was evidence of an interaction between the level of health literacy and PiKS and KiKS scores for the relationship with general and diabetes-related CKD self-care summary scores (P-value-interaction < 0.001). In stratified analyses by health literacy level, KiKS scores were not observed to associate with general or diabetes-related CKD self-care, and only among those with adequate health literacy were PiKS scores observed to positively associate with general CKD self-care summary scores (β = 0.97, 95% CI: 0.33–1.61) (Supplementary Table S2). There was also evidence of an interaction by CKD stage on the relationship of PiKS scores, KiKS scores, and health literacy with CKD self-care summary scores (P-value-interaction < 0.001), in which PiKS scores were positively associated with general CKD self-care summary scores among those with CKD stage 1 to 2 and CKD stage 3 (β = 2.03, 95% CI: 0.27–3.78 and β = 1.22, 95% CI: 0.44–1.99, respectively), and a positive trend observed for those with CKD stages 4 to 5 (β = 0.91, 95% CI: −0.17 to 1.98) (Figure 2; Supplementary Table S3). The results across annual income groups (≤$55,000 vs. >$55,000) and racial groups (nonwhite vs. white) were consistent with the primary results (Supplementary Table S4). The results of the sensitivity analyses incorporating individual dietary behavior scores into the CKD self-care summary score were also consistent with results of the primary analyses (Supplementary Table S5). In secondary analyses that assessed the association of PiKS scores, KiKS scores, and health literacy with self-reported participation in individual self-care behaviors, higher exercise and medication adherence scores were observed to associate with inadequate and adequate health literacy, respectively, and nonsmoking was associated with higher PiKS scores. KiKS scores were not associated with any individual behaviors (Supplementary Table S6).
Table 3.
Association of health literacy, and objective kidney disease knowledge and perceived kidney disease knowledge with CKD self-care
| General CKD self-carea | Unadjusted |
Model 1 |
Model 2 |
|||
|---|---|---|---|---|---|---|
| β (95% CI) | P | β (95% CI) | P | β (95% CI) | P | |
| Adequate health literacy | 0.89 (−0.21 to 1.98) | 0.11 | −0.11 (−1.52 to 1.29) | 0.87 | −0.45 (−1.84 to 0.94) | 0.52 |
| Objective kidney disease knowledgeb | 0.30 (−0.12 to 0.72) | 0.16 | 0.42 (−0.10 to 0.95) | 0.12 | 0.13 (−0.41 to 0.68) | 0.63 |
| Perceived kidney disease knowledgec | 0.71 (0.29–1.12) | 0.001 | 1.09 (0.56–1.63) | <0.001 | 1.07 (0.50–1.63) | <0.001 |
| Diabetes-related CKD self-cared | Unadjusted |
Model 1 |
Model 2 |
|||
|---|---|---|---|---|---|---|
| β (95% CI) | P | β (95% CI) | P | β (95% CI) | P | |
| Adequate health literacy | 1.42 (−2.44 to 5.28) | 0.47 | 0.19 (−4.97 to 5.34) | 0.94 | −0.72 (−6.08 to 4.64) | 0.79 |
| Objective kidney disease knowledgeb | 0.80 (−0.66 to 2.27) | 0.28 | 1.01 (−0.86 to 2.88) | 0.29 | 0.89 (−1.11 to 2.89) | 0.38 |
| Perceived kidney diesase knowledgec | 1.25 (−0.19 to 2.68) | 0.09 | 0.95 (−0.94 to 2.85) | 0.32 | 0.76 (−1.22 to 2.74) | 0.45 |
CKD, chronic kidney disease.
Unadjusted Model
Model 1: adjusted for sex, race, age, education, income, estimated glomerular filtration rate, diabetes, + urine protein:creatinine, hypertension status, body mass index, awareness of CKD diagnosis, number of times in 1 year evaluated by nephrologist.
Model 2: adjusted for sex, race, age, education, income, estimated glomerular filtration rate, urine protein:creatinine, diabetes status, hypertension status, body mass index, awareness of CKD diagnosis, number of times in one year evaluated by nephrologist + health literacy, PiKS score, KiKS score.
n = 275.
Determined by Kidney Disease Knowledge Survey (KiKS) score (per SD).
Determined by Perceived Kidney Disease Knowledge Survey (PiKS) score (per SD).
n = 112.
Figure 2.
Multivariable adjusted association of the summary chronic kidney disease (CKD) self-care measure, objective kidney disease knowledge (per SD Kidney Disease Knowledge Survey [KiKS] score), and perceived kidney disease knowledge (per SD Perceived Kidney Disease Knowledge Survey [PiKS] score) stratified by CKD stage. CI, confidence interval.
Discussion
To date, research efforts to optimize self-care in earlier stages of kidney disease have been limited. To ultimately improve self-care practices and potentially identify targets for intervention, we examined the association of kidney disease knowledge and health literacy with self-care behaviors among adults with non–dialysis-dependent CKD. Health literacy was not observed to be associated with self-care behaviors after adjustment for potential confounders. Higher scores of perceived kidney disease knowledge were associated with higher self-reported participation in general CKD self-care behaviors. Greater levels of objective kidney disease knowledge also trended with more self-care behaviors, and with a stronger association observed among patients with adequate health literacy than those with inadequate health literacy. Interestingly, behaviors related to smoking avoidance and adherence to medication and diabetic care routines were high, with dietary practices and exercise notably lower.
In prior studies of adults with kidney disease, greater objective health-related knowledge has been associated with higher arteriovenous access use and improved blood pressure control, which may be attributed to better self-care practices.13,21 Yet, in this study, we did not find a clear association between objective kidney disease knowledge and self-care behaviors. This finding may not be surprising because simply acquiring knowledge is likely not sufficient for engagement in self-care behaviors. It is postulated that self-efficacy, the belief an individual holds about his or her abilities to organize and execute the actions to manage disease, is necessary for behavior engagement.22 Higher perceived self-efficacy has been associated with better self-care behaviors in kidney disease and other chronic disease populations,6,23, 24, 25 and individuals with lower self-efficacy are less likely to perform self-care behaviors.26,27 Another explanation for the lack of a clear association between objective knowledge and self-care is the level of health literacy. In this study, we found a statistical interaction between objective knowledge and health literacy, and that higher objective knowledge scores were observed to be associated with more self-care only among those with adequate health literacy, which may suggest that in addition to acquiring disease-related knowledge, adequate health literacy also may need to be present for engagement in self-care behaviors.
Among adults with end-stage kidney disease and in other chronic disease populations, health literacy has been associated with patient self-care behaviors and health outcomes28, 29, 30; however, studies including individuals with earlier stages of kidney disease, diabetes, or heart failure have reported conflicting results detailing the association between low health literacy and self-care.31, 32, 33, 34 In this study, we did not find a clear association between the level of health literacy and CKD self-care behaviors. The low prevalence of inadequate health literacy in our study population may have reduced the power to detect this association. In addition, previous research also suggests that health literacy and self-efficacy are both closely related to self-care practices, but the relationship between health literacy and self-efficacy is not well understood.35,36 More research is needed to further understand the relationship among health literacy, self-efficacy, and CKD self-care to effectively develop and deliver health education and information in a way that is impactful for the individualized patient.
The measure of perceived kidney disease knowledge is novel in that it assesses the level of self-confidence in one’s kidney disease knowledge and its management. Perceived kidney disease knowledge likely represents a subdomain of self-efficacy, in line with other self-efficacy domains related to knowledge in medications, or for managing one’s health.37,38 Greater perceived kidney disease knowledge as measured by the PiKS was consistently associated with self-care behaviors, even after adjusting for objective knowledge and health literacy. This supports the idea that self-efficacy in one’s knowledge of kidney disease and management has an important influence on self-care practices. Previous literature has consistently identified self-efficacy as a modifiable risk factor that can improve medication adherence and dietary behaviors, as well as improve health outcomes, including quality of life and mortality in dialysis patients.39, 40, 41 Further, prior work has shown that objective kidney disease knowledge as measured by the KiKS and perceived kidney disease knowledge as measured by PiKS are only low to moderately associated with each other,17 for unclear reasons,42 suggesting they are likely not in the same construct. Thus the PiKS may offer a novel target to assess patient risk for unfavorable general CKD self-care, and present a new target for educational and support interventions. Interestingly, the PiKS measure was not associated with diabetes-related self-care behaviors, which might be due to reduced power because only 38% of the sample had diabetes (n = 145), or it may be because perceived kidney disease knowledge is not related to participation in diabetes-related self-care behaviors in CKD.
Supporting a patient’s self-efficacy of his or her CKD knowledge appears from our study, as an important component to include in CKD education, but questions arise about how to support this new subdomain of self-efficacy. According to Bandura,43 self-efficacy is an important determinant of behavior engagement and the most effective way to optimize patient self-efficacy is through incremental mastery experiences. Applied to our findings, this would suggest that providing not only CKD education, but also positive feedback to patients about what they have learned, and how well they have learned it also would make sense. Extending on the teach-back method offers a platform for clinicians to provide this positive feedback. Teach-back allows for clinicians to confirm that messaging of health information during a clinical encounter has been understood by patients,44,45 and it could offer an important opportunity for a clinician to segue into another point to make for the patient, namely to acknowledge and even praise patients incrementally on what they have learned and how well they have learned it. By using positive reinforcement within a routine clinical encounter around disease education, clinicians could support and strengthen a patient’s self-efficacy about kidney disease knowledge. Other mechanisms also may be useful, but as a whole require further study.46
Last, results from the reported CKD self-care behaviors indicate that patients had the most difficulty partaking in a healthy diet and physical activity; the latter of which patients reported engaging in only a mean of 2.5 days in the past week. This is a problem because healthy diet and physical activity are cornerstones to overall health. Studies have shown that busy lifestyles and competing priorities may override these healthy behaviors. In one study of more than 200 “healthy” women ages 40 to 60 years, “distant benefits from exercise such as health promotion, disease prevention, and longevity” were not as compelling to actual behavior change as other daily priorities and responsibilities.47 This may be the case in our cohort as well, despite our population’s need to engage in these behaviors perhaps even more than a “healthy” population, given their CKD. It has been suggested that one solution may be to rebrand self-care behaviors by promoting them not for long-term health gains in the future, but rather, to enhance and improve how one feels each day.47
The results of this study need to be interpreted in the setting of its limitations. First, the study’s cross-sectional design limits our ability to establish the directionality of the associations found. Second, the study population was also well educated, predominantly white, and with adequate health literacy, which may limit its generalizability, as a recent systematic review concluded that limited health literacy is common among individuals with CKD, especially among those with low socioeconomic status and nonwhite ethnicity.48 However, in stratified analyses, results were consistent despite level of annual income (≤ or > $55,000) or by racial group (white vs. nonwhite). A third limitation includes the use of only self-reported measures, which also may have introduced reporting bias. However, the self-care behaviors were assessed with a validated instrument. A fourth limitation is that the assessment of the previous 7 days might not be representative of usual behavior and the lack of assessing pill burden might affect the level of self-reported medication adherence. Fifth, we did not measure the level of motivation or self-efficacy related to behaviors of the study participants, which also could be integral to self-care behavior participation.39 Despite these limitations, there are strengths to note, including a study population with a range of disease severity (i.e., CKD stages 1–5) and assessment of behaviors that are advisable to all adults with CKD to manage their disease, but have not been previously well-studied. Further, we offer a novel construct, self-efficacy about one’s disease knowledge and its management, as a new factor associated with, and potentially influential to self-care. Ultimately, the goal is to improve self-care in CKD, especially in the early stages, which would provide an opportunity to more effectively manage kidney disease, tailor educational needs, and develop supportive interventions for patients. Information from this study and other work can be incorporated into education and support efforts now to optimize self-care for those with non–dialysis-dependent CKD, as part of evidence-based best practices in health care.49 Future education efforts should consider incorporating support for self-efficacy of CKD knowledge, which also could be studied for its association with clinical outcomes using our PiKS measure. More research is still needed to better understand the relationship among health literacy, self-efficacy, knowledge, and self-care behaviors in CKD.
Disclosure
NDE received compensation for delivering a lecture at a Fresenius Medical Care North American Live Series in November 2018. All the other authors declared no competing interests.
Acknowledgments
SJS reports funding from the National Institutes of Health (NIH) National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) K23 DK 118198–01A1. JWN reports funding sources from NIH NIDDK K23 DK097183, NIH NIDDK R01 DK115844, NIH National Center for Advancing Translational Sciences (NCATS) UL 1TR002240. Support for this work was also provided by K23DK080952 and K23DK080952-02S1 to KLC. NDE is supported by K23DK114526.
Author Contributions
Research idea and study design: SJS, JWN; data acquisition: TAI, JWN, KLC; statistical analysis: SJS, JWN; data analysis/interpretation: SJS, KLC, AF, ACR, TAI, KLC, NDE, JWN; supervision or mentorship: JWN, TAI, KLC. Each author contributed important intellectual content during manuscript drafting or revision and accepts accountability for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved.
Footnotes
Figure S1. Flow diagram of study recruitment.
Table S1. Self-Care behavior scores for individual behaviors and summary measures of study participants (n = 401).
Table S2. Association of PiKS and KiKS scores with self-care summary scores, by health literacy level.
Table S3. Association of health literacy, and objective kidney disease knowledge and perceived kidney disease knowledge with CKD self-care by CKD stage.
Table S4. Association of health literacy, and objective kidney disease knowledge and perceived kidney disease knowledge with CKD self-care by white versus nonwhite race and by annual income (≤$55,000 vs. >$55,000).
Table S5. Association of summary self-care scores including 7 individual self-care behaviors and health literacy, objective, and perceived knowledge scores.
Table S6. Association of health literacy, and objective kidney disease knowledge and perceived kidney disease knowledge with CKD self-care individual behaviors (n = 275).
STROBE Statement.
Supplementary Material
References
- 1.Couser W., Remuzzi G., Mendis S., Tonelli M. The contribution of chronic kidney disease to the global burden of major noncommunicable diseases. Kidney Int. 2011;80:1258–1270. doi: 10.1038/ki.2011.368. [DOI] [PubMed] [Google Scholar]
- 2.National Kidney Foundation K/DOQI Clinical practice guidelines on hypertension and antihypertensive agents in chronic kidney disease. Am J Kidney Dis. 2004;43:S1–S290. [PubMed] [Google Scholar]
- 3.Curtin R., Johnson H., Schatell D. The peritoneal dialysis experience: insights form long-term patients. Nephrol Nurse J. 2004;31:615–624. [PubMed] [Google Scholar]
- 4.Curtin R., Mapes D., Schatell D., Burrows-Hudson S. Self-management in patients with end stage renal disease: exploring domains and dimensions. Nephrol Nurs J. 2005;32:389–398. [PubMed] [Google Scholar]
- 5.Peng S., He J., Huang J. Self-management interventions for chronic kidney disease: a systematic review and meta-analysis. BMC Nephrology. 2019;20:142. doi: 10.1186/s12882-019-1309-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Curtin R., Walters B., Schatell D. Self efficacy and self management behaviors in patients with chronic kidney disease. Adv Chronic Kidney Dis. 2008;15:191–205. doi: 10.1053/j.ackd.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 7.Sheridan S., Halpern D., Viera A. Interventions for individuals with low health literacy: a systematic review. J Health Commun. 2011;16:20–54. doi: 10.1080/10810730.2011.604391. [DOI] [PubMed] [Google Scholar]
- 8.Institute of Medicine . National Academies Press; Washington, DC: 2004. Health Literacy: Prescription to End Confusion. [PubMed] [Google Scholar]
- 9.Fraser S., Roderick P., Casey M. Prevalence and associations of limited health literacy in chronic kidney disease: a systematic review. Nephrol Dial Transplant. 2013;28:129–137. doi: 10.1093/ndt/gfs371. [DOI] [PubMed] [Google Scholar]
- 10.Ricardo A., Yang W., Lora C. Limited health literacy is associated with low glomerular filtration in the Chronic Renal Insufficiency Cohort (CRIC) study. Clin Nephrol. 2014;81:30–37. doi: 10.5414/CN108062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Green J., Mor M., Shields A. Associations of health literacy with dialysis adherence and health resource utilization in patients receiving maintenance hemodialysis. Adv Chronic Kidney Dis. 2013;62:73–80. doi: 10.1053/j.ajkd.2012.12.014. [DOI] [PubMed] [Google Scholar]
- 12.Cavanaugh K., Wingard R., Hakim R. Low health literacy associates with increased mortality in ESRD. J Am Soc Nephrol. 2010;21:1979–1985. doi: 10.1681/ASN.2009111163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cavanaugh K., Wingard R., Hakin R. Patient dialysis knowledge is associated with permanent arteriovenous access use in chronic hemodialysis. Clin J Am Soc Nephrol. 2009;4:950. doi: 10.2215/CJN.04580908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Levey A., Bosch J., Lewis J. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999;130:461–470. doi: 10.7326/0003-4819-130-6-199903160-00002. [DOI] [PubMed] [Google Scholar]
- 15.Inker L., Astore B., Fox C. KDOQI US commentary on the 2012 KDIGO clnical practice guidleine for the evaluation and management of CKD. Am J Kidney Dis. 2014;63:713–735. doi: 10.1053/j.ajkd.2014.01.416. [DOI] [PubMed] [Google Scholar]
- 16.Wright J., Wallston K., Elasy T. Development and results of a kidney disease knowledge survey given to patients with CKD. Am J Kidney Dis. 2011;57:387–395. doi: 10.1053/j.ajkd.2010.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wright Nunes J., Wallston K., Eden S. Associations among perceived and objective kidney disease knowledge and statisfaction with physician communication in patients with chronic kidney disease. Kidney Int. 2011;80:1344–1351. doi: 10.1038/ki.2011.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Davis T., Long S., Jackson R. Rapid estimate of adult literacy in medicine: a shortened screening instrument. Fam Med. 1993;25:391–395. [PubMed] [Google Scholar]
- 19.Toobert D., Hampson S., Glasgow R. The Summary of Diabetes Self-Care Activities Measure, results from 7 studies and a revised scale. Diabetes Care. 2000;23:943–950. doi: 10.2337/diacare.23.7.943. [DOI] [PubMed] [Google Scholar]
- 20.DeWalt D., Berkman N., Sheridan S. Literacy and health outcomes: a systematic review of the literature. J Gen Intern Med. 2004;19:1228–1239. doi: 10.1111/j.1525-1497.2004.40153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wright-Nunes J., Luther J., Ikizler T., Cavanaugh K. Patient knowledge of blood pressure target is associated with improved blood pressure control in chronic kidney disease. Patient Educ Couns. 2012;88:184–188. doi: 10.1016/j.pec.2012.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bandura A. Freeman; New York, NY: 1997. Self-Efficacy: The Exercise of Control. [Google Scholar]
- 23.Lorig K., Holman H. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med. 2003;26:1–7. doi: 10.1207/S15324796ABM2601_01. [DOI] [PubMed] [Google Scholar]
- 24.Weng L., Dai Y., Huang H.L., Chiang Y.J. Self-efficacy, self-care behaviors and quality of life of kidney transplant recipients. J Adv Nurs. 2010;66:828–838. doi: 10.1111/j.1365-2648.2009.05243.x. [DOI] [PubMed] [Google Scholar]
- 25.Wild M., Wallston K., Green J. The Perceived Medical Condition Self-Management Scale can be applied to patients with chronic kidney disease. Kidney Int. 2017;92:972–978. doi: 10.1016/j.kint.2017.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yehle K., Plake K. Self-efficacy and educational interventions in heart failure: a review of the literature. J Cardiovasc Nurs. 2010;25:175–188. doi: 10.1097/JCN.0b013e3181c71e8e. [DOI] [PubMed] [Google Scholar]
- 27.Bourbeau J., Nault D., Dang-Tan T. Self-management and behaviour modification in COPD. Patient Educ Couns. 2004;52:271–277. doi: 10.1016/S0738-3991(03)00102-2. [DOI] [PubMed] [Google Scholar]
- 28.Rothman R., DeWalt D., Malone R. Influence of patient literacy on the effectiveness of a primary care-based diabetes disease management program. JAMA. 2004;292:1711–1716. doi: 10.1001/jama.292.14.1711. [DOI] [PubMed] [Google Scholar]
- 29.Devraj R., Gordon E. Health literacy and kidney disease: toward a new line of research. Am J Kidney Dis. 2009;53:884–889. doi: 10.1053/j.ajkd.2008.12.028. [DOI] [PubMed] [Google Scholar]
- 30.Berkman N., Seridan S., Donahue E. Low health literacy and health outcomes: an updated systemic review. Ann Intern Med. 2011;155:97–107. doi: 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- 31.Golin C., Liu H., Hays R. A prospective study of predictors of adherence to combination antiretroviral medications. J Gen Intern Med. 2002;17:756–765. doi: 10.1046/j.1525-1497.2002.11214.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wong K., Velasquez A., Powe N., Tuot D. Association between health literacy and self-care behaviors among patients with chronic kidney disease. BMC Nephrology. 2018;19:196. doi: 10.1186/s12882-018-0988-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Von Wagner C., Steptoe A., Wolf M., Wardle J. Health literacy and health actions: a review and a framework from health psychology. Health Educ Behavior. 2009;36:860–877. doi: 10.1177/1090198108322819. [DOI] [PubMed] [Google Scholar]
- 34.Chen A., Yehle K., Albert N. Relationship between health literacy and heart failure knowledge, self-efficacy, and self-care adherence. Res Social Admin Pharm. 2013;10:378–386. doi: 10.1016/j.sapharm.2013.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.von Wagner C., Semmler C., Good A., Wardle J. Health literacy and self-efficacy for participating in colorectal cancer screening. The role of information processing. Patient Educ Couns. 2009;75:352–357. doi: 10.1016/j.pec.2009.03.015. [DOI] [PubMed] [Google Scholar]
- 36.Wolf M., Davis T., Osborn C. Literacy, self-efficacy, and HIV adherence. Patient Educ Couns. 2007;65:253–260. doi: 10.1016/j.pec.2006.08.006. [DOI] [PubMed] [Google Scholar]
- 37.Smith M., Wallston K., Smith C. The development and validation of the Perceived Health Competence Scale. Health Educ Res. 1995;10:51–64. doi: 10.1093/her/10.1.51. [DOI] [PubMed] [Google Scholar]
- 38.Cameron K., Ross E., Clayman M. Measuring patients' self-efficacy in understanding and using prescription medication. Patient Educ Couns. 2010;80:372–376. doi: 10.1016/j.pec.2010.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Luszczynska A., Mohamed N., Schwarzer R. Self-efficacy and social support predict benefit finding 12 months after cancer surgery: the mediating role of coping strategies. Psycholology, Health, & Medicine. 2005;10:365–375. [Google Scholar]
- 40.Takaki J., Yano E. Possible gender differences in the relationships of self-efficacy and the internal loss of control with compliance in hemodialysis patients. Behavioral Medicine. 2006;32:5–11. doi: 10.3200/BMED.32.1.5-11. [DOI] [PubMed] [Google Scholar]
- 41.Oka M., Chaboyer W. Influence of self-efficacy and other factors on dietary behaviors in Japanese hemodialysis patients. Int J Nurs Pract. 2001;7:431–439. doi: 10.1046/j.1440-172x.2001.00334.x. [DOI] [PubMed] [Google Scholar]
- 42.Sepucha K., Fagerlin A., Couper M. How does feeling informed relate to being informed? The DECISIONS survey. Med Decis Making. 2010;30:77S–84S. doi: 10.1177/0272989X10379647. [DOI] [PubMed] [Google Scholar]
- 43.Bandura A. Self-efficacy. In: Weiner I., Craighead W., editors. In The Corsini Encyclopedia of Psychology. John Wiley; Hoboken, NJ: 2010. pp. 1534–1536. [Google Scholar]
- 44.Peter D., Robinson P., Jordan M. Reducing readmissions using teach-back: enhancing patient and family education. J Nurs Adm. 2015;45:35–42. doi: 10.1097/NNA.0000000000000155. [DOI] [PubMed] [Google Scholar]
- 45.Kripalani S., Bengtzen R., Henderson L., Jacobson T. Clinical research in low-literacy populations: using teach-back to assess comprehension of informed consent and privacy information. IRB. 2008;30:13–19. [PubMed] [Google Scholar]
- 46.Ha Dinh T., Bonner A., Clark R. The effectiveness of the teach-back methods on adherence and self-management in health education for people with chronic disease: a systematic review. JBI Database System Rev Implement Rep. 2016;14:210–247. doi: 10.11124/jbisrir-2016-2296. [DOI] [PubMed] [Google Scholar]
- 47.Segar M., Eccles J., Richardson C. Rebranding exercise: closing the gap between values and behavior. Int J Behav Nutr Phys Act. 2011;8:94. doi: 10.1186/1479-5868-8-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Taylor D., Fraser S., Bradley J. A systematic review of the prevalence and associations of limited health literacy in CKD. Clin J Am Soc Nephrol. 2017;12:1070–1084. doi: 10.2215/CJN.12921216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Adams K., Corrigan J., editors. Priority Areas for National Action: Transforming Health Care Quality. Institute of Medicine (US) Committee on Identifiying Priority Areas for Quality Improvement. National Academies Press; Washington, DC: 2013. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.