Abstract
Background
The optimal management of elderly patients with non-ST-segment elevation myocardial infarction (NSTEMI) is still discussed. We aimed to study short- and long-term survival in NSTEMI patients ≥75 years managed with an invasive or a conservative strategy.
Methods
NSTEMI patients admitted to Oslo University Hospital Ulleval during 2005–2011 were included consecutively in a prospective registry. Vital status until December 31, 2013, was obtained from the Norwegian Cause of Death Registry. Patients ≥75 years were identified, and 30-day and 7-year survival were analyzed. Logistic- and Cox regression was used to estimate OR and hazard ratio (HR) for death in the invasive versus conservative group, adjusting for registered confounders.
Results
There were 2,064 NSTEMI patients ≥75 years (48.2% women); 1,200 (58.1%) were treated with an invasive strategy, and were younger, more likely to be male and previously revascularized compared to 864 (41.9%) patients treated conservatively (p < 0.0001 for all). Survival at 30-day was 94.9% in the invasive and 76.6% in the conservative group. For 30-day survivors, 7-year survival was 47.4% (95% CI 42.9–51.8) and 11.6% (95% CI 8.3–15.6), respectively. After multivariate adjustment, an invasive strategy was associated with lower long-term risk (adjusted HR [aHR] 0.49 [95% CI 0.41–0.59]). Actual revascularization was associated with lower risk of long-term mortality compared to angiography only (aHR<sub>PCI</sub> 0.73 [95% CI 0.59–0.90], aHR<sub>CABG</sub> 0.43 [95% CI 0.28–0.65]).
Conclusion
In this real-life cohort of NSTEMI patients ≥75 years, 30-day survival was 95%, and 7-year survival was 47% with an invasive strategy. Revascularized patients had a superior long-term prognosis. With a conservative strategy, short- and long-term survival was lower, probably due to selection bias and unmeasured confounding.
Keywords: Non-ST-segment elevation myocardial infarction, Elderly, Invasive strategy, Long-term survival
Introduction
Several randomized controlled trials (RCTs) have demonstrated improved outcomes in patients with non-ST-segment elevation myocardial infarction (NSTEMI) managed with a routine invasive compared to a conservative strategy [1, 2, 3]. Guidelines from the American Heart Association/American College of Cardiology and the European Society of Cardiology recommend a routine invasive strategy in patients with NSTEMI without age restrictions [4, 5]. It is advised to consider benefits versus risks, including patient preferences, in older patients that are frail or have comorbid conditions with risk of adverse outcomes.
Elderly patients have been underrepresented in most RCTs performed, and outcome data in patients ≥75 years with NSTEMI are limited. Results from 2 smaller RCTs of invasive management in elderly patients with NSTEMI differed regarding a benefit of a routine invasive strategy [6, 7]. The larger after-80 study [8], comparing an invasive versus a conservative strategy in 457 patients ≥80 years, showed a 47% risk reduction for the primary endpoint (a composite of myocardial infarction [MI], urgent revascularization, stroke, or death) with the invasive strategy, but no significant difference in all-cause mortality [8]. In a large observational study including octogenarians with unstable angina or NSTEMI, an invasive strategy (≤48 h) was associated with lower in-hospital mortality, but higher risk of cardiogenic shock [9]. Other observational studies have shown a favorable prognosis up to 1 year with an invasive strategy for elderly NSTEMI patients [10, 11], but long-term data are lacking. Due to the sparse data from clinical trials as well as from the real-world setting, the optimal management strategy for older patients with NSTEMI remains a subject of debate. The aim of the present study was to study short- and long-term survival in a cohort of NSTEMI patients ≥75 years admitted to a cardiac center in Norway and managed with an invasive or a conservative strategy.
Methods
Study Population
This was an observational cohort study using data registered prospectively in the Oslo University Hospital (OUH) Ulleval MI registry. OUH Ulleval is a community hospital for 190,000 inhabitants and serves as a tertiary cardiac center for the region of Eastern Norway with a catchment population of 1,400,000 people. From September 1, 2005, all consecutive patients with acute MI (AMI) admitted to our hospital were prospectively recorded in a local registry. The diagnosis of AMI was made according to the current AMI definition [12, 13], using troponin T as the cardiac biomarker. Classification of ST-segment elevation MI or NSTEMI was based on the diagnostic electrocardiogram [14]. The inclusion to our local registry closed on December 31, 2011, due to the establishment of a national MI registry in Norway with a different owner.
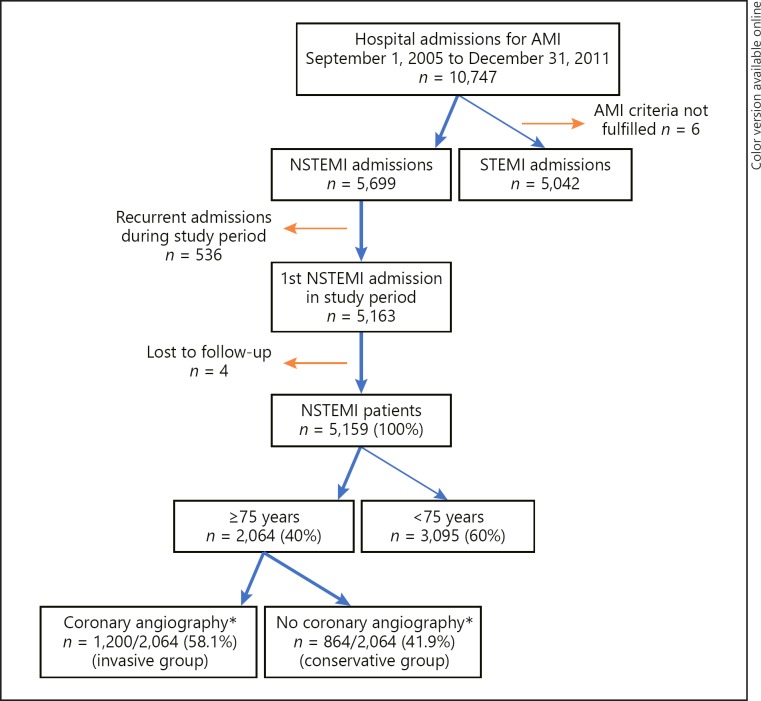
In the present study, only the first admission for NSTEMI during the study period was included. The study population flow chart is presented in Figure 1. Patients aged ≥75 years with NSTEMI were divided in 2 groups: (1) the invasive group defined as patients who underwent coronary angiography during the index hospitalization with percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) if indicated, in addition to recommended medical therapy and (2) the conservative group receiving recommended medical therapy only. Therapeutic decisions were solely at the discretion of the treating physician. Reasons for using an invasive or conservative strategy were not recorded in the registry.
Fig. 1.
Flow chart. * During index hospitalization. AMI, acute myocardial infarction; NSTEMI, non-ST-elevation myocardial infarction; STEMI, ST-elevation myocardial infarction.
Data Collection, Definition of Variables, and Validation
Data regarding baseline cardiovascular risk factors, treatment, invasive procedures, coronary angiograms, in-hospital complications, and in-hospital mortality were registered in an electronic database developed by the Mid-Norway Health Authority as described previously [14]. Variables were predefined in the OUH Ulleval MI registry user manual [15]. Coronary angiograms were described as normal if no visible atherosclerotic lesions, as nonobstructive coronary artery disease (CAD) if <50% stenosis, or as significant CAD if ≥50% stenosis were present. One-vessel disease was defined as significant CAD in one vessel, and multiple vessel disease as the presence of significant CAD in >1 coronary arteries or in the left main coronary artery.
An internal validation procedure of the variables registered for 200 random patients was performed by the primary investigator. Values were compared with the patients' hospital records, and the estimated correlation between registry data and patient records was >90%. The continuous variable serum (s)-creatinine at admission had 10.6% missing values, and a sensitivity analysis was performed with normal (defined as 70 µmol/L) or high (defined as 300 µmol/L) values replacing missing values. For all other included variables, missing values were <5%.
Follow-Up and Outcomes
Vital status until the end of follow-up on December 31, 2013, was obtained by linkage to the Norwegian Cause of Death registry. Follow-up time was defined as time from hospital admission to death or end of follow-up, whichever came first, and differed between patients due to the dynamic inclusion period. No information was available with respect to treatment after discharge from the index hospital admission.
Two primary analyses were performed. In the first, the primary endpoint was 30-day survival. In the second, the primary endpoint was survival during maximum 7 years of follow-up in patients being alive at day 30 after admission (a so-called landmark analysis) [16]. Secondary endpoints were OR for the association between an invasive strategy and 30-day mortality, and hazard ratio (HR) for mortality during follow-up among 30-day survivors in the invasive compared to the conservative group. In the landmark analysis of patients surviving the first 30 days, follow-up time was defined from day 30 to end of follow-up.
Ethics
The establishment of the local MI registry and the conduction of this study were approved by the Privacy Protection Officer at OUH. The Ministry of Health and Care Services approved exemption from the duty of confidentiality (November 16, 2011) and The Norwegian Data Protection Authority provided concession for data linkage with the Norwegian Cause of Death Registry (January 5, 2012). All data were anonymized before analysis.
Statistical Analysis
Categorical variables are reported by numbers and percentage, after removing missing values (denominators may vary). Continuous variables are reported by mean ± SD or median (25–75th percentile). Differences between the invasive and conservative groups in baseline risk factors and complications were tested with chi-square or Fisher exact tests for categorical variables and 2-sample t test or Mann-Whitney U test for continuous variables, as appropriate. Survival from admission to day 30 and 7-year survival from day 30 were calculated with the life-table method and illustrated with the Kaplan-Meier survival function. Survival functions were compared with the log-rank test. Patients in the invasive group were considered as the exposed, while patients in the conservative group were the non-exposed. Logistic regression was used to calculate OR with 95% CI for the association between exposure and 30-day mortality. Based on previous knowledge [17, 18, 19, 20, 21, 22, 23] and clinical considerations, the following covariates were included to adjust for confounding: age, gender, previous hypertension, previous MI, previous revascularization, previous stroke, diabetes mellitus, peripheral artery disease, s-creatinine at admission, out-of-hospital resuscitation, heart failure, cardiogenic shock, atrial fibrillation/-flutter, and antibiotic treatment. Cox regression was used to calculate HR with 95% CI for long-term mortality after 30 days in the exposed versus non-exposed. The proportional hazards assumption was evaluated using the log-log Kaplan-Meier plot. Confounding adjustment was as in the logistic regression. Pre-specified analyses for effect modification by age, gender and s-creatinine were performed by forcing an interaction term into the multivariate regression models, one at a time. As the primary analyses were significant, subgroup analysis of survival among patients in the invasive group treated with PCI, CABG or no revascularization was performed [24]. All tests were two-tailed, and a p value <0.05 was considered significant. Analyses were performed with STATA 13 (Statacorp LP, TX, USA). The study confines with the STrengthening the Reporting of OBservational studies in Epidemiology checklist for reporting of observational studies [25].
Results
Study Population
Among 5,159 NSTEMI patients admitted to our hospital during 2005–2011, 2,064 patients (40.0%) were ≥75 years and constitute the study cohort (Fig. 1). The mean age was 82 ± 5.5 years and 48.2% were women. A total of 1,200 patients (58.1%) underwent coronary angiography during the index hospitalization with PCI or CABG if indicated (invasive group), and 864 patients (41.9%) received recommended medical therapy only (conservative group). The median time from symptom onset to coronary angiography was 3 [2, 3, 4, 5] days. Patients in the invasive group were younger, more likely to be men and previously revascularized, and less likely to have had a previous stroke and elevated s-creatinine at admission (Table 1).
Table 1.
Baseline characteristics
| NSTEMI patients ≥75 years (n = 2,064) |
p value | ||
|---|---|---|---|
| invasive group (n = 1,200) | conservative group (n = 864) | ||
| Age, mean ± SD | 80.4±4.0 | 86.4±5.3 | <0.0001 |
| Women, n (%) | 473 (39.4) | 521 (60.3) | <0.0001 |
| Diabetes, n (%) | 248 (20.7) | 164 (19.0) | 0.343 |
| Hypertension, n (%) | 602 (50.1) | 419 (48.4) | 0.503 |
| Previous MI, n (%) | 396 (33.0) | 300 (34.8) | 0.401 |
| Previous revascularization, n (%) | 321 (26.8) | 129 (14.9) | <0.0001 |
| Previous stroke, n (%) | 165 (13.8) | 203 (23.6) | <0.0001 |
| Peripheral artery disease, n (%) | 127 (10.6) | 75 (8.7) | 0.154 |
| S-creatinine at admission, µmol/L, median (25–75th percentile) | 87 (72–107) | 99 (76–132) | <0.0001 |
| Out-of-hospital resuscitation, n (%) | 21 (1.8) | 16 (1.9) | 0.863 |
NSTEMI, non-ST-elevation myocardial infarction; MI, myocardial infarction; s-creatinine, serum-creatinine.
Revascularization and In-Hospital Complications
In the invasive group, 1,057 patients (88.1%) had significant one- or multiple-vessel CAD, and 706 patients (58.8%) were treated with PCI or CABG (Table 2). In the conservative group, by definition, no coronary angiography was performed during the index hospitalization. The proportion of patients with out-of-hospital resuscitation, cardiogenic shock, and in-hospital arrhythmias were similar in both groups (Tables 1, 2). Compared to the conservative group, patients in the invasive group were less likely to have atrial fibrillation/flutter, heart failure, stroke, and antibiotic treatment during the hospital stay (Table 2).
Table 2.
Invasive procedures, in-hospital complications, and death
| NSTEMI patients ≥75 years (n = 2,064) |
p value | ||
|---|---|---|---|
| invasive group (n = 1,200) | conservative group (n = 864) | ||
| Coronary angiography, n (%) | 1,200 (100) | - | - |
| PCI, n (%) | 580 (48.3) | - | - |
| CABGa, n (%) | 126 (10.5) | - | - |
| Symptom onset to angiography, days, median (25–75th percentile) | 3 (2–5) | - | - |
| Normal vessels or nonobstructive CAD, n (%) | 131 (11.0) | - | - |
| One-vessel disease, n (%) | 449 (37.8) | - | - |
| Multiple vessel disease, n (%) | 608 (51.2) | - | - |
| Cardiogenic shock, n (%) | 15 (1.3) | 15 (1.7) | 0.363 |
| Atrial fibrillation, n (%) | 62 (5.2) | 136 (15.7) | <0.0001 |
| Heart failure, n (%) | 106 (8.8) | 322 (37.3) | <0.0001 |
| Atrioventricular block 2–3°, n (%) | 14 (1.2) | 11 (1.3) | 0.827 |
| In-hospital stroke, n (%) | 13 (1.1) | 41 (4.8) | <0.0001 |
| Treatment with antibiotics, n (%) | 101 (8.4) | 387 (44.8) | <0.0001 |
| VT/VF >48 h from admission, n (%) | 11 (0.9) | 5 (0.6) | 0.388 |
| Gastrointestinal bleeding, n (%) | 4 (0.3) | 33 (3.8) | <0.0001 |
| In-hospital death, n (%) | 29 (2.4) | 157 (18.2) | <0.0001 |
CABG during index admission or planned for CABG later.
NSTEMI, non-ST-elevation myocardial infarction; PCI, percutaneous coronary intervention; CABG, coronary artery bypass grafting; CAD, coronary artery disease; VT, ventricular tachycardia; VF, ventricular fibrillation.
Outcomes
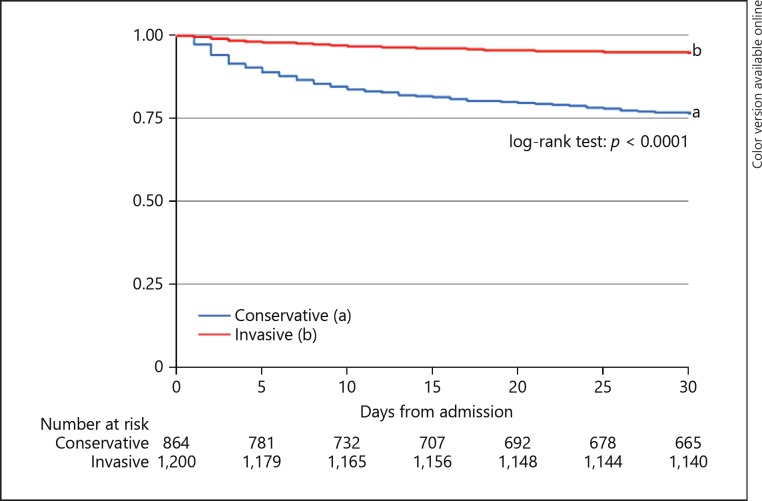
During the first 30 days, 60/1,200 (5.0%) of patients treated invasively died and 199/864 (23.0%) in the conservative group (Table 3, Fig. 2).
Table 3.
30-Day and long-term survival* in NSTEMI patients ≥75 years
| Invasive group, (n = 1,200), % (95% CI) | Conservative group, (n = 864), % (95% CI) | |
|---|---|---|
| 30-Day survival | 94.9 (93.5–96.0) | 76.6 (73.7–79.3) |
| Landmark analysis: survival in patients alive 30 days from admission | (n = 1,140) | (n = 665) |
| 1 year | 90.8 (89.0–92.3) | 66.8 (63.1–70.2) |
| 2 years | 84.3 (82.0–86.3) | 53.2 (49.4–56.9) |
| 3 years | 78.0 (75.4–80.3) | 38.8 (35.0–42.5) |
| 4 years | 70.9 (67.9–73.6) | 28.5 (24.9–32.2) |
| 5 years | 62.1 (58.7–65.3) | 20.3 (16.8–24.0) |
| 6 years | 52.9 (48.9–56.7) | 15.5 (12.1–19.2) |
| 7 years | 47.4 (42.9–51.8) | 11.6 (8.3–15.6) |
| End of follow-up | 44.2 (38.7–49.5) | 7.9 (4.4–12.9) |
Life-table method.
Follow-up time from admission (n = 2,064): 1,011 days (25–75th percentile: 248–1,566).
NSTEMI, non-ST-elevation myocardial infarction.
Fig. 2.
30-day survival. Patients aged ≥75 years with NSTEMI. Kaplan-Meier survival plot.
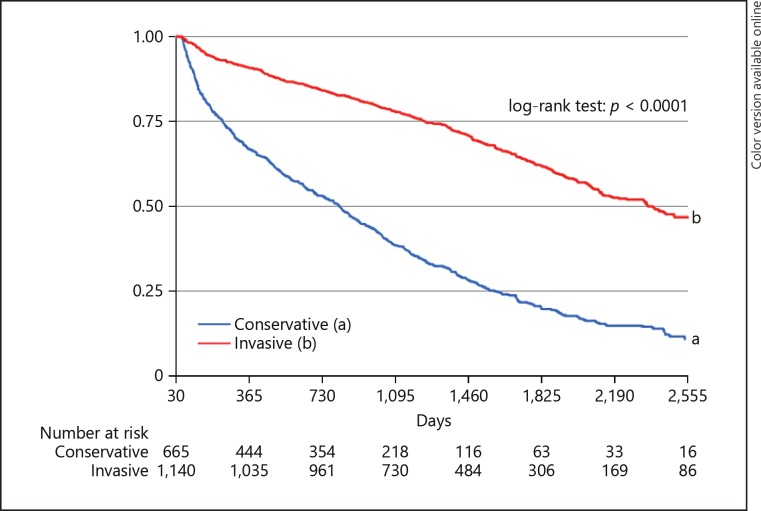
Among patients who survived the first 30 days (n = 1,805), median follow-up time was 1,155 days (634–1,687), and maximum follow-up time was 2,974 days. Estimated 7-year survival was 47.4% in the invasive group and 11.6% in the conservative group (Table 3, Fig. 3). After multivariate adjustment, an invasive strategy was associated with 51% lower risk of death during follow-up compared to a conservative strategy (Table 4). The proportional hazards assumption was considered valid.
Fig. 3.
Long-term survival. NSTEMI patients ≥75 years alive at day 30 (Landmark analysis). Kaplan-Meier survival plot. Median follow-up 1,155 days (25–75th percentile: 634–1,687).
Table 4.
Invasive strategy and mortality, NSTEMI patients ≥75 years
| OR (95% CI) | p value | |
|---|---|---|
| Association between an invasive strategy and 30-day mortalitya | ||
| Unadjusted | 0.18 (0.13–0.24) | <0.0001 |
| Age adjusted | 0.23 (0.16–0.32) | <0.0001 |
| Adjusted for baseline characteristicsb | 0.31 (0.21–0.45) | <0.0001 |
| Multivariate adjustedc | 0.39 (0.25–0.60) | <0.0001 |
| HR (95% CI) | p value | |
|---|---|---|
| Long-term mortality in the invasive versus the conservative group for patients surviving the first 30 days (n = 1,805)d | ||
| Unadjusted | 0.29 (0.26–0.33) | <0.0001 |
| Age adjusted | 0.36 (0.31–0.43) | <0.0001 |
| Adjusted for baseline characteristicsb | 0.40 (0.33–0.47) | <0.0001 |
| Multivariate adjustedc | 0.49 (0.41–0.59) | <0.0001 |
Logistic regression.
Adjustment for baseline characteristics: Age, female gender, s-creatinine, out-of-hospital resuscitation, previous hypertension, -myocardial infarction, –revascularisation or -stroke, diabetes mellitus, peripheral artery disease.
Multivariate adjusted: adjustment for baseline characteristics + in-hospital atrial fibrillation/flutter, heart failure, cardiogenic shock, antibiotic treatment.
Cox regression with landmark at 30 days; median follow-up 1,155 days (25–75th percentile: 634–1,687).
NSTEMI, non-ST-elevation myocardial infarction; HR, hazard ratio.
There was effect modification by level of s-creatinine at admission on the association between an invasive strategy and long-term mortality (p interaction = 0.006). When patients were dichotomized according to s-creatinine levels (<110 or ≥110 µmol/L), the effect was larger for patients with s-creatinine <110 µmol/L at admission (adjusted HR [aHR] 0.45 [95% CI 0.38–0.54]) than for patients with s-creatinine ≥110 µmol/L (aHR 0.64 [95% CI 0.47–0.87]). There was no significant effect modification by age (p = 0.166) or gender (p = 0.791). In a sensitivity analysis, there were no alteration of the association between s-creatinine and mortality in the Cox regression model. Therefore, we assumed that s-creatinine values were missing completely at random.
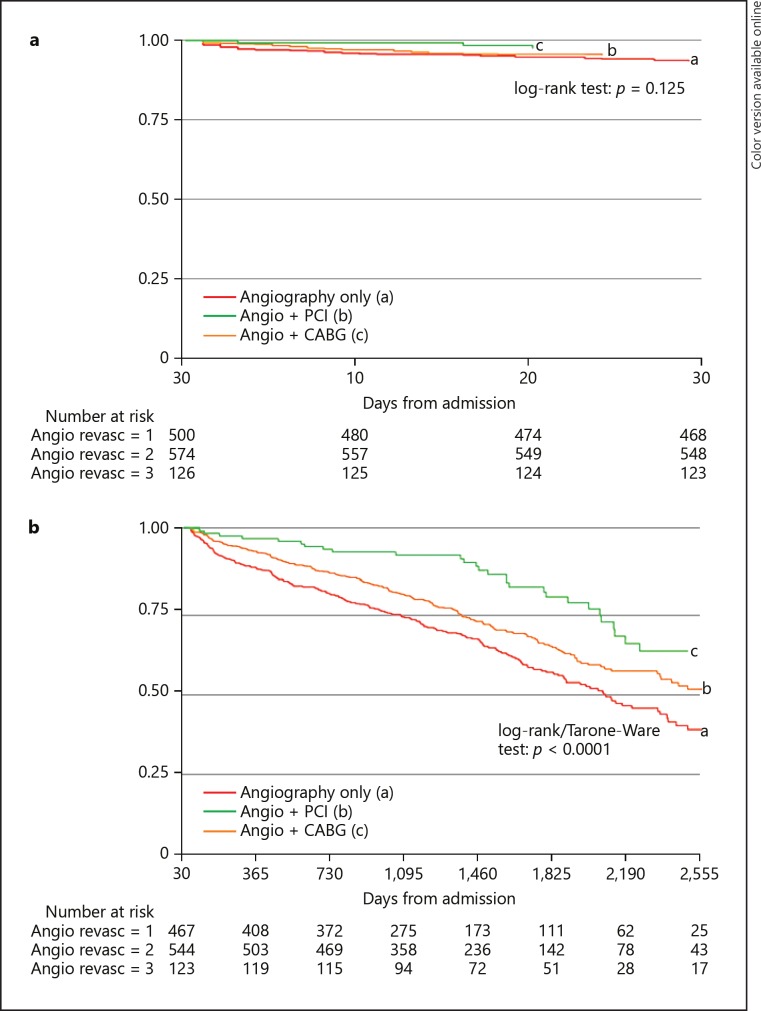
In a subgroup analysis of patients treated invasively, 30-day survival was similar for patients undergoing angiography only and for those revascularized with PCI or CABG (p = 0.125; Fig. 4a). Revascularization with PCI or CABG was not independently associated with 30-day survival after adjustment for age and other baseline characteristics (adjusted ORPCI 0.77 [95% CI 0.41–1.43], adjusted ORCABG 0.48 [95% CI 0.12–1.96]).
Fig. 4.
Actual revascularization. NSTEMI patients ≥75 years managed with angiography only (a), angiography + PCI (b) or angiography + CABG (c). a 30-Day survival. Kaplan-Meier survival plot. b Long-term survival after 30 days. Kaplan-Meier survival plot. PCI, percutaneous coronary intervention; CABG, coronary artery bypass grafting; revasc, revascularization.
After 30-days, estimated 7-year survival was 43.7% (95% CI 37.2–50.1) for patients with angiography only (n = 467), 55.1% (95% CI 49.0–60.8) with PCI (n = 544), and 67.5% (95% CI 55.4–77.0) with CABG (n = 125; Fig. 4b). After 30 days, actual revascularization with PCI or CABG was associated with lower risk of long-term mortality, also after multivariate adjustment (aHRPCI 0.73 [95% CI 0.59–0.90], p = 0.003 and aHRCABG 0.43 [95% CI 0.28–0.65], p < 0.0001). The PH-assumption was regarded valid.
Discussion
In this observational study of patients with NSTEMI aged ≥75 years, the main findings were (1) 30-day survival was near 95%, and 7-year survival was almost 50%, with the use of an invasive strategy. (2) Short- and long-term survival in the conservative group were lower, with a 30-day survival of 77%, and 7-year survival of only 12%. (3) Among invasively treated patients, revascularization with PCI or CABG was associated with improved long-term survival compared to angiography only.
To our knowledge, this is the first study to document survival exceeding 1 year for NSTEMI patients ≥75 years treated with an invasive strategy. In line with our results, previous studies have reported in-hospital mortality ranging from 4 to 6% for invasively treated versus 7–11% for conservatively treated elderly patients with NSTE-ACS [9, 11]. Among 1,936 NSTEMI patients ≥75 years, 1-year mortality was 10.7% for invasively versus 27.9% for conservatively treated [10]. In a pooled analysis from the FRISC-II, Conservative Treatment in Unstable Coronary Syndromes and RITA-3 (FIR) trials, 5-year cardiovascular mortality for elderly NSTE-ACS patients was only 18.5% [3]. The diverging results of mortality in observational cohorts and RCT's, suggest selection of healthier, lower-risk patients for RCTs than in real-life clinical practice. The problem in the present study was a selection of patients considered for an invasive strategy, both in community hospitals and in the tertiary center. Selection bias can result in overestimation of survival rates or the effect of an intervention. Since this was a registry based on clinical practice, the therapeutic strategy was at the physician's discretion, and no specific exclusion criteria were applied for invasive treatment. The lack of specific criteria for therapeutic strategy might limit the external validity and generalizability of our results. Furthermore, patients in our study were treated in 2005–2011, before wide use of 2nd generation drug-eluting stents, newer antiplatelet agents and catheterization techniques and survival rates may not be generalizable to all elderly NSTEMI patients.
Although RCTs are the gold standard for evaluating the effect of interventions, including elderly patients in clinical trials may be difficult, and RCTs of invasive treatment in elderly patients have been terminated prematurely due to slow recruitment [26]. Therefore, results from observational studies with high internal validity can provide important knowledge reflecting clinical practice for elderly patients underrepresented or excluded from clinical trials [27].
As expected, patients treated invasively in our study were younger (mean age 80.4 vs. 86.4 years). They were more likely men and had a higher percentage previous revascularization, but less often had a previous stroke. These factors are associated with risk of CAD and adverse outcomes in the setting of ACS [28, 29]. Other known prognostic factors, such as bleeding history or anaemia [29], were not registered in this study, but may have influenced the treatment decision and outcomes in this elderly cohort. Diabetes, hypertension, and peripheral artery disease were similar for patients treated invasively or conservatively [30]. The fact that higher risk elderly AMI patients are not treated invasively is described as the “age-risk paradox” [31], that is, the advantage of PCI increases with background risk, but that increased background risk results in a patient not being revascularized. Complicating observational studies of elderly patients, it may be the presence of contraindications to coronary angiography or PCI (and thus another disease), that account for the increased mortality risk, and not the conservative strategy itself [32]. Comorbidities such as cancer, liver disease, dementia, or chronic obstructive pulmonary disease and life expectancy should be considered [4] in the choice of treatment strategy. Previous studies of elderly patients with AMI or NSTE-ACS have reported lower prevalence of comorbidities among invasively compared to conservatively treated (chronic obstructive pulmonary disease 10–18 vs. 13–26%, cancer 6 vs. 12%, and dementia 5 vs. 18%, respectively) [9, 33]. Frailty can be defined as an age-related vulnerability to a stressor event, increasing the risk of adverse outcomes [34]. Mortality risk is increased among frail compared to non-frail elderly AMI patients, independent of chronological age and clinical risk scores [35, 36, 37, 38]. Unfortunately, these factors were not registered in the present study and could therefore not be adjusted for in the risk estimates.
Patients treated invasively had lower levels of s-creatinine at admission compared to patients treated conservatively. Our finding of effect modification by level of s-creatinine suggests the invasive strategy to be less effective in elderly NSTEMI patients with renal dysfunction. This corresponds to findings that moderate to severe renal dysfunction is associated with mortality among invasively treated AMI patients [20]. There is a need for more knowledge about the influence of an invasive strategy in elderly NSTEMI patients with renal dysfunction.
The association between actual revascularization with PCI or CABG and improved long-term survival may be less influenced by selection bias. Reasons for not performing PCI or CABG were unfortunately not registered in our study, and factors such as non-obstructive coronary lesions, unsuitable coronary anatomy, technical difficulties, or per-procedural complications may have influenced long-term survival. In line with our results, a per-protocol analysis from the Invasive versus Conservative Treatment in Unstable Coronary Syndromes trial [39] found that actual revascularization was associated with reduced 4-year mortality among NSTE-ACS patients, as opposed to the original intention-to-treat analysis that was neutral [24].
Our study describes better survival for elderly NSTEMI patients clinically selected for an invasive strategy compared to conservative strategy. However, the study was not designed for determining a treatment effect, and selection bias and confounding factors may account for the observed difference in risk and survival between groups. Patients that were revascularized had a better long-term prognosis. The proportion of elderly patients treated with an invasive strategy was quite low (only 48%), as in previous studies of elderly NSTE-ACS patients [9, 10, 11]. However, a total of 59% of NSTEMI patients ≥75 years treated with an invasive strategy were revascularized. For comparison, 67% of invasively treated in the total cohort of NSTEMI patients during 2005–2011 from our center (all ages) received actual revascularization [40]. One can speculate that more elderly NSTEMI patients could benefit from an invasive strategy with revascularization. With the higher life expectancy and growth of the elderly population, an evidence-based strategy on how to treat elderly patients with NSTEMI is essential [8]. Adequately powered RCTs for mortality after an invasive versus conservative strategy in elderly AMI patients are wanted. Awaiting this, more descriptive studies are needed of prognostic factors both for treatment decisions and long-term survival to better anticipate the best treatment for complex, high-risk individuals, often found among elderly patients.
Strengths and Limitations
The strengths of our study are long-term survival estimates for a large, consecutive NSTEMI cohort ≥75 years reflecting clinical practice. The subgroup analysis of actual revascularization differentiates between patients selected for an invasive strategy based on clinical features and shows a strong association between treatment and long-term survival for elderly NSTEMI patients. The landmark analysis of survival after 30 days was performed to reduce immortal time bias [41], that is, bias due to acute illness severity with death before coronary angiography could be performed.
The main limitation of our study was the observational design with a physician selection of patients for invasive or conservative strategy. The treatment decision was not registered. Unmeasured confounding may have influenced the treatment strategy and survival. Heart rate, blood pressure, left ventricular ejection fraction, medications after discharge, and compliance were not registered. With the emergence of high-sensitivity cardiac troponin assays and increasing awareness that reference values may be different for women and men, diagnostic sensitivity for NSTEMI may have changed since the study period [42]. In the future, characteristics of clinical NSTEMI cohorts may potentially alter due to enhanced diagnostic accuracy and risk stratification by added biomarkers, that is, growth differentiation factor-15, natriuretic peptides, copeptin, or heart-type fatty acid-binding protein [43, 44, 45].
Revascularization or cardiac rehabilitation during follow-up may have influenced long-term survival. Non-cardiovascular causes of death may influence long-term survival [40], especially in elderly cohorts. End points such as burden of symptoms, hospital readmissions, or quality of life during long-term follow-up are all important outcomes, which should be included in future studies.
This study was conducted in a university hospital, being a combination of a community hospital and a tertiary cardiac center, and the results are not necessarily generalizable to all elderly NSTEMI patients. Despite our efforts to convey bias by prospective registration, landmark analysis, and controlling for confounders, a causal effect of an invasive strategy on survival in elderly NSTEMI patients cannot be inferred.
Conclusion
In this real-life cohort of NSTEMI patients ≥75 years, 30-day survival was 95%, and 7-year survival was 47% with an invasive strategy. Revascularized patients had a superior long-term prognosis. Short- and long-term survival with a conservative strategy was significantly lower, probably due to selection bias and unmeasured confounding.
Disclosure Statement
The authors have no conflicts of interest to disclose.
Funding Source
Funded by grant number 2013028 from the Scientific Board of the South-Eastern Norway Regional Health Authority, Hamar, Norway.
Author Contributions
K.M.K.: has contributed in study design, validation, analysis and interpretation of results, drafting of the paper, tables and figures, and writing of the final document. J.M.G.: has contributed in study design, analysis and interpretation of results, and writing of the final document. J.E. and G.O.A. have contributed in data collection, study design, analysis and interpretation of results, and writing of the final document. E.F. have contributed in study design, analysis and interpretation of results, and writing of the final document. C.H.H. have contributed in data collection, validation and writing of the final document. S.H. had the MI registry idea, contributed in study design, validation, analysis and interpretation of results, drafting of the paper and tables, and writing of the final document. All authors have approved the final version for publication.
Acknowledgments
The authors wish to thank the physicians at the Department of Cardiology, OUH Ulleval, for data collection, the Mid-Norway Regional Health Authority for supplying the electronic database, and the Norwegian Cause of Death registry for mortality data.
References
- 1.Lagerqvist B, Husted S, Kontny F, Ståhle E, Swahn E, Wallentin L, Fast Revascularisation during InStability in Coronary artery disease (FRISC-II) Investigators 5-year outcomes in the FRISC-II randomised trial of an invasive versus a non-invasive strategy in non-ST-elevation acute coronary syndrome: a follow-up study. Lancet. 2006 Sep;368((9540)):998–1004. doi: 10.1016/S0140-6736(06)69416-6. [DOI] [PubMed] [Google Scholar]
- 2.Fox KA, Clayton TC, Damman P, Pocock SJ, de Winter RJ, Tijssen JG, et al. FIR Collaboration Long-term outcome of a routine versus selective invasive strategy in patients with non-ST-segment elevation acute coronary syndrome a meta-analysis of individual patient data. J Am Coll Cardiol. 2010 Jun;55((22)):2435–45. doi: 10.1016/j.jacc.2010.03.007. [DOI] [PubMed] [Google Scholar]
- 3.Damman P, Clayton T, Wallentin L, Lagerqvist B, Fox KA, Hirsch A, et al. Effects of age on long-term outcomes after a routine invasive or selective invasive strategy in patients presenting with non-ST segment elevation acute coronary syndromes: a collaborative analysis of individual data from the FRISC II - ICTUS - RITA-3 (FIR) trials. Heart. 2012 Feb;98((3)):207–13. doi: 10.1136/heartjnl-2011-300453. [DOI] [PubMed] [Google Scholar]
- 4.Roffi M, Patrono C, Collet JP, Mueller C, Valgimigli M, Andreotti F, et al. ESC Scientific Document Group 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC) Eur Heart J. 2016 Jan;37((3)):267–315. doi: 10.1093/eurheartj/ehv320. [DOI] [PubMed] [Google Scholar]
- 5.Amsterdam EA, Wenger NK, Brindis RG, Casey DE, Jr, Ganiats TG, Holmes DR, Jr, et al. ACC/AHA Task Force Members. Society for Cardiovascular Angiography and Interventions and the Society of Thoracic Surgeons 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014 Dec;130((25)):2354–94. doi: 10.1161/CIR.0000000000000133. [DOI] [PubMed] [Google Scholar]
- 6.Bach RG, Cannon CP, Weintraub WS, DiBattiste PM, Demopoulos LA, Anderson HV, et al. The effect of routine, early invasive management on outcome for elderly patients with non-ST-segment elevation acute coronary syndromes. Ann Intern Med. 2004 Aug;141((3)):186–95. doi: 10.7326/0003-4819-141-3-200408030-00007. [DOI] [PubMed] [Google Scholar]
- 7.Savonitto S, Cavallini C, Petronio AS, Murena E, Antonicelli R, Sacco A, et al. Italian Elderly ACS Trial Investigators Early aggressive versus initially conservative treatment in elderly patients with non-ST-segment elevation acute coronary syndrome: a randomized controlled trial. JACC Cardiovasc Interv. 2012 Sep;5((9)):906–16. doi: 10.1016/j.jcin.2012.06.008. [DOI] [PubMed] [Google Scholar]
- 8.Tegn N, Abdelnoor M, Aaberge L, Endresen K, Smith P, Aakhus S, et al. After Eighty study investigators Invasive versus conservative strategy in patients aged 80 years or older with non-ST-elevation myocardial infarction or unstable angina pectoris (After Eighty study): an open-label randomised controlled trial. Lancet. 2016 Mar;387((10023)):1057–65. doi: 10.1016/S0140-6736(15)01166-6. [DOI] [PubMed] [Google Scholar]
- 9.Kolte D, Khera S, Palaniswamy C, Mujib M, Fonarow GC, Ahmed A, et al. Early invasive versus initial conservative treatment strategies in octogenarians with UA/NSTEMI. Am J Med. 2013 Dec;126((12)):1076–83.e1. doi: 10.1016/j.amjmed.2013.07.024. [DOI] [PubMed] [Google Scholar]
- 10.Bauer T, Koeth O, Jünger C, Heer T, Wienbergen H, Gitt A, et al. Acute Coronary Syndromes Registry (ACOS) Investigators Effect of an invasive strategy on in-hospital outcome in elderly patients with non-ST-elevation myocardial infarction. Eur Heart J. 2007 Dec;28((23)):2873–8. doi: 10.1093/eurheartj/ehm464. [DOI] [PubMed] [Google Scholar]
- 11.Devlin G, Gore JM, Elliott J, Wijesinghe N, Eagle KA, Avezum A, et al. GRACE Investigators Management and 6-month outcomes in elderly and very elderly patients with high-risk non-ST-elevation acute coronary syndromes: The Global Registry of Acute Coronary Events. Eur Heart J. 2008 May;29((10)):1275–82. doi: 10.1093/eurheartj/ehn124. [DOI] [PubMed] [Google Scholar]
- 12.Alpert JS, Thygesen K, Antman E, Bassand JP. Myocardial infarction redefined—a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol. 2000 Sep;36((3)):959–69. doi: 10.1016/s0735-1097(00)00804-4. [DOI] [PubMed] [Google Scholar]
- 13.Thygesen K, Alpert JS, White HD, Jaffe AS, Apple FS, Galvani M, et al. Joint ESC/ACCF/AHA/WHF Task Force for the Redefinition of Myocardial Infarction Universal definition of myocardial infarction. Eur Heart J. 2007 Oct;28((20)):2525–38. doi: 10.1093/eurheartj/ehm355. [DOI] [PubMed] [Google Scholar]
- 14.Kvakkestad KM, Abdelnoor M, Claussen PA, Eritsland J, Fossum E, Halvorsen S. Long-term survival in octogenarians and older patients with ST-elevation myocardial infarction in the era of primary angioplasty: A prospective cohort study. Eur Heart J Acute Cardiovasc Care. 2016 Jun;5((3)):243–52. doi: 10.1177/2048872615574706. [DOI] [PubMed] [Google Scholar]
- 15.Claussen PA, Abdelnoor M, Kvakkestad KM, Eritsland J, Halvorsen S. Prevalence of risk factors at presentation and early mortality in patients aged 80 years or older with ST-segment elevation myocardial infarction. Vasc Health Risk Manag. 2014 Dec;10:683–9. doi: 10.2147/VHRM.S72764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van Houwelingen HC. Dynamic Prediction by Landmarking in Event History Analysis. Scand J Stat. 2007;34((1)):70–85. [Google Scholar]
- 17.Bagnall AJ, Goodman SG, Fox KA, Yan RT, Gore JM, Cheema AN, et al. Canadian Acute Coronary Syndrome Registry I and II Investigators. Canadian Global Registry of Acute Coronary Events (GRACE/GRACE2) Investigators Influence of age on use of cardiac catheterization and associated outcomes in patients with non-ST-elevation acute coronary syndromes. Am J Cardiol. 2009 Jun;103((11)):1530–6. doi: 10.1016/j.amjcard.2009.01.369. [DOI] [PubMed] [Google Scholar]
- 18.Milcent C, Dormont B, Durand-Zaleski I, Steg PG. Gender differences in hospital mortality and use of percutaneous coronary intervention in acute myocardial infarction: microsimulation analysis of the 1999 nationwide French hospitals database. Circulation. 2007 Feb;115((7)):833–9. doi: 10.1161/CIRCULATIONAHA.106.664979. [DOI] [PubMed] [Google Scholar]
- 19.DeGeare VS, Stone GW, Grines L, Brodie BR, Cox DA, Garcia E, et al. Angiographic and clinical characteristics associated with increased in-hospital mortality in elderly patients with acute myocardial infarction undergoing percutaneous intervention (a pooled analysis of the primary angioplasty in myocardial infarction trials) Am J Cardiol. 2000 Jul;86((1)):30–4. doi: 10.1016/s0002-9149(00)00824-9. [DOI] [PubMed] [Google Scholar]
- 20.Sabroe JE, Thayssen P, Antonsen L, Hougaard M, Hansen KN, Jensen LO. Impact of renal insufficiency on mortality in patients with ST-segment elevation myocardial infarction treated with primary percutaneous coronary intervention. BMC Cardiovasc Disord. 2014 Feb;14((1)):15. doi: 10.1186/1471-2261-14-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kvakkestad KM, Sandvik L, Andersen GO, Sunde K, Halvorsen S. Long-term survival in patients with acute myocardial infarction and out-of-hospital cardiac arrest: A prospective cohort study. Resuscitation. 2018 Jan;122:41–7. doi: 10.1016/j.resuscitation.2017.11.047. [DOI] [PubMed] [Google Scholar]
- 22.Carnendran L, Abboud R, Sleeper LA, Gurunathan R, Webb JG, Menon V, et al. Trends in cardiogenic shock: report from the SHOCK Study. The SHould we emergently revascularize Occluded Coronaries for cardiogenic shocK? Eur Heart J. 2001 Mar;22((6)):472–8. doi: 10.1053/euhj.2000.2312. [DOI] [PubMed] [Google Scholar]
- 23.Wu AH, Parsons L, Every NR, Bates ER, Second National Registry of Myocardial Infarction Hospital outcomes in patients presenting with congestive heart failure complicating acute myocardial infarction: a report from the Second National Registry of Myocardial Infarction (NRMI-2) J Am Coll Cardiol. 2002 Oct;40((8)):1389–94. doi: 10.1016/s0735-1097(02)02173-3. [DOI] [PubMed] [Google Scholar]
- 24.Hirsch A, Windhausen F, Tijssen JG, Oude Ophuis AJ, van der Giessen WJ, van der Zee PM, et al. Invasive versus Conservative Treatment in Unstable coronary Syndromes Investigators Diverging associations of an intended early invasive strategy compared with actual revascularization, and outcome in patients with non-ST-segment elevation acute coronary syndrome: the problem of treatment selection bias. Eur Heart J. 2009 Mar;30((6)):645–54. doi: 10.1093/eurheartj/ehn438. [DOI] [PubMed] [Google Scholar]
- 25.STROBE statement—checklist of items that should be included in reports of observational studies (STROBE initiative) Int J Public Health. 2008;53((1)):3–4. doi: 10.1007/s00038-007-0239-9. [DOI] [PubMed] [Google Scholar]
- 26.Bueno H, Betriu A, Heras M, Alonso JJ, Cequier A, García EJ, et al. TRIANA Investigators Primary angioplasty vs. fibrinolysis in very old patients with acute myocardial infarction: TRIANA (TRatamiento del Infarto Agudo de miocardio eN Ancianos) randomized trial and pooled analysis with previous studies. Eur Heart J. 2011 Jan;32((1)):51–60. doi: 10.1093/eurheartj/ehq375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sørensen HT, Lash TL, Rothman KJ. Beyond randomized controlled trials: a critical comparison of trials with nonrandomized studies. Hepatology. 2006 Nov;44((5)):1075–82. doi: 10.1002/hep.21404. [DOI] [PubMed] [Google Scholar]
- 28.Six AJ, Backus BE, Kelder JC. Chest pain in the emergency room: value of the HEART score. Neth Heart J. 2008 Jun;16((6)):191–6. doi: 10.1007/BF03086144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moscucci M, Fox KA, Cannon CP, Klein W, López-Sendón J, Montalescot G, et al. Predictors of major bleeding in acute coronary syndromes: the Global Registry of Acute Coronary Events (GRACE) Eur Heart J. 2003 Oct;24((20)):1815–23. doi: 10.1016/s0195-668x(03)00485-8. [DOI] [PubMed] [Google Scholar]
- 30.Fox KA, Carruthers KF, Dunbar DR, Graham C, Manning JR, De Raedt H, et al. Underestimated and under-recognized: the late consequences of acute coronary syndrome (GRACE UK-Belgian Study) Eur Heart J. 2010 Nov;31((22)):2755–64. doi: 10.1093/eurheartj/ehq326. [DOI] [PubMed] [Google Scholar]
- 31.Di Bari M, Balzi D, Fracchia S, Barchielli A, Orso F, Sori A, et al. Acute Myocardial Infarction in Florence 2 (AMI Florence-2) Working Group Decreased usage and increased effectiveness of percutaneous coronary intervention in complex older patients with acute coronary syndromes. Heart. 2014 Oct;100((19)):1537–42. doi: 10.1136/heartjnl-2013-305445. [DOI] [PubMed] [Google Scholar]
- 32.Gottlieb S, Boyko V, Harpaz D, Hod H, Cohen M, Mandelzweig L, et al. Israeli Thrombolytic Survey Group Long-term (three-year) prognosis of patients treated with reperfusion or conservatively after acute myocardial infarction. J Am Coll Cardiol. 1999 Jul;34((1)):70–82. doi: 10.1016/s0735-1097(99)00152-7. [DOI] [PubMed] [Google Scholar]
- 33.Libungan B, Karlsson T, Albertsson P, Herlitz J. Elderly patients with myocardial infarction selected for conservative or invasive treatment strategy. Clin Interv Aging. 2015 Jan;10:321–7. doi: 10.2147/CIA.S74012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013 Mar;381((9868)):752–62. doi: 10.1016/S0140-6736(12)62167-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ekerstad N, Swahn E, Janzon M, Alfredsson J, Löfmark R, Lindenberger M, et al. Frailty is independently associated with 1-year mortality for elderly patients with non-ST-segment elevation myocardial infarction. Eur J Prev Cardiol. 2014 Oct;21((10)):1216–24. doi: 10.1177/2047487313490257. [DOI] [PubMed] [Google Scholar]
- 36.Sanchis J, Bonanad C, Ruiz V, Fernández J, García-Blas S, Mainar L, et al. Frailty and other geriatric conditions for risk stratification of older patients with acute coronary syndrome. Am Heart J. 2014 Nov;168((5)):784–91. doi: 10.1016/j.ahj.2014.07.022. [DOI] [PubMed] [Google Scholar]
- 37.Pogorevici A, Citu IM, Bordejevic DA, Caruntu F, Tomescu MC. Canada acute coronary syndrome score was a stronger baseline predictor than age ≥75 years of in-hospital mortality in acute coronary syndrome patients in western Romania. Clin Interv Aging. 2016 Apr;11:481–8. doi: 10.2147/CIA.S104943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.White HD, Westerhout CM, Alexander KP, Roe MT, Winters KJ, Cyr DD, et al. TRILOGY ACS investigators Frailty is associated with worse outcomes in non-ST-segment elevation acute coronary syndromes: insights from the TaRgeted platelet Inhibition to cLarify the Optimal strateGy to medicallY manage Acute Coronary Syndromes (TRILOGY ACS) trial. Eur Heart J Acute Cardiovasc Care. 2016 Jun;5((3)):231–42. doi: 10.1177/2048872615581502. [DOI] [PubMed] [Google Scholar]
- 39.Hirsch A, Windhausen F, Tijssen JG, Verheugt FW, Cornel JH, de Winter RJ, Invasive versus Conservative Treatment in Unstable coronary Syndromes (ICTUS) investigators Long-term outcome after an early invasive versus selective invasive treatment strategy in patients with non-ST-elevation acute coronary syndrome and elevated cardiac troponin T (the ICTUS trial): a follow-up study. Lancet. 2007 Mar;369((9564)):827–35. doi: 10.1016/S0140-6736(07)60410-3. [DOI] [PubMed] [Google Scholar]
- 40.Kvakkestad KM, Wang Fagerland M, Eritsland J, Halvorsen S. Gender differences in all-cause, cardiovascular and cancer mortality during long-term follow-up after acute myocardial infarction; a prospective cohort study. BMC Cardiovasc Disord. 2017 Mar;17((1)):75. doi: 10.1186/s12872-017-0508-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Suissa S. Immortal time bias in pharmaco-epidemiology. Am J Epidemiol. 2008 Feb;167((4)):492–9. doi: 10.1093/aje/kwm324. [DOI] [PubMed] [Google Scholar]
- 42.Shah AS, McAllister DA, Mills R, Lee KK, Churchhouse AM, Fleming KM, et al. Sensitive troponin assay and the classification of myocardial infarction. Am J Med. 2015 May;128((5)):493–501.e3. doi: 10.1016/j.amjmed.2014.10.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mueller C. Biomarkers and acute coronary syndromes: an update. Eur Heart J. 2014 Mar;35((9)):552–6. doi: 10.1093/eurheartj/eht530. [DOI] [PubMed] [Google Scholar]
- 44.Wang J, Wei L, Yang X, Zhong J. Roles of Growth Differentiation Factor 15 in Atherosclerosis and Coronary Artery Disease. J Am Heart Assoc. 2019 Sep;8((17)):e012826. doi: 10.1161/JAHA.119.012826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mueller C, Möckel M, Giannitsis E, Huber K, Mair J, Plebani M, et al. ESC Study Group on Biomarkers in Cardiology of the Acute Cardiovascular Care Association Use of copeptin for rapid rule-out of acute myocardial infarction. Eur Heart J Acute Cardiovasc Care. 2018 Sep;7((6)):570–6. doi: 10.1177/2048872617710791. [DOI] [PubMed] [Google Scholar]