Abstract
Background and Purpose
Stroke is the leading cause of serious, long-term disability in the United States and the number of stroke survivors is projected to rise. Physical functioning status may be compromised in survivors living in low socioeconomic status environments in comparison to higher socioeconomic status environments. Higher socioeconomic status environments may include benefits in the built environment such as sidewalks, accessible transit, or low traffic volume. Investigation is needed to understand the effects of the socioenvironmental context on trajectories of stroke survivors’ physical health-related quality of life (PH-QOL) over time.
Methods
Participants from the REasons for Geographic and Racial Differences in Stroke (REGARDS) study enrolled in the ancillary Caring for Adults Recovering from the Effects of Stroke (CARES) project completed the SF-12 around 6–12, 18, 27, and 36 months post-stroke. Measures of area-level income, wealth, education, and employment at the census tract level were combined to represent participants’ neighborhood socioeconomic status (nSES). Linear mixed models were used to predict trajectories of PH-QOL over time, controlling for individual characteristics.
Results
The average trajectory of PH-QOL was flat over time. However, women and younger stroke survivors had better trajectories over time than men and older stroke survivors. Higher nSES was significantly associated with better PH-QOL across all time points (β=1.73, 95% CI: 0.17, 3.30), after controlling for demographic variables and severity of stroke.
Conclusions
Our findings demonstrate that nSES, gender, and age are associated with the post-stroke recovery process. The results of this study suggest the importance of evaluating the environment surrounding stroke survivors when they return to their home communities. Future research should identify specific features of the environment within different socioeconomic status neighborhoods to better understand how they contribute to PH-QOL among stroke survivors.
Keywords: Neighborhood, Stroke, Socioeconomic status, Longitudinal study
Subject terms: Ischemic Stroke, Intracranial Hemorrhage, Quality and Outcomes
INTRODUCTION
Stroke is a leading cause of serious long-term disability within the United States.1, 2 Individuals that continue to live within their community with the residual effects of a stroke often experience change in their health-related quality of life.3, 4 Stroke survivors have often reported lower physical health-related quality of life (PH-QOL) in comparison to non-stroke community-dwelling seniors.3, 5, 6 PH-QOL theoretically reflects elements of physiologic reserve and has been shown to be a powerful predictor of health outcomes, such as mortality and physical function.7, 8 Acquired functioning limitations due to a stroke, such as physical and cognitive limitations, have repeatedly been found to reduce stroke survivors’ PH-QOL.4, 6, 9
However, some individuals appear to adapt to ongoing cognitive and mobility limitations and report a high PH-QOL.4, 5, 10 Most often, higher PH-QOL is achieved through continued engagement in social interactions and participation in valued life activities.5, 10 To minimize the decline in PH-QOL, stroke survivors can increase social support, access educational resources, or decrease social isolation.3–5, 10 Pearlin’s theory of sociology of stress suggests that attributes of the built and social environment may serve as buffers by moderating the relationship between stressful life events and health outcomes.11 After a stroke, individuals may be more or less susceptible to indirect negative health consequences as a function of the built and social environment surrounding them. Hence, it is important to investigate if structural characteristics surrounding stroke survivors play a role in trajectories of engagement and participation within their community.
Approximately 20% of PH-QOL within the general United States population can be attributed to direct clinical care.12 The remaining 80% of PH-QOL can be attributed to social and economic factors, the physical environment, and health behaviors. There is a need to identify areas outside of clinical care, within the socio-environmental context, that influence individual PH-QOL post-stroke. Previous studies have observed that women have lower PH-QOL than men post-stroke, and that gender differences in PH-QOL widen over time.13 Age has also been identified as an important socio-environmental characteristic, whereby strokes at a later age result in worse PH-QOL and declining PH-QOL trajectories.14 Lastly, neighborhood socioeconomic status (nSES) captures the context in which people live and possess both physical and social attributes which has been previously shown to predict stroke mortality.15 Our goal is to examine long-term trajectories of PH-QOL and determine if socio-environmental characteristics shape PH-QOL trajectories. To accomplish this goal, we investigated stroke survivors’ change in PH-QOL over time, the effects of demographic characteristics (i.e., age, gender) and nSES on change in PH-QOL over time, and explored the interaction of these factors.
METHODS
To abide by its obligations with the National Institutes of Health/National Institute of Neurological Disorders and Stroke, the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study facilitates data sharing through formal data use agreements. Any investigator is welcome to access the REGARDS data through this process. Requests for data access may be sent to regardsadmin@uab.edu.
Study Population
Study participants were randomly selected from a commercially available list of individuals living within the United States. Through a stratified random sampling design REGARDS aimed to enroll half African American participants and half White participants, half male participants and half female participants, and half of the participants holding residence within the “stroke belt” region (states of AL, AR, GA, LA, MS, NC, SC, and TN) and half of the participants holding residence within the other 48 contiguous states. Potential participants were invited via mail and then followed up with attempted contact through phone calls. Initial screening for eligibility was completed. In order to be eligible for the parent REGARDS study, all participants needed to be: age 45 or older; self-identify as African American or White and not Hispanic; no previous diagnosis of cancer; ability to communicate in English; and not hold residence or be on a waiting list for a nursing home. The proportion of known eligible participants who agreed to be interviewed was over 60%.16 The sampling, recruitment, and telephone interviewing procedures for REGARDS have been described in additional detail elsewhere.16 After enrollment, REGARDS administered a computer-assisted telephone interview to obtain baseline information included in this analysis: race, gender, age, education, and income. Participants were contacted every six months to collect information about incident stroke.
Those who self-reported stroke symptoms during a follow-up call within the parent REGARDS study were potential participants for the Caring for Adults Recovering from the Effects of Stroke (CARES) ancillary study.17, 18 Beginning in August of 2005, trained interviewers contacted potential participants from the parent REGARDS cohort and established eligibility for the CARES study. Participants were eligible for the CARES study if they were community-dwelling, active participants within REGARDS, self-reported incident stroke, and had a primary family caregiver who would agree to participate.17, 18
Within the current project, participants were excluded from the study sample if there was no confirmation of stroke through medical record review. Within REGARDS, two trained adjudicators with expertise in stroke, including one neurologist, reviewed and adjudicated index hospitalization event medical records. The same two adjudicators used diagnostic data and imaging to confirm stroke and record stroke severity. The CARES enrollment goal was to complete baseline interviews 6 to 12 months post-stroke.17, 18 Follow-up assessments were then scheduled around 18, 27, and 36 months after the stroke date, totaling up to four longitudinal data points collected within the CARES study.17, 18 Participants provided written informed consent to be a part of both CARES and REGARDS, and studies were approved by all participating Institutional Review Boards.
Measures
The main exposure variable, nSES, was calculated based on participants’ census tract. To obtain nSES, each participant’s baseline address was geocoded using ArcGIS. Only results where geocoding could match an address to a longitude/latitude with 80% or higher probability were included in this study. The geocoded address was linked to its respective census tract based on the 2013 Census TIGER/Lines (US Census Bureau, Geography Division). An index of nSES used in previous research was calculated based on six census variables from the 2013 American Communities Survey including: log of median household income, log of median value of owner-occupied housing units, proportion of households receiving interest, dividend, or net rental income, proportion of adults aged ≥25 years with a high school diploma, proportion of adults aged ≥25 years with college degree, and proportion of people employed in executive, managerial, or professional occupations.19, 20 The composite nSES variable is a standard score according to the United States nSES distribution. When considering all tracts in the United States, the nSES variable had a mean of 0 and a standard deviation of 1, with higher scores indicating higher socioeconomic status of the neighborhood.
The main outcome of this study, PH-QOL, was self-reported using the SF-12 around 6–12, 18, 27, and 36 months post-stroke. A physical composite score representing PH-QOL was calculated using weighted item composites from the SF-12. The score was then standardized to have a population mean of 50 and standard deviation of 10, with higher scores indicating better self-reported functioning. PH-QOL has been shown to be valid and reliable measure of health-related quality of life.21 The time of each PH-QOL observation was calculated by taking the date of observation and subtracting the stroke date, resulting in the number of days since stroke. For ease of interpretation, the number of days was divided by 30 to provide an estimate of time that indicates the months since the stroke date, and time (months) was centered at six months post-stroke.
Confounders included in this analysis are age, gender, race, education, and income. In addition, we adjusted for stroke severity so that PH-QOL is comparable across subjects. Stroke severity and age at the time of stroke were obtained through medical record review. The National Institute of Health Stroke Scale (NIHSS) is a measure of stroke severity that is widely used and has shown to be a reliable, valid, and responsive tool to measure stroke severity.22 Scores on NIHSS range from 0 to 42, with higher scores indicating a more severe stroke. Age was centered at age 75, the overall mean of the study population for interpretability of the intercepts. Self-reported gender (male, female), race (white, black), education (less than high school, high school graduate, some college, college graduate or more), and income (less than $20,000, $20,00-$34,999, $35,000-$74,999, $75,000 or more) were obtained through the parent REGARDS study during the baseline assessment.
Statistical Analysis
Demographic, health, and neighborhood characteristics were summarized for the total study sample and stratified by tertile of nSES. Participants whose first observation date was greater than 36 months post-stroke, were excluded from the analysis (N=11). Three participants (1%) were missing nSES and 48 participants (17%) were missing NIHSS. Multiple imputation techniques were used to classify missing data in predictor variables to reduce potential biases and improve precision in our estimates.23 This model included nSES, stroke severity, education, income, race, gender, and age as predictors. One hundred datasets including imputed outcomes were generated, with estimates produced using the STATA procedure MI ESTIMATE. Details of this approach are available elsewhere.24
To estimate the trajectories of the PH-QOL over time post-stroke we utilized linear mixed modeling. Using linear mixed modeling procedures we first estimated the average trajectory of the PH-QOL with time (months) as a predictor, accounting for the correlation of variance of observations within an individual. Models were estimated using maximum likelihood estimation. Within the first model we assessed the correlation of observations over time and different functional forms of time. The second model included characteristics of the individual (i.e.., age, gender), testing for their influence on the trajectories of PH-QOL over time (i.e.., age by time interaction, gender by time interaction). Gender and age associations with PH-QOL trajectories were identified a priori as important socio-environmental characteristics of post-stroke health.13, 14 The third model included a main effect of nSES on the PH-QOL intercept. Within our final, and fourth model, we assessed the interaction between nSES and time to examine the influence of nSES on the trajectories of PH-QOL over time. The association between nSES and trajectories of PH-QOL was identified a priori given the social and physical attributes of neighborhoods that have been previously associated with overall health and wellbeing.25 Throughout the model fitting process Bayesian Information Criterion (BIC) was assessed to provide evidence for the fit of the model, with lower BIC values indicating a better model fit.26
RESULTS
A total of 360 participants were enrolled into the CARES sample. Of the 360 participants, 55 did not have an adjudicated stroke, 11 participants first observation was beyond 36 months post-stroke, and 10 participants’ stroke event occurred after the follow-up observations. This resulted in a total sample size of 284 participants in our analytic sample. Stroke participants within our analytic sample completed their first CARES questionnaire an average of five months after their first self-reported stroke symptoms, and 69 months after their initial baseline assessment from the REGARDS parent study. As shown in Table 1, the average age of participants at the time of their stroke was 74 years of age, those living in high nSES environments tended to be older than those living in mid or low nSES environments. Approximately half of our study sample were female, the proportion of which decreased with increasing nSES. Approximately 60% of the sample self-identified as white, the proportion of which drastically increased with increasing nSES. The proportion of participants with higher individual-level education and income increased with increasing nSES. Self-reported PH-QOL was somewhat stable over time for the study sample, but varied between tertiles of nSES (Table 1).
Table 1.
Demographic, functioning, and socioeconomic characteristics by neighborhood socioeconomic status (nSES) tertilea among participants included in the study sample who were enrolled in the CARES ancillary study.
| Overall (n = 284b) |
Low nSES (n = 131) |
Mid nSES (n = 88) |
High nSES (n = 65) |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | Mean/% | SD | Mean/% | SD | Mean/% | SD | Mean/% | SD | |
| Age at stroke | 74.3 | 0.4 | 73.3 | 0.7 | 74.4 | 0.8 | 76.2 | 0.8 | |
| Female | 49.6 | 59.5 | 40.9 | 41.5 | |||||
| White | 59.5 | 35.1 | 73.9 | 89.2 | |||||
| NIHSS | 2.0 | 0.2 | 2.2 | 0.3 | 2.5 | 0.5 | 0.9 | 0.3 | |
| Education | |||||||||
| < HS | 13.7 | 20.6 | 10.2 | 4.6 | |||||
| HS graduate | 26.4 | 29.0 | 27.3 | 20.0 | |||||
| Some college | 27.5 | 27.5 | 30.7 | 23.1 | |||||
| College graduate + | 32.4 | 22.9 | 31.8 | 52.3 | |||||
| Income | |||||||||
| Refused | 11.3 | 13.7 | 10.2 | 7.7 | |||||
| < $20,000 | 21.5 | 32.8 | 18.2 | 3.1 | |||||
| $20,000 - $34,999 | 31.0 | 29.0 | 34.1 | 30.8 | |||||
| $35,000 - $74,999 | 26.4 | 18.3 | 25.0 | 44.6 | |||||
| $75,000 and above | 9.9 | 6.1 | 12.5 | 13.8 | |||||
| nSES | −0.3 | 0.1 | −1.0 | 0.0 | −0.2 | 0.0 | 1.0 | 0.1 | |
| PH-QOL post-stroke | |||||||||
| 6–12 months | 39.9 | 0.6 | 38.6 | 0.9 | 38.6 | 1.1 | 44.3 | 1.3 | |
| 18 months | 39.9 | 0.8 | 37.7 | 1.2 | 39.3 | 1.3 | 45.3 | 1.6 | |
| 27 months | 40.6 | 0.8 | 39.5 | 1.3 | 39.5 | 1.4 | 44.4 | 1.7 | |
| 36 months | 40.1 | 0.9 | 40.4 | 1.2 | 37.3 | 1.5 | 43.4 | 1.8 | |
Note. CARES = Caring for Adults Recovering from the Effects of Stroke; nSES = neighborhood socioeconomic status; NIHSS = National Institutes of Health Stroke Scale; HS = high school; PH-QOL = physical health-related quality of life;
nSES tertile cut points were generated based on tertiles of nSES for the contiguous United States
Of the 360 participants within the Caring for Adults Recovering from the Effects of Stroke (CARES) project, 55 did not have an adjudicated stroke, 11 participants first observation was beyond 36 months post-stroke, and 10 participants’ stroke event occurred after the follow-up observations.
As shown in Table 2, Model 1, the overall average predicted value of PH-QOL for the study population at six months post-stroke was 40.1, approximately one standard deviation below the mean. When examining the population PH-QOL, it appears as if PH-QOL stays relatively constant over time (β = −0.03, SE = 0.2). With the inclusion of individual-level characteristics in Model 2, we see trajectories of PH-QOL are significantly different by gender and age at the time of stroke. Women have much lower values of PH-QOL at six months post-stroke than men (β = −3.96, SE = 1.33). However, women tend to increase over time (β = 0.12, SE = 0.05) and men decline over time (β = −0.09, SE = 0.03). Additionally, we observe an inverse relationship between stroke severity and PH-QOL. With the addition of nSES in Model 3, we observe that with a one standard deviation increase in nSES there is a 1.79 (SE = 0.71) increase in PH-QOL score, independent of individual-level characteristics. Relationships described in Model 2 persist within Model 3. Within Model 4 there is not a significant interaction between nSES and time, after controlling for all other variables within the model.
Table 2.
Effect estimates of neighborhood socioeconomic status (nSES) on trajectories of physical health-related quality of life following a stroke.
| Model 1a | Model 2b | Model 3c | Model 4d | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | β | SE | β | SE | β | SE | β | SE | |||
| Intercept (6 months PS) | 40.11*** | 0.67 | 47.07*** | 2.19 | 47.57*** | 2.17 | 47.57*** | 2.17 | |||
| Individual Effects | |||||||||||
| Age at strokee | −0.02 | 0.09 | −0.05 | 0.09 | −0.04 | 0.09 | |||||
| Female | −3.96** | 1.33 | −3.82** | 1.31 | −3.84** | 1.32 | |||||
| White | 0.16 | 1.22 | −0.84 | 1.26 | −0.84 | 1.26 | |||||
| Education | |||||||||||
| < HS | 0.09 | 1.91 | 0.48 | 1.89 | −0.49 | 1.89 | |||||
| HS graduate | −2.93 | 1.51 | −2.67 | 1.49 | −2.67 | 1.49 | |||||
| Some college | −1.33 | 1.43 | −1.11 | 1.41 | −1.11 | 1.41 | |||||
| College graduate + | − | − | − | − | − | − | |||||
| Income | |||||||||||
| Refused | −3.16 | 2.43 | −2.48 | 2.41 | −2.49 | 2.41 | |||||
| < $20,000 | −4.56* | 2.30 | −3.72 | 2.30 | −3.72 | 2.30 | |||||
| $20,000 - $34,999 | −2.50 | 2.02 | −2.06 | 2.00 | −2.06 | 2.00 | |||||
| $35,000 - $74,999 | −2.70 | 1.98 | −2.84 | 1.95 | −2.84 | 1.95 | |||||
| $75,000 and above | − | − | − | − | − | − | |||||
| NIHSS | −0.61*** | 0.17 | −0.62*** | 0.17 | −0.62*** | 0.17 | |||||
| Neighborhood Effects | |||||||||||
| nSES | 1.79* | 0.71 | 1.73* | 0.80 | |||||||
| Time (months PS) | |||||||||||
| Time (months)f | −0.03 | 0.2 | −0.09** | 0.03 | −0.09** | 0.03 | −0.09** | 0.03 | |||
| Female × Time | 0.12* | 0.05 | 0.11* | 0.05 | 0.12* | 0.05 | |||||
| Age × Time | −0.01** | 0.00 | −0.01* | 0.00 | −0.01* | 0.00 | |||||
| nSES × Time | 0.00 | 0.03 | |||||||||
p < .05;
p < .01;
p < .001
Note. PS = post-stroke; NIHSS = National Institutes of Health Stroke Scale; HS = high school; nSES = neighborhood socioeconomic status
Model 1 estimates the grand mean of physical quality of life among participants, after accounting for the random effect of the intercept
Model 2 estimates the effects of individual characteristics on the intercept and the slope of physical quality of life post-stroke
Model 3 estimates the effects of individual characteristics on the slope and intercept of physical quality of life, and effects of neighborhood socioeconomic status on the intercept of physical quality of life post-stroke
Model 4 estimates the effects of individual characteristics, neighborhood socioeconomic status, and the effects of these parameters on the intercept and the slope of physical quality of life post-stroke
Age centered at 75 years of age
Time measured as months since stroke occurrence
DISCUSSION
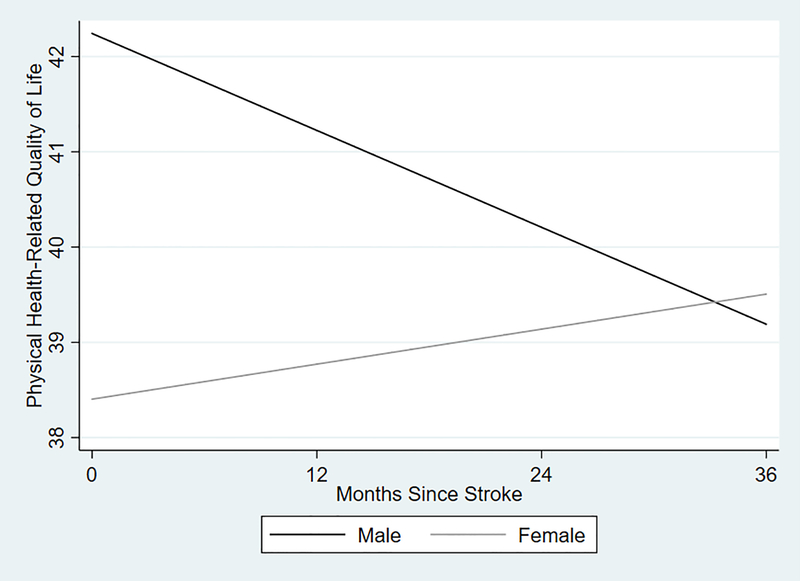
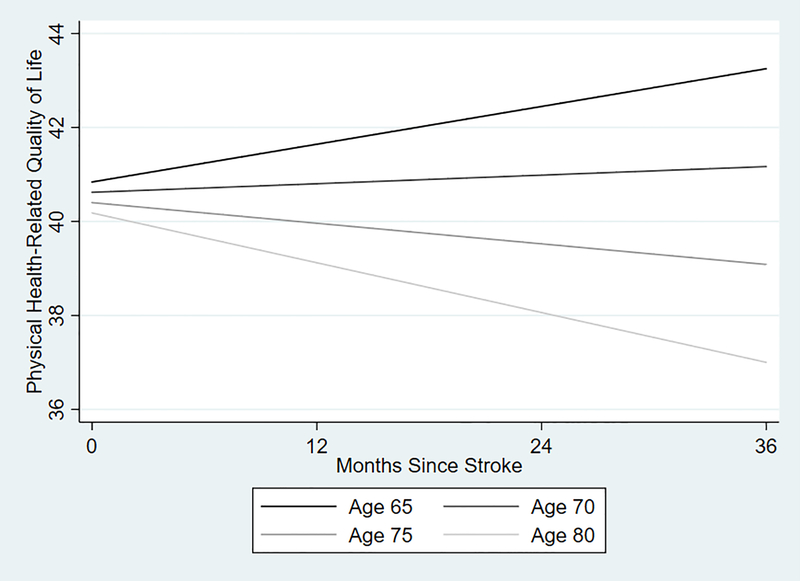
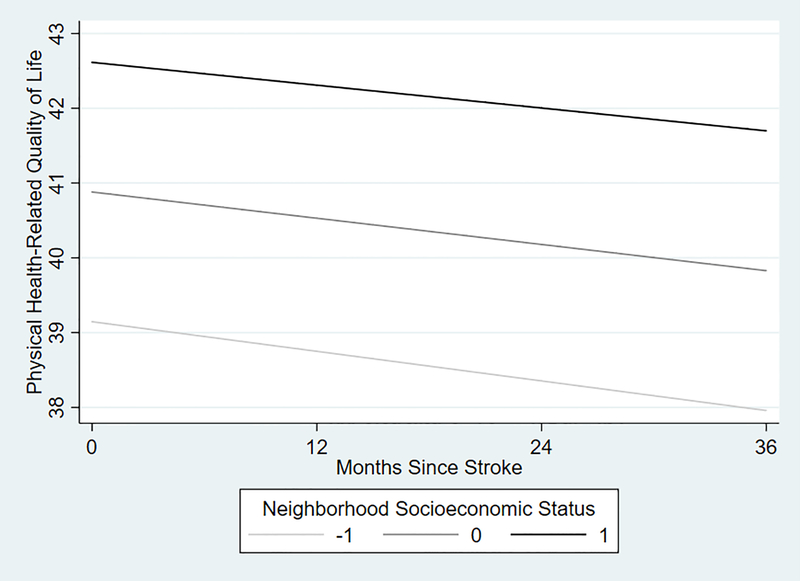
There is minimal research on the role of neighborhood context on post-stroke outcomes. Our results feature the neighborhood context, an important and often overlooked component of the stroke recovery process. Our goal was to examine trajectories of PH-QOL and determine if socio-environmental characteristics shape PH-QOL trajectories. The results provided descriptive evidence of the long-term post-stroke PH-QOL recovery process. When examining the overall average PH-QOL among participants post-stroke, it appears there is no change in population recovery over time. However, the population average trajectory masked changes in PH-QOL over time by different subgroups. We observed drastic differences in observed PH-QOL recovery for women and men and for people who have their stroke at younger ages in comparison to older ages. While estimates for one month appear small, when examined over the entire study period the changes in PCS are similar in magnitude to what others have described as clinically meaningful.27 For example, the intercept for men is 3.6 units higher than the intercept for women; however, over a three year period men decrease by 3.24 units (−0.09*36), whereas women improve by 1.08 units ((−0.09+0.12)*36). Therefore, the average group trajectory among women surpassed the average group trajectory among men over the study period (Figure 1). Younger stroke survivors had trajectories suggesting improvement over time, contrasted with decline over time in older stroke survivors (Figure 2). We found nSES was significantly associated with PH-QOL as a main effect, with stroke survivors living in high nSES showing better function at all time points, but these results show no interaction with time. Those living in more advantaged neighborhoods had higher levels of PH-QOL post-stroke, independent of individual functioning, individual socioeconomic status, and demographic characteristics.
Figure 1.
Predicted trajectories of post-stroke physical health-related quality of life from the SF-12 among men and women over time, as shown in Table 2, Model 4, setting all other variables within the model at their average value.
Figure 2.
Predicted trajectories of post-stroke physical health-related quality of life from the SF-12 among participants with varying levels of age at time of stroke, as shown in Table 2, Model 4, holding all other variables within the model at their average value.
This was one of few studies to describe trajectories of quality of life beyond one-year post-stroke.28, 29 We found that recovery post-stroke overall was quite flat, but uncovered that these trajectories varied by socio-demographic characteristics. Our findings confirm previous work reporting lower levels of quality of life 6–12 months post-stroke among women in comparison to men, after accounting for age differences.13, 30, 31 The underpinnings of our observed differences in trajectories of PH-QOL between women and men are not clear. Future research should explore if these effects are the result of differing social networks among women and men during long-term stroke recovery. We also observed differences in recovery post-stroke by age at the time of stroke. It is possible that these differing trajectories are due to differences in physiologic reserve among older adults and differing vulnerability when responding to a stroke event.32
Environmental attributes have been shown to influence the disabling process.33 Within this study we observed nSES was positively associated with PH-QOL. A one standard deviation increase in nSES resulted in a 1.79 unit increase in PH-QOL, above and beyond individual-level characteristics (Figure 3), a result that was maintained at three years post-stroke. In comparison, a one standard deviation increase in nSES is similar in magnitude to the protective effects of decreasing the age at stroke by 36 years. This supports previous work which has found nSES to be an independent predictor of post-stroke mortality, above and beyond individual characteristics.34 However, we did not observe a statistical interaction between stroke severity and time on PH-QOL outcomes, as hypothesized (Table 2, Model 4). This may be explained by nSES serving as a proxy measure of important underlying neighborhood characteristics, which could drive an interaction. Given high-quality care varies by neighborhood context, it is possible that access to high-quality care is the mechanism through which nSES shifted our population intercept, but not population trajectories.35 Future research should examine the specific components of neighborhood environments and if specific features (e.g. social support, built environment, high-quality care) contribute to differing recovery post-stroke.
Figure 3.
Predicted trajectories of post-stroke physical health-related quality of life from the SF-12 among participants living in low socioeconomic neighborhoods, medium socioeconomic neighborhood, and high socioeconomic neighborhoods based off United States standardized cut-points, as shown in Table 2, Model 4, holding all other variables within the model at their average value.
This study had a number of strengths in its design and analytic approach. Within the REGARDS study there is a rigorous stroke identification process with medical chart review. The CARES study includes a population-based sample that is culturally and geographically diverse. In addition, our sample was made up of community-dwelling stroke survivors who would be the most likely to be impacted by the surrounding outdoor environment. Lastly, given the longitudinal data collection, we were able to estimate long-term trajectory of recovery post-stroke. However, our study does have notable limitations. This study population excludes individuals who died or were placed in a nursing home and is likely to be a healthier sub-sample of stroke survivors within the overall REGARDS cohort. Given PH-QOL is self-reported by the stroke survivors there is a potential for bias in our outcome ascertainment, including differential item functioning by nSES group. A substantial proportion of participants (17%) were missing the NIHSS. There are also potential factors that were not included in this analysis that may serve as confounders of the relationship between nSES and PH-QOL. nSES is a proxy measure for more specific features within the environment. Important components of the neighborhood context were not captured within this study (e.g. social support, built environment, high-quality care). The composite nSES may conceal true relationships between components of neighborhood and trajectories of PH-QOL over time. Additional research is needed to understand the role specific components of the neighborhood context have on the post-stroke recovery process.
CONCLUSIONS
This study found age and gender were significantly associated with trajectories of PH-QOL, where women and younger-aged stroke survivors fared better over time than men and older-aged stroke survivors. On average, participants living in more advantaged neighborhoods had higher levels of quality of life post-stroke, independent of individual functioning, individual socioeconomic status, and demographic characteristics. There is a pressing need to have a greater understanding of the environment’s role in long-term post-stroke participation and quality of life. Studies exploring the specific components of advantaged neighborhoods that are beneficial for post-stroke health are needed to inform effective environmental interventions.
ACKNOWLEDGMENTS
None
SOURCES OF FUNDING
This research project is supported by cooperative agreement U01 NS041588 co-funded by the National Institute of Neurological Disorders and Stroke (NINDS) and the National Institute on Aging (NIA), National Institutes of Health, Department of Health and Human Service. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NINDS or the NIA. The authors thank the other investigators, the staff, and the participants of the REGARDS study for their valuable contributions. A full list of participating REGARDS investigators and institutions can be found at http://www.regardsstudy.org. Additional funding was provided by investigator-initiated grants (R01 NS092706, Natalie Colabianchi and Suzanne Judd, MPIs and R01 NS075047, David Roth, PI). Representatives from NINDS did not have any role in the design and conduct of the study, the collection, management, analysis, and interpretation of the data, or the preparation or approval of the manuscript. Research reported in this publication was also supported by the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health under award number F31 HD098870.
Footnotes
CONFLICT-OF-INTREST/DISCLOSURE
Disclosures: None
REFERENCES
- 1.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. ; Heart disease and stroke statistics-2016 update: A report from the american heart association. Circulation. 2016;133:e38–360 [DOI] [PubMed] [Google Scholar]
- 2.Center for Disease Control and Prevention. Prevalence and most common causes of disability among adults: United states, 2005. MMWR Morb Mortal Wkly Rep. 2009;58:421–426 [PubMed] [Google Scholar]
- 3.Haley WE, Roth DL, Kissela B, Perkins M, Howard G. Quality of life after stroke: A prospective longitudinal study. Qual Life Res. 2011;20:799–806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.King RB. Quality of life after stroke. Stroke. 1996;27:1467–1472 [DOI] [PubMed] [Google Scholar]
- 5.Clarke P, Marshall V, Black SE, Colantonio A. Well-being after stroke in canadian seniors: Findings from the canadian study of health and aging. Stroke. 2002;33:1016–1021 [DOI] [PubMed] [Google Scholar]
- 6.Pan JH, Song XY, Lee SY, Kwok T. Longitudinal analysis of quality of life for stroke survivors using latent curve models. Stroke. 2008;39:2795–2802 [DOI] [PubMed] [Google Scholar]
- 7.Kissela B The value of quality of life research in stroke. Stroke. 2006;37:1958–1959 [DOI] [PubMed] [Google Scholar]
- 8.Bukan RI, Moller AM, Henning MA, Mortensen KB, Klausen TW, Waldau T. Preadmission quality of life can predict mortality in intensive care unit--a prospective cohort study. Journal of Critical Care. 2014;29:942–947 [DOI] [PubMed] [Google Scholar]
- 9.Clarke PL, Lawrence JM, Black SE. Changes in quality of life over the first year after stroke: Findings from the sunnybrook stroke study. Journal of Stroke and Cerebrovascular Diseases. 2000;9:121–127 [DOI] [PubMed] [Google Scholar]
- 10.Glass T, Matchar DB, Belyea M, Feussner JR. Impact of social support on outcome in first stroke. Stroke. 1993;24:64–70 [DOI] [PubMed] [Google Scholar]
- 11.Pearlin LI. The sociological study of stress. Journal of Health and Social Behavior. 1989;30:241–256 [PubMed] [Google Scholar]
- 12.Robert Wood Johnson Foundation. County health rankings & roadmaps: Building a cluture of health, county by county. 2016
- 13.Bushnell CD, Reeves MJ, Zhao X, Pan W, Prvu-Bettger J, Zimmer L, et al. Sex differences in quality of life after ischemic stroke. Neurology. 2014;82:922–931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pucciarelli G, Lee CS, Lyons KS, Simeone S, Alvaro R, Vellone E. Quality of life trajectories among stroke survivors and the related changes in caregiver outcomes: A growth mixture study. Arch Phys Med Rehabil. 2019;100:433–440.e431 [DOI] [PubMed] [Google Scholar]
- 15.Elfassy T, Grasset L, Glymour MM, Swift S, Zhang L, Howard G, et al. Sociodemographic disparities in long-term mortality among stroke survivors in the united states. Stroke. 2019;50:805–812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Howard VJ, Cushman M, Pulley L, Gomez CR, Go RC, Prineas RJ, et al. The reasons for geographic and racial differences in stroke study: Objectives and design. Neuroepidemiology. 2005;25:135–143 [DOI] [PubMed] [Google Scholar]
- 17.Haley WE, Allen JY, Grant JS, Clay OJ, Perkins M, Roth DL. Problems and benefits reported by stroke family caregivers: Results from a prospective epidemiological study. Stroke. 2009;40:2129–2133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Roth DL, Haley WE, Clay OJ, Perkins M, Grant JS, Rhodes JD, et al. Race and gender differences in 1-year outcomes for community-dwelling stroke survivors with family caregivers. Stroke. 2011;42:626–631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Diez Roux AV, Kiefe CI, Jacobs DR, Haan M, Jackson SA, Nieto FJ, et al. Area characteristics and individual-level socioeconomic position indicators in three population-based epidemiologic studies. Ann Epidemiol. 2001;11:395–405 [DOI] [PubMed] [Google Scholar]
- 20.Diez Roux AV, Merkin SS, Arnett D, Chambless L, Massing M, Nieto J, et al. Neighborhood of residence and incidence of coronary heart disease. N Engl J Med. 2001;345:99–106 [DOI] [PubMed] [Google Scholar]
- 21.Ware J, Kosinski M, Keller SD. A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Medical Care. 1996;34:220–233 [DOI] [PubMed] [Google Scholar]
- 22.Brott T, Adams HP, Olinger CP, Marler JR, Barsan WG, Biller J, et al. Measurements of acute cerebral infarction: A clinical examination scale. Stroke. 1989;20:864–870 [DOI] [PubMed] [Google Scholar]
- 23.Rubin DB. Multiple Imputation for Nonresponse in Surveys. Vol. 81 John Wiley & Sons; 2004. [Google Scholar]
- 24.Royston P Multiple imputation of missing values. Stata Journal. 2004;4:227–241 [Google Scholar]
- 25.Diez Roux AV, Mair C. Neighborhoods and health. Annals of the New York Academy of Sciences. 2010;1186:125–145 [DOI] [PubMed] [Google Scholar]
- 26.Raftery AE. Bayesian model selection in social research. Sociological Methodology. 1995:111–163 [Google Scholar]
- 27.Lim LY, Fisher JD. Use of the 12-item short-form (sf-12) health survey in an australian heart and stroke population. Quality of Life Research. 1999;8:1–8 [DOI] [PubMed] [Google Scholar]
- 28.De Wit L, Theuns P, Dejaeger E, Devos S, Gantenbein AR, Kerckhofs E, et al. Long-term impact of stroke on patients’ health-related quality of life. Disabil Rehabil. 2017;39:1435–1440 [DOI] [PubMed] [Google Scholar]
- 29.Leach MJ, Gall SL, Dewey HM, Macdonell RA, Thrift AG. Factors associated with quality of life in 7-year survivors of stroke. J Neurol Neurosurg Psychiatry. 2011;82:1365–1371 [DOI] [PubMed] [Google Scholar]
- 30.Gargano JW, Reeves MJ. Sex differences in stroke recovery and stroke-specific quality of life: Results from a statewide stroke registry. Stroke. 2007;38:2541–2548 [DOI] [PubMed] [Google Scholar]
- 31.Gall S, Phan H, Madsen TE, Reeves M, Rist P, Jimenez M, et al. Focused update of sex differences in patient reported outcome measures after stroke. Stroke. 2018;49:531–535 [DOI] [PubMed] [Google Scholar]
- 32.Cai W, Zhang K, Li P, Zhu L, Xu J, Yang B, et al. Dysfunction of the neurovascular unit in ischemic stroke and neurodegenerative diseases: An aging effect. Ageing Research Reviews. 2017;34:77–87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Clarke P, Ailshire JA, Bader M, Morenoff JD, House JS. Mobility disability and the urban built environment. Am J Epidemiol. 2008;168:506–513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Brown AF, Liang LJ, Vassar SD, Merkin SS, Longstreth WT, Ovbiagele B, et al. Neighborhood socioeconomic disadvantage and mortality after stroke. Neurology. 2013;80:520–527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Baicker K, Chandra A, Skinner J. Geographic variation in health care and the problem of measuring racial disparities. Perspectives in Biology and Medicine. 2005;48:42–S53 [PubMed] [Google Scholar]