Over the past decade, the interest in pursuing nephrology training has declined dramatically, particularly among United States medical school graduates. According to a 2018 report from the Association of American Medical Colleges Center for Workforce Studies, only 20% of nephrology fellows were United States medical school graduates.S1 As a result, nephrology programs are struggling to fill their positions. In 2018, only 325 prospective applicants applied for the available 464 nephrology positions within the 92 Accreditation Council for Graduate Medical Education accredited fellowships, resulting in 56% of slots remaining unfilled.S2 The declining interest in nephrology as a subspecialty is more significant in view of the increasing prevalence of chronic kidney disease and end-stage kidney disease in the United States.S3 The growing concern related to a potential shortfall in the nephrology workforce has even led the renal community to question the future of the specialty and its ability to address the needs of a growing chronic kidney disease population.1
In response to this crisis, the American Society of Nephrology, in collaboration with the George Washington University Health Workforce Institute, created a task force in 2010 charged with increasing interest in nephrology careers. Toward that goal, the task force created multiple initiatives, including analyses of the current job market and factors influencing interest in the specialty. The findings of the task force highlighted the limited opportunities offered by the job market and provided invaluable data about the perception of the specialty from the viewpoints of nephrology fellows, current clinical practitioners, and representatives of large dialysis organizations.2 However, the task force focused primarily on nephrology physicians/trainees, without extending its research to include internal medicine residents. The attitudes and opinions of medicine residents are of particular interest because these trainees constitute the main pipeline for the specialty. Additionally, among the few studies considering perceptions among this group, only one used focus groups to inform the survey questions.3 The remainder obtained data from questionnaires designed by the investigators without input from residents.4, 5, 6 None of the studies were grounded in a theoretical framework, which is a synthesis of guiding concepts and theories that justify a research question. This lack of grounding is of particular importance because frameworks are critical to substantiate the importance and significance of the work.S4
Our study aimed to identify factors that influence internal medicine residents’ decisions to pursue specialty training, focusing specifically on residents’ perceptions of nephrology. To achieve this goal, our study predominantly utilized “how” and “why” questions, to capture thematic responses of the participants without constraining their responses to choices predetermined by the survey design.
Results
We used a qualitative design consisting of semi-structured interviews in order to obtain the data. Our analysis was guided by the content analysis approach,S5 and the choice of interview questions was guided by the Professional Identify Formation framework.S6 A sample of the questions that were posed to residents can be found in Table 1. Please refer to the Supplementary Methods section for additional details.S7–S9
Table 1.
Interview guide with a sample of the questions that were posed to residents
| Interview topic | Question | Possible follow-up question |
|---|---|---|
| Existing personal identity | Tell me about yourself | Any family members in the medical field? |
| Why did you decide on internal medicine? | Did anyone play a role in your decision? | |
| Previous experiences | What were your favorite and least favorite rotations? | Why? |
| What did you like/dislike about your rotation? | Why? | |
| Formal learning | How do you describe your experience in medical school? | What were your favorite/least favorite topics? Why? |
| How do you describe your nephrology experience? | Was nephrology hard? Was it taught well? | |
| Career choice | What are the factors that encouraged you in pursuing a specialty? | Which specialty do you plan on pursuing? When did you make that choice? Why? |
| What do you find attractive or unattractive about nephrology? | Can you give an example? |
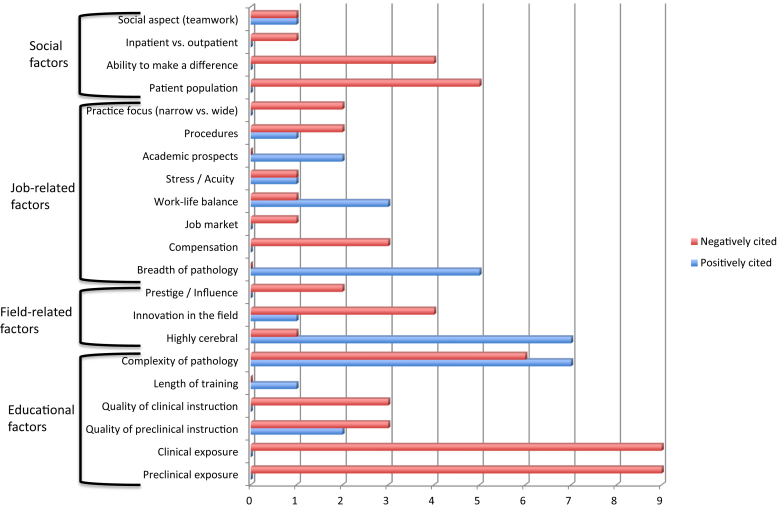
Ten residents were interviewed. Five were males, and 8 were graduates of American medical schools. Six were in postgraduate year 1, and 4 were in postgraduate year 2 (Table 2). In order to identify general factors influencing career decision-making, we inquired about the reasons that inspired the residents to pursue a career in medicine, and then we sorted our findings into 3 broad categories: personal attributes, social factors, and specialty-specific factors. Personal attributes included factors such as family influence and personal preference, and social factors grouped transformative experiences, role of mentors, and educational experiences. Specialty-specific factors revolved around factors specific to the specialty field, the nature of the job, the lifestyle, and patient characteristics, as detailed in Table 3. We focused particularly on the factors affecting the field of nephrology, and we provide those results in Figure 1. In the following paragraphs, we use verbatim quotes from the interviews in order to explain the process with more clarity.
Table 2.
Demographic characteristics of the study participants
| Student # | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| Age (yr; average: 30.5) | 32 | 34 | 31 | 28 | 33 | 28 | 30 | 35 | 26 | 28 |
| Gender | M | F | F | F | M | M | F | M | M | F |
| School | AMG | AMG | AMG | IMG | AMG | AMG | AMG | AMG | IMG | AMG |
| PGY | 1 | 2 | 1 | 1 | 1 | 1 | 2 | 2 | 1 | 2 |
AMG, American medical school graduate; F, female; IMG, international medical school graduate; M, male; PGY, postgraduate year.
Table 3.
General (nephrology-independent) factors influencing career decision-making
| Personal attributes | Social factors | Subspecialty-specific factors |
|---|---|---|
| Personal preference | Role models/mentors | Field-related factors
|
| Family influence | Transformative events | Lifestyle-related factors
|
| Experiences | Formal learning (preclinical)
|
Job-related factors
|
| Values | Clinical years
|
Patient-related factors
|
Figure 1.
Factors specifically affecting the field of nephrology. The numbers indicate the number of residents citing the specific factor.
Factors Specifically Affecting the Field of Nephrology
Lack of exposure to nephrology, in both the clinical and preclinical years, appeared to be the most important negative factor as it was cited by 9 out of 10 residents (Figure 1).
#3 “I shadowed nephrology for a day, but I did not rotate through. It was not a part of the medical school curriculum.”
#5 “At our school when I went to the basic sciences, we didn't have nephrology as a course. It was kind of spread throughout all the classes and it kind of varied and so I would say most of it was taught within our pathology course or histology course.”
Lack of innovation in the field of nephrology appeared to be another major deterring factor (cited by 4 of 10 residents). Another factor accounting for the negative perception was the patient population, notably the chronicity of dialysis patients (cited by 5 of 10 residents):
#8 [What I dislike about nephrology is] the stigma regarding dialysis and the difficulty in some of the patients to be compliant even though you know what the outcome is going to be. Young people with ridiculously high blood pressure, trying to get them to take their medications. That would be frustrating.
#6 What I don't like about it is . . . a lot of your patients are undergoing dialysis and are just there kind of living their life on dialysis. You're not really doing much for them. You're just basically acting as their kidneys every other day.
#9 the negative thing was . . . that the medicine of nephrology is not veering towards something new. It has been stale for a while.
On the other hand, nephrology was viewed positively as a “smart” or “brainy” specialty. The breadth of pathology was also often viewed as an encouraging factor, steering physicians away from the routine of daily practice. Interestingly, the complexity of the field was mentioned as both a negative and a positive factor by the residents, often by the same resident at different points during the interview.
#1 It takes a lot of diagnostic skills. . . . I think that is a very cerebral specialty where you have a lot of personal diagnostic skills involved.”
General (Nephrology-Independent) Factors Influencing Career Decision-Making
We asked the residents about the factors that inspired them to pursue a career in medicine, and we grouped them into 3 broad categories: personal attributes, social factors, and specialty-related factors. Each category was further divided into several subcategories, detailed in Table 3.
Personal Attributes
Personal attributes are determined by personal characteristics, self-chosen or mandated commitments, beliefs about one’s self, and the impact of multiple life experiences.S6 They were categorized into personal preference, family influence such as the presence of a physician in the family, personal experiences, and values. Some examples are as follows:
#2 I was an animal science major . . . I have a Ph.D. in Molecular Medicine . . .. I was never really happy with a life of research . . ... You don't get that satisfaction of the interpersonal, you know. I'm really more of like, I like to talk to people, I like to spend time with people, learn their stories. I like to do all those things and you don't get to do anything of that when you are standing at a lab bench [personal preference].
#5 The job I had there was mostly sitting in a cubicle, typing on a computer all day. It wasn't very social and some people like really thrive in that, but after about a year I was like this has been very low stress, very enjoyable but I think I still want to do medicine as a career [personal preference].
#2 I went [to medicine] because I was really interested in helping people [values].
#10 “I knew I wanted to do something in terms of helping others . . .. I saw the physician-patient relationship is where my initial interest in medicine started [values].
#2 My mom's a nurse practitioner and I went on a couple of international medical missions with her[family influence and personal experiences].
#5 My parents are both in the medical field. Neither of them are physicians. My mom is a nurse and has been one for a very long time. My dad is you can call it a biomedical technician. He repairs x-ray equipment [family influence].
Social Factors
These factors revolved around the influences of mentors or role models, the exposure to transformative events such as a memorable patient encounter, and education received in the clinical and preclinical years.
#2 So, I'm with this woman and my very first patient that I saw with her. We walked into the ICU and this patient is on a vent and was totally out, but the whole family is there. So, she walks in and grabs this patient's hand and she goes Hi, my name is Dr. X. It is Thursday and 3:30 p.m. and I want you to know that you're safe . . .…. The whole family just started to cry. Like, they just started balling. They were like nobody has acknowledged that he is a person here for the entirety of the time that he has been here and like, I was crying . . .. She made a huge difference in those peoples' lives [transformative experience and mentor/role model influence].
#10 “I . . .shadowed] a pulmonologist in the ICU . . .. I thought she was phenomenal with patients. I went to lots of end-of-life conversations, but it was my first time ever being in one of those and it was very overwhelming, but I remember seeing how she would act [role model].
#8 As a first-year med student I was able to close up a right atrium in a 3-month-old and as a first-year med student I was sewing up saphenous vein harvest sites and when they actually ran out of residents in the surgery program, they let me be 1st assist through an entire bypass operation, I was the only person in there, well with the main surgeon as well [autonomy].
#3 I think the favorite was my subinternship in Internal Medicine, being able to be hands-on, being able to really make some key medical decisions. . .. It was just me and the staff on my rotation. I thought there is a lot of education and I made an independent decision [autonomy].
#2 They put me on gen. surg. and you just get yelled at a lot and nobody was really teaching me. It was in a particularly malignant surgical program and so the residents were crawling over each other to do procedures and nobody was interested in helping me” [environment].
#5 My least favorite (rotation) was neurology. I was not super good at doing oral presentations yet. I was not super good about figuring out how to do a thorough morning chart review. So, no matter how I hard I worked, I felt like I wasn't doing a very good job [performance].
Specialty-Specific Factors
These factors revolved around the particularities of the different specialties, notably in what makes a career choice more or less attractive. Specialty-specific factors were further divided into field, lifestyle, job, and patient-related factors (Table 3).
Discussion
Our study highlights residents’ perception of the field of nephrology and emphasizes specifically the lack of exposure to nephrology as one of the major challenges facing the specialty. It also recognizes the key influence of mentorship and role models on the choice of a career path.
Although the literature on career choice is abundant, only a few studies focus specifically on nephrology. Those report a wide variety of factors influencing the choice to pursue a nephrology career, such as lack of interest in the subject, difficulty of the subject, a perception that earning potential is limited, patient non-adherence, concern for work–life balance, and few opportunities to perform procedures.3, 5, 6 However, most of those studies were survey-based, which means that subjects were surveyed on factors thought to be important by the authors. Our study is the first of its kind as it discusses residents’ perception of nephrology in an open-ended fashion. As a result, it is the first to highlight the lack of exposure to nephrology as a key deterrent to pursuit of the specialty. Parker et al.1 alluded to this postulation, although they did not have evidence to demonstrate it. Interestingly, this finding was reported in geriatrics. Blachman et al.7 conducted a qualitative study of geriatric fellows and showed that early exposure to geriatrics was the most influential career-affecting factor. Exposure to the specialty of interest was also recognized in the rheumatology literature8 and the surgical literature, the latter emphasizing specifically that early exposure increased students’ interest.9 We believe the most important finding in our study is the identification of reduced nephrology exposure as a major factor in reducing interest in nephrology as a career choice. We are perplexed by the reports indicating that nephrology is not a fundamental part of educational curricula, given the fundamental role of the kidney in volume homeostasis and metabolism. However, our findings offer an opportunity for the nephrology community to increase its involvement in education, both in medical school and residency. Interventions should target trainees in the early stages of their training.
The perceived renal patient population is another factor that negatively impacts residents, a finding that has also been reported in other studies.6 Unfortunately, internal medicine residency programs (IMRPs) are hospital-based, and most residents are exposed to very sick and noncompliant end-stage kidney disease patients who tend to have a >30% risk of 30-day readmission. Residents in internal medicine lack exposure to high-functioning end-stage kidney disease patients in the ambulatory setting. Our study did not find compensation levels or work–life balance to be important contributors to interest in nephrology among our survey participants, similar to findings from a study from the United Kingdom, where “future financial prospects” were noted to be “unimportant influences.”4 These results are contrary to other reports in the literature that identified financial and lifestyle considerations as key factors.5 Additionally, the American Society of Nephrology task force reports that approximately 24% of early career nephrologists are dissatisfied with their pay.2
In regard to the factors influencing the choice of a career in general, our findings are concordant with the literature, in that this choice stems from an array of personal attributes and social factors.S6 We highlight in particular the role of mentorship and role models, as well as the impact of transformative experiences, all which were previously identified as key elements.S10,S11 We also note the family’s influence on the decision to pursue medicine, as well as the altruistic desire to help people and make a difference, which is in line with what is known on the topic.S12,S13 Understanding those factors and adapting those themes into interventions can help generate transformational educational experiences, which in turn can lead to increased resident interest in nephrology.
Our study has several limitations. First, we acknowledge that a qualitative design limits generalizability, as it is not intended to show statistical significance. However, the aim of a qualitative study is not to test a hypothesis but rather to provide a detailed description of a phenomenon in order to build a theory. Second, we recognize that we selected residents from a single, large medical center (Cleveland Clinic Foundation Internal Medicine Residency Program, Cleveland, OH). Therefore, it is possible that participants’ responses may have been biased by the strength of a particular influence that is prominent in such a center but is not as important in a smaller community-based program. However, as the study was qualitative and intended to reveal perceptions of nephrology, our sampling was aimed not at population representation but at supporting theme identification and framework construction. Additionally, the veracity of the results was ensured through a rigorous scientific analysis using the well documented methodology of qualitative content analysis.S5 Finally, we realize that the residents participating in the interviews had already determined not to pursue a nephrology fellowship. Although we feel that we reached data adequacy for our defined aim, we recognize that residents interested in pursuing a nephrology fellowship might be driven by different factors, and this possibility needs to be addressed in future studies.
Conclusion
In sum, our study describes the perception of internal medicine residents regarding the field of nephrology. In particular, it highlights the lack of exposure to nephrology as a key deterrent to pursuit of a nephrology career. We believe our findings contribute to the literature because they suggest that the nephrology community must increase its involvement in resident education. We plan to use our findings to inform the construction of a survey that can be applied at a national level. Our experience using the Professional Identify Formation framework was helpful and offered insight and solid guidance in the interview process. Future studies should consider interviewing residents planning to pursue nephrology in order to identify the positive factors fostering this decision. Additionally, investigations are needed to develop improved recruitment strategies that will help sustain the future of the specialty.
Disclosure
All the authors declared no competing interests.
Acknowledgments
The William and Sandra Bennett Clinical Scholar Programs Educational Grant of the American Society of Nephrology supported this work (grant number ASN1805GN).
Footnotes
Supplementary Material
References
- 1.Parker M.G., Ibrahim T., Shaffer R. The future nephrology work force: will there be one? Clin J Am Soc Nephrol. 2011;6:1501–1506. doi: 10.2215/CJN.01290211. [DOI] [PubMed] [Google Scholar]
- 2.Quigley L., Salsberg E., Collins A. American Society of Nephrology; Washington, DC: 2018. Report on the 2018 Survey of Nephrology Fellows. [Google Scholar]
- 3.Nair D., Pivert K.A., Baudy A., 4th, Thakar C.V. Perceptions of nephrology among medical students internal medicine residents: a national survey among institutions with nephrology exposure. BMC Nephrol. 2019;20:146. doi: 10.1186/s12882-019-1289-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barat A., Goldacre M.J., Lambert T.W. Career choices for nephrology and factors influencing them: surveys of UK medical graduates. RSM Open. 2018;9 doi: 10.1177/2054270418793024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Daniels M.N., Maynard S., Porter J. Career interest and perceptions of nephrology: a repeated cross sectional survey of internal medicine residents. PLoS One. 2017;12 doi: 10.1371/journal.pone.0172167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jhaveri K.D., Sparks M.A., Shah H.H. Why not nephrology? A survey of US internal medicine subspecialty fellows. Am J Kidney Dis. 2013;61:540–546. doi: 10.1053/j.ajkd.2012.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blachman NL, Blaum CS, Zabar S. Reasons geriatrics fellows choose geriatrics as a career, and implications for workforce recruitement [e-pub ahead of print]. Gerontol Geriatr Educ. 10.1080/02701960.2019.1604341. Accessed September 12, 2019. [DOI] [PubMed]
- 8.Kolasinski S.L., Bass A.R., Kane-Wanger G.F. Subspecialty choice: Why did you become a rheumatologist? Arthritis Rheum. 2007;57:1546–1551. doi: 10.1002/art.23100. [DOI] [PubMed] [Google Scholar]
- 9.Schmidt L.E., Cooper C.A., Guo W.A. Factors influencing US medical students' decision to pursue surgery. J Surg Res. 2016;203:64–74. doi: 10.1016/j.jss.2016.03.054. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.