Abstract
Introduction:
The purpose of this study is to reconcile public health workforce supply and demand data to understand whether the expected influx of public health graduates can meet turnover events.
Methods:
Four large public health workforce data sources were analyzed to establish measures of workforce demand, voluntary separations, and workforce employees likely to retire at state and local health departments. Data were collected in 2014–2016 and analyzed in 2016 and 2017. Potential workforce supply (i.e., candidates with formal public health training) was assessed by analyzing data on public health graduates. Supply and demand data were reconciled to identify potential gaps in the public health workforce.
Results:
At the state and local level, ≅197,000 staff are employed in health departments. This is down more than 50,000 from 2008. In total, ≥65,000 staff will leave their organizations during fiscal years 2016–2020, with ≤100,000 staff leaving if all planned retirements occur by 2020. During 2000–2015, more than 223,000 people received a formal public health degree at some level. More than 25,000 students will receive a public health degree at some level in each year through 2020.
Conclusions:
Demands for public health staff could possibly be met by the influx of graduates from schools and programs of public health. However, substantial implications exist for transferal of institutional knowledge and ability to recruit and retain the best staff to sufficiently meet demand.
INTRODUCTION
Concerns about worker supply have been at the forefront of public health workforce planning discussions for decades.1–3 Public health has been bracing for the possibility of mass retirements as the workforce ages,4 and the economic recession has had a substantial influence on funding for public health, resulting in the loss of approximately 50,000 state and local public health jobs attributable to layoffs and attrition since 2008.5–7 Although studies report that some job loss associated with budget reductions has stabilized in recent years,8 the governmental public health workforce is still operating at reduced capacity at a time when turnover, recruitment, and retention are challenging across occupations9–11 and service demands are changing with healthcare reform and the growth of Federally Qualified Health Centers and other safety net providers.12–14
Periodic point estimates of public health workforce size and composition have been drawn from multiple sources that represent different study methodologies and varying data quality.15 The most recent estimates enumerating the federal, state, and local public health workforce report a steady drop in overall size from approximately 500,000 (220/100,000 population) in 1980,16 to approximately 448,000 (158/100,000 population) in 2000,17,18 and to 291,000 (93/100,000 population) in 2014.18 Further, the public health system lacks a framework for systematically evaluating the workforce capacity required to ensure effective delivery of essential public health services, making supply needs and demand difficult to project.
Workforce projections rely on the reconciliation of the potential inflows and outflows of workers into a system. For the public sector more broadly, and public health more specifically, this means reconciling the potential supply of new public health workers with the demand generated by those leaving governmental public health. However, limited information is available about voluntary turnover, and even less about eligible, planned, or actual retirements.8,10,19 This study reconciles public health workforce supply and demand data from state and local health departments to understand more fully whether the expected influx of public health graduates could plausibly meet needs generated by retirement and other worker turnover events in these settings.
METHODS
Demand for state and local governmental public health staff was assessed by reconciling data from four sources: Association of State and Territorial Health Officials (ASTHO) and National Association of County and City Health Officials (NACCHO) 2016 profile surveys; 2014 Public Health Workforce Interests and Needs Survey (PH WINS); and the 2016 Workforce Gaps Survey (WGS; Appendix Figure 1, available online). ASTHO and NACCHO profiles are mainstays in public health workforce research.20,21 PH WINS represents the first large-scale, nationally representative survey of the public health workforce with >23,000 respondents.4,22 The WGS included four primary domains: workforce characteristics, retirement, leadership perceptions around workforce gaps, and succession planning. This study draws from the first two WGS domains. Data source methodology has been described elsewhere.11,12,23
ASTHO and NACCHO profiles provided workforce size data. Measures of demand (i.e., positions vacated through retirement and voluntary separation from the public health workforce) were reconciled across the four data sources. Because attrition, where vacancies are left purposefully unoccupied, is a well-known and common means of dealing with budget shortfalls, measures of demand might be reasonably viewed as maximum estimates. The ASTHO profile collects data on retirement eligibility, the NACCHO profile on retirements, PH WINS on intent to leave or retire, and WGS on retirement eligibility, actual retirements, and voluntary separations. The data sources aligned to measure all components for fiscal year (FY) 2015, and certain components for FY2013–2016; local health department (LHD) staff size and full-time employees data were aligned to identify correlation with the size of the population served. Demand was first examined by way of total turnover and was then adjusted to account for the relatively limited number of current state health agency (SHA) positions nationwide that are held by those with public health degrees. Retirement eligibility, planned retirements, and actual retirement data were used to estimate the proportion of the workforce likely to retire by 2020. Intent to leave and actual nonretirement voluntary separations data were used to estimate the proportion of the workforce likely to leave governmental public health. PH WINS data were used to conduct demographic comparisons among staff, new hires, and those with positions designated within the public health sciences (PHS) planning to leave and retire. PHS positions were used as coded by PH WINS, as opposed to clinical or administrative positions.4
Potential workforce supply was defined as the supply of candidates with formal public health training in the U.S., using data from the U.S. National Center for Education Statistics (NCES), which collects graduation, financial, staffing, and enrollment data from >7,400 U.S. colleges and universities, 2,100 of which have awarded graduate degrees or certificates.24 The following NCES Classification of Instructional Program categories were used: public health–related (51.22), epidemiology (26.1309), biostatistics (26.1102), and health policy analysis (44.0503).25 Because the field considers formal public health training as the standard entry degree for new public health staff,26–30 this study considers all public health graduate students and those with public health undergraduate degrees as potential workforce supply for health departments, even if preparing for work in other health sectors.31,32
Demand and supply data were reconciled to identify potential gaps in the public health workforce; to create conservative estimates, the authors anticipated a relatively stagnant-sized workforce for the near future given recent cuts11,21,33 and considered supply scenarios where graduates per year were constant at 2015 levels, and one scenario where growth in the number of degrees awarded per year grew linearly (baseline 2013–2015). Datasets were integrated and managed in Stata, version 13. The Centers for Disease Control and Prevention IRB determined that this study was not human subjects research.
RESULTS
The 2016 NACCHO profile indicates that the LHD workforce is estimated at 147,000 full-time and part-time staff (95% CI=135,000, 159,000), down from 162,000 in 2013 and 190,000 in 2008. Approximately 103,000 of these staff are employed by local governments, 18,000 by state governments, and 26,000 in shared state–local arrangements. At the state level, the ASTHO profile estimates that SHAs employ ≅104,000 staff across the country: 50,000 work in the central office and 54,000 work within local or regional offices, which likely include those reported by NACCHO, employed by state government and in shared state–local arrangements.21
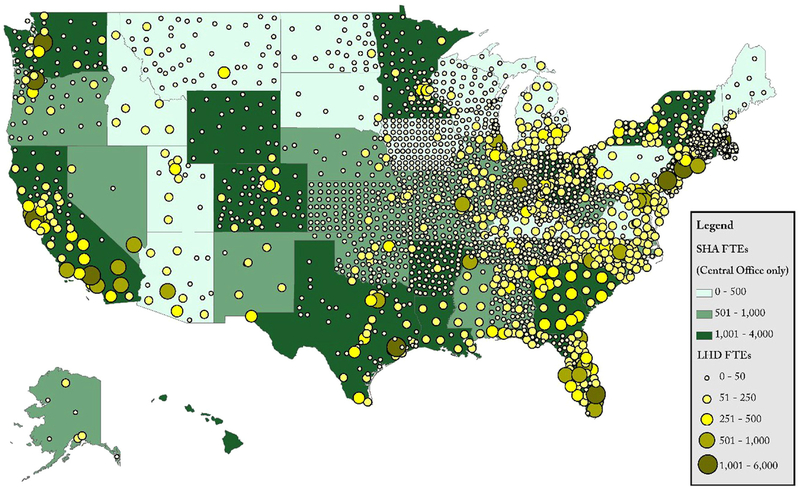
The alignment of NACCHO and ASTHO enumeration data yielded ≅197,000 staff across state health departments and LHDs in 2016. Significant interstate variation was observed (Figure 1), with ≅6% of the LHDs employing 42% of all LHD staff nationwide. When examining full-time employees, ≅80% of LHDs employ ≤50 staff, 17% employ 51–250 staff, and 3% employ >250 staff. LHD total staff size and number of full-time employees were correlated with the size of the population served (r =0.8630 and r =0.8686, respectively; Figure 1).
Figure 1. Size of the governmental public health workforce in state and local departments, 2016.
Note: Hawaii and Rhode Island do not have local health departments (LHDs). Hawaii and Alaska are not pictured to scale. Estimates from LHDs that did not respond to the 2016 Profile were imputed on the basis of previous surveys or jurisdiction size. Data sources: ASTHO 2016 Profile and NACCHO 2016 Profile.
ASTHO, Association of State and Territorial Health Officials; FTE, full time employees; NACCHO, National Association of County and City Health Officials; SHA, state health agency.
Overall, during FY2013–2015, ≅11% of the SHA’s workforce turned over (median 10%, SD 7%). According to PH WINS, ≅24% of SHA staff are = planning to retire by 2020. The average planned age of retirement is 62 or 63 years (Appendix Figure 2, available online). Although variable across SHAs, a mean of 24% of staff were judged retirement-eligible by their SHA in FY2015 (median 18%, SD=17%, range, 5%–83%). During FY2015, ≅6% of PH WINS SHA respondents reported planning to retire that year, and approximately half of those respondents, in aggregate on average (mean 54%, median 50%, SD=25%), followed through with retirement, representing <3% of all PH WINS respondents. Overall, retirements accounted for ≅33% of turnover in a given SHA (median 31%, SD=21%). Although retirement eligibility could not be assessed nationally for LHDs, PH WINS indicated that 4.5% of large LHD staff and 6% of other LHD staff had planned to retire during 2015; however, on average, the NACCHO profile reports that only 3.1% of LHD staff retired during that year. Staff who quit/resign, or otherwise voluntarily leave to pursue other opportunities, constitute the largest driver of turnover. PH WINS indicated that 20% of the SHA workforce was considering leaving their organization during FY2015. However, among 21 SHAs with sufficient data to calculate planned versus actual retirements and voluntary separations, only 52% of the expected nonretirement separations were observed during that period (median 48%, SD=27%; Table 1).
Table 1.
Voluntary Separations at State Health Agencies as a Percent of Those Expecting to Retire and Those Considering Leaving for FY2015
| Descriptive statistics | Separations overall (%) | Retirements (%) | Nonretirements (%) |
|---|---|---|---|
| Average | 50 | 54 | 52 |
| Median | 49 | 50 | 48 |
| SD | 24 | 25 | 27 |
| Min | 8 | 22 | 5 |
| Max | 101 | 121 | 122 |
| na | 27 | 30 | 21 |
Number of states. Estimates were created by capturing actual separations (2016 ASTHO Profile), retirements (2016 Workforce Gaps Study), and intent to leave or retire (2014 PH WINS), and reconciling these estimates for states where all data points were represented.
ASTHO, Association of State and Territorial Health Officials; FY, fiscal year; PH WINS, Public Health Workforce Interests and Needs Survey.
By extrapolating the 24% of PH WINS respondents who indicated they were planning to retire by 2020 to the ≅197,000 state and local public health workforce nationwide, ≅47,000 staff nationally are planning to retire by 2020. However, if the substantial difference between planned versus actual retirements in FY2015 holds, and trends in delayed retirement continue, fewer staff will retire by 2020, perhaps as few as 25,000. In addition, other voluntary (nonretirement) separations are expected. The authors estimate an additional 40,000–50,000 staff will be needed by 2020 to replace the workforce likely to leave governmental public health for nonretirement reasons. In total, this indicates >65,000 staff will leave their organizations in FY2016–2020, with up to 100,000 staff leaving if all planned retirements occur by 2020.
NCES reports that 280 institutions collectively conferred ≅10,900 bachelor’s, 14,000 master’s, and 1,300 doctoral degrees in public health during 2015. During 2000–2015, ≅224,000 public health degrees were awarded in the U.S. (Table 2). Estimates indicate that 37% of doctoral degree recipients have a public health master’s degree and o6% of master’s students have a bachelor’s in public health.32 Considering the proportion of people with multiple public health degrees, this implies ≅200,000 people received a formal public health degree at some level during 2000–2015. By 2020, an additional 55,000 undergraduate and 77,000 graduate public health degrees will be awarded, according to conservative estimates.
Table 2.
Public Health Degrees Awarded, U.S., 2000–2015
| Year | Bachelor’s | Master’s | Doctoral | Total |
|---|---|---|---|---|
| 2000 | 1,622 | 5,340 | 559 | 7,521 |
| 2001 | 1,499 | 5,407 | 537 | 7,443 |
| 2002 | 1,438 | 5,536 | 533 | 7,507 |
| 2003 | 1,430 | 6,017 | 580 | 8,027 |
| 2004 | 1,469 | 6,590 | 653 | 8,712 |
| 2005 | 1,828 | 7,124 | 748 | 9,700 |
| 2006 | 2,209 | 7,520 | 755 | 10,484 |
| 2007 | 2,827 | 8,097 | 847 | 11,771 |
| 2008 | 3,376 | 8,736 | 872 | 12,984 |
| 2009 | 3,815 | 9,381 | 870 | 14,066 |
| 2010 | 4,485 | 10,165 | 948 | 15,598 |
| 2011 | 5,356 | 11,215 | 981 | 17,552 |
| 2012 | 6,464 | 12,201 | 1,173 | 19,838 |
| 2013 | 8,113 | 12,773 | 1,146 | 22,032 |
| 2014 | 9,629 | 13,514 | 1,238 | 24,381 |
| 2015 | 10,938 | 14,052 | 1,316 | 26,306 |
| Total | 66,498 | 143,668 | 13,756 | 223,922 |
Source: U.S. National Center for Education Statistics.
DISCUSSION
Reconciling supply and demand of the public health workforce is critical to quantifying workforce shortages and determining whether recent public health graduates can potentially meet impending turnover demands. This study represents the first reconciliation of public health workforce supply and demand data that considers planned and actual retirements, yielding a better understanding of workforce shortages to aid national workforce development efforts.
This study indicates that the projected demand for at least 65,000 new staff through 2020 can potentially be met by the influx of public health graduates (Table 3). NCES data suggest approximately 132,000 degrees in public health will be awarded in the U.S. during 2015–2019. However, given the recent growth in public health degrees conferred at the undergraduate and graduate levels,25,31 linear trends may be exceeded and upward of 150,000 undergraduate and graduate degrees could be conferred during this period. Furthermore, NCES reports a slight undercount of true conferrals among Association of Schools and Programs of Public Health members,33 which might indicate an underestimate of public health graduates in the pipeline. Although succession planning, the maintenance of institutional knowledge, regional variability in formally trained public health staff, and competition for staff with the private sector represent meaningful workforce challenges, nationwide raw supply numbers appear promising.
Table 3.
Estimates of Supply and Demand for State and Local Governmental Public Health Staff Before 2020
| Supply/demand categories | Estimates |
|---|---|
| Demand | |
| Total staff (SHA and LHD)a | 197,000 |
| Average annual FY2013–2015 staff separations (including retirements) | 11% |
| Staff planning to retire 2015–2019 | 47,000 |
| Estimated retirements 2017–2020 | 25,000–47,000 |
| Estimated voluntary, nonretirement separations 2017–2020 | 40,000–50,000 |
| Estimated retirement and other voluntary separations 2017–2020 | 65,000–97,000 |
| Supply | |
| Students receiving master’s/doctoral degrees 2015–2019b (assumes no growth) | 77,000 |
| Students receiving master’s/doctoral degrees 2015–2019c (assumes linear growth) | 83,000 |
| Students receiving bachelor’s degrees 2015–2019b (assumes no growth) | 55,000 |
| Students receiving bachelor’s degrees 2015–2019c (assumes linear growth) | 70,000 |
The state portion of this estimate is drawn from a nationally representative survey. The local portion comes from 13,000 LHD staff responses, which were extrapolated to the national LHD workforce.
Assumes no growth year-to-year, compared with 2015.
Assumes linear growth, compared with prior 3 years (baseline 2013–2015).
FY, fiscal year; LHD, local health department; SHA, state health agency.
Two additional points support the notion that graduate supply could meet workforce demands. First, a relatively limited percentage of LHD and SHA staff (17% overall) have any type of formal public health education.34 Although 75% of SHA staff had a bachelor’s degree and 38% had a master’s degree, the percentage of public health degrees was limited. Even if health departments continue hiring public health–trained staff at higher rates (as PH WINS data show34), other degree pipelines will meet some of the turnover and retirement needs. The second consideration, according to PH WINS, is that just 44% of SHA respondents and 29% of LHD respondents hold a position within the public health sciences, the most critical area for public health–specific training. This translates into approximately 70,000 staff nationwide, an estimated 16,000 of whom are planning to retire by 2020. A final consideration is that just 9% of those who say they are planning to retire or considering leaving are considering another position within public health—91% plan to leave the field.35 All public health graduates may not be suitable for, or interested in, these vacated positions. However, numerically, supply should plausibly meet demand.
These estimates do have implications for the severity of the potential workforce shortage. The public health enterprise should consider whether its workforce is aging at a higher rate than the general workforce or if fewer younger workers are being recruited. On average, public health staff are aged 48 years, 6 years older than the rest of the U.S. workforce, with 47% of the public health workforce aged ≥50 years, and 15% aged ≥60 years. Comparatively, only 15% of this workforce is aged <35 years.36 These findings are consistent with those reported among the Centers for Disease Control and Prevention employees, validating that the public health workforce is aging across the governmental enterprise. With an aging workforce, retirement is imminent. Although this study reports that approximately 25% of the SHA workforce is planning to retire by 2020, it also highlights that only about 54% of those planning to retire in FY2015 actually did. Although delayed retirement is more likely among those with a college degree, higher-paid occupations, and those in the health sector, evidence shows that those in the public sector did not delay retirement during the Great Recession.37–40 Exactly where retirement will be by 2020 remains unclear.
Despite a sizeable number of staff planning to retire, and a number of others indicating they are considering leaving their organization, these findings do not necessarily indicate a vast workforce shortage among health departments, particularly among staff in PHS positions. Vacancies are relatively consistent in proportion, separations are stable, and retirements are modest. The political winds are currently favoring smaller government, with some agencies continuing to offer early retirement. However, this might not always be the case. Although the public health system might have the pipeline from which to recruit and replace staff leaving the workforce, substantial implications exist for the transfer of institutional knowledge, succession planning, and the workforce more broadly. The 2016 WGS identified that a number of public health leaders felt they needed more candidates to fill their positions, and that offering competitive salaries was a significant challenge to recruitment efforts.36 With increasing student debt, decreasing funding of governmental public health, and continual increase in health spending, early career positions within government might be difficult to find and be relatively low paying. This might indicate that health departments are not competitive enough to attract the most qualified candidates, or, because hiring limitations or less competitive recruitment packages make the positions less attractive, the private, academic, and healthcare sectors might be siphoning recent graduates. Although increasing the number of public health workers in the healthcare delivery system is a positive outcome given the emphasis on population health and preventive care, governmental public health agencies have an important role in service delivery and will require workers with PHS expertise.
To address possible workforce shortages, public health leaders and decision makers should strategically speak with one voice41 and develop workforce planning models for public health agencies that include monitoring and evaluation of the workforce, along with relevant succession planning, as critical steps in ensuring key public health positions are maintained. Targeted efforts should emphasize reevaluation of retention practices, preparing talent within the organization, and planning recruitment activities for external candidates as well as developing cross-cutting skills in the workforce as an effective approach to maximizing human resources.
Limitations
This study has limitations stemming from data sources used and the imputation and extrapolation addressing missing data issues. ASTHO, NACCHO, and WGS data sources relied on self-reported data. NCES graduation data are self-reported by institutional registrars, which might introduce data errors. Furthermore, ASTHO and NACCHO profiles and NCES data are longitudinal, whereas PH WINS and WGS are cross-sectional. Supply and demand estimates created in this study that draw on local PH WINS staff data have the potential for bias, because the frame is not nationally representative. However, the actual variables used (proportion of respondents intending to retire) were consistent across all PH WINS frames, and data have broad utility for national estimates.42,43 Another limitation is reconciling self-reported estimates from different sources. Although quality-control analyses among comparable data points in the dataset were strong, results were not perfect. Additionally, substantial variation was observed between expected and actual retirements. Even though this was treated as a measure of how likely staff are to follow through on their intent to leave or retire, an alternative explanation relates to the actual retirements reported by SHAs. Future studies might consider asking these questions from the same instrument, or assembling more administrative data sources (rather than self-report). Finally, although outside the scope of this study, both the federal public health and primary care workforces substantially impact state and local decisions and would be valuable to include in future research.
CONCLUSIONS
This study represents a substantial contribution to understanding workforce shortages, and its findings reveal broader implications for public health workforce development. Considerable potential demand during the next few years was identified. Even if every staffer who planned to retire did retire, and all who were considering leaving their organizations did leave, the number of graduates with formal public health training would still far surpass the number needed for replacement nationally because of retirements or other voluntary separations. However, competitive recruitment practices and succession planning both would be of critical importance. Unknown is whether governmental public health can successfully compete with the private healthcare sector.
Only 17% of the workforce presently has formal public health training.34 Even among PHS staff, only 30% have a formal public health degree of some kind, and other undergraduate and graduate programs will likely be educating much of the workforce of the future despite the National Academy of Medicine’s stated desire that those in governmental public health have a formal public health degree.
This does not mean a workforce shortage is impossible, or even unlikely, because health departments have noted attracting qualified candidates and competing with other employers is challenging. Instead, workforce shortages might better be construed as more than a mere supply and demand numbers game, as supply might not exceed public health’s ability to recruit and retain the best staff to sufficiently meet future demand.
Supplementary Material
ACKNOWLEDGMENTS
Funding for this work was provided by the Centers for Disease Control and Prevention (NU38OT000161). The conclusions, findings, and opinions expressed by authors contributing to this manuscript do not necessarily reflect the official position of the Centers for Disease Control and Prevention.
Dr. Beck serves as an Assistant Editor for the American Journal of Preventive Medicine. She had no involvement in the peer review and decision-making processes for this paper.
No financial disclosures were reported by the authors of this paper.
Footnotes
SUPPLEMENTAL MATERIAL
Supplemental materials associated with this article can be found in the online version at https://doi.org/10.1016/j.amepre.2017.10.026.
REFERENCES
- 1.Sumaya CV. Enumeration and composition of the public health workforce: challenges and strategies. Am J Public Health. 2012;102(3):469–474. 10.2105/AJPH.2011.300388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beck AJ, Boulton ML. Building an effective workforce: a systematic review of public health workforce literature. Am J Prev Med. 2012;42(5 Suppl 1):S6–S16. 10.1016/j.amepre.2012.01.020. [DOI] [PubMed] [Google Scholar]
- 3.Gebbie K, Merrill J, Tilson HH. The public health workforce. Health Aff (Millwood). 2002;21(6):57–67. 10.1377/hlthaff.21.6.57. [DOI] [PubMed] [Google Scholar]
- 4.Sellers K, Leider JP, Harper E, et al. The Public Health Workforce Interests and Needs Survey: the first national survey of state health agency employees. J Public Health Manag Pract. 2015;21(Suppl 6): S13–S27. 10.1097/PHH.0000000000000331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Association of State and Territorial Health Officials. Budget cuts continue to affect the health of Americans. Research Brief. Update March 2012 https://www.aahd.us/wp-content/uploads/2012/04/ASTHO-Budget-Cuts-Impact-Research-0312.pdf. March 20, 2016.
- 6.Leider JP, Shah GH, Castrucci BC, Leep CJ, Sellers K, Sprague JB. Changes in public health workforce composition: proportion of part-time workforce and its correlates, 2008–2013. Am J Prev Med. 2014;47 (5 Suppl 3):S331–S336. 10.1016/j.amepre.2014.07.017. [DOI] [PubMed] [Google Scholar]
- 7.Robin N, Leep CJ. NACCHO’s National Profile of Local Health Departments Study: looking at trends in local public health departments. J Public Health Manag Pract. 2017;23(2):198–201. 10.1097/PHH.0000000000000536. [DOI] [PubMed] [Google Scholar]
- 8.Newman SJ, Ye J, Leep CJ. Workforce turnover at local health departments: nature, characteristics, and implications. Am J Prev Med. 2014;47 (5 Suppl 3):S337–S343. 10.1016/j.amepre.2014.07.023. [DOI] [PubMed] [Google Scholar]
- 9.Beck AJ, Boulton M, Lemmings J, Clayton JL. Challenges to recruitment and retention of the state health department epidemiology workforce. Am J Prev Med. 2012;42(1):76–80. 10.1016/j.amepre.2011.08.021. [DOI] [PubMed] [Google Scholar]
- 10.Leider JP, Harper E, Shon JW, Sellers K, Castrucci BC. Job satisfaction and expected turnover among federal, state, and local public health practitioners. Am J Public Health. 2016;106(10):1782–1788. 10.2105/AJPH.2016.303305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Association of County and City Health Officials. National Profile of Local Health Departments. 2014. http://archived.naccho.org/topics/infrastructure/profile/upload/2013-National-Profile-of-Local-Health-Departments-report.pdf.
- 12.Association of State and Territorial Health Officials. ASTHO Profile of Health. Volume 3; 2014. http://www.astho.org/Profile/Volume-Three/. [Google Scholar]
- 13.University of Michigan Center of Excellence in Public Health Workforce. Public Health Workforce Enumeration, 2012. 2013. http://www.phf.org/resourcestools/Documents/UM_CEPHS_Enumeration2012_Revised_July_2013.pdf.
- 14.Katz A, Felland LE, Hill I, Stark LB. A long and winding road: federally qualified health centers, community variation and prospects under reform. Res Brief. 2011;(21):1–9. [PubMed] [Google Scholar]
- 15.Merrill J, Btoush R, Gupta M, Gebbie K. A history of public health workforce enumeration. J Public Health Manag Pract. 2003;9(6):459–470. 10.1097/00124784-200311000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Gebbie KM. The Public Health Work Force: Enumeration 2000. U.S. DHHS, Health Resources and Services Administration, Bureau of Health Professions, National Center for Health Workforce Information and Analysis; 2000. [Google Scholar]
- 17.Gebbie KM, Raziano A, Elliott S. Public health workforce enumeration. Am J Public Health. 2009;99(5):786–787. 10.2105/AJPH.2008.137539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Beck AJ, Boulton ML, Coronado F. Enumeration of the governmental public health workforce, 2014. Am J Prev Med. 2014;47(5 Suppl 3): S306–S313. 10.1016/j.amepre.2014.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pourshaban D, Basurto-Davila R, Shih M. Building and sustaining strong public health agencies: determinants of workforce turnover. J Public Health Manag Pract. 2015;21(Suppl 6):S80–S90. 10.1097/PHH.0000000000000311. [DOI] [PubMed] [Google Scholar]
- 20.National Association of County and City Health Officials. National Profile of Local Health Departments. 2017. http://nacchoprofilestudy.org/.
- 21.Association of State and Territorial Health Officials. ASTHO Profile of Health. Volume 4; 2017. http://www.astho.org/Profile/. [Google Scholar]
- 22.Leider JP, Bharthapudi K, Pineau V, Liu L, Harper E. The methods behind PH WINS. J Public Health Manag Pract. 2015;21(Suppl 6): S28–S35. 10.1097/PHH.0000000000000285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Leep CJ, Shah GH. NACCHO’s National Profile of Local Health Departments study: the premier source of data on local health departments for surveillance, research, and policymaking. J Public Health Manag Pract. 2012;18(2):186–189. 10.1097/PHH.0b013e31824445ae. [DOI] [PubMed] [Google Scholar]
- 24.Fuller C The History and Origins of Survey Items for the Integrated Postsecondary Education Data System. National Postsecondary Cooperative. Washington, DC: U.S. Department of Education; 2013. [Google Scholar]
- 25.Association of Schools of Public Health. Annual Data Report 2013. Washington, DC; 2013. [Google Scholar]
- 26.Moser JM. Core academic competencies for master of public health students: one health department practitioner’s perspective. Am J Public Health. 2008;98(9):1559–1561. 10.2105/AJPH.2007.117234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bailey S Training the public health practitioner. J Public Health Manag Pract. 2003;9(2):87–88. 10.1097/00124784-200303000-00001. [DOI] [PubMed] [Google Scholar]
- 28.Stewart KE, Halverson PK, Rose AV, Walker SK. Public health workforce training: application of the Council on Linkages’ Core Competencies. J Public Health Manag Pract. 2010;16(5):465–469. 10.1097/PHH.0b013e3181ce4f0b. [DOI] [PubMed] [Google Scholar]
- 29.Sellers K, Leider JP, Harper M, et al. The Public Health Workforce Interests and Needs Survey: the first national survey of state health agency employees. J Public Health Manag Pract. 2015;21(Suppl 6):S13–S27. 10.1097/PHH.0000000000000331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hemans-Henry C, Blake J, Parton H, Koppaka R, Greene CM. Preparing Master of Public Health graduates to work in local health departments. J Public Health Manag Pract. 2016;22(2):194–199. 10.1097/PHH.0000000000000232. [DOI] [PubMed] [Google Scholar]
- 31.Leider JP, Castrucci BC, Plepys CM, Blakely C, Burke E, Sprague JB. Characterizing the growth of the undergraduate public health major: U.S., 1992–2012. Public Health Rep. 2015;130(1):104–113. 10.1177/003335491513000114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Riegelman RK. Undergraduate public health education: past, present, and future. Am J Prev Med. 2008;35(3):258–263. 10.1016/j.amepre.2008.06.008. [DOI] [PubMed] [Google Scholar]
- 33.National Association of County and City Health Officials. 2008 National Profile of Local Health Departments. 2009. http://archived.naccho.org/topics/infrastructure/profile/resources/2008report/upload/NACCHO_2008_ProfileReport_post-to-website-2.pdf.
- 34.Leider JP, Harper E, Bharthapudi K, Castrucci BC. Educational attainment of the public health workforce and its implications for workforce development. J Public Health Manag Pract. 2015;21(Suppl6):S56–S68. 10.1097/PHH.0000000000000306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liss-Levinson R, Bharthapudi K, Leider JP, Sellers K. Loving and leaving public health: predictors of intentions to quit among state health agency workers. J Public Health Manag Pract. 2015;21(Suppl 6): S91–S101. 10.1097/PHH.0000000000000317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bureau of Labor Statistics. Educational attainment for workers 25 years and older by detailed occupation. 2013. https://www.bls.gov/emp/ep_table_111.htm.
- 37.Levanon G, Cheng B. U.S. workers delaying retirement: who and why and implications for businesses. Bus Econ. 2011;46(4):195–213. 10.1057/be.2011.27. [DOI] [Google Scholar]
- 38.Scommegna P U.S. Baby Boomers Likely to Delay Retirement. Population Reference Bureau. 2014. www.prb.org/Publications/Articles/2014/us-babyboomers-retirement.aspx. Accessed November 16, 2017.
- 39.Munnell AH, Sanzenbacher GT, Rutledge MS. What Causes Workers to Retire Before They Plan? Center for Retirement Research; 2015. http://crr.bc.edu/working-papers/what-causes-workers-to-retire-before-they-plan/. [Google Scholar]
- 40.Kerrigan H Government Unprepared for Boomers’ Mass Exodus. http://www.governing.com/gov-government-unprepared-for-boomers-mass-exodus.htmlGoverning.com. December 1, 2012.
- 41.Kaufman NJ, Castrucci BC, Pearsol J, et al. Thinking beyond the silos: emerging priorities in workforce development for state and local government public health agencies. J Public Health Manag Pract. 2014;20(6):557–565. 10.1097/PHH.0000000000000076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shah GH, Madamala K. Knowing where public health is going: levels and determinants of workforce awareness of national public health trends. J Public Health Manag Pract. 2015;21(Suppl 6):S102–S110. 10.1097/PHH.0000000000000312. [DOI] [PubMed] [Google Scholar]
- 43.Ye J, Leep C, Robin N, Newman S. Perception of workforce skills needed among public health professionals in local health departments: staff versus top executives. J Public Health Manag Pract. 2015; 21(suppl 6):S151–S158. 10.1097/PHH.0000000000000299. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.