Abstract
Objective
Urethral injury occurs in 10% of patients who suffer from pelvic fractures. Urethroplasty is performed after an interval of 3 months to stabilize the perineal hematoma. It has been reported that the rate limiting step in anastomotic urethroplasty is finding the posterior urethra. Even for the most experienced surgeons, at times, this step can be challenging. The aim of the present study was to describe a novel technique for understanding the three-dimensional (3D) anatomy which would also help in surgical planning and making urethroplasty easy, a step ahead of conventional imaging.
Material and methods
Ours is a tertiary referral center with an experience of >1307 cases of pelvic fracture urethral distraction defects. This study was conducted between January 2018 and July 2018. Ethics approval was obtained. No patients incurred any cost for the study. A computerized tomography scan was performed with the bladder filled with contrast saline, and the same solution was injected into the anterior urethra, with a gauze piece tied around the glans. 3D images were then reconstructed, and data were transferred to the 3D Ultimaker™ printer. 3D models were printed to mimic the anatomy of pelvic fracture urethral distraction.
Results
A total of 10 models were created. The models, along with conventional urethrogram, were shown to fellows and observers. Visually, they gave a score of 4.3/5. In correlation with urethroplasty, understanding the anatomy of the posterior urethra was also important.
Conclusion
3D printing can be applied to pelvic fracture urethral injury to understand the anatomy of the posterior urethra, its distance from the rectum, length of gap, relation to the posterior urethra, direction of displacement of the urethra, and if pubectomy is required or not.
Keywords: 3D printing, pelvic fracture urethral injury, urethroplasty
Introduction
Urethral injury occurs in 10% of patients who suffer from pelvic fracture. Urethral injury spectrum may vary from a minor stretch injury where urethral continuity is maintained as opposed to a severe injury disrupting the bladder neck and involvement of the rectum. The current standard of care is delayed repair after the initial urinary drainage using a suprapubic catheter (SPC). Delayed repair is usually performed after an interval of 3 months to help stabilize the perineal hematoma. The posterior urethra, which includes the membranous urethra, prostate, and bladder, is invariably displaced upwards.
The most unpredictable part of the operation is what additional steps may be required to bridge the gap between the two ends of the urethra. Mundy et al.[1] quoted that the rate limiting step in anastomotic urethroplasty is finding the posterior urethra. Even for the most experienced surgeon, this step can be quite challenging.
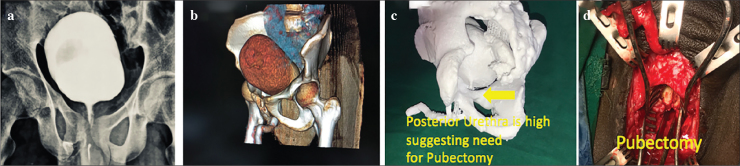
The preoperative assessment includes a retrograde urethrogram and micturating urethrogram (Figure 1a). However, this imaging modality is two-dimensional. It is hard to correctly predict from this imaging the direction in which the posterior urethra may be pulled. The posterior urethra may be pulled posteriorly toward the rectum or anteriorly toward the pubic bone while at times it is somewhere in between. In complex cases, CT scan or MRI may be performed to evaluate the proximal end of the urethra.
Figure 1. a–d.
MCU of a patient with PFUI. (a) 3D reconstruction on CT scan. (b) 3D printed model. (c) The posterior urethra is above the inferior margin of the pubic bone as depicted by the printed model, suggesting the need for inferior pubectomy (d)
In the present study, we describe a novel method to ascertain this complex anatomy in a three-dimensional view and help predict the steps of the subsequent repair.
Material and methods
Our tertiary referral center has performed approximately 4358 urethroplasties since 1995. We have one of the largest databases of PFUI repairs, with 1307 urethroplasties. We have shared our experience on managing these complex repairs in our recent study.[2]
A case-control ethics-approved pilot study was conducted over a period of 7 months from January 2018 to July 2018 including 10 consecutive patients with PFUI. The study was approved by the ethics committee. Written informed consent was obtained from the patients. No patients incurred any cost for the CT scan or 3D printing.
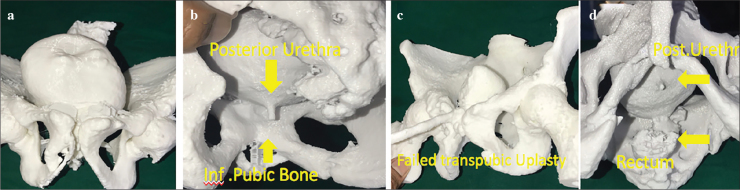
A CT scan was performed on all patients to evaluate the anatomical relationship of the two ends of the urethra (Figure 1b). The bladder was filled through the SPC tract with an admixture of sterile normal saline and radiocontrast. A 50 mL diatrizoate meglumine injection (65%) diluted in 500 mL sterile normal saline was used. The anterior urethra was distended with the same solution, and a gauze piece was tied at the glans to retain the mixture. A CT scan of the pelvis was performed from the distended bladder to the penis. The scan time was <10 s. The CT images are then processed in standard 3D reconstructive software. The Ultimaker™ 3D printer was then used to reconstruct a 3D printed model of the anatomy (Figures 1c, d, 2a–d, 3a, b). It uses acrylic fibers to reconstruct a 3D printed model, which averagely takes 20 h. This was performed for each of the 10 patients in the study.
Figure 2. a–d.
Frontal view of another patient with a three-dimensional printed model. (a) Posterior view showing the relationship of the posterior urethra with the inferior border of the pubic bone, suggesting the need for pubectomy. (b) 3D printed model of another patient with small bladder, transpubic urethroplasty showing the dilated posterior urethra and end to side anastomosisfrontal view. (c) Inferior view (d)
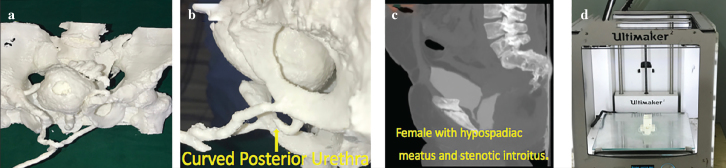
Figure 3. a–d.
3D printed model of another patient showing long gap. (a) Inferior view showing the posterior urethra which is curved upwards. (b) 3D CT of a girl showing PFUI with urethrovaginal fistula. (c) 3D printer (d)
Results
These models help us understand the anatomy of the posterior urethra. These depicted the exact displacement of the posterior urethra, its relation to the pubic bone, its relation to the rectum, displacement from the midline, and also the status of the anterior urethra. In a female patient after PFUI, she had continence with incontinence of urine. On 3D CT (Figure 3c) scan and then 3D printing, it was found that she was voiding in the vagina due to hypospadiac meatus. We operated based on this and made a distal pedicled labial flap tube, and the patient is continent.
We also conducted a survey of visiting urologists who come to our center for fellowship and observership (2 fellows, 2 consultants, and >30 visiting urologists in that time frame). We showed them the preoperative urethrogram and 3D models of all participating patients. The survey asked if the models were useful for them to make a preoperative assessment of requirement of inferior pubectomy to bridge the gap between the two ends of the urethra. The opinion of all of them suggested that these were extremely useful. The anatomy of the injury studied on 3D models prior to urethroplasty helped in better surgical time. However, this cannot be statistically analyzed as it is the subjective perception of the observing and operating urologist.
Discussion
3D printing has been extensively tried and tested for automobile components and artificial limbs, and now trials are being undertaken for medical science. Currently, the available 3D printers (Figure 3D) use acrylic fibers for printing.
Most 3D printers use CT imaging to print models. High-speed printers are available but are associated with a high cost of printing. These printers need imaging performed with radiocontrast to acquire 3D images. Printed models can mimic real-life anatomy or can be downsized to miniature models. Scaling down provides an option of reducing the cost and time of printing.
Thus far, surgery involved imaging a three-dimensional image from a two-dimensional imaging modality. PFUI repairs are one of the most complex surgeries performed by reconstructive urologists worldwide.
The question for each reconstructive urologist is the gap between the two ends of the urethra and the steps required to bridge the gap.[1] A routine Retrograde Urethrogram and Micturating urethrogram gives a basic understanding of the anatomy. The aim of our pilot study was to evaluate if 3D imaging assists in better preoperative planning in these cases.
3D printing can help understand the following:
Complex anatomy of the posterior urethra, such as Re Re do PFUI, bulbar necrosis, rectourethral fistula, young girls with urethrovaginal fistula, bladder neck injury, and double block,[2]
Its distance from the rectum,
Length of the urethral gap,
Relation to the posterior urethra,
Direction of displacement of the urethra,
If inferior pubectomy is required or not.
The limitations of the study include that this can be pursued as a randomized study between multicenters. The technology of 3D printing may not be easily available, and the model is scaled to 80% size for faster availability. True depiction would be to print 100% original size of the patient. Faster 3D printers including the soft tissues may improve further the perception of 3D printing.
We are considering future 3D printing utilizing a material similar to the bone. This will help reconstructive urologists practice pubectomy on the 3D model prior to surgical repair, which may reduce the operative time and improve outcomes.
In conclusion, 3D printing of PFUI is feasible using the CT scan data. It could be useful as a training tool for urologists or can be used for complex cases.[3] In our high-volume center, we have used it for complex PFUI.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the ethics committee of Kulkarni Reconstructive Urology Cneter (Protocol 004/2018).
Informed Consent: Written informed consent was obtained from patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – P.M.J.; Design – P.M.J.; Supervision – S.B.K.; Resources – P.M.J., S.B.K.; Materials – P.M.J.; Data Collection and/or Processing – P.M.J.; Analysis and/or Interpretation – P.M.J., S.B.K.; Literature Search – P.M.J., S.B.K.; Writing Manuscript – P.M.J.; Critical Review – P.M.J., S.B.K.; Other – P.M.J., S.B.K.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Mundy AR. Urethroplasty for posterior urethral strictures. Br J Urol. 1996;78:243–7. doi: 10.1046/j.1464-410X.1996.11617.x. [DOI] [PubMed] [Google Scholar]
- 2.Kulkarni SB, Surana S, Desai DJ, Orabi H, Iyer S, Kulkarni J, et al. Management of complex and redo cases of pelvic fracture urethral injuries. Asian J Urol. 2018;5:107–17. doi: 10.1016/j.ajur.2018.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cacciamani GE, Okhunov Z, Meneses AD, Rodriguez-Socarras ME, Rivas JG, Porpiglia F, et al. Impact of Three-dimensional Printing in Urology: State of the Art and Future Perspectives. A Systematic Review by ESUT-YAUWP Group. Eur Urol. 2019;76:209–21. doi: 10.1016/j.eururo.2019.04.044. [DOI] [PubMed] [Google Scholar]